Abstract
Aims:
To evaluate outcomes of deep anterior lamellar keratoplasty (DALK) in pediatric eyes with unilateral severe chemical injury which have undergone autologous simple limbal epithelial transplant (SLET).
Settings and Design:
The study design was a retrospective case series.
Materials and Methods:
This retrospective, case series of all children <16 years of age that have undergone DALK following autologous SLET procedure in unilateral severe chemical injury evaluates the outcomes and complications in the setting of a tertiary care center in North India.
Statistical Analysis Used:
Nonparametric data have been expressed as median (range), parametric qualitative data as percentage, and quantitative data as a mean ± standard deviation. Spearman's correlation coefficient is used for finding a correlation between variables.
Results:
Eleven eyes of 11 children (5 male and 6 female) with a mean age of 8.9 ± 4.7 years underwent DALK following ocular surface reconstruction with autologous SLET earlier for unilateral severe chemical injury with limbal stem cell deficiency. Follow-up ranged from 6 to 18 months (13.00 ± 4.58 months) following DALK procedure. All patients with a minimal follow-up of 6 months were evaluated for visual outcomes. Visual acuity ranged from 0.3 to 3 logMAR units (0.6 ± 0.2 logMAR units). Complications were encountered in three patients. Anatomical success was seen in 72.72% patients and visual success was noted in 54.54% patients.
Conclusions:
DALK is a feasible option in children with severe unilateral chemical injury who have undergone ocular surface reconstruction with autologous SLET procedures.
Key words: Keratoplasty, limbal transplantation, outcomes
Ocular chemical injuries constitute a major part of the ocular emergencies which need prompt and consistent management as these are potentially blinding conditions.[1] Limbal stem cell deficiency (LSCD) is an important consequence of the ocular chemical injuries which can have varied manifestations such as loss of palisades of Vogt, localized vascularization or conjunctivalization in mild grade chemical injuries to severe conjunctivalization, keratinization, symblepharon formation, and subsequent loss of vision in severe chemical injuries.[2,3,4] Cosmetic and visual rehabilitation in such patients is quite a challenging task considering the associated morbidity of the ocular surface and loss of limbal stem cells which threatens the survival of the corneal graft. These limbal cells are essential for the epithelialization of the cornea. Therefore, ocular surface rehabilitation forms the stepping stone in such cases before any further procedures can be performed.[2,5] Various modalities of limbal stem cell transplantation (LSCT) to replenish the limbal stem cells have been tested over the years, and the decision for undertaking any particular procedure solely depends on the severity of LSCD and the laterality of the condition.[6,7,8,9,10] Cultivated limbal epithelial transplant (CLET) has shown good results in both unilateral and bilateral ocular chemical injuries.[7,9,11] The newer modality described is the simple limbal epithelial transplant (SLET) in uniocular chemical injuries.[8,12,13,14,15] This technique co-opts the advantages of combining conjunctival limbal autograft and cultivated limbal stem cell transplant and obviates the need for ex vivo expansion of cells and expensive laboratory setup.[2,8,9] Once ocular surface stabilization is achieved with SLET reconstruction, visual rehabilitation can be undertaken as either lamellar or full-thickness keratoplasty. The inflammatory response to any kind of injury is expected to be more in the pediatric age group.[7,8] Existing literature provides us insight into the outcomes of penetrating keratoplasty after limbal transplantation[16,17] and a few cases of deep anterior lamellar keratoplasty (DALK) following chemical injury.[18,19,20,21] This retrospective review presents the outcomes of DALK after SLET in cases of uniocular chemical injury in the pediatric age group. In this study, we found out that DALK is a feasible option in children with unilateral chemical injury who have undergone autologous SLET procedure for ocular surface reconstruction.
