Abstract
BACKGROUND AND OBJECTIVE:
Studies have shown that pre-Ramadan structured educational program for patients with diabetes mellitus (DM) is beneficial. In this study, our aim was to evaluate the degree of adherence of treating physicians to such programs and their influence on the patient's knowledge and behavior.
MATERIALS AND METHODS:
This cross-sectional study was carried out on adult patients with DM attending a university hospital, who were observed while fasting during Ramadan 1436/2015. Data was collected using a questionnaire-based interview. Baseline characteristics were obtained, and patients were asked whether they had had pre-Ramadan education or not and who the provider was. Patients' knowledge of the components of the recommended structured pre-Ramadan educational program was also tested. Comparison between patients who had the education and those who did not was done using Chi-square test and independent samples Student's t-test; p ≤ 0.05 was considered statistically significant.
RESULTS:
A total of 298 patients with type 1 or type 2 DM were included in the study; 75.5% of the patients were aged 40 years or older. Only 30% had pre-Ramadan education delivered mainly by diabetic educators or the treating physicians (52% and 44%, respectively). Patients who had the education were younger (mean age: 45.6 ± 17.4 vs. 50.3 ± 14.4, respectively, p = 0.0048), had higher educational qualifications, were more likely to be employed, and self-monitored their blood glucose more frequently (p = 0.0001). There was no difference between the two groups with regard to their knowledge of diet and exercise.
CONCLUSION:
The adherence to the pre-Ramadan educational program by the treating physician was low. It is necessary to increase the awareness about the importance of these programs among health-care professionals. The programs should target the less educated, the unemployed, and older patients.
Key words: Diabetes, education, fasting, hypoglycemia, Ramadan
Introduction
Fasting in the holy month of Ramadan is one of the five pillars of Islam. All healthy Muslims are obliged to fast Ramadan each year once they reach puberty. Individuals must refrain from eating, drinking, and using oral medication between dawn and sunset. Depending on the season and geographic setting, the duration of the daily fast may range from 12 to 20 h. Ramadan fasting has several potential benefits particularly to healthy individuals but may adversely affect sick patients including those with diabetes mellitus (DM). Adverse effects which may affect patients with DM during Ramadan fasting include hypoglycemia, hyperglycemia, diabetic ketoacidosis (DKA), dehydration, and increased risk of thrombosis, resulting in stroke and retinal artery occlusion.[1] Patients with DM are classified as low risk, moderate risk, high risk, and very high risk for the development of such complications. Those in the categories of high risk and very high risk are usually advised not to fast.[2] In general, the Quran exempts an individual from fasting if the health of that individual can be adversely affected by fasting.[3] However, a population-based study conducted during Ramadan 1422/2001 in 13 Islamic countries which involved 12,914 diabetic patients showed that 42.8% of patients with type 1 diabetes and 79.7% of patients with type 2 diabetes reported that they fasted Ramadan.[4] The same study also showed that the risk of severe hypoglycemia increased 4.7-fold in patients with type 1 diabetes and around 7.5-fold in patients with type 2 diabetes during fasting. Based on these findings, several recommendations have been made by different medical societies for the management of diabetes in patients who elect to fast in Ramadan.[1,2,5] Patients' education through the delivery of structured educational program individually or in groups has been identified as an important component of the management of these patients. The educational program is supposed to be presented by the medical team, that is, by the treating physician and/or diabetic educators. Education needs to be given before the start of Ramadan and should be directed to the general public, health-care professionals, and patients with DM.[6] Individuals presenting the structured focused Ramadan education should stress on four key areas: (1) Meal planning and dietary advice, (2) exercise, (3) blood glucose monitoring, and (4) recognition and management of complications.[6] In addition, advice on the change in doses of medication and timing need to be emphasized.[6,7] Few studies have been conducted lately that showed the positive impact of pre-Ramadan diabetes education on decreasing the risk of complications and improving the control of DM.[8,9,10] One study showed that 75% of patients admitted with DKA during Ramadan had not had any structured educational program on diabetes management while they fast.[11]
Adherence of health-care providers to such educational programs has not been well studied in most of the Muslim countries. The aim of this study was to evaluate the adherence of health-care providers to the presentation of pre-Ramadan educational program to patients attending one of the university hospitals in Saudi Arabia and study the effect of the educational program on the knowledge and behavior of the patient.
