Abstract
Background:
This study was conducted to assess the validity and reliability of ankle-brachial index (ABI) by oscillometric blood pressure (BP) measurement as compared with an automated ABI as a gold standard.
Materials and Methods:
This study was conducted at Golden Jubilee Medical Center, Thailand. All the data were collected from 303 patients at risk of peripheral arterial disease (PAD) who were 45 years of age or above and who underwent treatment at the outpatient medical clinic between June and December 2015. Patients who were followed up at the medical clinic had both oscillometric BP measurement (Terumo, ES-P600) and an automated ABI (oscillometric method) at the same time. Sensitivity, specificity, positive predictive value, and negative predictive value of the oscillometric BP measurements to predict an abnormal ABI (<0.90) were determined using the automated ABI as the gold standard.
Results:
ABI values were similar between the two methods. The oscillometric BP method for determining an ABI (cutoff point <0.90) on the right side had a sensitivity of 88.89%, specificity of 99.32%, an accuracy of 99.01%, a positive predictive value of 80%, and a negative predictive value of 99.32% whereas ABI on the left side had a sensitivity of 69.23%, a specificity of 99.66%, an accuracy of 98.35%, a positive predictive value of 90%, and a negative predictive value of 98.63%. Reliability of the oscillometric BP method by Kappa statistics was 0.84 on the right side and 0.77 on the left side (P = 0.000).
Conclusion:
The oscillometric BP method is a reliable and useful alternative to conventional automated ABI determination in patients with no severe arterial occlusion for estimation of the prevalence and screening of PAD in primary health-care settings.
Keywords: Automated ankle-brachial index, oscillometric blood pressure, peripheral arterial disease, reliability, validity
INTRODUCTION
Peripheral arterial disease (PAD) is typically asymptomatic and underdiagnosed and this has resulted in the instigation of primary care PAD screening through ankle-brachial index (ABI) measurement. The ABI is the accepted noninvasive gold standard for both diagnosing PAD and the assessment of disease severity.[1,2,3] The ABI has been beneficial for screening generally asymptomatic persons with PAD, and to help in direct medical treatment, exercise programs, angioplasty, and surgery.[4] Even though previous studies have shown that the oscillometric method can be used to measure ABI, the accuracy of oscillometric ABI versus Doppler ABI is controversial. Some authors propose replacing Doppler ABI by oscillometry,[5,6] but other studies have reported a poor agreement between ABI values determined by Doppler and oscillometry.[7,8] Using the Doppler-derived ABI as the gold standard, the sensitivity and specificity of the oscillometric method for determining an ABI ≤ 0.9 are 71% and 92%, respectively. In one study, the overall accuracy for correctly identifying an ABI of 0.9 with the oscillometric method was 82%.[9] However, the accuracy of instruments is different depending on instrument type, general practice population, severity of PAD patients, and cutoff point.[10,11] This study examined patients at risk of PAD in a hospital setting with different criteria from previous studies. This study used blood pressure (BP) measurement (oscillometric BP, Terumo, ES-P600) to manually calculate ABI values as compared with an automated ABI (VP-2000/1000 Type 230, oscillometric method). This automated ABI method is expensive, complex, and requires special training, and is usually only used in larger hospitals. The oscillometric BP method is easy, simple, and requires minimal training, and can be used in large and small hospitals, health-care centers, and in the home. In Thailand, no study has compared oscillometric BP to measure ABI values to those of an automated ABI instrument. Thus, it is important to know whether the oscillometric BP technique is as accurate a measure of ABI as the automated ABI, as that would benefit primary health-care centers and community hospitals, as well as enable self-measurement among the general or at-risk populations for PAD. Thus, the aim of the present study was to assess the validity and reliability of the ABI by oscillometric BP measurement as compared with the automated ABI as the gold standard.