Materials and Methods
Study design, approval, and subjects
This is a retrospective case series study which was done in accordance with the tenets of Declaration of Helsinki and clearance from the Institutional Ethics Committee was obtained. Clinical records of follow-up pediatric patients (<18 years of age) in the period of April 2014 to July 2016, with unilateral severe chemical injury (total LSCD with the absence of palisades of Vogt, presence of conjunctivalization of the cornea or pannus 360° of the limbus/corneal surface, or partial LSCD of ≥6 clock hours involvement of the limbus) who had undergone autologous SLET by a single surgeon (MV) were reviewed to study the outcomes of lamellar keratoplasty following ocular surface reconstruction by SLET in these eyes affected with severe ocular morbidity. Diagnosis of LSCD was done by clinical impression on examination in two patients not cooperative for impression cytology and supported by impression cytology confirming the presence of goblet cells on the corneal surface in nine children.
Retrospective data collection
The preoperative details which were noted included demographics, primary etiology, impression cytology reports, any previous ocular surgery, visual acuity at presentation, extent of LSCD, any coexistent lid anomalies or presence of symblepharon, intraocular pressure, and the interval duration between the various procedures. The follow-up parameters noted included visual acuity (in logMAR scale) after SLET and DALK and ocular surface stability (defined as ocular surface without recurrent surface epithelial morbidity and hyperemia) after SLET and outcomes of DALK (visual acuity and postoperative complications).
Retrospective surgical details
Autologous simple limbal epithelial transplant
Donor limbal tissue was retrieved from the healthy fellow eyes of the patients of uniocular chemical injuries as 2 mm × 2 mm strips including conjunctival and corneal epithelium and was cut into 7–8 small pieces. Removal of pannus and symblepharon (if any) from the corneal surface was then carried out. The amniotic membrane was then placed over the corneal surface and was anchored to surrounding conjunctiva with the help of 8-0 vicryl sutures (Johnson and Johnson medical Ltd., Livingston UK). Cut pieces of the donor limbus from the other eyes were then placed over the amniotic membrane with the help of human fibrin glue (TISSEL Kit, Baxter AG, Vienna, Austria) and allowed to dry followed by placement of bandage contact lens over the cornea.
Deep anterior lamellar keratoplasty
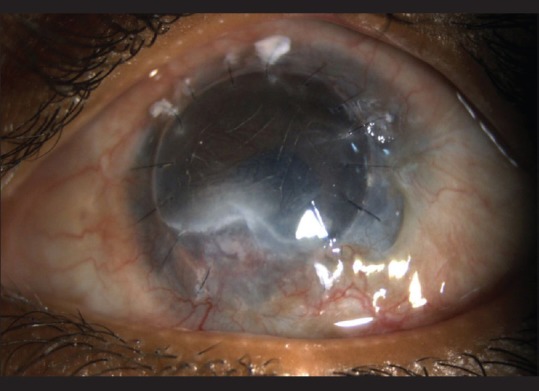
The technique for DALK included manual deep lamellar dissection (with intraoperative pachymetry-assisted manual lamellar dissection of recipient bed in few cases) till the host Descemet's membrane was reached. Donor tissue was stripped off its Descemet's membrane and trephined to adequate size and was then sutured to the recipient bed by 16 interrupted 10-0 monofilament nylon sutures [Fig. 1].
Figure 1.
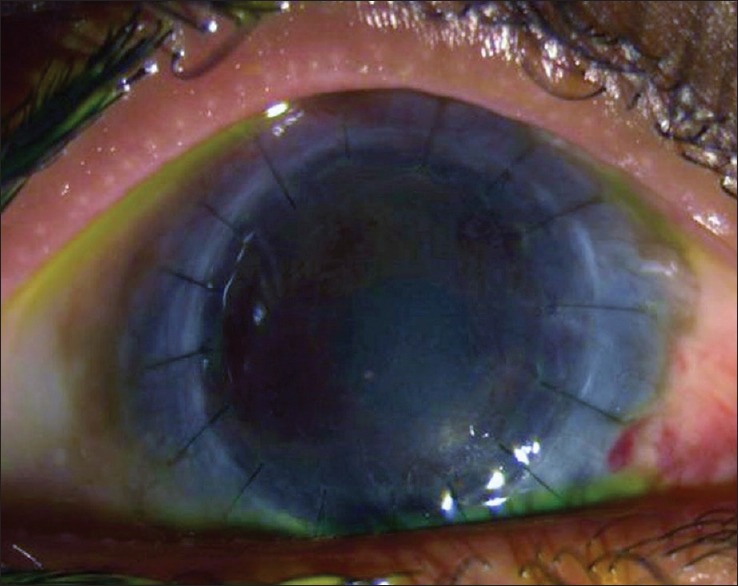
Immediate postoperative deep anterior lamellar keratoplasty
Outcome measures
The primary outcome measure was the success of the graft, defined as a completely epithelialized, clear, and avascular graft. Failure was defined as the occurrence of persistent epithelial defects, progressive conjunctivalization or opacification into the visual axis, microbial keratitis, and need for repeat surgery. The grafts that did not clear within 2 weeks following the transplantation were considered as primary graft failure and those occurring after it were considered as secondary graft failures. The secondary outcome measures were the improvement in best-corrected visual acuity (BCVA) by ≥2 lines of Snellen visual acuity, complications, or any recurrences of LSCD.