Materials and Methods
This was a cross-sectional study conducted between September 2015 and April 2016 at King Fahd Hospital of the University, Al Khobar, Saudi Arabia. The study included adult patients above the age of 18 with type 1 or type 2 DM, who fasted during the month of Ramadan of the year 1436/2015. Pregnant women and patients who refused to consent to the study were excluded from the study. Conveniently available sample was used, and data were collected using a questionnaire-based interview carried out on a one-on-one basis by one of the researchers. Patients were recruited from inpatient wards and outpatient clinics. After explaining the objective of the research and assuring the patients of the confidentiality of data, consent was taken and the data were collected. Baseline data included information on age, gender, level of education, type of diabetes and its duration, type of diabetic therapy used, and who the treating physician was. Patients were also asked whether they had had pre-Ramadan education for the year of 1436/2015 or not, who the provider was, and what type of information was delivered. Patients who got their information through the media, the Internet and family, were considered as having received pre-Ramadan education. Patients' knowledge of the details of the recommended structured pre-Ramadan educational program was also assessed. Patients were asked about the risks of fasting in Ramadan when to break the fast, recognition of complications, meal planning, physical activity, and blood glucose monitoring during Ramadan. The study was approved by the Institutional Review Board (IRB) of the University of Dammam in accordance with the local regulations (IRB – 2015-01-152 on 30/08/2015).
Data were analyzed using Statistical Package for Social Sciences version 22 (IBM), (Software, SPSS, inc., Chicag, IL, USA). Categorical variables are presented in the form of frequencies, percentages, and means ± standard deviations. Comparison between patients who had had instructions and those who had not had any instruction was done using Chi-square test and independent samples Student's t-test. P ≤ 0.05 was considered statistically significant. Regression analysis was done to study the effect of different variables on the likelihood of getting the education.
Results
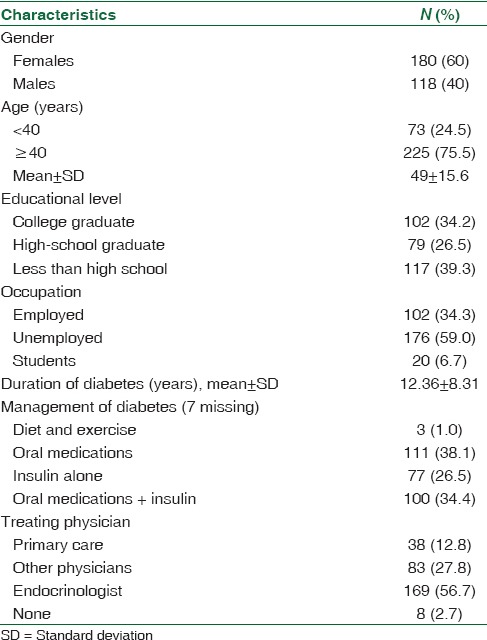
A total of 298 patients were recruited. As shown in Table 1, the mean age was 49 ± 15.6 years; 75.5% of patients were 40 years or older, and 60% were females. Furthermore, 60.7% were at least high-school graduates. The mean duration of DM was 12.36 ± 8.31 years. Patients who were being managed by lifestyle modification represented only 1% of diabetics while the majority took insulin either by itself or in combination with oral glucose lowering agents (OGLAs). More than half of the patients were being managed by an endocrinologist.
Table 1.
Characteristics of the study participants
Only 30% of the interviewed patients had had pre-Ramadan education. Table 2 shows the comparison between patients who had the pre-Ramadan education and patients who had not had it. Patients who had the education were significantly younger than the ones who had not had any instruction (mean age: 45.6 ± 17.4 vs. 50.3 ± 14.4, respectively, p = 0.0048). More than 60% of patients in the group who had not had any instructions were females. There were also significantly more college graduates in the group that had been given pre-Ramadan instructions compared to patients who had not had any (p = 0.0453 and p = 0.0197, respectively). There is a significantly higher percentage of patients with less than high school education among females who had not had pre-Ramadan education than patients who had received it (p = 0.001). Results also showed that there were more unemployed females (75.3% vs. 60%, p = 0.0004) in the group who had not received the instructions compared to the group who had the instructions.
Table 2.
