Abstract
Context and Objective:
Simvastatin is a widely used cholesterol-lowering drug, which has been found to have a number of pleiotropic effects. The aim of this study was to evaluate the antimicrobial effectiveness of simvastatin against selected oral streptococci as determined by the minimum inhibitory concentration (MIC).
Methods:
Streptococcus mutans, Streptococcus sanguis, Streptococcus anginosus, and Streptococcus salivarius were the test microorganisms. The serial dilution method was used to determine the MIC of simvastatin against these organisms. The MIC was defined as the lowest concentration of simvastatin that completely inhibited growth of the test organisms.
Results:
The data indicate that simvastatin inhibits the growth of the test organisms, with MIC's ranging from 7.8 to 15.6 μg/ml.
Conclusions:
Simvastatin has MIC's against the selected bacteria that compare favorably with reported values for topical agents such as essential oil, chlorhexidine gluconate, and triclosan. The levels of simvastatin required to inhibit bacterial growth of oral bacteria exceed the reported levels of the drug found in plasma or crevicular fluid of patients who are treated with this cholesterol-lowering drug. However, clinical studies are warranted to investigate the potential use of simvastatin as a novel antiplaque agent that could be used in local drug delivery to the oral cavity of those patients who are prescribed this cholesterol-lowering drug.
Keywords: Bacteriostatic, simvastatin, streptococci
Introduction
Cardiovascular disease (CVD), including heart attack, angina, and stroke, is ranked as the number one cause of mortality worldwide.[1] High blood cholesterol is linked to CVD.[2] Statins, cholesterol-lowering drugs, are first choice drugs for reducing the chance of suffering a CVD event.
A number of unintended side effects of statins have been reported.[3] Although not thought of traditionally as antimicrobials, statins have been shown to have antimicrobial effects.[4] Hence, the aim of this study was to assess the in vitro efficacy of simvastatin against selected strains of oral streptococci as determined by the minimum inhibitory concentration (MIC).
Methods
Bacterial strains
Streptococcus mutans (25,175), Streptococcus anginosus (33,397), Streptococcus sanguis (10,556), and Streptococcus salivarius (2593) were purchased from the American Type Culture Collection (Manassas, VA, USA). All streptococci were inoculated in/on brain heart infusion (BHI) broth/agar and grown at 37°C in anaerobic jars in an atmosphere of carbon dioxide. The concentration of log phase cells that were used was between 108 and 1010 colony-forming unit (CFU)/ml as determined by serial plating.
Preparation of simvastatin
Simvastatin (5 mg, Sigma Chemical Co., St. Louis, Mo., USA) was solubilized in 100% dimethyl sulfoxide (DMSO) resulting in a 12 mM solution, and then diluted 1:2 in eight steps with DMSO to make stock solutions ranging from 6 mM to 24.7 nM.
Determination of minimum inhibitory concentration by broth dilution assay
For bacterial growth studies, 75 μl of each simvastatin/DMSO solution was used. To this, a fixed culture of bacteria (75 μl bacterial suspension, OD 600 nm = 1.5, 1010–1012 CFU/ml) and 2.85 ml media were added to obtain a final volume of 3 ml. The final concentration of DMSO in each experimental tube was 2.5%. DMSO alone (75 μl), added to bacterial suspension (75 μl) and media (2.85 ml), was used as control. Growth curves were generated for each tube by removing 100 μl samples, adding 900 μl clear media, and measuring turbidity on a spectrophotometer at 600 nm. The MIC was considered to be the lowest concentration of simvastatin that prevented bacterial growth, i.e., a clear test tube.[5] Each clear experimental tube was subsequently subcultured onto agar plates and the plates were incubated for 24 h to determine minimum bactericidal concentration (MBC) of simvastatin. Experiments were repeated three times for each bacterial species.