Statistical analysis
The data were recorded in an Excel spreadsheet and analyzed using SPSS software version 17 (SPSS Inc., Chicago, Illinois, USA). For descriptive purposes, nonparametric data have been expressed as median (range), parametric qualitative data have been expressed as a percentage, and quantitative data have been expressed as a mean ± standard deviation. Spearman's correlation coefficient is used for finding a correlation between variables and P < 0.05 is taken as statistically significant.
Results
Eleven patients were included in this study, of which six (54.55%) were females and five (45.45%) were males [Table 1]. Mean age of presentation was 8.9 ± 4.7 years (2–16 years). Six patients (54.55%) had right eye involvement and other five (45.45%) had the involvement of the left eye. Most common mode of injury was the chuna packet injury in eight (72.73%) patients, followed by firecracker injury in two (18.18%) patients and painting lime injury in one (9.09%) patient. Five (45.45%) out of 11 patients had symblepharon release or amniotic membrane transplantation as the initial procedure before SLET and other six (54.55%) had no prior ocular surgery. Mean duration between the chemical injury and SLET was 11.63 ± 2.97 months (9–17 months) and mean duration between SLET and DALK was 11.63 ± 2.21 months (9–15 months). At the time of presentation, mean limbal involvement was 8.27 ± 2.19 clock hours with the BCVA of 2.45 ± 0.52 logMAR units. Tear film analysis revealed the existence of severe LSCD with dry eye disease (extensive ocular surface damage due to chemical injury produces LSCD with associated damage to goblet cells and accessory lacrimal glands of the conjunctiva coupled with surface irregularities and can interfere with the normal tear film anatomy)[22] in five (45.45%) patients at the time of presentation.
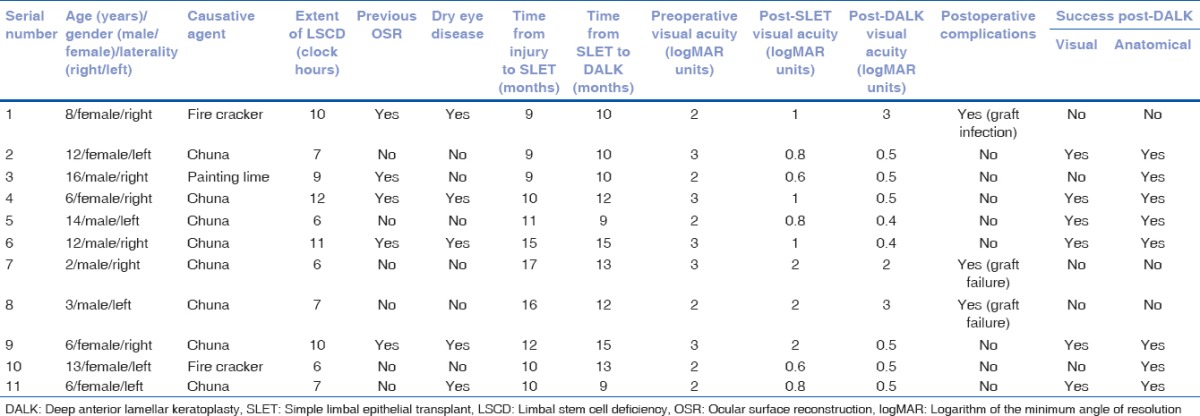
Table 1.
