Abstract
Objectives
The purpose of this cross-sectional study was to examine differences in hip abductor (ABD) strength and composition between older adults who primarily use medial vs cross-step recovery strategies to lateral balance perturbations.
Design
Cross-Sectional
Setting
University Research Laboratory
Participants
Forty community dwelling older adults divided into medial steppers (N=14) and cross-steppers (N=26) based on first step of balance recovery after a lateral balance perturbation.
Interventions
Not applicable
Main Outcomes
CT scans to quantify lean tissue (LT) and intramuscular adipose tissue (IMAT) IMAT areas in the hip ABD, Hip ABD isokinetic torque and first step length.
Results
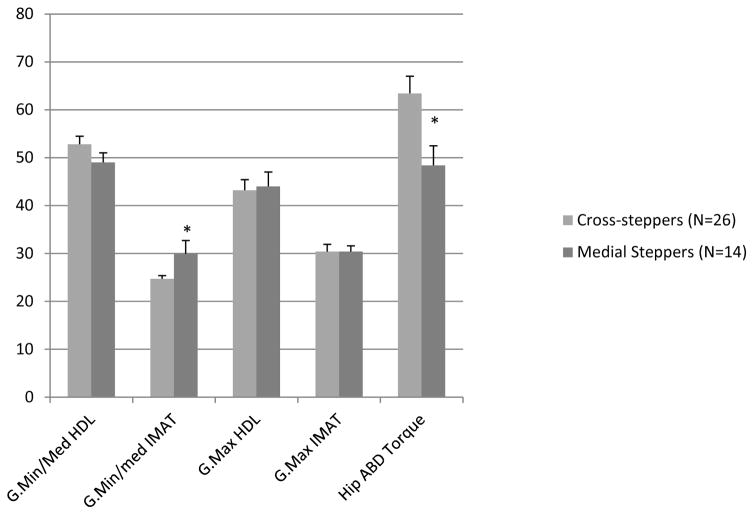
Medial steppers took medial-steps in 71.1% of trials vs 4.6% of trials with cross-steps. The cross steppers when compared with medial steppers, had lower hip ABD IMAT (24.7 ± 0.7 vs 29.9 ± 2.8%; p<0.05), greater ABD torque (63.3 ± 3.6 vs 48.4 ± 4.1 N.M; p<0.01), and greater 1st step-length (0.75 ± 0.03 vs 0.43 ± 0.08; p<0.001). There was no difference in hip ABD LT between the groups (p>0.05).
Conclusions
Our findings suggest that older adults who initially use a medial step to recover lateral balance have lower hip ABD torque and may be less able to execute a biomechanically more stable cross-step. This may be related to increased IMAT levels. Assessments and interventions for enhancing balance and decreasing fall risk should take the role of the hip ABD into account.
Keywords: Falls, stepping, balance recovery, hip abductors, muscle strength, intramuscular fat
Injurious falls due to impaired balance function are a leading cause of morbidity and mortality amongst older adults. 1 The ability to safely maintain mobility with aging is critical as immobility is the leading cause of long term care admissions.2 While the causes of balance dysfunction and dysmobility are multifactorial in nature, recent evidence demonstrates that high levels of intramuscular adipose tissue (IMAT) within the postural and locomotor muscles is associated with increased risk of falls,3,4 and may be related to decreased muscle activation,5 altered balance,3,6 and impaired stepping behavior 3,6 ultimately contributing to altered mobility and balance function.6–11 In particular, greater levels of IMAT in the gluteal muscles appears to be especially problematic for older adults as it relates to decreased hip abductor strength, increased gait variability, and decreased balance. 3,6 Furthermore, higher levels of IMAT are found in the hip abductors of older adults with a self-reported history of falls.3
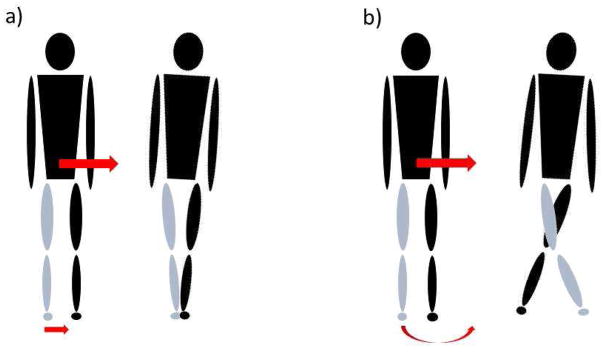
The impairment of hip abductor muscles may contribute to an inability to meet the high functional demands of gait and limit the ability of older adults to safely recover from imbalance especially in the lateral direction.12,13 The vulnerability to loss of balance in the lateral direction with aging has been hypothesized to be due in part to the unique biomechanical challenges of lateral balance recovery.12,13 When protective steps are taken in response to disturbances of standing balance, alterations in the base of support (BOS) through stepping must be effectively directed, timed, and repositioned in relation to the position and motion of the body center of mass (COM) in order to sustain standing stability. During externally applied lateral challenges to balance, the COM is initially displaced sideways such that the lower limb on the side of the direction of imbalance is passively loaded together with a concomitant unloading of the opposite limb.14–16 Following lateral waist-pull perturbations of standing balance, younger adults frequently perform a single lateral step with the passively loaded limb to recover balance. In contrast, older individuals more commonly use either cross-over steps with the unloaded limb or, especially if they have a history of falls, a short-medial step with the passively unloaded limb (Fig. 1).17 Reliance on a medial stepping strategy to recover lateral balance may be more problematic for effectively stabilizing balance than the lateral or crossover steps because it initially limits the change in BOS needed to recover balance. This limitation invariably necessitates that a second lateral step with the opposite limb be taken to recover balance.