MATERIALS AND METHODS
Study design and population
The experimental study was conducted at the Golden Jubilee Medical Center, Mahidol University, Thailand. Using a sample size calculation with an acceptable error of 5%, a sample size of 169 patients was needed. All the data were collected from 303 patients at risk of PAD who were 45 years of age or older and who underwent treatment at the outpatient medical clinic of the Golden Jubilee Medical Center between June and December 2015. Three inclusion criteria were applied from the guidelines of PAD:[12] (1) patients who had three of seven risk factor symptoms (e.g., diabetes Type 1 or Type 2 or impaired fasting glucose, hypertension (BP >140/90 mmHg or currently treated with antihypertensive agents), chronic kidney disease Stage III–V, dyslipidemia or currently treated with a lipid-modifying agent, currently smoking (>1 cigarettes/day), male older than 55 years, female older than 65 years, and a family history of premature atherosclerosis); (2) patients who had a previous history of cardiovascular events (year of events) with one out of seven symptoms (e.g., chronic stable angina, myocardial infarction, unstable angina, stroke (ischemic), transient ischemic attack, aortic dissection, and peripheral vascular disease); and (3) patients who have a history of cardiovascular intervention (year of intervention) (year of events) with one out of eight symptoms (e.g., percutaneous coronary intervention [PCI], coronary artery bypass graft [CABG], aortic surgery, peripheral artery angioplasty, peripheral artery bypass surgery, amputation of ischemic limbs, carotid stenting, or carotid endarterectomy). The present study was approved by the Ethical Committee of the Faculty of Social Sciences and Humanities, Mahidol University, Institutional Review Board, number 2014/259.1809. All the patients who participated in the study gave written informed consent prior to participation.
Study instruments
The present study used two measurements: oscillometric BP, which can be used in general hospitals and at home (Terumo, ES-P600), and an automated ABI (VP-2000/1000 Type 230, diagnostic tool, machine calculation) as a gold standard for screening at-risk patients used in large hospitals. Both methods were subject to controlled reliability testing on thirty persons before application to the actual sample. Accuracy was 93.33% on the right side and 90% on the left side. Both methods were equally reproducible.
Data collection
Data collection was performed by one practical nurse who was trained in the study design, with two measurements of intraobserver reliability. Patients who were followed up at a medical clinic had both oscillometric BP measurement and automated ABI at the same time. Patients were placed in the supine position, and after 10 min of rest, oscillometric BP measured the brachial BP on both arms and at the posterior tibial artery on both ankles with standard BP cuffs (automated BP measurement in general people), and the ABI value was calculated by hand. The ABI values are calculated by systolic BP of the posterior tibial artery at the ankle in each leg (right and left) divided by the highest brachial arterial systolic pressure of arms (right or left). The automated ABI uses cuffs attached to the brachial and ankle locations at the same time, after which the Doppler blood flow sensor measures systolic BP at the limbs simultaneously.
Statistical analysis
Percentage, mean, median, and standard deviation were used to analyze the descriptive data. The ABI values between the oscillometric BP and the automated ABI as the gold standard for screening at-risk patients were tested by Pearson's Chi-square test. Based on the inter-method concordance on the binary determination of a pathological index, patients were designated to normal ABI group (≥0.9) or abnormal ABI group (<0.9), meaning that the cutoff analysis was ABI < 0.9, as determined by the kappa coefficient (k).[13] Sensitivity, specificity, positive predictive value, negative predictive value, and receiver operator characteristic (ROC) curves of the oscillometric BP measurements to predict an abnormal ABI were determined using the automated ABI as the gold standard. Statistical analyses were performed using PASW Statistics 18.
RESULTS
Three hundred and three patients who visited the medical clinic at Golden Jubilee Medical Center, Mahidol University, Thailand, had ABI determined using both manual oscillometric BP measurement and an automated ABI measurement. The mean patient age was 69.0 years. Most of the patients did not smoke or drink alcohol. Ninety-eight percent of patients had hypertension and dyslipidemia. Forty-five percent of patients had diabetes. Some patients had a history of cardiovascular events such as stroke and had a previous history of cardiovascular intervention such as PCI or CABG [Table 1].
Table 1.