Demographic data of patients who underwent deep anterior lamellar keratoplasty following simple limbal epithelial transplant procedure for unilateral chemical injury
Nine of the 11 eyes (81.82%) had stable and improved ocular surface after SLET with no conjunctivalization over visual axis and no goblet cells over central cornea with better tear film distribution. Anatomical success (defined as no recurrence or <2 clock hours of keratolimbal vascularization or conjunctivalization confirmed by impression cytology of the corneal epithelium) was seen in nine (81.82%) out of eleven patients whereas failure (defined as recurrence of >2 clock hours of keratolimbal vascularization or conjunctivalization with graft opacification confirmed by impression cytology of corneal epithelium for the presence of goblet cells) of the autologous SLET occurred in 2 (18.18%) patients and required a repeated procedure for ocular surface reconstruction. Focal recurrences of mild keratolimbal conjunctivalization/vascularization of 1–1.5 clock hours were seen to occur in nine patients. These areas were managed by simple observation only, and no interventions were done for these areas as the patients did not consent for custom SLET procedures. These focal recurrences were noted to be nonprogressive and did not encroach into the visual axis.[23] Visual success defined as an improvement by ≥2 lines was noted in seven patients (63.63%) and four patients (36.36%) had either no improvement or improvement by one line only. The BCVA after SLET was 1.17 ± 0.54 logMAR units. No complication in terms of ocular surface infection was seen in any of the cases. Out of the 11 cases, 9 had mid-to-deep stromal involvement with visual axis opacification and 2 patients had deeper involvement of varying degrees which was not involving the visual axis. DALK was subsequently performed after a mean duration of 11.63 ± 2.21 months (9–15 months) following the SLET procedure. All 11 eyes underwent a successful manual DALK procedure with no immediate postoperative complication [Fig. 2]. One patient had an intraoperative perforation in the paracentral region of thinning which was managed intraoperatively with careful dissection aided by intraoperative optical coherence tomography-aided surgery and the DALK was successfully completed. No postoperative Descemet's detachment or double chamber was observed in any of our cases. Following DALK procedure, epithelial healing time was noted to be an average of 10.8 ± 2.9 days [Fig. 3]. The defect healed in <4 days in three patients and took more than 4 days in eight patients. Anatomical success was seen in eight (72.72%) out of eleven eyes, whereas failure of the graft occurred in three (27.27%) eyes. Primary graft failure was not seen in any of the 11 cases of DALK. Secondary graft failure was seen in three DALK grafts. Secondary graft failure was due to graft infection (1), presumed graft rejection (1), and compromised host endothelium (1). The latter two (18.18%) patients had vascularization and opacification of the graft with a graft clarity of zero at 6 months follow-up period, of which one patient needed a repeat full-thickness graft and the others needed a repeat lamellar graft. Acute graft rejection was not noted in our series, but we presume that one of the graft failures which required a penetrating keratoplasty was a failure due to graft rejection as the patient was not compliant to regular follow-up. Graft infection was noted in one patient at 5-month follow-up period, and a therapeutic graft replacement was done as the infection was limited to the donor graft [Fig. 4] The graft survival probability was 75% at 6-month follow-up period, which remained the same at the last follow-up [Fig. 5]. Patients were followed up for a mean duration of 13.00 ± 4.58 months (6–18 months) after the DALK procedure. The mean BCVA after DALK was 0.6 ± 0.2 logMAR units. Eight (72.72%) out of 11 patients had a vision of ≥0.5 logMAR units at 6-month follow-up and three patients (27.27%) had BCVA of ≤1 logMAR units. Visual success defined as improvement by ≥2 lines was noted in six patients (54.54%) and five patients (45.45%) had either no improvement or improvement by one line only.
Figure 2.
