Abstract
Purpose
This study evaluates accuracy of self-reported weight in adolescent bariatric surgery patients.
Materials and Methods
During follow-up visits, participants self-reported weight and had weight measured. Differences between self-reported and measured weights were analyzed from 60 participants.
Results
Participants were 70% (n=42) female, 72% (n=43) white, mean age of 20.8 years and median body mass index of 36.6 kg/m2. At an average 3.5 years following surgery, females underestimated weight (0.5kg, range: −18.7 to 5.6kg), while males overestimated (1.1kg, range: −7.8 to 15.2kg). Most (80%, n=48) reported within 5kg of measured weight. The majority of adolescents who previously underwent bariatric surgery reported reasonably accurate weights, but direction of misreporting varied by gender.
Conclusion
Self-reported weights could be utilized when measured values are unavailable without markedly biasing the interpretation of outcomes.
Introduction
Self-reported body weights are frequently utilized in epidemiologic studies, since they are relatively low burden and inexpensive. Many investigators have cautioned against use of self-reported weight estimates in obese populations due to underreporting bias1–3, and indeed there is evidence to also suggest that underreporting in adolescent females may increase over time as they age into adulthood4. Similar underreporting relationships have also been observed within middle-aged bariatric cohorts5, 6. However, the literature currently lacks information regarding the accuracy of self-reported weight within adolescent bariatric populations. To address this gap in the literature, we sought to examine the accuracy of self-reported weight in adolescents who had undergone bariatric surgery.
Methods
The Teen Longitudinal Assessment of Bariatric Surgery (Teen-LABS) study is an ongoing prospective, multi-center investigation of the safety and efficacy of bariatric surgery in adolescents ages 19 and younger7, 8. Analyses were restricted to participants who had completed a post-operative study visit between 6 months and 6 years, and for whom post-operative weight data included a (1) self-reported weight gathered during a visit scheduling phone call, and (2) a subsequent measured weight within 30 days, collected in-person using an electronic scale (Tanita Scale Model TBF310). For participants with self-reported and measured data across multiple study time points (n=10), a single time point was randomly selected, resulting in an analysis sample of 60 subjects.
Frequencies and percentages were calculated for categorical variables. Means and standard deviations or medians and interquartile ranges (IQR) were calculated for continuous variables. Fisher’s exact, t-test, and Wilcoxon rank-sum tests were used to compare characteristics by sex. Difference in weight measurement, calculated as self-reported minus measured, was evaluated using Bland-Altman plots9. Median differences were plotted against the measured weight values, with the 5th and 95th percentiles of the difference utilized as the limits of agreement9. Wilcoxon signed rank tests were used to determine if median sex-specific difference in weight measurement values differed from zero. Gender-stratified robust linear regression models were used to evaluate the association between measured weight and the difference of weight values. Covariates considered for inclusion in the adjusted models included: age, race, study visit location (clinic, home), and time since surgery. Reported p-values are two-sided and considered statistically significant at < 0.05.
Results
Sixty participants were evaluated, of which 42 were female (70%), 72% were white, and the majority underwent Roux-en-Y gastric bypass (67%) (Table 1). Mean age at baseline was 17.2 years (min: 13, max: 19) and median baseline BMI (measured weight) was 50.9 kg/m2 (min: 41, max: 87). At the point of post-operative measurement (average of 3.5 years post bariatric surgery), mean age was 20.8 years and median BMI (measured weight) was 36.6 kg/m2. Median self-reported body weights were 96.6kg for females and 115.2kg males, while the measured weight (on average, 15 days following self-report) was 98.5kg and 112.6kg for females and males, respectively. Overall, participants underestimated weight by 0.3 kg (min: −18.7kg, max: +15.2kg). Most (80%) participants reported weight values within 5kg of measured values, while 93% fell within ±10kg. Crude comparisons between subjects reporting within ± 5kg and beyond ± 5kg of true weight indicated the more accurate reporters had a lower BMI at the post-operative measure (35.1 vs. 43.2 kg/m2, p=0.03) (Table 2).
Table 1.
