Abstract
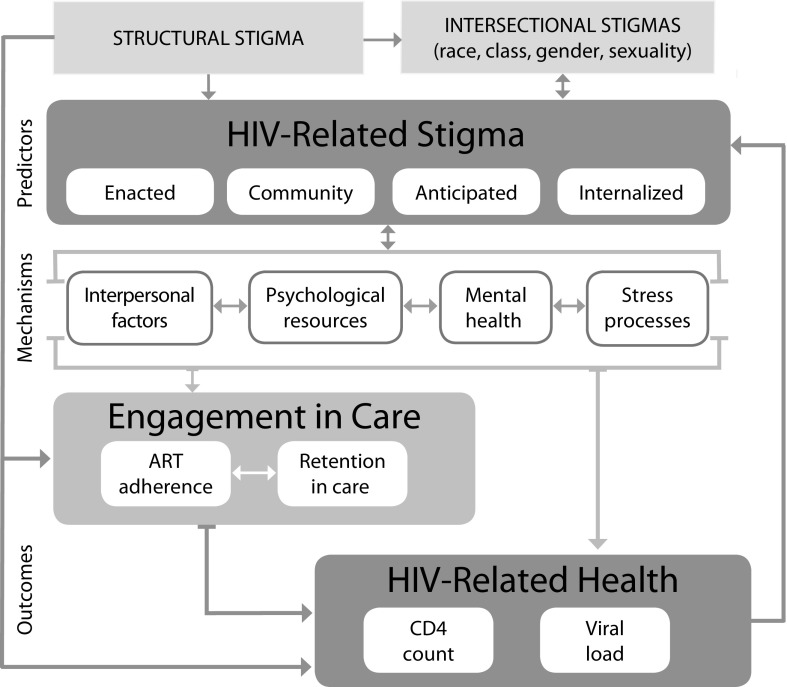
We present a conceptual framework that highlights how unique dimensions of individual-level HIV-related stigma (perceived community stigma, experienced stigma, internalized stigma, and anticipated stigma) might differently affect the health of those living with HIV.
HIV-related stigma is recognized as a barrier to both HIV prevention and engagement in HIV care, but little is known about the mechanisms through which stigma leads to worse health behaviors or outcomes. Our conceptual framework posits that, in the context of intersectional and structural stigmas, individual-level dimensions of HIV-related stigma operate through interpersonal factors, mental health, psychological resources, and biological stress pathways.
A conceptual framework that encompasses recent advances in stigma science can inform future research and interventions aiming to address stigma as a driver of HIV-related health.
Adherence to HIV care and treatment recommendations is essential for ensuring health, longevity, and a suppressed viral load among people living with HIV (PLWH). Yet, in the United States, for example, fewer than two thirds of PLWH are virally suppressed,1 suggesting that too few PLWH in the United States have access to the benefits of recent advances in viral control and transmission prevention. One major barrier to adherence to care and treatment is HIV-related stigma. Stigma is a pervasive social process: individuals with socially undesirable attributes or identities are seen as having lower social value than are others and as a consequence face prejudice and discrimination. The attribute that is the target of stigmatization may be a particular racial or ethnic background, poverty, a chronic disease, sexual orientation, or any other characteristic that is interpreted in society as a sign of the flawed or inferior character of the person.
A growing body of literature suggests that fears and experiences of HIV-related stigma not only affect the quality of life and mental health of PLWH but are also related to poor engagement in HIV care and treatment. Meta-analyses of research suggest that persons who perceive high levels of HIV-related stigma have lower access to medical care, poorer antiretroviral therapy (ART) adherence, and lower utilization of HIV care.2,3
However, there are notable gaps in the literature, with little theoretical work highlighting the role of specific dimensions of HIV-related stigma in shaping engagement in HIV care and health outcomes. Furthermore, there is no existing model to frame the psychosocial and biological mechanisms that explain how these dimensions of stigma affect HIV-related health at an individual level. Understanding mechanisms linking stigma to health behaviors and outcomes has important implications for future intervention development, policy, and service provision.
We propose a conceptual framework for individual-level dimensions of stigma and potential individual and interpersonal mechanisms explaining how stigma affects HIV-related health at an individual level. We draw on the literature, general stigma theories developed in areas other than HIV, and recent biopsychosocial evidence to understand ties between stigma, health behaviors, and HIV-related health outcomes.