Characteristics of the sample
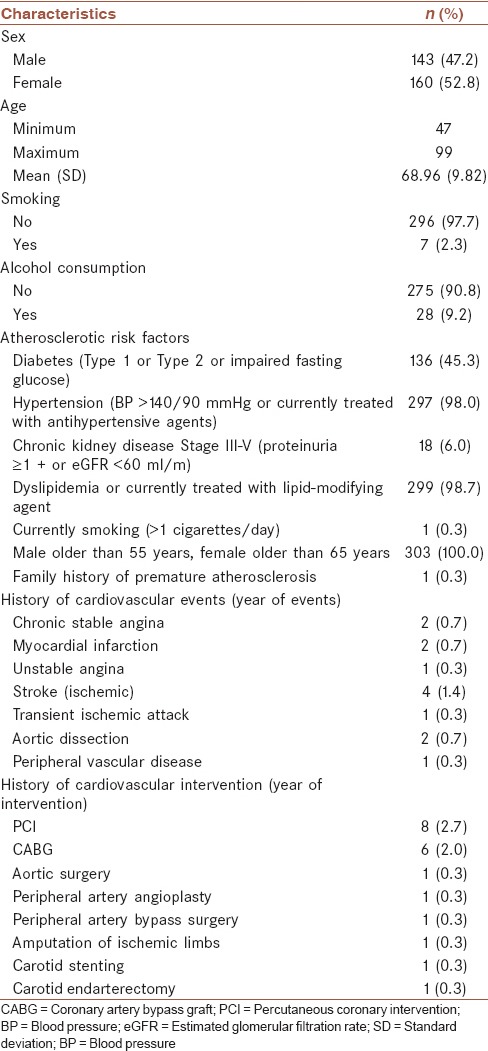
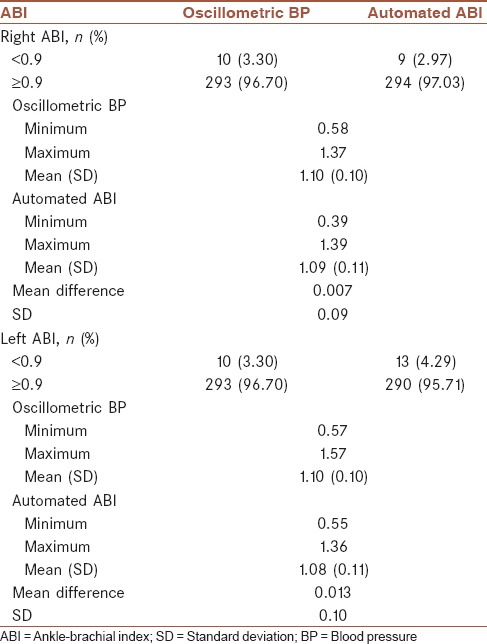
Ninety-seven percent of patients had normal ABI values on both sides as determined with both methods (oscillometric BP and automated ABI). Only 3%–4% of patients had ABI abnormal values (<0.9), on both sides and with both methods. The present study found that ABI values were nearly identical between the two methods. The mean difference between the methods was 0.007 on the right side and 0.013 on the left side [Table 2].
Table 2.
Ankle-brachial index of the oscillometric blood pressure and automated ankle-brachial index measures
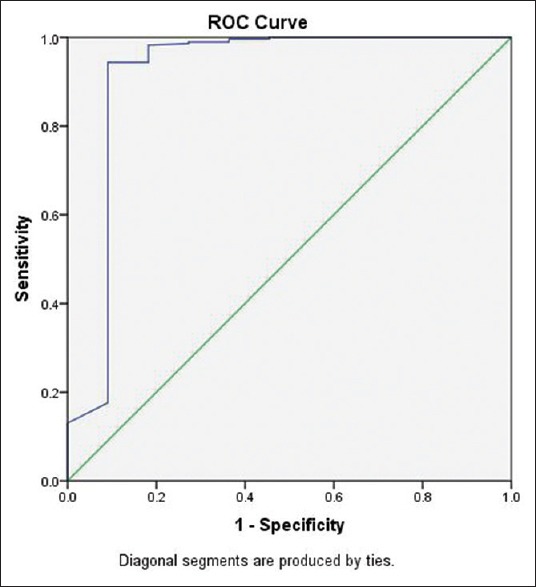
At the cutoff point of <0.90, the validity of the oscillometric BP method for determining an ABI on the right side had a sensitivity of 88.89%, a specificity of 99.32%, an accuracy of 99.01%, a positive predictive value of 80%, and a negative predictive value of 99.32%. Correspondingly, an ABI on the left side had a sensitivity of 69.23%, a specificity of 99.66%, an accuracy of 98.35%, a positive predictive value of 90%, and a negative predictive value of 98.63%. Reliability of the oscillometric BP method by Kappa statistics was 0.84 on the right side and 0.77 on the left side (P = 0.000) [Table 3]. Using the automated ABI as a gold standard, oscillometric BP performance for diagnosis of PAD showed an area under curve the receiver operating characteristic curve (ROC) of 0.99 on the right side and 0.92 on the left side [Figures 1 and 2].