Growth curve determination of bacteriostatic action of simvastatin
For each strain of bacteria, growth curves were started by adding a fixed culture of bacteria (150 μl bacterial suspension, OD 600 nm = 1.5) to 5.7 ml of BHI media. Growth was monitored by measuring the increase in turbidity on a spectrophotometer (OD = 600 nm). After 3 h, simvastatin was added at its MIC, and turbidity was measured for another 6 h. At the end of this time (9 h. total incubation), the cells were pelleted in sterile Eppendorf tubes, washed twice in sterile isotonic saline, and transferred back into sterile BHI (6 ml). The turbidity was measured for another 15 h (24 h total). Growth curves were generated without simvastatin to serve as control. Experiments were repeated three times for each bacterial species.
Results
Determination of minimum inhibitory concentration by broth dilution assay
Growth curves for S. anginosus in the presence of simvastatin are shown in Figure 1. Similar curves were generated for the other streptococci (data not shown). The MIC of simvastatin against the selected oral bacteria was determined to be 37.5 μM (15.6 μg/ml) for S. mutans and S. sanguis and 18.75 μM (7.8 μg/ml) for S. anginsous and S. salivarius. However, the minimum bactericidal activity was not determined by subculture since aliquots (100 μl) from clear culture tubes showed bacterial growth when streaked onto agar plates and incubated for 24 h. This measure of antibacterial activity indicates that simvastatin is a bacteriostatic antimicrobial agent against these bacteria.
Figure 1.
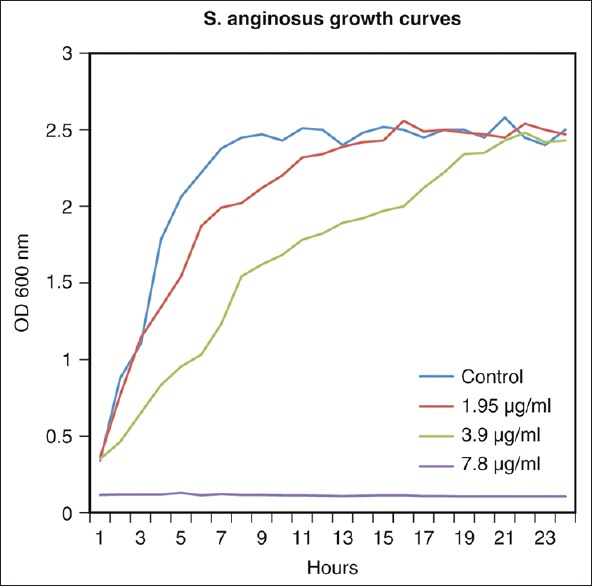
Growth curve of Streptococcus anginosus in the presence of simvastatin: An example of the interference caused by the minimum inhibitory concentration (7.8 μg/ml) and at two concentrations (3.95 and 1.98 μg/ml) below the minimum inhibitory concentration
Growth curve determination of bacteriostatic action of simvastatin
When MIC concentrations of simvastatin were added to growing bacterial cultures, slowed growth rates were observed as compared to control growth curves. However, when the simvastatin-treated bacteria were washed and transferred to growth medium lacking simvastatin, they resumed growth [Figure 2]. This measure of antibacterial activity confirms that simvastatin is a bacteriostatic antimicrobial agent against these strains of bacteria.
Figure 2.