CONCEPTUAL FRAMEWORK
The minority stress model4 was developed to understand the effects of minority sexual orientations on mental health. The model extends theories of stress and adaptation to explain the higher prevalence of mental disorders experienced by lesbian, gay, and bisexual people than by heterosexual individuals. However, the model may be applied to other minority statuses and identities (e.g., race/ethnicity, gender, HIV serostatus). The main tenet of the minority stress model is that individuals who are socially categorized in marginalized groups experience more social stress than do their counterparts because of their minority social position and that this has implications for their health.
Structural and Intersectional Stigma
Structural stigma at the macro level refers to attitudes in societies, practices, structures, services, and laws that work to the disadvantage of minority groups.5 Structural stigma can work in the absence of individual discrimination (e.g., via inequitable social policies, resource allocation, and other unequal distribution of opportunity). Structural stigma may directly affect health and operate through micro- (or individual-) level dimensions of stigma to affect health. Although macrolevel stigmas are fundamental to stigma-stress-health processes, we focus on microlevel dimensions of HIV-related stigma and their effects, a focus that is well supported by research and forms the basis for the majority of existing intervention strategies.
The intersectionality framework emphasizes the importance of understanding how multiple social statuses or identities intersect at the micro level (e.g., HIV status, race, gender, sexual orientation, socioeconomic status) and at the macro level (e.g., HIV stigma, racism, sexism, heterosexism, classism) to produce health inequalities.6 Similar to minority stress theory, the intersectional approach acknowledges the contextual and population-specific nature of individual and social experiences: experiences for one population group (e.g., Black lesbian women in the United States) may be distinct from those of another (e.g., lesbian women in South Africa), even though they share some intersecting categories of difference. Shaped by this framework, the concept of intersectional stigma has been applied in the HIV literature to refer to the tendency for PLWH to simultaneously experience stigma and discrimination because of HIV and other aspects of their identities, such as their race, economic situation, or sexual orientation.6
It is important to note that intersectional stigma is conceptualized as operating at an intermediate meso (or community and social networks) level in addition to the macro and micro levels. Stigma processes at the meso level reflect community and social norms, which may be population and location dependent (i.e., cultural beliefs, history, and practices may be reflected in different stigma experiences in specific population groups by locale). For example, a literature review comparing HIV status disclosure patterns across contexts suggests that frequencies of disclosure tend to be higher in higher-income countries (where HIV incidence and prevalence are generally lower7) than in low- and middle-income countries.8 This finding is contextualized by research reports that involuntary disclosure is common in the latter settings.
Relatedly, nondisclosure (a manifestation of stigma) is prompted by anticipation of stigma. More research is needed to elucidate contextual variables that play a role in shaping the effects of HIV-related stigma. Intersectional stigma, including at the meso level, is integral to stigma theory and is thus included in our conceptual model (Figure 1). However, we maintain our primary focus on elucidating how microlevel dimensions of HIV-related stigma affect health.
FIGURE 1—
Conceptual Framework for HIV-Related Stigma, Engagement in Care, and Health Outcomes
Note. ART = antiretroviral therapy.
Individual-Level HIV-Related Stigma
The minority stress model posits that social stress processes range from distal to proximal to the person in the following order: (1) external stressful events such as acts of discrimination by others, (2) expectations of such events (anticipation), (3) internalization of negative attitudes in the community, and (4) concealment of one’s sexual orientation.4 The model also acknowledges that subjective perception of stigmatizing attitudes in the community is an important factor.
Adapting the minority stress model to HIV-related stigma, and integrating it with the literature in HIV research, our conceptual model posits numerous HIV-related dimensions operating at the individual (micro) level, each of which has the potential to influence HIV-related health behaviors and the health of PLWH (Figure 1): (1) enacted or experienced HIV stigma (actual experiences of discrimination, devaluation, and prejudice by others because of one’s HIV-positive status), (2) perceived HIV stigma in the community (an individual’s perceptions of the existence and severity of stigmatizing attitudes in the community), (3) anticipated HIV stigma (PLWH’s expectations that others will treat them negatively in future situations because of their HIV status), and (4) internalized HIV stigma (PLWH’s endorsement and acceptance of negative assumptions about their character because they have HIV and experience self-deprecating feelings and cognitions such as shame, self-blame, and embarrassment). We conceptualize concealment of one’s HIV status as one of the downstream effects of these dimensions of stigma.
These individual-level dimensions of HIV stigma appear to be differentially associated with health behaviors and outcomes. For example, internalized stigma appears to uniquely predict outcomes related to affective and cognitive functioning (e.g., depression, helplessness, low self-esteem), even when controlling for the effects of other stigma dimensions.9,10 This finding is coherent theoretically, because PLWH who internalize social stigma and accept their HIV status as an indication of their worth as a person may experience changes in affect and self-referencing cognitions.