Table 3.
Ankle-brachial index values between oscillometric blood pressure and automated ankle-brachial index
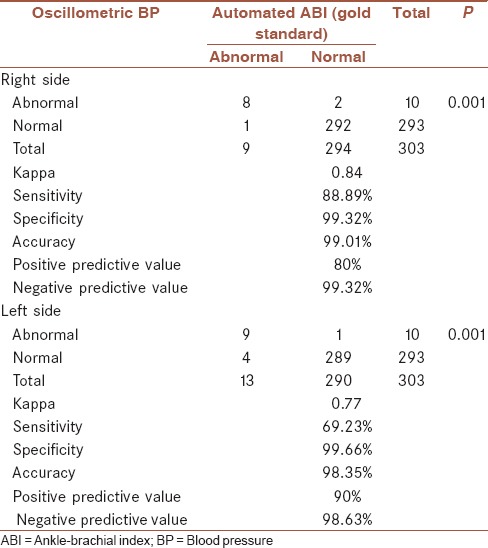
Figure 1.
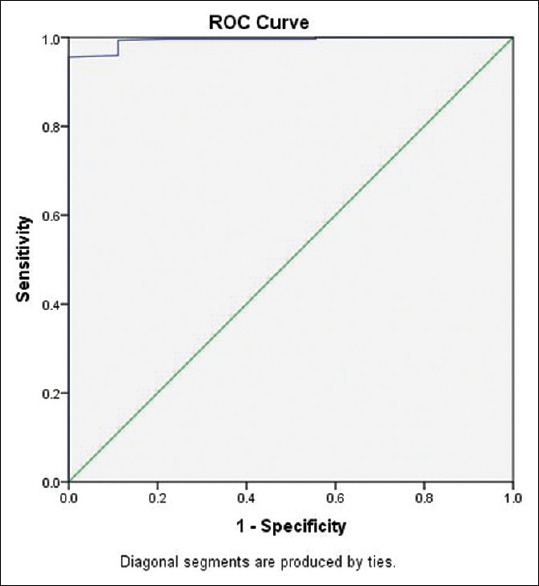
Receiver operator characteristic curve of the right oscillometric blood pressure
Figure 2.
Receiver operator characteristic curve of the left oscillometric blood pressure
DISCUSSION
The results of this study showed that the oscillometric BP method (Terumo, ES-P600) had high validity and reliability in measurement when compared with the automated ABI values (VP-2000/1000 Type 230, oscillometric method). The oscillometric BP method for determining an ABI (cutoff point <0.90) on the right side had a sensitivity of 88.89%, a specificity of 99.32%, an accuracy of 99.01%, a positive predictive value of 80%, and a negative predictive value of 99.32% whereas ABI on the left side had a sensitivity of 69.23%, a specificity of 99.66%, an accuracy of 98.35%, a positive predictive value of 90%, and a negative predictive value of 98.63%. The agreement of both measurements was high (a Kappa of 0.84 on the right side implies an “almost perfect agreement” while a Kappa of 0.77 on the left side implies “substantial agreement”) when compared with other studies. It was possible to determine the ABI in 99% of patients. Only three patients did not have leg oscillometric BP measurements, but they did undergo automated ABI. For patients who had ABI values of <0.74, the oscillometric BP method was not sensitive enough to detect risk for patients with severe PAD. This is similar to a previous study which found that oscillometer OMRON-M3 showed calcified legs and oscillometric “error” readings as arteriopathy equivalents, with a sensitivity of 78.2%, a specificity of 96%, and a cutoff point of 0.96 (sensitivity: 87%, specificity: 91%).[10] Automated oscillometric ABI correlated well with Doppler measurements with high agreement in oligo-symptomatic nondiabetic patients.[14] The oscillometric measurement of ABI had a good correlation with Doppler ultrasound measurements, and there was little difference between the two different machines tested.[15,16,17,18] Our results are in contrast to a previous study in which the oscillometric method compared to the Doppler method showed that it was of low sensitivity (50%), specificity (100%), Kappa (0.65), and correlations in ABIs were 0.46 for the left leg and 0.61 for the right leg.[19] Some studies have shown that automatic oscillometric ABI devices (BOSO ABI) cannot be used interchangeably for standard Doppler ABI measurement in diagnosing PAD, but their high negative predictive value allows their use as a screening tool for PAD.[20] The differences in accuracy of the tests depend on instrument type, measurement methods, PAD severity patients or without PAD, and cutoff point. Limitation of this study includes the small number of patients with abnormal ABI values resulting in uncertain differences between the two measurements. However, this study proposes that the oscillometric BP method can be used to measure ABI values in patients with no severe arterial occlusion when cases have an ABI value of more than 0.74. If the oscillometric BP method cannot determine the ABI value, severe PAD should be suspected. Examination is a reliable indicator of atherosclerosis to identify patients who need intense risk factor modification although a professional specialist should be consulted to apply further diagnostic tests. Future studies should measure sensitivity, specificity, and accuracy of ABI using oscillometric BP measurement as compared with angiogram (a diagnostic test) for detecting patients with PAD.