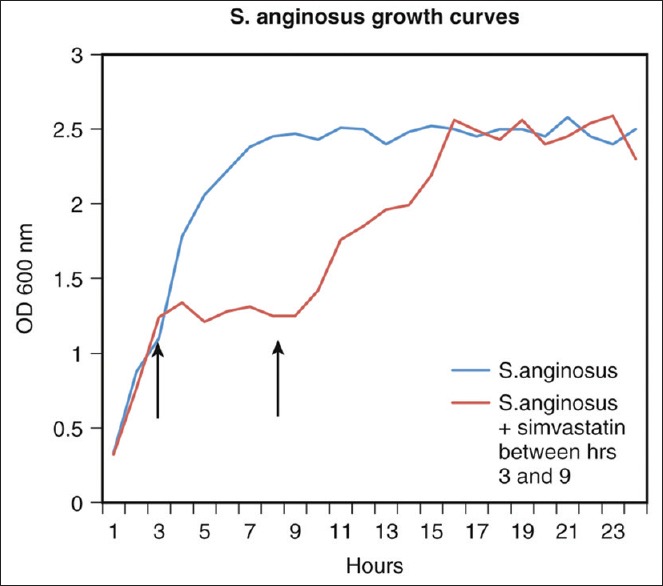
Effect of minimum inhibitory concentration of simvastatin on growth curve of Streptococcus anginosus. Simvastatin (minimum inhibitory concentration = 7.8 μg/ml) added to log phase (left arrow) inhibited growth of the bacteria; removal of simvastatin (right arrow) allowed bacteria to resume growth, thus confirming bacteriostatic effect of simvastatin
Discussion
Statins, cholesterol-lowering drugs, are first choice drugs for reducing the chance of suffering a CVD event. Statins inhibit 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase leading to decreased synthesis of endogenous cholesterol.[6] HMG-CoA reductase is a rate-limiting enzyme in the human mevalonate pathway, an important cellular metabolic pathway present in all higher eukaryotes and many bacteria.[7] The bacteria used in this study possess the gene for HMG-CoA reductase.[8] Statins also have a range of cholesterol independent results, including anti-inflammatory functions[9,10] and antimicrobial activity.[11] Statins inhibit several clinical isolates of methicillin-resistant Staphylococcus aureus, vancomycin-resistant enterococci, Escherichia coli, Porphyromonas gingivalis, and Aggregatibacter actinomycetemcomitans in vitro.[12,13] Likewise, there is some evidence that statins may aid in treating a range of other bacterial infections.[14]
Although the exact mechanism by which simvastatin inhibits the growth of these streptococci is unknown, it is possible that it inhibits bacterial HMG-CoA reductase. There are two distinct classes of HMG-CoA reductase enzymes, the human or eukaryotic Class I enzyme and the prokaryotic Class II enzyme.[15] Crystal structures of a representative of each class of the enzyme have been determined, the Class I human enzyme[7] and the Class II enzyme from Pseudomonas mevalonii.[16] The enzymes are not identical, having different crystal structure, and they react differently to statins.[17] The Class II enzymes are not as easily inhibited by statin drugs, requiring a thousand-fold higher concentration of statins than the Class I enzymes.[18]
These experiments demonstrate the in vitro bacteriostatic effect of simvastatin on S. mutans, S. anginsosus, S. sanguis, and S. salivarius.
Only data for S. anginosus were presented in the figures, but similar results were obtained for the other bacteria, all of which are potentially pathogenic. Oral streptococci of the S. anginosus group are frequently found in abscesses.[19] S. mutans, in addition to being the primary causal agent responsible for dental caries,[20] is commonly found in coronary plaque specimens.[21] Along with S. mutans, S. salivarius and S. sanguis belong to the viridans group streptococci, common etiologic agents of subacute bacterial endocarditis.[22]
Simvastatin has in vitro efficacy against the specific strains of bacteria used in this study at concentrations slightly less than the observed MIC's of 15.6–7.8 μg/ml, i.e., slowed growth curves were observed down to approximately 1.0 μg/ml. DMSO, a cryopreservative agent routinely used in microbiology, was used to solubilize simvastatin and had no effect on bacterial growth.[23] The MBC could not be determined because the simvastatin/DMSO combination became insoluble at concentrations higher than 4–5 times the MIC. Routinely, the MBC of bacteriostatic agents is many-fold higher than their MIC.[24] At its MIC, simvastatin prevents the growth of the tested bacteria but does not kill them. As this study was conducted using in vitro treatment of planktonic cells, it is not clear whether similar effects would be seen in vivo insofar as the bacteria would be contained within a biofilm. Studies are underway to assess the effect of statins on bacteria in a biofilm.