Conversely, anticipated stigma uniquely predicts health care behaviors, such as adherence to medication.10 This occurs partly because PLWH who anticipate stigmatizing attitudes and behaviors from others may be less likely to take actions (like visiting an HIV clinic) that they fear may increase the likelihood of such attitudes and behaviors from others. Several studies also suggest that physical health indicators (e.g., viral load, CD4 counts) are uniquely predicted by experienced stigma and that this effect is not mediated by adherence to treatment recommendations, perhaps because the stress of experienced stigma has direct negative effects on health.9,11
Sources of Stigma
PLWH may anticipate and experience stigma from different sources, such as friends and family, sexual partners, co-workers, strangers, health care workers, and institutions. Evidence has been accumulating that the source of stigma makes a difference. For example, HIV-related stigma from male partners and other family members may be more harmful for the mental and physical health of pregnant women living with HIV than is stigma from other sources.12
Anticipation and experience of stigma specifically from health care workers seem to be particularly detrimental to treatment outcomes for PLWH, leading to outcomes such as lack of physician trust, low quality of life, and poor ART adherence.11
Mechanisms for Effects on Health
According to the fundamental cause theory of stigma,13 individuals living with stigmatized identities have worse health outcomes because of several mediating mechanisms: (1) reduced availability of resources (such as power, social status, social connections, and financial resources), (2) social isolation and lack of social support, (3) maladaptive psychological and behavioral responses (maladaptive coping strategies such as avoidance and drinking), and (4) physiological stress responses that negatively affect health in the long term. We adapted this formulation to research on HIV-related stigma, and our conceptual framework identifies multiple mechanisms that may help to explain the negative effects of HIV-related stigma dimensions and their sequelae on adherence to HIV treatment recommendations: interpersonal factors, worsened mental health, compromised psychological resources, and stress and biological pathways (Figure 1).
Poor engagement in HIV care, in turn, may alter HIV clinical outcomes. That is, stigma dimensions may negatively affect HIV clinical outcomes through either behavioral or nonbehavioral pathways, such as physiological stress processes. We have not included financial resources as an individual-level mechanism in our model because (1) structural stigma may play a major and direct role at the macro level in depleting financial resources for PLWH, and (2) empirical evidence for this mechanism at an individual level is scarce at this time.
Interpersonal factors.
Interpersonal factors include the social dynamics of stigma that influence HIV-related health behaviors and health outcomes. Disclosure is such an interpersonal factor. PLWH who have higher levels of anticipated stigma or perceived community stigma may not disclose their HIV status to others to avoid negative social judgment and perceived or actual discrimination from others.8 Lack of disclosure, in turn, may have a negative effect on engagement in HIV care if it limits ability to stick with clinic visits or medication in an effort to keep such behaviors secret from others. Conversely, unwanted HIV status disclosure may result in experiences of stigma and discrimination, which could impede access to care and adherence.
Lack of social support and loneliness can be caused by multiple forms of HIV-related stigma. Experienced, perceived community, internalized, and anticipated stigma may all lead to self-imposed social isolation.14 They can also lead to not disclosing serostatus, which—in a cyclical manner—limits the number of people that PLWH can rely on for instrumental and emotional support. The intentional choice to protect oneself from anticipated stigma can lead to fewer sources of social support, thus creating fewer opportunities for nonstigmatizing, supportive relationships. In a longitudinal study in Uganda, internalized stigma predicted decreased levels of perceived social support.15 Loneliness or a lack of social support can hinder visit and ART adherence, either directly or, as a recent study found, through higher levels of depression.14
Mental health.
The mental health sequelae of stigma have received increased attention in the literature, partly because of the known detrimental effects of mental illness on HIV-related health outcomes and engagement in care behaviors. Depression is a mental health condition that has been consistently linked to both experienced and internalized HIV-related stigma; depressive symptoms, in turn, are associated with nonadherence to HIV treatment recommendations14 and may also have direct negative effects on immunological status.16 Studies have found support for the mediating effect of depression in the internalized stigma–ART adherence association.14
HIV-related stigma may also be associated with increased levels of anxiety,2 which in turn is associated with HIV medication nonadherence17 and may also have direct immunological effects.18 Social anxiety can be an outcome of anticipated, perceived community, and internalized stigma. For example, a recent study found that the effect of HIV-related internalized stigma on medication adherence is mediated by attachment-related anxiety (characterized by fears of abandonment by relationship partners) and by concerns about being seen by others while taking HIV medication.19 However, the literature on the role of anxiety in HIV-related outcomes is in its infancy, suggesting an important next step in stigma research.