Figure 1.
Types of induced first-step protective responses following a waist perturbation. The arrow indicates the direction of pull. The grey leg is the stepping leg and black leg the stance leg. a) Demonstrates a medial recovery step while b) shows a cross-over recovery step.
It has been hypothesized that the medial stepping strategy may be attributable to impaired hip abductor muscle performance as it does not require the rapid torque production needed to unload the passively loaded limb for lateral stepping, and avoids the longer time in single limb support and more complex limb trajectory associated with crossover-stepping.14,15 These observations suggest that adults with impaired lateral balance function who utilize a medial stepping strategy, may do so due to impaired hip abductor muscle- performance. However, the relationships between impaired hip abductor strength and associated muscle composition changes with protective stepping behavior remains to be determined. Therefore, the purpose of this study was to compare the hip abductor muscle strength and composition between older adults who primarily use-an initial medial stepping strategy with those who mainly perform cross-over stepping for balance recovery following externally applied lateral waist-pull perturbations. We hypothesized that older adults who primarily use a medial stepping strategy to maintain standing balance will have lower hip abductor muscle strength and greater IMAT compared to older adults who utilize more biomechanically complex crossover stepping.
METHODS
Participants
Healthy community dwelling older adult volunteers were recruited for this study. All participants were part of a larger study focused on examining lateral balance stability in older adults and were recruited from the Baltimore/Washington area. Complete inclusion/exclusion criteria have been previously reported. 3,6 Briefly, inclusion criteria included: age ≥ 65 years and being a healthy community dwelling individual able to complete all muscle composition, and balance testing. Exclusion criteria included: a significant cognitive impairment, depression, the inability to ambulate independently without the use of an assistive device, or current engagement in a structured exercise program 3 or more days per week. Participants were initially screened via telephone by the recruitment staff, followed by a medical examination performed by a physician geriatrician to ensure the participant met all requirements for inclusion/exclusion criteria. Height (m) and weight (kg) were measured and used to calculate BMI. Because obesity is known to result in muscle fatty infiltration, for this analysis we sought to include only individuals who had a BMI of less than 30 kg/m2. A fall assessment was conducted during the initial telephone screening and consisted of a fall history during the past 12 months. A faller was classified as anyone who had experienced a fall in the last 12 months as per the World Health Organization criteria.18 All subjects provided written informed consent that was approved by the research ethics committee from the Institutional Review Board of University of Maryland, Baltimore and the Baltimore Veteran’s Administration Research and Development prior to participation.