CONCLUSION
The oscillometric BP method is a reliable and useful alternative to conventional automated ABI determination in patients with no severe arterial occlusion for estimation of the prevalence and screening of PAD in primary health-care settings.
Financial support and sponsorship
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: the study was financially supported by Vejdusit Foundation under the Royal Patronage of H.R.H. Princess Galyani Vadhana Kromluangnaradhiwas Rajanagarindra.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The author would like to thank Golden Jubilee Medical Center, Mahidol University, and the staff for their assistance in collecting data.
REFERENCES
- 1.Weitz JI, Byrne J, Clagett GP, Farkouh ME, Porter JM, Sackett DL, et al. Diagnosis and treatment of chronic arterial insufficiency of the lower extremities: A critical review. Circulation. 1996;94:3026–49. doi: 10.1161/01.cir.94.11.3026. [DOI] [PubMed] [Google Scholar]
- 2.Sacks D, Bakal CW, Beatty PT, Becker GJ, Cardella JF, Raabe RD, et al. Position statement on the use of the ankle-brachial index in the evaluation of patients with peripheral vascular disease: A consensus statement developed by the standards division of the society of cardiovascular and interventional radiology. J Vasc Interv Radiol. 2002;13:353. doi: 10.1016/s1051-0443(07)61735-7. [DOI] [PubMed] [Google Scholar]
- 3.Diehm N, Baumgartner I, Jaff M, Do DD, Minar E, Schmidli J, et al. A call for uniform reporting standards in studies assessing endovascular treatment for chronic ischaemia of lower limb arteries. Eur Heart J. 2007;28:798–805. doi: 10.1093/eurheartj/ehl545. [DOI] [PubMed] [Google Scholar]
- 4.Rooke TW, Hirsch AT, Misra S, Sidawy AN, Beckman JA, Findeiss LK, et al. 2011 ACCF/AHA Focused Update of the Guideline for the Management of Patients with Peripheral Artery Disease (Updating the 2005 Guideline): A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2011;58:2020–45. doi: 10.1016/j.jacc.2011.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vega J, Romaní S, Garcipérez FJ, Vicente L, Pacheco N, Zamorano J, et al. Peripheral arterial disease: Efficacy of the oscillometric method. Rev Esp Cardiol. 2011;64:619–21. doi: 10.1016/j.recesp.2010.10.019. [DOI] [PubMed] [Google Scholar]
- 6.Beckman JA, Higgins CO, Gerhard-Herman M. Automated oscillometric determination of the ankle-brachial index provides accuracy necessary for office practice. Hypertension. 2006;47:35–8. doi: 10.1161/01.HYP.0000196686.85286.9c. [DOI] [PubMed] [Google Scholar]
- 7.Vinyoles E, Pujol E, Casermeiro J, de Prado C, Jabalera S, Salido V. Ankle-brachial index to detect peripheral arterial disease: Concordance and validation study between Doppler and an oscillometric device. Med Clin (Barc) 2007;128:92–4. doi: 10.1016/s0025-7753(07)72499-5. [DOI] [PubMed] [Google Scholar]
- 8.Hamel JF, Foucaud D, Fanello S. Comparison of the automated oscillometric method with the gold standard Doppler ultrasound method to access the ankle-brachial pressure index. Angiology. 2010;61:487–91. doi: 10.1177/0003319709360522. [DOI] [PubMed] [Google Scholar]