Subject characteristics by sex.
| Total (N=60) |
Female (n=42) |
Male (n=18) |
p-value* | |
|---|---|---|---|---|
| Age at Surgery (years), x̄ (SD) | 17.3 (1.72) | 17.2 (1.67) | 17.4 (1.89) | 0.68 |
| Age at Measurement (years), x̄ (SD) | 20.8 (2.10) | 20.8 (2.04) | 20.7 (2.28) | 0.84 |
| Race | 0.19 | |||
| White | 71.7% (43) | 66.7% (28) | 83.3% (15) | |
| Non-white | 28.3% (17) | 33.3% (14) | 16.7% (3) | |
| Surgical Procedure, % (n) | 0.30 | |||
| Roux-en-Y Gastric Bypass | 66.7% (40) | 71.4% (30) | 55.6% (10) | |
| Gastric Band | 8.3% (5) | 9.5% (4) | 5.6% (1) | |
| Sleeve gastrectomy | 25.0% (15) | 19.1% (8) | 38.9% (7) | |
| Years since surgery, x̄ (SD) | 3.5 (1.42) | 3.6 (1.36) | 3.3 (1.58) | 0.42 |
| Baseline Body Mass Indexa, median (IQR) | 50.9 (45.4,58.4) | 50.1 (45.2,57.0) | 53.9 (48.7,60.8) | 0.18 |
| Visit location, % (n) | 0.71 | |||
| Clinic | 51 (85.0%) | 35 (83.3%) | 16 (88.9%) | |
| Home | 9 (15.0%) | 7 (16.7%) | 2 (11.1%) | |
| Body Mass Indexa at measurement, median (IQR) | 36.6 (30.7,43.9) | 36.6 (30.6,44.0) | 37.3 (33.1,43.8) | 0.87 |
| Percent Weight changeb, x̄ (SD) | −26.9 (16.04) | −26.3% (16.01) | −28.3% (16.49) | 0.67 |
| Measured Weight (kg), median (IQR) | 103.8 (88.0,127.4) | 98.5 (86.4,118.7) | 112.6 (100.8,143.9) | 0.03 |
| Self-reported Weight (kg), median (IQR) | 100.9 (86.1,124.1) | 96.6 (85.0,113.6) | 115.2 (100.0,147.7) | 0.01 |
| Difference in weightc, median (IQR) | −0.3 (−2.7,1.6) | −0.5 (−2.9,0.9) | 1.1 (−2.5,2.9) | 0.12 |
| Days between Report & Measured Weight, x̄ (SD) | 15.4 (8.85) | 15.5 (8.27) | 15.1 (10.33) | 0.85 |
Females compared to males.
Using measured weight.
Percent weight change from baseline measurement.
Difference = (Self-report minus Measured).
SD = Standard Deviation.
IQR = Interquartile range.
Table 2.
Select Characteristics by Level of Self-Report Accuracy (Within ±5kg, Beyond ±5kg).
| Within ±5kg | Beyond ±5kg | p-value | |
|---|---|---|---|
| N | 48 | 12 | |
| Age at Measurement (years), x̄ (SD) | 33 (68.8%) | 9 (75.0%) | 0.99 |
| Females, n (%) | 37 (77.1%) | 6 (50.0%) | 0.08 |
| White, n (%) | 20.9 (2.19) | 20.4 (1.68) | 0.43 |
| Visit Location=Clinic, n (%) | 40 (83.3%) | 11 (91.7%) | 0.67 |
| Years since surgery, x̄ (SD) | 3.4 (1.48) | 3.8 (1.18) | 0.38 |
| Body Mass Index at measurement, median (IQR) | 35.1 (29.0,42.2) | 43.2 (37.4,49.3) | 0.03 |
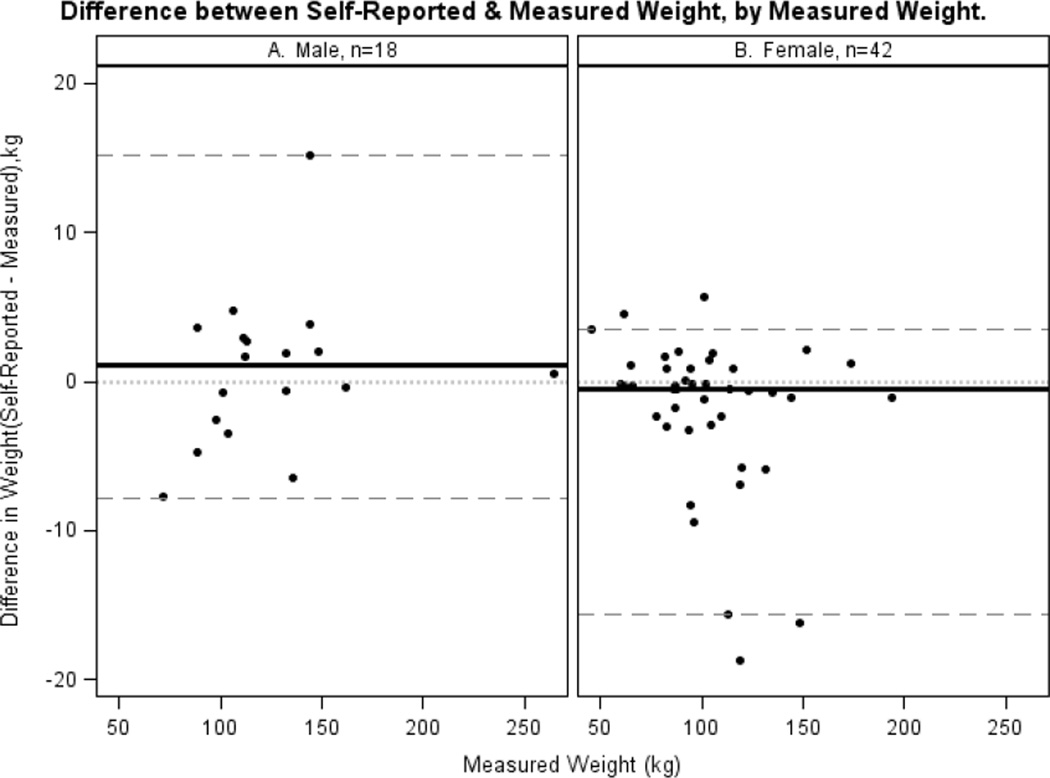