Characteristics of the study participants by receiving pre-Ramadan education
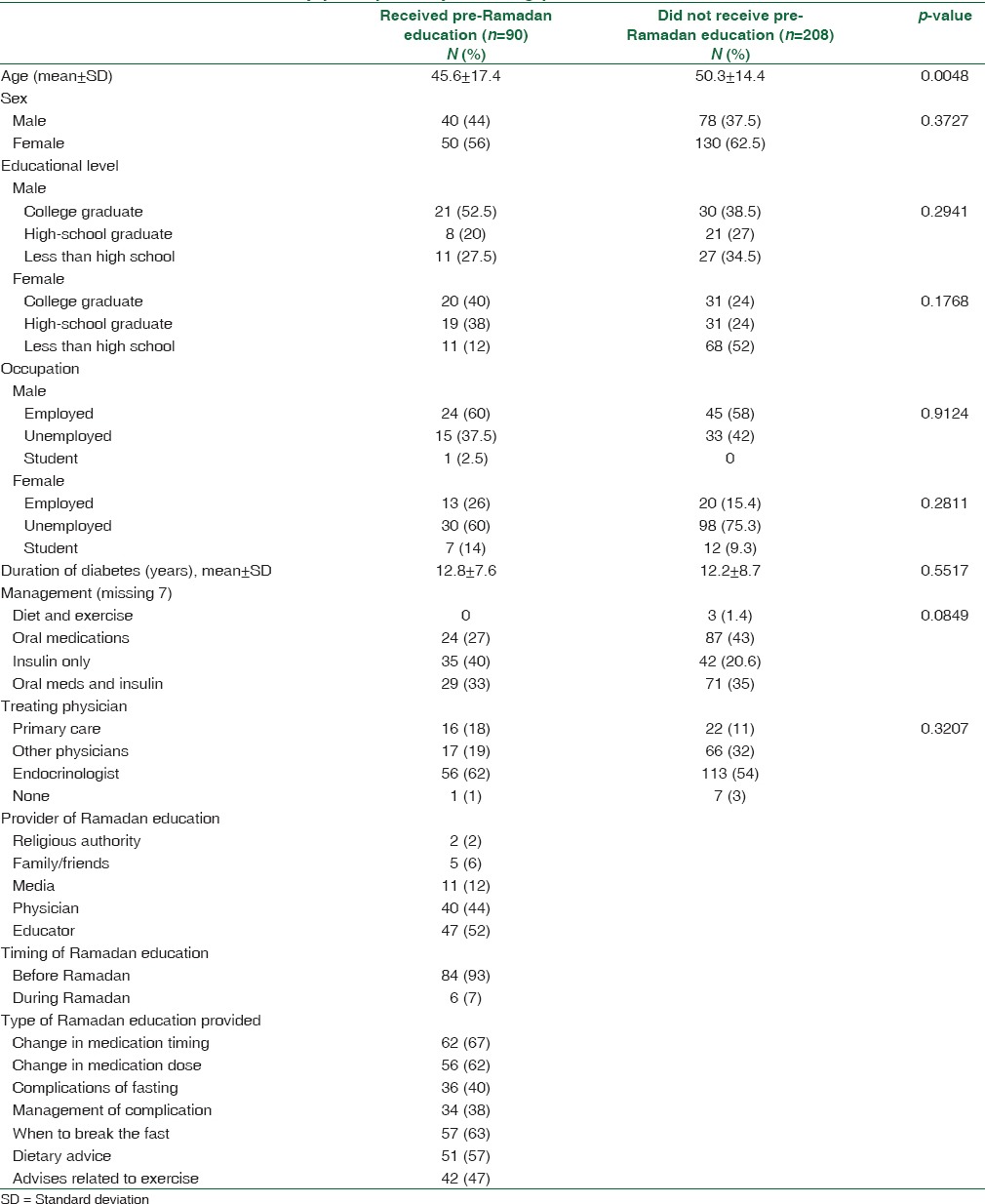
Patients who had pre-Ramadan education were more likely to be managed with insulin (p < 0.0001) while patients who did not get pre-Ramadan education were more likely to be managed with OGLAs alone (43% vs. 27%, p = 0.0007). In addition, patients who were being managed by an endocrinologist were more likely to have received instructions (62% vs. 54%, p = 0.0369). However, logistic regression analysis showed no significant associations between these variables and receipt of instructions. Patients get pre-Ramadan education from a variety of sources but mainly from physicians (44%) and diabetic educators (52%). More than 90% of the patients had the program before Ramadan. Not all patients who had the education were given all the suggested components of the structured educational program. For example, only 40% of the patients were informed on the possible complications of DM when fasting in Ramadan and only 38% of patients were given instructions on how to manage these complications. Furthermore, only 47% of patients were given advice on physical activity during Ramadan, and only 57% of the patients who had the structured education were given advice on their diet.