Muscle Composition
Computed tomography (CT) methods have previously been reported in detail. 3,6 Participants underwent a continuous CT scan (Siemens Somatom Sensation 64 Scanner) from the 2nd lumbar vertebrae to the patella. Muscle composition and cross sectional area of high density lean tissue (HDL) and low density lean tissue (IMAT) of the gluteus maximus (g.max) and the gluteus medius and minimus (g.min/med) were determined using Medical Image Processing, Analysis and Visualization (MIPAV, v 7.0, NIH) software, with procedures previously reported.19 CT data for each muscle was expressed as a cross-sectional area of tissue (cm2) using Hounsfield units (HU) for HDL between 30–80 and IMAT as 0–29. HDL and IMAT were normalized for the respective muscle’s size by calculating a percentage of each measure relative to the muscle cross sectional area.
Strength Testing
Peak torque of the hip abductors was determined utilizing isokinetic strength testing (Biodex System 4, Biodex Medical Systems, Shirley, NY) conducted by trained staff. Bilateral concentric contractions were performed at 60°/s from 0° to 30° of hip abduction in supported standing.3 An external stabilization frame was used to minimize extraneous body movements while standing as reported in prior studies. 20
Balance and Postural Perturbation Testing
The Dynamic Gait Index (DGI) was used to assess clinical dynamic balance.21,22 The DGI consist of 8-itmes to measure dynamic balance including walking: on level surface, with changing speed, horizontal head turns, vertical head turns, pivot turns, around obstacles, and stair climbing. Performance on each item is rated from 0 (severe impairment) to 3 (normal ability) with a maximum total score of 24. 21,22 Participant stepping response was evaluated utilizing lateral postural perturbations applied via waist-pulls, using a computer-controlled motorized puller.17 Participants stood in a comfortable position wearing their normal walking shoes in a quiet comfortable stance with feet approximately shoulder width apart. Foot tracings were taken to ensure that foot placement was consistent between trials. 23 An inelastic adjustable belt, snugly secured around the waist was aligned with the participant’s pelvis so that waist-pulls were applied in the medio-lateral direction. The magnitude of the perturbations ranged from Level 1 through Level 5 (smallest magnitude 1 to largest magnitude 5; displacement 4.5–22.5 cm, velocity: 8.6–50 cm/s, acceleration: 180–900 cm/s2). Testing included a total of sixty pseudorandom arranged perturbations (5 pull intensities x 2 directions x 6 repetitions). Subjects wore a safety harness to prevent them from falling over in case of loss of balance. Participants were instructed to react naturally to the waist-pulls to prevent themselves from falling. For step characteristic analysis and classification as a cross-stepper or medial stepper, we focused on the most challenging perturbation Level 5 (d=13.5 cm; v=45.0 cm.s−1) as it provided a more homogeneous distribution of step types (cross-steppers vs medial steppers) between the groups. Based on their first step responses at level 5 participants were classified as either cross steppers (cross front or back steps) or medial steppers. Those who took ≥51% cross-steps were classified as cross-steppers while those who took ≥51% medial steps were classified as medial steppers. Global first step length was calculated as the maximal foot displacement in the combined anterior/posterior and medial/lateral directions.13 Step length normalized by leg length using the following equation:
Statistical Analyses
All statistical analyses were performed using SPSS Statistics v 22 (IBM software). statistical software. Chi square tests were used to compare the number of fallers and the sex differences between cross-steppers and medial steppers. Independent t-tests were used to compare all other demographics, hip abductor HDL%, IMAT%, torque, and normalized step length between cross and medial steppers. Significance was set at p < 0.05.
RESULTS
Fifty-eight individuals were initially identified for this analysis, 17 were excluded for incomplete CT data or having a BMI > 30 kg/m2, one individual took neither medial nor cross-over steps and was therefore removed from further analysis leaving 40 older adults in the final analyses. Twenty-six individuals were identified as cross-steppers and fourteen were identified as medial steppers. Subject demographics of each group are summarized in Table 1. While those who took an initial cross step tended to be younger, with a higher DGI score this was not a statistically significant difference, BMI’s, history of falls, and sex also did not differ between the groups (Table 1, p=0.10–0.30).