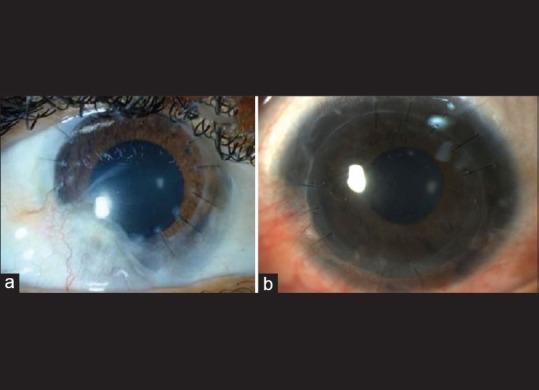
(a) 8 months post-operative DALK with focal area of recurrence (b) More than 6-month postoperative deep anterior lamellar keratoplasty
Figure 3.
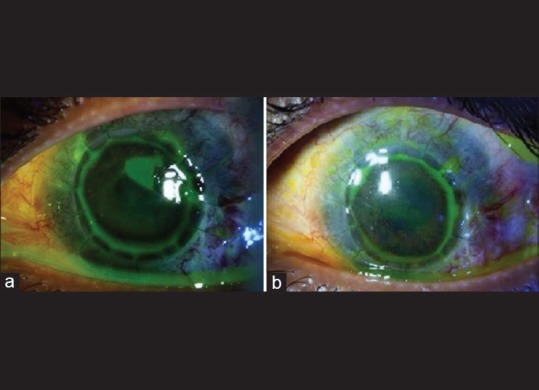
(a) Epithelial defect at day 6 postdeep anterior lamellar keratoplasty. (b) Complete healing of the epithelial defect at day 10 postdeep anterior lamellar keratoplasty
Figure 4.
Graft infection post deep anterior lamellar keratoplasty
Figure 5.
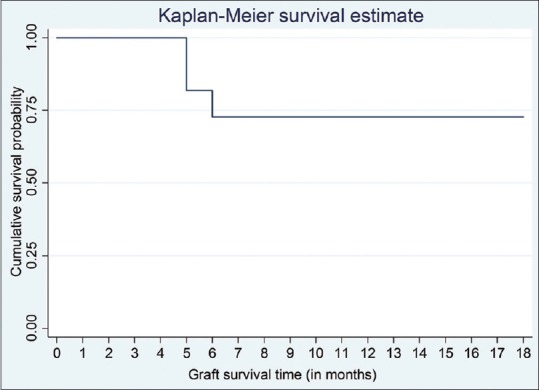
Kaplan–Meier survival probability for post simple limbal epithelial transplant deep anterior lamellar keratoplasty graft
On Spearman's rank correlation test, no significant correlation seen between the BCVA at presentation with post-SLET BCVA (R = 0.5023, P = 0.115) and post-DALK BCVA (R = 0.1190, P = 0.727); however, a strong correlation was seen between the post-SLET BCVA and post-DALK BCVA (R = 0.7914, P = 0.003). There was no significant correlation seen between the post-DALK BCVA with the preoperative grade of chemical injury based on the involvement of limbal clock hours (R = 0.1053, P = 0.7581).
Discussion
Chemical injuries remain one of the leading causes of ocular morbidity in children in the Indian population and cause significant ocular surface damage leading to blindness. Keratoplasties were not successful in such cases, and stem cell transplantation seems to be a viable option for ocular surface rehabilitation in such cases.[2,9,10]
Limbal transplantation is performed in such cases to establish the barrier function of limbal stem cells and to replenish the corneal epithelial cells for stable and healthy ocular surface.[8,12,13] Combined LSCT (Limbal cell transplantation with penetrating keratoplasty) has been described but has shown higher risk of graft rejection.[14] Hence, in our study, we performed sequential two-staged procedures, wherein keratoplasty was performed only after a stable and noninflamed ocular surface was achieved after autologous SLET. In our study, chuna packet injury was the most common mode of chemical injury in children. One of our cases had graft infection which was attributable to the younger age of the patient, poor compliance to follow-up, and probably a higher rate of ocular microbial flora affection in these compromised ocular surfaces. Poor ocular surface, delayed healing of the epithelial defect, and poor hygiene can also result in higher postkeratoplasty morbidity in these eyes with compromised ocular surfaces.[7,9] We also had to wait for a period of time longer than 6 months (11.63 ± 2.21 months) for the ocular surface stabilization and inflammation control before we could consider DALK in these severely injured eyes.