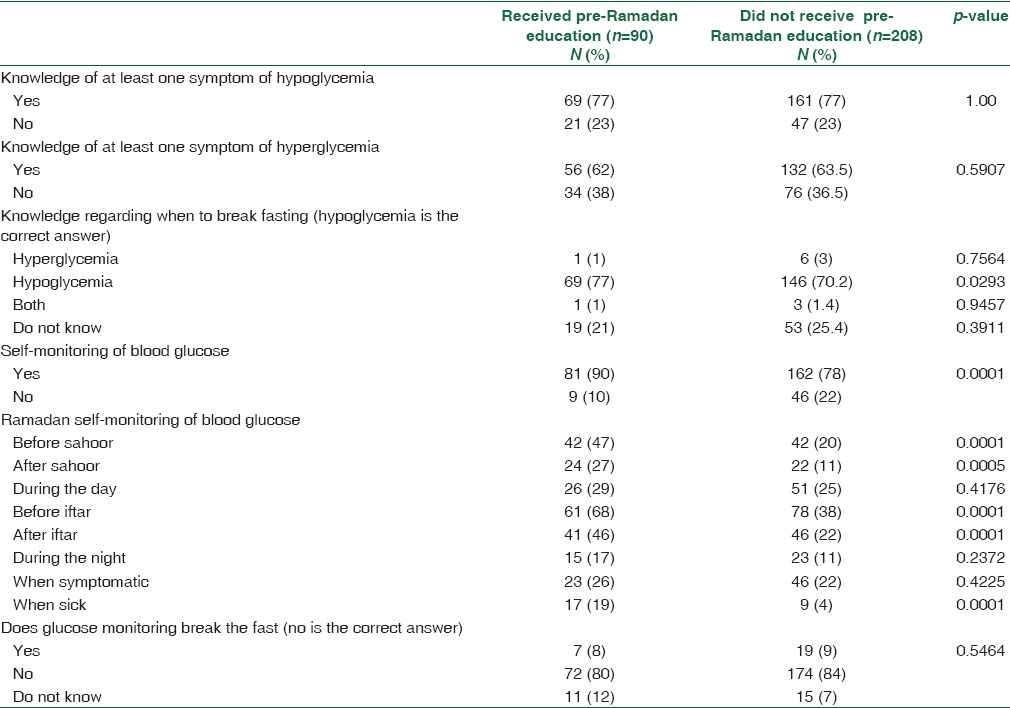
Table 3 represents the comparison of knowledge on diabetes of patients who had the education on fasting in Ramadan and patients who did not. There is no significant difference in the knowledge of hypoglycemic and hyperglycemic symptoms between the two groups, but knowledge on the need to break the fast in the event of hypoglycemia was significantly higher in the group that was instructed (77% vs. 70.2%, p = 0.0293). In addition, there was a higher percentage of patients who did not know when to break the fast in the group that did not get the pre-Ramadan education (25.4% vs. 21%), but p-value for the difference between the two groups was not significant (p = 0.3911). There is no significant difference between the two groups in the percentage of patients who did not believe that self-monitoring of blood glucose (SMBG) broke the fast (p = 0.5464). However, as a result of pre-Ramadan education, there were more patients who performed SMBG (90% vs. 78%, p = 0.0001) and more patients who did SMBG during the fast at different times of the day. For example, the number of patients who performed SMBG before sahoor and before iftar was significantly higher in the group that had had the pre-Ramadan education (47% vs. 20%, p = 0.0001, and 68% vs. 38%, p = 0.0001, respectively).
Table 3.