Table 1.
Group Characteristics for Cross Steppers and Medial Steppers
| Cross stepper (N=26) | Non-cross Stepper (N=14) | |
|---|---|---|
| Age (year) | 74 ± 1.3 | 76 ± 2.0 |
| Sex (female/male) | 14/12 | 11/3 |
| BMI (kg/m2) | 26.3 ± 0.6 | 25.2 ± 0.5 |
| Non-Fallers/Fallers | 23/4 | 9/5 |
| Dynamic Gait Index | 21 ± 0.6 | 20 ± 0.9 |
BMI, Body Mass Index; All values are means SEM;
p<0.05 between groups
Stepping characteristics between groups
At perturbation level-5, the cross-stepping group used a cross-step for balance recovery in 92% of trials, while the medial step group used a cross step in 18% of the trials and performed a medial step towards the midline of the body during the majority (71%) of the trials. (Table 2) At this perturbation level, the cross-step group also took a 54% longer first step with fewer total steps for balance recovery than those who mainly utilized medial steps (Table 2, p<0.05).
Table 2.
Stepping Characteristics for Cross Steppers versus Medial Steppers
| Cross Stepper (N=26) | Medial Steppers (N=14) | |
|---|---|---|
| Mean steps for balance recovery (#) | 1.8 ± 0.1 | 2.1 ± 0.2^ |
| Normalized Step Length | 0.75 ± 0.03 | 0.43 ± 0.08^ |
| Percentage of first steps that are cross-steps (%) | 92.7 ± 2.6 | 18.3 ± 6.3^ |
| Percentage of first steps that are medial steps (%) | 4.8 ± 2.3 | 71.1 ± 9.3^ |
All values are means ± SEM;
p<0.002 between groups;
All data provided is for first step responses taken at perturbation level-5
Differences in muscle composition and hip abductor torque between groups
The left and right legs of individuals were initially compared. No difference was found for left versus right leg for muscle composition or hip abductor torques therefore left and right leg were averaged for each individuals. As shown in Figure 2, individuals who took a cross-step demonstrated a trend towards higher levels of HDL in their g.min/med muscles with 3.8% higher HDL (p=0.09) than the medial steppers. A significant difference (p<0.05) was also found for the amount of IMAT within the g.min/med, with the cross steppers having 5.2% lower levels of IMAT (p=0.03) indicating lower levels of IMAT then those who did not use a cross-stepping strategy. No significant differences were found for HDL or IMAT in the g.max between groups. Eight individuals (7 cross-steppers and 1 medial stepper) were missing strength testing for hip abductor strength. In the remaining 32 individuals, differences were found in the hip abductor torques between groups with the cross-stepping group demonstrating 26% higher hip abductor torques (p=0.01) than the medial-stepping group.
Figure 2.
Differences in the percentage (mean ± standard error) of Gluteus maximus and minimus/medius high density lean and IMAT from CT and the hip abductor torque (N.M) as tested with the biodex between groups (cross-steppers vs medial steppers). Significant differences were seen between the groups for both Gluteus min/med IMAT and hip abductor torque. *P<0.05.
DISCUSSION
The hip abductor muscles are important for balance, mobility, and stepping functions. 3,4,6 The purpose of this investigation was to examine the differences in hip abductor strength and composition between older adults who primarily utilize a cross-over step compared with those who use the less demanding medial step for balance recovery in order to elucidate the relationship of hip abductor strength and composition with stepping behavior. The primary new finding of this study was that older adults who primarily use a medial stepping strategy exhibited lower hip abductor torque and had increased IMAT of the hip abductors compared to those who mainly utilized a cross-stepping strategy.