The anatomic and visual outcomes in the pediatric age group are different from those of adults owing to the increased amount of inflammatory response associated with any type of injury.[7,8] There is a paucity of literature on outcomes of lamellar keratoplasty following limbal transplantation in pediatric age group, so we wished to study the outcomes of lamellar keratoplasty after SLET in severe cases of ocular chemical injury sequelae. Pediatric cases of chemical injury are more difficult scenarios due to the requirement of examination under anesthesia for every follow-up visit, review, and assessment and subsequent interventions. Given the poor socioeconomic status of the patients who sustain these ocular chemical injuries, they are also not amenable to refractive rehabilitation with contact lenses following successful SLET procedures. Early surgical intervention for better corneal clarity is also necessitated to prevent amblyopia implications. Hence, we report the outcomes of DALK following SLET procedure in pediatric cases. In our study, we found out the anatomical success in 81.82% and visual success in 63.63% of the children who underwent SLET which is comparable to the previous study by Basu et al. which evaluated the long-term clinical outcomes of SLET and reported a survival probability of 72% in children.[8] The previous study was done at our center which evaluated and compared the outcomes of CLET in children and adults reported the anatomical success in 87.8% and visual success in 78.7% of children.[7]
Post-DALK, poorer outcomes in pediatric age group as compared to the adults might be attributed to the inadequate hygienic precautions, poor compliance to medications, difficulty of examining the children properly, suture-related complications, and amblyopic stimulus due to sensory visual loss related to corneal involvement.[7,9] These factors could also lead to suboptimal visual outcomes as compared to the anatomical outcomes. However, in our study, we did not find any significant difference between the anatomical and visual outcomes post-DALK (P = 0.565) which could be explained by the fact that the mean age of the children in our study was 8.9 ± 4.7 years and most of the children were beyond the amblyogenic age group. In our study, the graft success was seen in 72.72% cases at 6-month follow-up period which was slightly more than the survival of the graft after penetrating keratoplasty following cultivated LSCT in a previous study done by Basu et al.[17] Visual success was seen in 72.72% cases which was comparable to the visual outcomes following penetrating keratoplasty after LSCT in a previous study done by Basu et al.[17]
In addition to the above factors, the duration between the ocular injury and visual rehabilitation surgeries also forms an important parameter in determining the anatomical and visual success after keratoplasty.[7] Persistent inflammation in pediatric age group might cause a delay between the ocular injury and visual rehabilitation surgeries, thereby leading to suboptimal outcomes.[7,9] One of the important concerns in performing DALK in pediatric eyes post-SLET ocular surface reconstruction includes the timing of surgery. An optimal interval between the SLET procedure and DALK is desirable to control the ocular surface inflammation which might be vital to the success of the subsequent lamellar procedure of the cornea. However, in view of the danger of amblyopia, an earlier DALK intervention is usually preferred. This aspect needs to be considered and frequent follow-up with longer topical steroid therapy might be mandated. The risk of graft infection in these compromised ocular surfaces also needs to be considered.[17,23] However, in our study, we did not find any significant correlation of the duration between ocular chemical injury and SLET with post-SLET BCVA (R = 0.512, P = 0.107) or with post-DALK BCVA (R = 0.243, P = 0.47). Furthermore, the correlation of the duration between SLET and DALK with post-DALK BCVA was not statistically significant (R = −0.0215, P = 0.95).
As the scope of this study was to analyze the outcomes of DALK in postautologous SLET scenario of pediatric eyes, the limiting factor of a small sample size precludes more elaborate comparative analysis with outcomes in adult cases, cases with penetrating keratoplasty, and long-term survival analysis, for which a larger study sample done prospectively would be more optimal.
DALK procedure in these cases was found to be technically more challenging as these patients had thinner corneas, poor visibility, superficial vascularization over corneas which lead to intraoperative and postoperative bleeding, and high chances of perforation. Therefore we recommend a layer-by-layer technique of manual dissection of host bed in such cases till the clear area is seen. None of the cases required a conversion to penetrating keratoplasty due to intraoperative perforation and no postoperative complication in terms of double chambers or Descemet's membrane detachment was noted in any of our case.