- 9.Kornø M, Eldrup N, Sillesen H. Comparison of ankle-brachial index measured by an automated oscillometric apparatus with that by standard Doppler technique in vascular patients. Eur J Vasc Endovasc Surg. 2009;38:610–5. doi: 10.1016/j.ejvs.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 10.Herráiz-Adillo Á, Martínez-Vizcaíno V, Cavero-Redondo I, Álvarez-Bueno C, Garrido-Miguel M, Notario-Pacheco B. Diagnostic accuracy study of an oscillometric ankle-brachial index in peripheral arterial disease: The influence of oscillometric errors and calcified legs. PLoS One. 2016;11:e0167408. doi: 10.1371/journal.pone.0167408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Špan M, Geršak G, Millasseau SC, Meža M, Košir A. Detection of peripheral arterial disease with an improved automated device: Comparison of a new oscillometric device and the standard Doppler method. Vasc Health Risk Manag. 2016;12:305–11. doi: 10.2147/VHRM.S106534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rooke TW, Hirsch AT, Misra S, Sidawy AN, Beckman JA, Findeiss LK, et al. 2011 ACCF/AHA Focused Update of the Guideline for the Management of Patients With Peripheral Artery Disease (Updating the 2005 Guideline) A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2011;58(19):2020–45. doi: 10.1016/j.jacc.2011.08.023. doi: 10.1016/j.jacc.2011.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Viera AJ, Garrett JM. Understanding interobserver agreement: The kappa statistic. Fam Med. 2005;37:360–3. [PubMed] [Google Scholar]
- 14.Diehm N, Dick F, Czuprin C, Lawall H, Baumgartner I, Diehm C. Oscillometric measurement of ankle-brachial index in patients with suspected peripheral disease: Comparison with Doppler method. Swiss Med Wkly. 2009;139:357–63. doi: 10.4414/smw.2009.12636. [DOI] [PubMed] [Google Scholar]
- 15.Arjun J, Jane B, Ted K. Comparison of automated oscillometric measurement of ankle brachial index with standard Doppler measurement as a screening tool for peripheral artery disease. J Vasc Ultrasound. 2013;37:71–5. [Google Scholar]
- 16.Verberk WJ, Kollias A, Stergiou GS. Automated oscillometric determination of the ankle-brachial index: A systematic review and meta-analysis. Hypertens Res. 2012;35:883–91. doi: 10.1038/hr.2012.83. [DOI] [PubMed] [Google Scholar]
- 17.Nelson MR, Quinn S, Winzenberg TM, Howes F, Shiel L, Reid CM. Ankle-Brachial Index determination and peripheral arterial disease diagnosis by an oscillometric blood pressure device in primary care: Validation and diagnostic accuracy study. BMJ Open. 2012;2 doi: 10.1136/bmjopen-2012-001689. pii: e001689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rosenbaum D, Rodriguez-Carranza S, Laroche P, Bruckert E, Giral P, Girerd X. Accuracy of the ankle-brachial index using the SCVL(®), an arm and ankle automated device with synchronized cuffs, in a population with increased cardiovascular risk. Vasc Health Risk Manag. 2012;8:239–46. doi: 10.2147/VHRM.S29405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Takahashi I, Furukawa K, Ohishi W, Takahashi T, Matsumoto M, Fujiwara S. Comparison between oscillometric- and Doppler-ABI in elderly individuals. Vasc Health Risk Manag. 2013;9:89–94. doi: 10.2147/VHRM.S39785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wohlfahrt P, Ingrischová M, Krajcoviechová A, Palous D, Dolejsová M, Seidlerová J, et al. A novel oscillometric device for peripheral arterial disease screening in everyday practice. The Czech-post MONICA study. Int Angiol. 2011;30:256–61. [PubMed] [Google Scholar]