The hip abductor muscles are critical for control motion in the frontal plane and stabilizing the pelvis/trunk to maintain upright posture during demanding balance tasks, especially during single limb stance. Furthermore, sensory receptors involving the M-L hip complex are thought to provide an important proprioceptive contribution around the hip joint24 that can be affected by fatigue25 resulting in impaired medial/lateral postural control.25 Although limb lift-off from the ground for cross-over steps is less demanding than for lateral stepping where active unloading of the passively loaded stepping limb is required, cross steps involve longer single limb stance time, a more complex limb movement trajectory, and precise COM control within a very narrow BSS (foot width) at step landing. Our current findings suggest that impaired hip abductor muscle torque production with increased IMAT may disrupt the ability to safely perform cross-over stepping due to its complex functional and biomechanical requirements.14,15 We found that those who initially used a medial step for balance recovery generally took shorter steps and required almost 50% more steps for balance recovery following a lateral perturbation than those who utilized a cross-step. It is probable that by performing a medial step, older adults with impaired hip abductor musculature were able to take biomechanical advantage of the passive limb unloading allowing for a quicker step that appears to avoid further challenging the impaired hip abductors through a longer more complex cross-over step.17 These findings are in agreement with prior studies demonstrating that older non-fallers utilize crossover-steps the majority of the time to recover from lateral balance perturbations while older fallers more often take medial steps. 17,26 However, the advantage of a more rapid step initiation with medial stepping would be countered by an initially less stable COM-BOS relationship due to the relatively small change in first step length that invariably required further steps in order sustain balance.
The mechanism for impaired hip abductor muscle performance is currently unknown though it is theorized that increased IMAT may play a role. IMAT is known to increase with age and inactivity.27 Further, it has been previously demonstrated that high levels of IMAT may result in impaired neuromuscular activation in older adults.5 Hence, it is conceivable that the observed increase in IMAT in the gluteal muscles may have resulted in impaired neuromuscular control and possible reduction in hip proprioception4 contributing to decreased hip joint stability and a diminished ability to respond to high level balance demands resulting in increased fall risk.3,4,6 Our results also suggest that enhancing performance of the hip abductor muscles might be an important focus for improving balance and reducing fall risk. Future work is needed to identify the mechanisms of impaired hip abductor function and determine the effects of exercise and balance interventions on hip abductor muscle composition, performance, and protective stepping behavior. In this study we also did not examine the differences in the hip adductors between the cross and medial steppers. Given the contribution of the adductors to taking a successful rapid cross-overs step future work should also examine differences in the adductors between those who take a cross over vs a medial step.
Study Limitations
This study was limited by the designed use of a mechanized waist-perturbation to elicit a stepping response. The common key between our stepping response and other losses of balance that may occur in non-laboratory settings, such as a slip/trip, is the change in body orientation relative to the base of support. Both circumstances require the ability to adequately respond to this change to prevent a fall. Thus our results likely represent the protective stepping differences in those who are able to successfully compensate for disturbances of balance vs those who are unable. While we did not account for limb dominance in the study all participants were pulled in both directions (left and right) and the torque from both legs was averaged it is unlikely this impacted our results. We also recognize we had a relatively small sample size and were missing data on approximately 7 individuals for hip abduction. We acknowledge that by limiting the study sample to non-obese relatively healthy older adults our results may not be generalizable to all older adults. It is also probable that our findings are conservative as it is likely that more frail older adults would demonstrate even greater impairments involving the hip abductors. This study may have limited potential for inferring causality between impaired hip abductors and step-recovery due to its cross-sectional nature, but does provide strong impetus to examine the effects of abductor muscle strengthening programs in relation to lateral balance function and fall prevention.
Conclusions
In conclusion, we found that older community dwelling adults who primarily use an initial medial step to recover balance following lateral balance perturbations demonstrate impaired hip abductor musculature and performance. Higher levels of IMAT and decreased hip abductor torque may have contributed to the preference for using medially directed steps to initiate lateral balance recovery at the expense of not executing biomechanically more stable cross-steps. These findings provide new information on the relationship between hip abductor IMAT, torque production, and lateral protective stepping responses. Moreover, the results suggest that rehabilitation assessments and interventions for enhancing balance and decreasing fall risk should target the hip abductor musculature.
Acknowledgments
This work was supported by grants from the National Institute on Aging (NIA) (RO1AG029510), The University of Maryland Claude D. Pepper Older Americans Independence Center grant from NIA (P60-AG12583), National Institute of Aging Training Grant (AG000219), a VA Senior Research Career Scientist Award and the Geriatric, Research, Education, and Clinical Center from Department of Veterans Affairs and Veterans Affairs Medical Center Baltimore. Final peer-reviewed version is subject to NIH Public Access Policy, and will be submitted to PubMed Central.