Simvastatin is one of the mainstays of treatment for controlling hyperlipidemia. Other statins, for example, rosuvastatin, pravastatin, lovastatin, fluvastatin, and atorvastatin, are available commercially, each having different pharmacokinetic properties. Only simvastatin was used in this study. Simvastatin is an inactive lactone prodrug which is reversibly converted to a competitive inhibitor of HMG-CoA reductase, simvastatic acid, in the gut wall and other tissues.[25] The bioavailability of simvastatin is <5%, and its half-life is 2–5 h.[26] Thus, for the average adult who has 5 L of blood and ingests one single dose of 60 mg simvastatin, the active metabolite reaches its peak plasma concentration of 0.6 μg/ml several hours later. Thus, these experiments indicate that simvastatin concentrations needed for in vitro antimicrobial inhibition (1.95–15.6 μg/ml MIC) slightly exceed the concentration present in human blood or crevicular fluid during statin treatment (0.6 μg/ml). This would imply that there is no relevant antibacterial effect of statins at concentrations attained in plasma or crevicular fluid. However, the results of in vitro studies are difficult to translate directly into clinical practice. MIC values are laboratory measures of a fixed concentration of an antibacterial agent being tested against an initially fixed concentration of bacteria that does not necessarily correspond to bacterial densities at site of infection. Clinical studies are warranted. Nevertheless, since the MIC is a measure of the potency of an antibacterial drug, simvastatin is less potent than either penicillin or amoxicillin (MIC 0.03–0.06 μg/ml) against oral streptococci.[27,28]
Statins have the potential to benefit oral health when locally delivered. In a clinical trial, Pradeep and Thorat[29] reported greater increase in clinical attachment and greater decrease in gingival index and probing depth at chronic periodontitis sites treated nonsurgically with scaling and root planing and locally delivered simvastatin, compared to scaling and root planing plus placebo in humans. Likewise, another clinical study utilizing topical application of simvastatin in the treatment of chronic periodontitis, indicated that scaling and root planning in the presence of a simvastatin gel significantly inhibited pro-inflammatory cytokines in crevicular fluid.[30] To date, there are no clinical studies relating simvastatin to reduced dental caries. However, although it has been widely used for its systemic hypolipidemic effect, it has not been considered as a topical antimicrobial agent. It is well known that dental caries is associated with microbial biofilm, of which streptococci are important members in both health and disease.[31] Dentists recommend the regular removal of this film on the teeth as the best treatment for preventing both dental caries and periodontal disease. However, it is appreciated by practicing dentists that most people have difficulty in accomplishing effective oral hygiene. Thus, any agent that adds even temporary stasis of biofilm formation could be a complementary method of plaque control, thus altering the disease process. The practical implications of the present study are that it would be a great advantage, for those prescribed simvastatin, to have this drug simultaneously help both systemically and locally in the oral cavity. This could be accomplished by having statin users chew, swish, and swallow, which is feasible since the drug is suitable to mucous membrane, odorless, tasteless, and does not alter taste perception.[32]
As a bacteriostatic agent, simvastatin may act synergistically with other plaque control agents and thus work in localized adjunctive therapy. It has been used in this way to eradicate Helicobacter pylori in patients receiving triple therapy for the treatment of peptic ulcer.[33] Bacteriostatic agents are often as effective as bactericidal agents in the treatment of Gram-positive infections in patients with uncomplicated infections and noncompromised immune systems.[34] Thus, simvastatin may prove to be a good candidate for a therapeutic agent to be used in local drug delivery to target oral bacteria.[35] In this regard, the MIC of simvastatin against oral bacteria compares favorably with essential oil (MIC 512 μg/ml),[36] chlorhexidine gluconate (MIC 1–2 μg/ml),[36] and triclosan (MIC 7.8 μg/ml).[37] These in vitro findings add to the existing evidence[38] that simvastatin has potential use as a novel antiplaque agent.