Psychological resources.
Psychological resources are the tools, skills, and personal identities that individuals use to cope with stressful life events. Treatment self-efficacy tends to be lower among persons who have high levels of internalized stigma.20 Internalized stigma may cause PLWH to perceive themselves as inferior or less capable in dealing with issues related to their treatment, and lowered self-efficacy related to HIV treatment can lead to lower ART adherence.20
A related, but analytically distinct, concept is resilience, often viewed as adaptive coping in response to stress. Among PLWH, resilience is associated with better ART adherence and lower likelihood of having a detectable viral load.21 It is plausible, but as yet untested, that resilience is a mediator or moderator (if it buffers the negative health effects of stigma on HIV-related health) of the stigma–adherence association.
Health care empowerment is the extent to which PLWH feel involved in decision-making about their health care and are able to deal with uncertainties in treatment outcomes.22 Although yet to be tested empirically, it is theoretically plausible that PLWH who experience stigma would tend to feel less empowered about their health care, leading to a lack of adherence to treatment recommendations. This dynamic may be pronounced among PLWH experiencing stigma and discrimination from health care workers.
Coping skills are another psychological resource that stigma may affect. In particular, stigma may result in maladaptive coping behaviors that adversely affect HIV-related health behaviors and outcomes. Avoidant coping occurs when PLWH avoid behaviors that would remind them about HIV, for example, not taking medication or skipping appointments as a means of lessening the cognitive or emotional reminder of one’s HIV status. Stigma may be related to concomitant anxiety and depression via unhealthy coping mechanisms of behavioral disengagement.23 Longitudinal research suggests that denial and avoidant coping predict clinical outcomes of HIV disease progression.24
Substance abuse is a particularly common method of avoidance coping, because it offers distraction from distressing thoughts associated with stigma. Substance use, in turn, worsens engagement in HIV care and treatment.25 Substance use can also be viewed as a mechanism of worsening mental health.
Stress and biological processes.
There is accumulating evidence that stressful experiences—including trauma, violence, poverty, and discrimination—may produce stress responses in the body. Studies have found a significant link between perceived discrimination (i.e., experienced stigma) and heightened stress responses.26 Stressful life circumstances may work through immunological and inflammatory pathways to result in chronic activation of stress-responsive biological systems.27 Chronic stress may also affect mental health (depression, anxiety), health behaviors (medication nonadherence, missed clinic visits, treatment interruptions), and immunological health (increased inflammation and immune activation).27
Pre-ART era studies suggested that the lack of disclosure and rejection sensitivity—often results of fears of stigma—directly and adversely affect clinical outcomes such as disease progression, CD4 counts, and viral loads.28 HIV-related stigma, then, may lead to chronic stress that worsens clinical outcomes both through biological mechanisms and through the behavioral pathways of reduced adherence to treatment recommendations. HIV-related stigma has also been associated with posttraumatic stress disorder.29 Trauma, in turn, can pose a direct physiological effect on immune activation and markers of aging, such as telomere shortening.30 More studies are needed to elucidate the multifaceted role of stigma in these biological processes.
Stigma dimensions and mechanisms.
Theoretically, it is plausible that different dimensions of stigma influence each other. A recent experience sampling study found that when PLWH experience discrimination in everyday life, they tend to report higher levels of internalized stigma (using within-person analyses), and this association is stronger for PLWH who perceive higher levels of stigma in the community.31 PLWH who perceive higher levels of stigma in the community are also more likely to experience internalized stigma.10 Those with higher levels of internalized stigma, in turn, were found to be more likely to anticipate stigmatizing attitudes from others. There was also evidence for a serial mediational model when predicting medication adherence: perceived community stigma predicted internalized stigma, which predicted anticipated stigma, which in turn predicted lower medication adherence. These complexities suggest the need for analytical and measurement approaches that can assess mediation across stigma dimensions and pathways and over time.
CONCLUSIONS
Although HIV-related stigma has been recognized as a reason for poor engagement in HIV care, less is known about the mechanisms through which stigma leads to negative health outcomes for individuals living with HIV. We posit that unique dimensions of stigma have differing pathways to and effects on health outcomes for individual PLWH and that stigma operates through interpersonal factors, mental health, compromised psychological resources, and biological stress pathways to adversely affect HIV-related health outcomes.