Females underestimated true weight by 0.5kg (p=0.0498), while males overestimated true weight by 1.1kg (p=0.65). Bland-Altman plots of difference in self-reported and measured weight by measured weight are presented by sex (Figure 1). These plots suggest females tend to increasingly underreport as measured weight increases, while no strong pattern is apparent among males. However, adjusted regression analyses indicate that the accuracy of self-reported weight did not vary as a function of measured weight in females (p=0.31) or males (p=0.52). No other characteristics, including time since surgery, were found to be significantly associated with self-reported weight accuracy.
Figure 1. Difference between Self-Reported & Measured Weight, by Measured Weight.
Panel A. Male, n=18.
Panel B. Female, n=42.
Discussion
Increasingly, adolescents are seeking weight loss procedures for management of severe obesity. Documenting outcomes of these procedures in adolescents is important, but one challenge is assessing weight longitudinally by direct measure in this increasingly mobile population. Conducting outcomes research using patient reported data collected remotely (e.g., by web-based or by telephonic data collection) is more feasible than performing in-person visits, especially for those participants who must travel large distances to reach the clinical center. Thus, it would be useful to better understand the potential error introduced by self-report estimates of weight. In this analysis, among adolescents who underwent weight loss surgery 6 months to 6 years prior to study, the accuracy of self-reported weights gathered by phone call was similar to that observed in an adult bariatric population5. Both males and females reported weights that were, on average, within 1kg of their weights as measured at a research visit within a month of the self-reported weight. However, in this sample males modestly overestimated their weight while females modestly underestimated their weights.
Prior studies have documented that obese adolescents provide more biased estimates of their weight than leaner peers6. Others have found a divergence in direction of error in self-reported estimates of weight by gender. Field and colleagues examined over four thousand participants in the National Longitudinal Study of Adolescent Health to assess predictors of discrepancy between weights based on self-reported vs. measured weights. They found obese males under-reported their weights by approximately 6 pounds (2.7kg) and females under-reported by 10 pounds (4.5kg)10. The reasons for the better accuracy of self-reported weight in our Teen-LABS sample are not clear, but it is possible that individuals who have undergone bariatric surgery have a greater awareness of factors associated with weight change or maintenance through exposure to a multidisciplinary clinical team8, or may simply measure their weight more frequently.