Conclusions
This study demonstrates the in vitro antimicrobial effect of simvastatin on streptococci commonly found in the mouth. Simvastatin has efficacy against these specific strains of bacteria at concentrations slightly less than the observed MIC's of 15.6–7.8 μg/ml, which compares favorably with reported values for topical agents such as essential oil, chlorhexidine gluconate, and triclosan. For patients who are prescribed simvastatin, this drug may act synergistically with other plaque control agents and thus work in localized adjunctive therapy if chewed and swished orally before swallowing.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, et al. Writing Group Members. Heart disease and stroke statistics-2016 update: A report from the American Heart Association. Circulation. 2016;133:e38–360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 2.Taylor F, Huffman MD, Macedo AF, Moore TH, Burke M, Davey Smith G, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2013;1:CD004816. doi: 10.1002/14651858.CD004816.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Macedo AF, Taylor FC, Casas JP, Adler A, Prieto-Merino D, Ebrahim S. Unintended effects of statins from observational studies in the general population: Systematic review and meta-analysis. BMC Med. 2014;12:51. doi: 10.1186/1741-7015-12-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jerwood S, Cohen J. Unexpected antimicrobial effect of statins. J Antimicrob Chemother. 2008;61:362–4. doi: 10.1093/jac/dkm496. [DOI] [PubMed] [Google Scholar]
- 5.NCCLS. Methods for Determining Bactericidal Activity of Antibacterial Agents: Approved Guideline. NCCLS document M-26-A. Wayne, PA, USA: NCCLS; 1999. [Google Scholar]
- 6.Steinberg D. The statins in preventive cardiology. N Engl J Med. 2008;359:1426–7. doi: 10.1056/NEJMp0806479. [DOI] [PubMed] [Google Scholar]
- 7.Istvan ES, Palnitkar M, Buchanan SK, Deisenhofer J. Crystal structure of the catalytic portion of human HMG-CoA reductase: Insights into regulation of activity and catalysis. EMBO J. 2000;19:819–30. doi: 10.1093/emboj/19.5.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilding EI, Brown JR, Bryant AP, Chalker AF, Holmes DJ, Ingraham KA, et al. Identification, evolution, and essentiality of the mevalonate pathway for isopentenyl diphosphate biosynthesis in gram-positive cocci. J Bacteriol. 2000;182:4319–27. doi: 10.1128/jb.182.15.4319-4327.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bonetti PO, Lerman LO, Napoli C, Lerman A. Statin effects beyond lipid lowering – are they clinically relevant? Eur Heart J. 2003;24:225–48. doi: 10.1016/s0195-668x(02)00419-0. [DOI] [PubMed] [Google Scholar]
- 10.Subramanian S, Emami H, Vucic E, Singh P, Vijayakumar J, Fifer KM, et al. High-dose atorvastatin reduces periodontal inflammation: A novel pleiotropic effect of statins. J Am Coll Cardiol. 2013;62:2382–91. doi: 10.1016/j.jacc.2013.08.1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hennessy E, Mooij MJ, Legendre C, Reen FJ, O’Callaghan J, Adams C, et al. Statins inhibit in vitro virulence phenotypes of Pseudomonas aeruginosa. J Antibiot (Tokyo) 2013;66:99–101. doi: 10.1038/ja.2012.95. [DOI] [PubMed] [Google Scholar]
- 12.Masadeh M, Mhaidat N, Alzoubi K, Al-Azzam S, Alnasser Z. Antibacterial activity of statins: A comparative study of atorvastatin, simvastatin, and rosuvastatin. Ann Clin Microbiol Antimicrob. 2012;11:13. doi: 10.1186/1476-0711-11-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Emani S, Gunjiganur GV, Mehta DS. Determination of the antibacterial activity of simvastatin against periodontal pathogens, Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans: An in vitro study. Contemp Clin Dent. 2014;5:377–82. doi: 10.4103/0976-237X.137959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tleyjeh IM, Kashour T, Hakim FA, Zimmerman VA, Erwin PJ, Sutton AJ, et al. Statins for the prevention and treatment of infections: A systematic review and meta-analysis. Arch Intern Med. 2009;169:1658–67. doi: 10.1001/archinternmed.2009.286. [DOI] [PubMed] [Google Scholar]