The authors would like to acknowledge the assistance of the Claude D. Pepper Older American Independence Center, University of Maryland, Baltimore and the assistance of the Geriatric Research Education and Clinical Centers recruitment team. They would also like to acknowledge Michelle Prettyman for her assistance with data collection during the study.
Abbreviations
- BOS
Base of support
- COM
Center of mass
- CT
Computed tomography
- DGI
Dynamic gait index
- G.max
Gluteus Maximus
- G.min/med
Gluteus minimums/medius
- HDL
High density lean
- HU
Hounsfield units
- IMAT
Intramuscular adipose tissue
Footnotes
The authors declare no conflict of interest
This work was presented at the American Physical Therapy Association Combined Sections Meeting, February 2016, Anaheim California.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Saveman BI, Bjornstig U. Unintentional injuries among older adults in northern Sweden--a one-year population-based study. Scand J Caring Sci. 2011;25(1):185–93. doi: 10.1111/j.1471-6712.2010.00810.x. [DOI] [PubMed] [Google Scholar]
- 2.Gaugler JE, Duval S, Anderson KA, Kane RL. Predicting nursing home admission in the U.S: a meta-analysis. BMC Geriatr. 2007:713. doi: 10.1186/1471-2318-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Inacio M, Ryan AS, Bair WN, Prettyman M, Beamer BA, Rogers MW. Gluteal muscle composition differentiates fallers from non-fallers in community dwelling older adults. BMC Geriatr. 2014:1437. doi: 10.1186/1471-2318-14-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kiyoshige Y, Watanabe E. Fatty degeneration of gluteus minimus muscle as a predictor of falls. Arch Gerontol Geriatr. 2015;60(1):59–61. doi: 10.1016/j.archger.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 5.Yoshida Y, Marcus RL, Lastayo PC. Intramuscular adipose tissue and central activation in older adults. Muscle Nerve. 2012;46(5):813–6. doi: 10.1002/mus.23506. [DOI] [PubMed] [Google Scholar]
- 6.Addison O, Young P, Inacio M, et al. Hip but not thigh intramuscular adipose tissue is associated with poor balance and increased temporal gait variability in older adults. Curr Aging Sci. 2014;7(2):137–43. doi: 10.2174/1874609807666140706150924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Addison O, Drummond MJ, LaStayo PC, et al. Intramuscular fat and inflammation differ in older adults: the impact of frailty and inactivity. J Nutr Health Aging. 2014;18(5):532–8. doi: 10.1007/s12603-014-0019-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bittel DC, Bittel AJ, Tuttle LJ, et al. Adipose tissue content, muscle performance and physical function in obese adults with type 2 diabetes mellitus and peripheral neuropathy. J Diabetes Complications. 2015;29(2):250–7. doi: 10.1016/j.jdiacomp.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Delmonico MJ, Harris TB, Visser M, et al. Longitudinal study of muscle strength, quality, and adipose tissue infiltration. Am J Clin Nutr. 2009;90(6):1579–85. doi: 10.3945/ajcn.2009.28047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hilton TN, Tuttle LJ, Bohnert KL, Mueller MJ, Sinacore DR. Excessive adipose tissue infiltration in skeletal muscle in individuals with obesity, diabetes mellitus, and peripheral neuropathy: association with performance and function. Phys Ther. 2008;88(11):1336–44. doi: 10.2522/ptj.20080079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tuttle LJ, Sinacore DR, Cade WT, Mueller MJ. Lower physical activity is associated with higher intermuscular adipose tissue in people with type 2 diabetes and peripheral neuropathy. Phys Ther. 2011;91(6):923–30. doi: 10.2522/ptj.20100329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maki BE, Holliday PJ, Topper AK. A prospective study of postural balance and risk of falling in an ambulatory and independent elderly population. J Gerontol. 1994;49(2):M72–84. doi: 10.1093/geronj/49.2.m72. [DOI] [PubMed] [Google Scholar]