Strengths of this study include use of standardized and scripted telephone interviews for collection of self-reported data, as well as uniform and protocol-driven weight measurements within a short period after telephone interview. Limitations include the fact that the study population was largely non-Hispanic, Caucasian and female, thus generalizability is limited. Findings are also limited due to small sample size, especially among males (n=18). Also, we cannot assume from these data that the accuracy of self-report is maintained over longer term follow-up.
Conclusion
In summary, this evidence suggests that for the majority of a post-operative bariatric sample of adolescents and young adults, self-reported weight reflects true weight reasonably well, and can thus be considered a valid surrogate when scale weight measurements are not available. However, additional research in larger, more racially and ethnically diverse populations is required to confirm our findings.
Acknowledgments
Grant Information: The Teen-LABS consortium is funded by cooperative agreements with the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), through grants: U01DK072493 (PI, Dr. Thomas Inge, CCHMC), UM1DK072493 (PI, Dr. Thomas Inge, CCHMC), and UM1DK095710 (PI, Dr. Ralph Buncher, University of Cincinnati). The study is also supported by grants UL1 TR000077-04 (Cincinnati Children’s Hospital Medical Center), UL1RR025755 (Nationwide Children’s Hospital), M01-RR00188 (Texas Children’s Hospital/Baylor College of Medicine), UL1 RR024153 and UL1TR000005 (University of Pittsburgh), UL1 TR000165 (University of Alabama, Birmingham).
Footnotes
Conflict of Interest Statement: Todd M Jenkins, Tawny W Boyce, C Ralph Buncher, Meg H Zeller, Anita P Courcoulas, Mary Evans, and Thomas H Inge all declare that they have no conflicts of interest related to this article.
Statement of Informed Consent: Informed consent was obtained from all individual participants included in the study.
Statement of Human Rights: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- 1.Himes JH, Faricy A. Validity and reliability of self-reported stature and weight of US adolescents. Am J Hum Biol. 2001;13(2):255–260. doi: 10.1002/1520-6300(200102/03)13:2<255::AID-AJHB1036>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 2.Himes JH, Hannan P, Wall M, Neumark-Sztainer D. Factors associated with errors in self-reports of stature, weight, and body mass index in Minnesota adolescents. Ann Epidemiol. 2005;15(4):272–278. doi: 10.1016/j.annepidem.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 3.Brener ND, McManus T, Galuska DA, Lowry R, Wechsler H. Reliability and validity of self-reported height and weight among high school students. J Adolesc Health. 2003;32(4):281–287. doi: 10.1016/s1054-139x(02)00708-5. [DOI] [PubMed] [Google Scholar]
- 4.Clarke P, Sastry N, Duffy D, Ailshire J. Accuracy of self-reported versus measured weight over adolescence and young adulthood: findings from the national longitudinal study of adolescent health, 1996–2008. Am J Epidemiol. 2014;180(2):153–159. doi: 10.1093/aje/kwu133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Christian NJ, King WC, Yanovski SZ, Courcoulas AP, Belle SH. Validity of self-reported weights following bariatric surgery. JAMA. 2013;310(22):2454–2456. doi: 10.1001/jama.2013.281043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.White MA, Masheb RM, Burke-Martindale C, Rothschild B, Grilo CM. Accuracy of self-reported weight among bariatric surgery candidates: the influence of race and weight cycling. Obesity (Silver Spring) 2007;15(11):2761–2768. doi: 10.1038/oby.2007.328. [DOI] [PubMed] [Google Scholar]
- 7.Inge TH, Zeller M, Harmon C, et al. Teen-Longitudinal Assessment of Bariatric Surgery: methodological features of the first prospective multicenter study of adolescent bariatric surgery. J Pediatr Surg. 2007;42(11):1969–1971. doi: 10.1016/j.jpedsurg.2007.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Michalsky MP, Inge TH, Teich S, et al. Adolescent bariatric surgery program characteristics: the Teen Longitudinal Assessment of Bariatric Surgery (Teen-LABS) study experience. Semin Pediatr Surg. 2014;23(1):5–10. doi: 10.1053/j.sempedsurg.2013.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8(2):135–160. doi: 10.1177/096228029900800204. [DOI] [PubMed] [Google Scholar]
- 10.Field AE, Aneja P, Rosner B. The validity of self-reported weight change among adolescents and young adults. Obesity (Silver Spring) 2007;15(9):2357–2364. doi: 10.1038/oby.2007.279. [DOI] [PubMed] [Google Scholar]