Stigma can worsen HIV-related health both directly through physiology and indirectly through engagement in care behaviors. Our conceptual framework posits that stigma at the structural level may also affect health outcomes for PLWH—either directly (e.g., if better qualified health professionals choose to specialize in diseases that are less stigmatized or to work in affluent neighborhood hospitals or offices where HIV is less common) or through individual-level dimensions, such as internalized stigma, and individual-level mechanisms, such as depression. This framework may inform future research and interventions aiming to address stigma as a driver of HIV-related health.
The Next Generation of Stigma Research
Although the literature provides evidence for the effects of HIV-related stigma on health outcomes for PLWH, most studies in this area have been cross-sectional. An important next step is to use longitudinal designs to provide stronger evidence for the causal effects and pathways of stigma. Another important research gap is to design stronger measurement strategies. Experience sampling methods may be used to assess current experiences and feelings of stigma in PLWH.31 Experience sampling methods ask participants to pause at certain times during daily life and make notes of their experience in real time; these methods offer strength over typical methods that rely on long-term recall and global assessments. To measure chronic stress, cortisol levels in hair provide an assessment of stress levels over the past 3 months.32 Another way to assess the biological stigma pathway is to conduct multiplexed assays from blood serum to simultaneously measure multiple biomarkers of inflammation and immune activation.33
An important level of complexity is introduced by intersectional stigma stemming from multiple social statuses or identities (e.g., HIV status, race, gender, sexual orientation, socioeconomic status), which encompasses stigma and discrimination at the macro, meso, and micro levels. Intersectional approaches also highlight protective factors, such as social support and adaptive coping strategies, that can emerge at the intersection of multiple identities.34 However, there is little understanding of how stigma associated with multiple identities affects adherence to HIV treatment recommendations and clinical outcomes. This knowledge could help tailor future interventions for groups at high risk for multiple stigmas and will have relevance beyond HIV, because intersectional stigma may amplify negative effects for a variety of health issues.35
The effects of structural stigma may be observed and examined at an individual level. However, it may also be examined at a population level through community-wide surveys. Furthermore, structural stigma may reflect an objective assessment of stigma in the community, whereas perceived community stigma at an individual level reflects the subjective interpretation of this objective reality. It will be important for future research to examine the association between objective and subjective measures of community stigma and how objective stigma leads to perceived community stigma, which in turn leads to internalized or anticipated stigma, and whether these processes are more likely to happen with some PLWH than with others.
HIV Prevention Interventions and Stigma
PLWH with suppressed viral loads are much less likely to transmit HIV to others, which is referred to as “treatment as prevention.” Another recent biomedical advance is the use of preexposure prophylaxis, which reduces the likelihood of HIV acquisition for individuals at risk.
The success of both treatment as prevention and preexposure prophylaxis may be affected by HIV-related stigma, and there may be unique manifestations of stigma related to these interventions. Both treatment as prevention and preexposure prophylaxis also have the potential to curb HIV incidence at the population level, and they may reduce stigma related to HIV and its effects—at both the macro and the micro levels.
Intervention and Policy Implications
In line with our proposed framework, interventions and policies should be developed to focus on specific dimensions of HIV-related stigma and particular mechanisms for their effects on ill health. To date, most HIV stigma interventions have focused only on broad cognitive factors underpinning stigma in individual PLWH, such as knowledge or fear.36 This shortcoming means that stigma interventions to date have been imprecise in terms of how they intend to shift the aspects of stigma that are harmful to health.
Understanding the causal mechanisms of stigma and HIV outcomes can refine the types of skills and behaviors included in future interventions. To address interpersonal factors such as low social support, social isolation, or interpersonal dynamics, interventions should focus on strategies to help with safe HIV disclosure and building social support. Interpersonal interventions also need to be targeted at the community level, because individual-level interventions are unlikely to comprehensively alter the stigmatization process.36
In light of the recent advances in understanding intersectional stigma, group- and community-based interventions could focus on multiple stigmas that high-risk communities face. Preliminary research has suggested that successful community interventions might include scaling up antiretroviral treatment (to ensure widespread health gains)37 and increasing access to livelihoods (to renew a sense of being productive, active members of a community).38
At the individual level, interventions can address perceived community stigma, internalized stigma, and anticipated stigma. Another intervention strategy may be to block the path from stigma to a mediating mechanism or to block the path from the mediating mechanism to nonadherence. That is, even if stigma does not change, a successful intervention might reduce the effect of stigma on adherence, which would promote health. As our framework highlights, such interventions can focus on building coping, resilience, empowerment, and self-efficacy skills. To address mental health factors, interventions should be linked with mental health services to address depression, anxiety, trauma, and substance abuse.
