Introduction
Internuclear ophthalmoplegia (INO) is caused by lesions in the medial longitudinal fasciculus (MLF), and is classically characterized by paresis of adduction on lateral gaze associated with nystagmus on abduction of the contralateral eye.[1]
We present a case of traumatic bilateral INO as an isolated sequela after closed head injury that completely resolved within 7 days.
Case Report
A 35-year-old male presented to the emergency department (ED) after a traffic accident. The patient had a frontal scalp laceration, brief loss of consciousness with retrograde amnesia, headache, and dizziness. There was no evidence of ocular or periorbital trauma. Initially, brain computed tomography performed in the ED revealed no specific finding. After regaining full consciousness, the patient complained of diplopia. He was admitted to the Department of Neurosurgery for observation, and no neurologic abnormalities were found. The patient was then referred for ophthalmologic evaluation, with the primary complaint of diplopia. The best-corrected visual acuity was 20/25 in the right eye and 20/20 in the left eye. The intraocular pressure was 11 mmHg in the right eye and 14 mmHg in the left eye. The pupillary response and slit lamp examination were normal. Ocular motility examination revealed restricted horizontal movement during lateral gaze in both eyes [Fig. 1]. The patient had an adduction deficit in the right eye and nystagmus in the left eye on leftward gaze. He also had an adduction deficit in the left eye and nystagmus in the right eye on rightward gaze. Upward and downward gaze were unremarkable.
Figure 1.
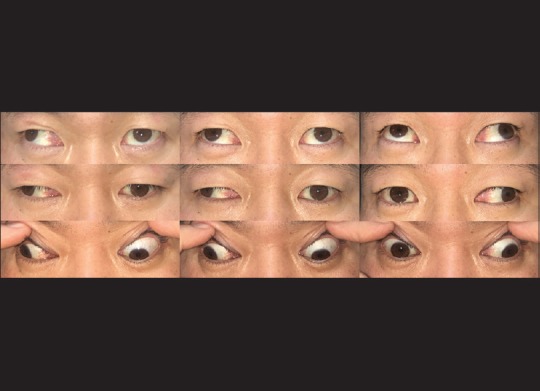
Patient was profoundly exotropic in primary position. On attempted right lateral gaze, the left eye failed to adduct across the midline. When the patient looked to the left, the right eye did not cross the midline
Magnetic resonance imaging of the brain was performed 2 days after injury and small focus of hemorrhage was found at the pontomesencephalic junction. Subsequent evaluation with susceptibility-weighted imaging definitely revealed a tiny hemorrhage [Fig. 2]. Seven days after the accident, his versions were completely normal [Fig. 3] and he had no subjective complaint of diplopia.
Figure 2.
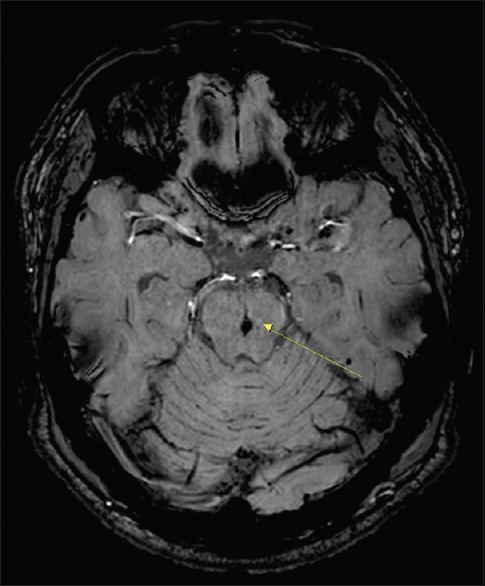
Susceptibility-weighted imaging. The arrow indicates signal changes in the pontomesencephalic junction
Figure 3.

Seven days after the accident, the versions were completely normal
Discussion
Internuclear ophthalmoplegia is characterized by impaired horizontal eye movement that is caused by a lesion in the MLF, a fiber tract that rises from the abducens nucleus in the pons to the contralateral oculomotor nucleus in the midbrain.[1] There are two possible causes of traumatic MLF lesions: Shear force within the brain stem may either stretch the perforating branches of the basilar artery and lead to ischemia,[2] or may stretch the MLF fiber tract itself.[3] Prognosis of traumatic INO is usually good, and most traumatic INO spontaneously resolves. The time to recovery of MLF function ranges between 48 h[4] and 1 year after the injury in the reported cases.[5] This patient recovered function of MLF within 7 days after the accident.
Conclusion
This case illustrates that minor head trauma can result in a discrete pontine hemorrhage manifesting as bilateral INO. Although isolated INO is rarely developed, INO should be considered in the differential diagnosis when one encounters an adduction deficit in a recently traumatized patient.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cogan DG, Kubik CS, Smith WL. Unilateral internuclear ophthalmoplegia; report of 8 clinical cases with one postmortem study. AMA Arch Ophthalmol. 1950;44:783–96. [PubMed] [Google Scholar]
- 2.Rich JR, Gregorius FK, Hepler RS. Bilateral internuclear ophthalmoplegia after trauma. Arch Ophthalmol. 1974;92:66–8. doi: 10.1001/archopht.1974.01010010070017. [DOI] [PubMed] [Google Scholar]
- 3.Devereaux MW, Brust JC, Keane JR. Internuclear ophthalmoplegia caused by subdural hematoma. Neurology. 1979;29:251–5. doi: 10.1212/wnl.29.2.251. [DOI] [PubMed] [Google Scholar]
- 4.Baker RS. Internuclear ophthalmoplegia following head injury. Case report. J Neurosurg. 1979;51:552–5. doi: 10.3171/jns.1979.51.4.0552. [DOI] [PubMed] [Google Scholar]
- 5.Constantoyannis C, Tzortzidis F, Papadakis N. Internuclear ophthalmoplegia following minor head injury: A case report. Br J Neurosurg. 1998;12:377–9. doi: 10.1080/02688699844943. [DOI] [PubMed] [Google Scholar]