This highlights the importance of stepwise sequential approach in cases of ocular chemical burns in pediatric age group, in which ocular surface reconstruction by SLET is followed by lamellar keratoplasty. Furthermore, a more frequent and a thorough follow-up period is essential to get better anatomical and visual outcomes in children. Simple limbal epithelial transplantation has promising results in ocular surface stabilization in uniocular chemical injuries, and once the ocular surface becomes stable, the lamellar keratoplasty may be performed as early as possible to avoid the risk of amblyopia and poorer anatomical and visual outcomes in pediatric age group. However, further prospective trials with larger sample size are required to evaluate long-term results to study the problems of higher susceptibility to graft infection and long-term visual outcomes in these eyes with compromised ocular surfaces.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Dua HS, King AJ, Joseph A. A new classification of ocular surface burns. Br J Ophthalmol. 2001;85:1379–83. doi: 10.1136/bjo.85.11.1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vazirani J, Mariappan I, Ramamurthy S, Fatima S, Basu S, Sangwan VS. Surgical management of bilateral limbal stem cell deficiency. Ocul Surf. 2016;14:350–64. doi: 10.1016/j.jtos.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 3.Dua HS, Azuara-Blanco A. Limbal stem cells of the corneal epithelium. Surv Ophthalmol. 2000;44:415–25. doi: 10.1016/s0039-6257(00)00109-0. [DOI] [PubMed] [Google Scholar]
- 4.Dua HS, Miri A, Alomar T, Yeung AM, Said DG. The role of limbal stem cells in corneal epithelial maintenance: Testing the dogma. Ophthalmology. 2009;116:856–63. doi: 10.1016/j.ophtha.2008.12.017. [DOI] [PubMed] [Google Scholar]
- 5.Gheorghe A, Pop M, Mrini F, Barac R, Vargau I. Ocular surface reconstruction in limbal stem cell deficiency. Rom J Ophthalmol. 2016;60:2–5. [PMC free article] [PubMed] [Google Scholar]
- 6.Haagdorens M, Van Acker SI, Van Gerwen V, Ní Dhubhghaill S, Koppen C, Tassignon MJ, et al. Limbal stem cell deficiency: Current treatment options and emerging therapies. Stem Cells Int. 2016;2016:9798374. doi: 10.1155/2016/9798374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ganger A, Vanathi M, Mohanty S, Tandon R. Long-term outcomes of cultivated limbal epithelial transplantation: Evaluation and comparison of results in children and adults. Biomed Res Int. 2015;2015:480983. doi: 10.1155/2015/480983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Basu S, Sureka SP, Shanbhag SS, Kethiri AR, Singh V, Sangwan VS. Simple limbal epithelial transplantation: Long-term clinical outcomes in 125 cases of unilateral chronic ocular surface burns. Ophthalmology. 2016;123:1000–10. doi: 10.1016/j.ophtha.2015.12.042. [DOI] [PubMed] [Google Scholar]
- 9.Sejpal K, Ali MH, Maddileti S, Basu S, Ramappa M, Kekunnaya R, et al. Cultivated limbal epithelial transplantation in children with ocular surface burns. JAMA Ophthalmol. 2013;131:731–6. doi: 10.1001/jamaophthalmol.2013.2308. [DOI] [PubMed] [Google Scholar]
- 10.Holland EJ. Management of limbal stem cell deficiency: A historical perspective, past, present, and future. Cornea. 2015;34(Suppl 10):S9–15. doi: 10.1097/ICO.0000000000000534. [DOI] [PubMed] [Google Scholar]