To influence biological pathways such as chronic stress processes, interventions could include mindfulness or stress-reduction programs, trauma-based therapies, or pharmacological treatment. Interventions at the systems level addressing structural stigma are also possible (i.e., policy interventions can prevent or minimize the processes by which stigma creates or reinforces negative social evaluation of minority groups) but potentially more difficult to implement.
The National HIV/AIDS Strategy for the United States puts forth the vision that “every person diagnosed with HIV deserves immediate access to treatment and care that is nonstigmatizing, competent, and responsive to the needs of the diverse populations impacted by HIV.”39(p3) It is high time that policies and programs strive to make such equitable and fair treatment of PLWH a reality.
By targeting appropriate dimensions and mechanisms of stigma, future policy and programs can better develop approaches that reduce stigma and ensure healthy lives for those living with HIV. In addition, the dimensions and mechanisms we posit in the context of HIV-related stigma may play important roles in other stigmatized health conditions, such as diabetes and asthma, and thus interventions addressing stigma may play an important role in improving health across a wide spectrum of population groups.40
ACKNOWLEDGMENTS
This study was funded by Women’s Interagency HIV Study (WIHS), National Institute of Mental Health ([NIH] substudy grants R01MH095683 and R01MH104114). The WIHS is funded primarily by the National Institute of Allergy and Infectious Diseases (NIAID), with additional cofunding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), the National Cancer Institute (NCI), the National Institute on Drug Abuse (NIDA), and the National Institute on Mental Health. Targeted supplemental funding for specific projects is also provided by the National Institute of Dental and Craniofacial Research, the National Institute on Alcohol Abuse and Alcoholism, the National Institute on Deafness and Other Communication Disorders, and the NIH Office of Research on Women’s Health. WIHS data collection is also supported by University of California, San Francisco Clinical and Translational Science Award ([CTSA] award UL1-TR000004) and Atlanta CTSA (award UL1-TR000454). This research was also supported by the University of Alabama at Birmingham (UAB) Center for AIDS Research, an NIH-funded program (grant P30 AI027767) that was made possible by the following institutes: NIAID, NCI, NICHD, NHLBI, NIDA, NIA, NIDDK, NIGMS, and OAR. WSR is supported by the Agency for Healthcare Research and Quality (institutional training grant T32HS013852).
WIHS comprised the following: (principal investigators): UAB-University of Mississippi WIHS (Michael Saag, Mirjam-Colette Kempf, and Deborah Konkle-Parker; grant U01-AI-103401); Atlanta WIHS (Ighovwerha Ofotokun and Gina Wingood; grant U01-AI-103408); Bronx WIHS (Kathryn Anastos; grant U01-AI-035004); Brooklyn WIHS (Howard Minkoff and Deborah Gustafson; grant U01-AI-031834); Chicago WIHS (Mardge Cohen; grant U01-AI-034993); Metropolitan Washington WIHS (Mary Young; grant U01-AI-034994); Miami WIHS (Margaret Fischl and Lisa Metsch; grant U01-AI-103397); University of North Carolina WIHS (Adaora Adimora; grant U01-AI-103390); Connie Wofsy Women’s HIV Study, Northern California (Ruth Greenblatt, Bradley Aouizerat, and Phyllis Tien; grant U01-AI-034989); WIHS Data Management and Analysis Center (Stephen Gange and Elizabeth Golub; grant U01-AI-042590); Southern California WIHS (Alexandra Levine and Marek Nowicki; grant U01-HD-032632; WIHS I–WIHS IV).
Note. The contents of this publication are solely the responsibility of the authors and do not represent the official views of the NIH.
HUMAN PARTICIPANT PROTECTION
Institutional review board approval was not needed for this article, because it did not involve the use of primary or secondary data.