Knowledge of diabetes among study participants by receiving pre-Ramadan education
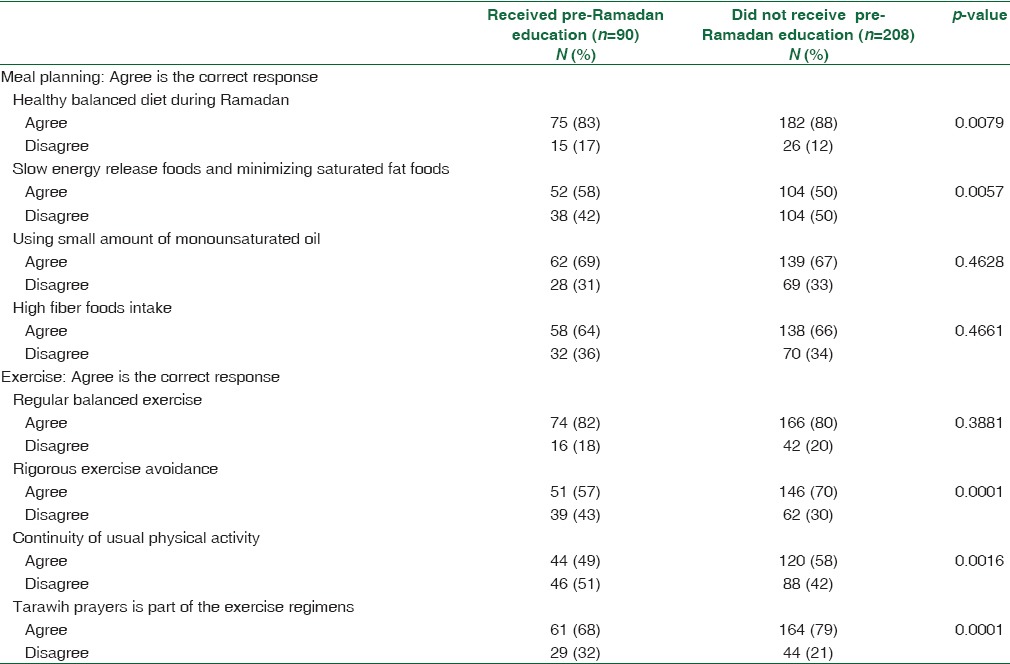
Patients' knowledge of diet and exercise during the month of Ramadan is shown in Table 4. There was no significant difference between the two groups as regards to two of the four statements related to diet, but the group that had the education had significantly better knowledge in one of the statements, and the group who did not get the education also had significantly better knowledge in another statement. However, the group that did not get the pre-Ramadan instructions had significantly better knowledge in three of the four statements related to exercise, but there was no significant difference between the two groups with regard to the fourth statement.
Table 4.
Knowledge about diet and exercise among study participants by receiving pre-Ramadan education
Discussion
Structured patient education, self-management, and lifestyle modification are important components of the care of patients with DM.[12,13] Ramadan-focused structured education is needed to minimize the challenges faced by diabetic patients who fast in Ramadan sometimes even against medical advice.
In this cross-sectional study, we evaluated the degree of adherence of health-care providers at one of the university hospitals to such an educational program. We found that less than one-third of patients had been given structured instructions on fasting during Ramadan 1436/2015. There are few studies in the literature for comparison, but a similar study was conducted by Masood et al.[14] in Pakistan at a primary care center and at a tertiary care center, in which they compared the Ramadan-specific education level of diabetic patients who fasted during Ramadan 2011. They reported that 55.32% patients from the primary care center and 61.80% patients from the tertiary care center had got pre-Ramadan education, which is double the percentage, found in this study. We think that our low percentage of patients who had pre-Ramadan education is because little attention is given to such an important educational program in this part of the world. Our finding is supported by the recently published multicenter study conducted in Egypt, Iran, Jordan, and Saudi Arabia by McEwen et al.,[10] where they found that only 14% of their patients stated that they usually had diabetes education before Ramadan and only 18% stated that they usually had diabetes education during Ramadan.
However, a recent study carried out in 13 countries of the Middle East, Asia, Europe, and North America indicated that 96.2% of physicians reported providing fasting-specific advice to their patients, and 62.6% reported using guidelines or recommendations for the management of diabetes during Ramadan. However, in that retrospective study, patients were not asked if they actually had a special education or not.[15] A study from France evaluated both diabetic Muslim patients and their general practitioners (GPs) attitudes and practices toward fasting during Ramadan. It was found that 85% of the GPs reported that they had spoken about Ramadan fasting with their patients while only 64% of the patients studied stated that they had discussed the issue with their GPs.[16] Furthermore, the study from France did not evaluate the use of the structured educational program and merely discussed the matter of fasting between the patient and his treating physician which did not indicate that a proper structured educational program or advice being given.