- 13.Mille ML, Johnson-Hilliard M, Martinez KM, Zhang Y, Edwards BJ, Rogers MW. One Step, Two Steps, Three Steps More … Directional Vulnerability to Falls in Community-Dwelling Older People. J Gerontol A Biol Sci Med Sci. 2013 doi: 10.1093/gerona/glt062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maki BE, Edmondstone MA, McIlroy WE. Age-related differences in laterally directed compensatory stepping behavior. J Gerontol A Biol Sci Med Sci. 2000;55(5):M270–7. doi: 10.1093/gerona/55.5.m270. [DOI] [PubMed] [Google Scholar]
- 15.Maki BE, McIlroy WE, Perry SD. Influence of lateral destabilization on compensatory stepping responses. J Biomech. 1996;29(3):343–53. doi: 10.1016/0021-9290(95)00053-4. [DOI] [PubMed] [Google Scholar]
- 16.Mille ML, Johnson ME, Martinez KM, Rogers MW. Age-dependent differences in lateral balance recovery through protective stepping. Clin Biomech (Bristol, Avon) 2005;20(6):607–16. doi: 10.1016/j.clinbiomech.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 17.Bair WN, Prettyman M, Beamer BA, Rogers MW. Kinematic and Behavioral Analyses of Protective Stepping Strategies and Risk for Falls among Community Living Older Adults. 2016 doi: 10.1016/j.clinbiomech.2016.04.015. Under Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Falls. 2012 at http://www.who.int/violence_injury_prevention/other_injury/falls/en/index.htm.
- 19.Ryan AS, Buscemi A, Forrester L, Hafer-Macko CE, Ivey FM. Atrophy and intramuscular fat in specific muscles of the thigh: associated weakness and hyperinsulinemia in stroke survivors. Neurorehabilitation and neural repair. 2011;25(9):865–72. doi: 10.1177/1545968311408920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hilliard MJ, Martinez KM, Janssen I, et al. Lateral balance factors predict future falls in community-living older adults. Arch Phys Med Rehabil. 2008;89(9):1708–13. doi: 10.1016/j.apmr.2008.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bogle Thorbahn LD, Newton RA. Use of the Berg Balance Test to predict falls in elderly persons. Physical therapy. 1996;76(6):576–83. doi: 10.1093/ptj/76.6.576. discussion 84–5. [DOI] [PubMed] [Google Scholar]
- 22.Shumway-Cook A, Ciol MA, Hoffman J, Dudgeon BJ, Yorkston K, Chan L. Falls in the Medicare population: incidence, associated factors, and impact on health care. Phys Ther. 2009;89(4):324–32. doi: 10.2522/ptj.20070107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pidcoe PE, Rogers MW. A closed-loop stepper motor waist-pull system for inducing protective stepping in humans. J Biomech. 1998;31(4):377–81. doi: 10.1016/s0021-9290(98)00017-7. [DOI] [PubMed] [Google Scholar]
- 24.Retchford TH, Crossley KM, Grimaldi A, Kemp JL, Cowan SM. Can local muscles augment stability in the hip? A narrative literature review. J Musculoskelet Neuronal Interact. 2013;13(1):1–12. [PubMed] [Google Scholar]
- 25.Arvin M, Hoozemans MJ, Burger BJ, et al. Effects of hip abductor muscle fatigue on gait control and hip position sense in healthy older adults. Gait Posture. 2015;42(4):545–9. doi: 10.1016/j.gaitpost.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 26.Sturnieks DL, Menant J, Vanrenterghem J, Delbaere K, Fitzpatrick RC, Lord SR. Sensorimotor and neuropsychological correlates of force perturbations that induce stepping in older adults. Gait Posture. 2012;36(3):356–60. doi: 10.1016/j.gaitpost.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 27.Addison O, Marcus RL, Lastayo PC, Ryan AS. Intermuscular fat: a review of the consequences and causes. Int J Endocrinol. 2014 doi: 10.1155/2014/309570. 2014309570. [DOI] [PMC free article] [PubMed] [Google Scholar]