- 11.Sharma S, Tandon R, Mohanty S, Sharma N, Vanathi M, Sen S, et al. Culture of corneal limbal epithelial stem cells: Experience from benchtop to bedside in a tertiary care hospital in India. Cornea. 2011;30:1223–32. doi: 10.1097/ICO.0b013e3181dc81f1. [DOI] [PubMed] [Google Scholar]
- 12.Sangwan VS, Basu S, MacNeil S, Balasubramanian D. Simple limbal epithelial transplantation (SLET): A novel surgical technique for the treatment of unilateral limbal stem cell deficiency. Br J Ophthalmol. 2012;96:931–4. doi: 10.1136/bjophthalmol-2011-301164. [DOI] [PubMed] [Google Scholar]
- 13.Mittal V, Jain R, Mittal R, Vashist U, Narang P. Successful management of severe unilateral chemical burns in children using simple limbal epithelial transplantation (SLET) Br J Ophthalmol. 2016;100:1102–8. doi: 10.1136/bjophthalmol-2015-307179. [DOI] [PubMed] [Google Scholar]
- 14.Queiroz AG, Barbosa MM, Santos MS, Barreiro TP, Gomes JÁ. Assessment of surgical outcomes of limbal transplantation using simple limbal epithelial transplantation technique in patients with total unilateral limbal deficiency. Arq Bras Oftalmol. 2016;79:116–8. doi: 10.5935/0004-2749.20160034. [DOI] [PubMed] [Google Scholar]
- 15.Vazirani J, Ali MH, Sharma N, Gupta N, Mittal V, Atallah M, et al. Autologous simple limbal epithelial transplantation for unilateral limbal stem cell deficiency: Multicentre results. Br J Ophthalmol. 2016;100:1416–20. doi: 10.1136/bjophthalmol-2015-307348. [DOI] [PubMed] [Google Scholar]
- 16.Sangwan VS, Matalia HP, Vemuganti GK, Ifthekar G, Fatima A, Singh S, et al. Early results of penetrating keratoplasty after cultivated limbal epithelium transplantation. Arch Ophthalmol. 2005;123:334–40. doi: 10.1001/archopht.123.3.334. [DOI] [PubMed] [Google Scholar]
- 17.Basu S, Mohamed A, Chaurasia S, Sejpal K, Vemuganti GK, Sangwan VS. Clinical outcomes of penetrating keratoplasty after autologous cultivated limbal epithelial transplantation for ocular surface burns. Am J Ophthalmol. 2011;152:917–24.e1. doi: 10.1016/j.ajo.2011.05.019. [DOI] [PubMed] [Google Scholar]
- 18.Toor GS, Basu S, MacNeil S, Sangwan VS. Successful deep anterior lamellar keratoplasty following multiple failed limbal transplantations for chronic ocular burns. BMJ Case Rep 2012. 2012:pii: Bcr2012006774. doi: 10.1136/bcr-2012-006774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ashar JN, Pahuja S, Ramappa M, Vaddavalli PK, Chaurasia S, Garg P. Deep anterior lamellar keratoplasty in children. Am J Ophthalmol. 2013;155:570–4.e1. doi: 10.1016/j.ajo.2012.09.029. [DOI] [PubMed] [Google Scholar]
- 20.Sharma S, Tandon R, Mohanty S, Kashyap S, Vanathi M. Phenotypic evaluation of severely damaged ocular surface after reconstruction by cultured limbal epithelial cell transplantation. Ophthalmic Res. 2013;50:59–64. doi: 10.1159/000346868. [DOI] [PubMed] [Google Scholar]
- 21.Fogla R, Padmanabhan P. Deep anterior lamellar keratoplasty combined with autologous limbal stem cell transplantation in unilateral severe chemical injury. Cornea. 2005;24:421–5. doi: 10.1097/01.ico.0000151550.51556.2d. [DOI] [PubMed] [Google Scholar]
- 22.Eslani M, Baradaran-Rafii A, Movahedan A, Djalilian AR. The ocular surface chemical burns. J Ophthalmol. 2014;2014:9. doi: 10.1155/2014/196827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vazirani J, Lal I, Sangwan V. Customised simple limbal epithelial transplantation for recurrent limbal stem cell deficiency. BMJ Case Rep 2015. 2015:pii: Bcr2015209429. doi: 10.1136/bcr-2015-209429. [DOI] [PMC free article] [PubMed] [Google Scholar]