The baseline characteristics of patients in our study in terms of age, gender distribution, and level of education are similar to the study by McEwen et al.,[10] but more male and female patients in their study were employed. Besides, they had fewer patients treated with insulin alone or in combination with OGLAs. As in our study, most of the patients in the McEwen et al.'s[10] study were treated by endocrinologists and had pre-Ramadan education from different sources.
It is interesting to note that the patients who had pre-Ramadan education in our study were generally younger, had a higher level of education, and were employed compared to the patients who did not get the education. Furthermore, there were more females in the group who did not receive the instructions. Patients' educational level plays an important role. There were more patients with less than high-school education who did not receive pre-Ramadan education. This might be explained by their inability to search for instructions on the internet, for example, or other resources on what to do about their disease during Ramadan.
These findings imply that patients' factors may contribute to the likelihood of getting the educational program related to fasting during Ramadan. Physician factors may also play a role. This may relate to physicians' lack of awareness about the importance of this educational program. Patients' treated by endocrinologists are more likely to get instructions and the physician would normally give instructions to patients being treated with insulin more than to patients on OGLAs alone. However, logistic regression analysis showed no significant associations between these factors and getting the education.
Another important finding in this study is that not only was less than one-third of diabetic patients given instructions on fasting in Ramadan but also those who did not get all the components of the suggested educational program. Most of the education was on the change in the times at which the medication is taken, which only 67% of the patients got, while the component that got the least mention was about the management of complications, which only 38% of the patients were given instruction on. This is different from the study by Masood et al.,[14] in which the delivery of components of the pre-Ramadan educational program ranged between 46.01% and 89.97% at the primary care center and between 57.08% and 97.89% at the tertiary care center. We think that the lack of coverage of all components of the educational program contributed to the unexpectedly low level of knowledge related to diet and exercise in the group who had the pre-Ramadan education. In addition, the difference between the two groups regarding the knowledge of diet and exercise will be better tested by a qualitative study, in which patients will be allowed to talk about what they know rather than be given logical statements to agree or disagree with. The quantitative method used here possibly contributed to the findings that the group who did not get the education showed significantly better knowledge in some of the statements.
It is expected that the two groups did not differ in their knowledge of the symptoms of hyperglycemia and hypoglycemia because this information is usually given to all diabetic patients outside the pre-Ramadan educational program. However, as a result of the education, the two groups differed significantly in some aspects of specific knowledge related to fasting in Ramadan such as breaking the fast during hypoglycemia. Although there was no difference in the misconception that SMBG breaks a fast, a significantly higher percentage of patients in the group that got the instructions monitored their blood sugar during the Ramadan fast. This is consistent with the findings of McEwen et al.,[10] which indicated an 80% increase in the frequency of glucose monitoring during fasting in the intervention group compared to 58% increase in their control group.
The strength of this study is that it is one of the few studies to use a control group and evaluate physician adherence to the pre-Ramadan educational program. Limitations of our study include the small sample size, the use of convenient sample, and the possibility of recall bias.
Conclusion
Ramadan fast may carry some risks to patients with DM. The structured pre-Ramadan educational program has been shown to improve metabolic control and reduce the risk of complications in diabetic patients who elect to fast. Unfortunately, in this study, adherence to the educational program by the treating physicians of patients is very low. There is a need to increase awareness in health-care professionals about the importance of these educational programs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Al-Arouj M, Assaad-Khalil S, Buse J, Fahdil I, Fahmy M, Hafez S, et al. Recommendations for management of diabetes during Ramadan: Update 2010. Diabetes Care. 2010;33:1895–902. doi: 10.2337/dc10-0896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Arouj M, Bouguerra R, Buse J, Hafez S, Hassanein M, Ibrahim MA, et al. Recommendations for management of diabetes during Ramadan. Diabetes Care. 2005;28:2305–11. doi: 10.2337/diacare.28.9.2305. [DOI] [PubMed] [Google Scholar]
- 3.The Holy Quran, Surat Al-Baqarah Aya 184, Printed by King Fahad Complex in 1428 H.