REFERENCES
- 1.Crepaz N, Tang T, Marks G, Mugavero MJ, Espinoza L, Hall HI. Durable viral suppression among HIV-diagnosed persons—United States, 2012–2013. Paper presented at Conference on Retroviruses and Opportunistic Infections (CROI) February 22–25, 2016; Boston, MA. [Google Scholar]
- 2.Rueda S, Mitra S, Chen S et al. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: a series of meta-analyses. BMJ Open. 2016;6(7):e011453. doi: 10.1136/bmjopen-2016-011453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katz IT, Ryu AE, Onuegbu AG et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. 2013;16(3) suppl 2:18640. doi: 10.7448/IAS.16.3.18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. PsycholBull. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hatzenbuehler ML, Link BG. Introduction to the special issue on structural stigma and health. Soc Sci Med. 2014;103:1–6. doi: 10.1016/j.socscimed.2013.12.017. [DOI] [PubMed] [Google Scholar]
- 6.Logie CH, James L, Tharao W, Loutfy MR. HIV, gender, race, sexual orientation, and sex work: a qualitative study of intersectional stigma experienced by HIV-positive women in Ontario, Canada. PLoS Med. 2011;8(11):e1001124. doi: 10.1371/journal.pmed.1001124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang H, Wolock TM, Carter A. Estimates of global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2015: the Global Burden of Disease Study 2015. Lancet HIV. 2016;3(8):e361–e387. doi: 10.1016/S2352-3018(16)30087-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Obermeyer CM, Baijal P, Pegurri E. Facilitating HIV disclosure across diverse settings: a review. Am J Public Health. 2011;101(6):1011–1023. doi: 10.2105/AJPH.2010.300102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. 2013;17(5):1785–1795. doi: 10.1007/s10461-013-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Turan B, Budhwani H, Fazeli PL et al. How does stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV stigma in the effects of perceived community stigma on health and psychosocial outcomes. AIDS Behav. 2017;21(1):283–291. doi: 10.1007/s10461-016-1451-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Turan B, Lanzi R, Turan JM, Smith W. HIV-related stigma in healthcare settings and health outcomes among people living with HIV. Paper presented at the 11th International Conference on HIV Treatment and Prevention Adherence. May 9–11, 2016; Fort Lauderdale, FL. [Google Scholar]
- 12.Turan JM, Nyblade L. HIV-related stigma as a barrier to achievement of global PMTCT and maternal health goals: a review of the evidence. AIDS Behav. 2013;17(7):2528–2539. doi: 10.1007/s10461-013-0446-8. [DOI] [PubMed] [Google Scholar]
- 13.Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103(5):813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Turan B, Smith W, Cohen MH et al. Mechanisms for the negative effects of internalized HIV-related stigma on antiretroviral therapy adherence in women: the mediating roles of social isolation and depression. J Acquir Immune Defic Syndr. 2016;72(2):198–205. doi: 10.1097/QAI.0000000000000948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tsai AC, Bangsberg DR, Emenyonu N, Senkungu JK, Martin JN, Weiser SD. The social context of food insecurity among persons living with HIV/AIDS in rural Uganda. Soc Sci Med. 2011;73(12):1717–1724. doi: 10.1016/j.socscimed.2011.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leserman J. Role of depression, stress, and trauma in HIV disease progression. Psychosom Med. 2008;70(5):539–545. doi: 10.1097/PSY.0b013e3181777a5f. [DOI] [PubMed] [Google Scholar]
- 17.Nilsson Schönnesson L, Williams ML, Ross MW, Bratt G, Keel B. Factors associated with suboptimal antiretroviral therapy adherence to dose, schedule, and dietary instructions. AIDS Behav. 2007;11(2):175–183. doi: 10.1007/s10461-006-9160-0. [DOI] [PubMed] [Google Scholar]
- 18.McGuire JL, Kempen JH, Localio R, Ellenberg JH, Douglas SD. Immune markers predictive of neuropsychiatric symptoms in HIV-infected youth. Clin Vaccine Immunol. 2015;22(1):27–36. doi: 10.1128/CVI.00463-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blake Helms C, Turan JM, Atkins G et al. Interpersonal mechanisms contributing to the association between HIV-related internalized stigma and medication adherence. AIDS Behav. 2017;21(1):238–247. doi: 10.1007/s10461-016-1320-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Seghatol-Eslami VC, Dark HE, Raper JL, Mugavero MJ, Turan JM, Turan B. Brief report: interpersonal and intrapersonal factors as parallel independent mediators in the association between internalized HIV stigma and ART adherence. J Acquir Immune Defic Syndr. 