- 4.Salti I, Bénard E, Detournay B, Bianchi-Biscay M, Le Brigand C, Voinet C, et al. A population-based study of diabetes and its characteristics during the fasting month of Ramadan in 13 countries: Results of the epidemiology of diabetes and Ramadan 1422/2001 (EPIDIAR) study. Diabetes Care. 2004;27:2306–11. doi: 10.2337/diacare.27.10.2306. [DOI] [PubMed] [Google Scholar]
- 5.Diabetes and Ramadan: Practical Guidelines. Brussels, Belgium: International Diabetes Federation; 2016. [Last accessed on 2016 Aug 04; Last accessed on 2016 Aug 04]. International Diabetes Federation and the DAR International Alliance. Available from: http://www.idf.org/guidelines/diabetes-in-ramadan ; http://www.daralliance.org . [Google Scholar]
- 6.Hassanein M. Ramadan focused diabetes education; a much needed approach. J Pak Med Assoc. 2015;65(5 Suppl 1):S76–8. [PubMed] [Google Scholar]
- 7.Hui E, Bravis V, Hassanein M, Hanif W, Malik R, Chowdhury TA, et al. Management of people with diabetes wanting to fast during Ramadan. BMJ. 2010;340:c3053. doi: 10.1136/bmj.c3053. [DOI] [PubMed] [Google Scholar]
- 8.Bravis V, Hui E, Salih S, Mehar S, Hassanein M, Devendra D. Ramadan Education and Awareness in Diabetes (READ) programme for Muslims with type 2 diabetes who fast during Ramadan. Diabet Med. 2010;27:327–31. doi: 10.1111/j.1464-5491.2010.02948.x. [DOI] [PubMed] [Google Scholar]
- 9.Ahmedani MY, Alvi SF, Haque MS, Fawwad A, Basit A. Implementation of Ramadan-specific diabetes management recommendations: A multi-centered prospective study from Pakistan. J Diabetes Metab Disord. 2014;13:37. doi: 10.1186/2251-6581-13-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McEwen LN, Ibrahim M, Ali NM, Assaad-Khalil SH, Tantawi HR, Nasr G, et al. Impact of an individualized type 2 diabetes education program on clinical outcomes during Ramadan. BMJ Open Diabetes Res Care. 2015;3:e000111. doi: 10.1136/bmjdrc-2015-000111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abdelgadir E, Hafidh K, Basheir A, Afandi B, Alawadi F, Rashid F, et al. Comparison of incidences, hospital stay and precipitating factors of diabetic ketoacidosis in Ramadan and the following month in three major hospitals in United Arab Emirates. A prospective observational study. J Diabetes Metab. 2015;6:3. [Google Scholar]
- 12.Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Hess Fischl A, et al. Diabetes self-management education and support in type 2 diabetes: A joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Diabetes Care. 2015;38:1372–82. doi: 10.2337/dc15-0730. [DOI] [PubMed] [Google Scholar]
- 13.Deakin TA, Cade JE, Williams R, Greenwood DC. Structured patient education: The diabetes X-PERT Programme makes a difference. Diabet Med. 2006;23:944–54. doi: 10.1111/j.1464-5491.2006.01906.x. [DOI] [PubMed] [Google Scholar]
- 14.Masood S, Alvi S, Ahmedani M, Kiran S, Zeeshan N, Basit A, et al. Comparison of Ramadan-specific education level in patients with diabetes seen at a primary and a tertiary care center of Karachi-Pakistan. Diabetes Metab Syndr Clin Res Rev. 2014;8:225–9. doi: 10.1016/j.dsx.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 15.Babineaux SM, Toaima D, Boye KS, Zagar A, Tahbaz A, Jabbar A, et al. Multi-country retrospective observational study of the management and outcomes of patients with type 2 diabetes during Ramadan in 2010 (CREED) Diabet Med. 2015;32:819–28. doi: 10.1111/dme.12685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gaborit B, Dutour O, Ronsin O, Atlan C, Darmon P, Gharsalli R, et al. Ramadan fasting with diabetes: An interview study of inpatients' and general practitioners' attitudes in the South of France. Diabetes Metab. 2011;37:395–402. doi: 10.1016/j.diabet.2010.12.010. [DOI] [PubMed] [Google Scholar]