2017;74(1):e18–e22. doi: 10.1097/QAI.0000000000001177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dale S, Cohen M, Weber K, Cruise R, Kelso G, Brody L. Abuse and resilience in relation to HAART medication adherence and HIV viral load among women with HIV in the United States. AIDS Patient Care STDS. 2014;28(3):136–143. doi: 10.1089/apc.2013.0329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnson MO, Sevelius JM, Dilworth SE, Saberi P, Neilands TB. Preliminary support for the construct of health care empowerment in the context of treatment for human immunodeficiency virus. Patient Prefer Adherence. 2012;6:395–404. doi: 10.2147/PPA.S30040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Varni SE, Miller CT, McCuin T, Solomon SE. Disengagement and engagement coping with HIV/AIDS stigma and psychological well-being of people with HIV/AIDS. J Soc Clin Psychol. 2012;31(2):123–150. doi: 10.1521/jscp.2012.31.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ironson G, Balbin E, Stuetzle R et al. Dispositional optimism and the mechanisms by which it predicts slower disease progression in HIV: proactive behavior, avoidant coping, and depression. Int J Behav Med. 2005;12(2):86–97. doi: 10.1207/s15327558ijbm1202_6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gonzalez A, Mimiaga MJ, Israel J, Andres Bedoya C, Safren SA. Substance use predictors of poor medication adherence: the role of substance use coping among HIV-infected patients in opioid dependence treatment. AIDS Behav. 2013;17(1):168–173. doi: 10.1007/s10461-012-0319-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135(4):531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. JAMA. 2007;298(14):1685–1687. doi: 10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- 28.Kemeny ME. Psychobiological responses to social threat: evolution of a psychological model in psychoneuroimmunology. Brain Behav Immun. 2009;23(1):1–9. doi: 10.1016/j.bbi.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 29.Katz S, Nevid JS. Risk factors associated with posttraumatic stress disorder symptomatology in HIV-infected women. AIDS Patient Care STDS. 2005;19(2):110–120. doi: 10.1089/apc.2005.19.110. [DOI] [PubMed] [Google Scholar]
- 30.O’Donovan A, Epel E, Lin J et al. Childhood trauma associated with short leukocyte telomere length in posttraumatic stress disorder. Biol Psychiatry. 2011;70(5):465–471. doi: 10.1016/j.biopsych.2011.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fazeli P, Turan JM, Budhwani H et al. Moment-to-moment within-person associations between acts of discrimination and internalized stigma in people living with HIV: an experience sampling study. Stigma and Health. 2016 doi: 10.1037/sah0000051. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Russell E, Koren G, Rieder M, Van Uum S. Hair cortisol as a biological marker of chronic stress: current status, future directions and unanswered questions. Psychoneuroendocrinology. 2012;37(5):589–601. doi: 10.1016/j.psyneuen.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 33.Wada NI, Jacobson LP, Margolick JB et al. The effect of HAART-induced HIV suppression on circulating markers of inflammation and immune activation. AIDS. 2015;29(4):463–471. doi: 10.1097/QAD.0000000000000545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wyatt GE, Gómez CA, Hamilton AB, Valencia-Garcia D, Gant LM, Graham CE. The intersection of gender and ethnicity in HIV risk, interventions, and prevention: new frontiers for psychology. Am Psychol. 2013;68(4):247–260. doi: 10.1037/a0032744. [DOI] [PubMed] [Google Scholar]
- 35.Hankivsky O. Women’s health, men’s health, and gender and health: implications of intersectionality. Soc Sci Med. 2012;74(11):1712–1720. doi: 10.1016/j.socscimed.2011.11.029. [DOI] [PubMed] [Google Scholar]
- 36.Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? J Int AIDS Soc. 2013;16(3 suppl 2):18734. doi: 10.7448/IAS.16.3.18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hargreaves JR, Stangl A, Bond V et al. HIV-related stigma and universal testing and treatment for HIV prevention and care: design of an implementation science evaluation nested in the HPTN 071 (PopART) cluster-randomized trial in Zambia and South Africa. Health Policy Plan. 2016;31(10):1342–1354. doi: 10.1093/heapol/czw071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tsai AC, Hatcher AM, Bukusi EA et al. A livelihood intervention to reduce the stigma of HIV in Rural Kenya: longitudinal qualitative study. AIDS Behav. 2017;21(1):248–260. doi: 10.1007/s10461-015-1285-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.National HIV/AIDS Strategy for the United States: Updated to 2020. Washington, DC: Office of National AIDS Policy; 2015. [Google Scholar]
- 40.Earnshaw VA, Quinn DM. The impact of stigma in healthcare on people living with chronic illnesses. J Health Psychol. 2012;17(2):157–168. doi: 10.1177/1359105311414952. [DOI] [PMC free article] [PubMed] [Google Scholar]