- 15.Bochar DA, Stauffacher CV, Rodwell VW. Sequence comparisons reveal two classes of 3-hydroxy-3-methylglutaryl coenzyme A reductase. Mol Genet Metab. 1999;66:122–7. doi: 10.1006/mgme.1998.2786. [DOI] [PubMed] [Google Scholar]
- 16.Lawrence CM, Rodwell VW, Stauffacher CV. Crystal structure of Pseudomonas mevalonii HMG-CoA reductase at 3.0 angstrom resolution. Science. 1995;268:1758–62. doi: 10.1126/science.7792601. [DOI] [PubMed] [Google Scholar]
- 17.Bischoff KM. Rodwell VW 3-Hydroxy-3-methylglutaryl-coenzyme A reductase from Haloferax volcanii: Purification, characterization, and expression in Escherichia coli. J Bacteriol. 1996;178:19–23. doi: 10.1128/jb.178.1.19-23.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tabernero L, Rodwell VW, Stauffacher CV. Crystal structure of a statin bound to a class II hydroxymethylglutaryl-CoA reductase. J Biol Chem. 2003;278:19933–8. doi: 10.1074/jbc.M213006200. [DOI] [PubMed] [Google Scholar]
- 19.Asam D, Spellerberg B. Molecular pathogenicity of Streptococcus anginosus. Mol Oral Microbiol. 2014;29:145–55. doi: 10.1111/omi.12056. [DOI] [PubMed] [Google Scholar]
- 20.Loesche WJ. Role of Streptococcus mutans in human dental decay. Microbiol Rev. 1986;50:353–80. doi: 10.1128/mr.50.4.353-380.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nakano K, Nemoto H, Nomura R, Inaba H, Yoshioka H, Taniguchi K, et al. Detection of oral bacteria in cardiovascular specimens. Oral Microbiol Immunol. 2009;24:64–8. doi: 10.1111/j.1399-302X.2008.00479.x. [DOI] [PubMed] [Google Scholar]
- 22.Baddour LM, Wilson WR, Bayer AS, Fowler VG, Jr, Bolger AF, Levison AE, et al. Viridans and subacute endocarditis AHA scientific statement: Infective endocarditis. Circulation. 2005;111:e394–434. doi: 10.1161/CIRCULATIONAHA.105.165564. [DOI] [PubMed] [Google Scholar]
- 23.Matzneller P, Manafi M, Zeitlinger M. Antimicrobial effect of statins: Organic solvents might falsify microbiological testing results. Int J Clin Pharmacol Ther. 2011;49:666–71. doi: 10.5414/cp201581. [DOI] [PubMed] [Google Scholar]
- 24.Levison ME. Pharmacodynamics of antimicrobial drugs. Infect Dis Clin North Am. 2004;18:451–65, vii. doi: 10.1016/j.idc.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 25.Lilja JJ, Kivistö KT, Neuvonen PJ. Grapefruit juice-simvastatin interaction: Effect on serum concentrations of simvastatin, simvastatin acid, and HMG-CoA reductase inhibitors. Clin Pharmacol Ther. 1998;64:477–83. doi: 10.1016/S0009-9236(98)90130-8. [DOI] [PubMed] [Google Scholar]
- 26.Neuvonen PJ, Niemi M, Backman JT. Drug interactions with lipid-lowering drugs: Mechanisms and clinical relevance. Clin Pharmacol Ther. 2006;80:565–81. doi: 10.1016/j.clpt.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 27.Järvinen H, Tenovuo J, Huovinen P. In vitro susceptibility of Streptococcus mutans to chlorhexidine and six other antimicrobial agents. Antimicrob Agents Chemother. 1993;37:1158–9. doi: 10.1128/aac.37.5.1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Castillo A, Liébana J, López E, Baca P, Liébana JM, Liébana MJ, et al. Interference of antibiotics in the growth curves of oral streptococci. Int J Antimicrob Agents. 2006;27:263–6. doi: 10.1016/j.ijantimicag.2005.10.017. [DOI] [PubMed] [Google Scholar]
- 29.Pradeep AR, Thorat MS. Clinical effect of subgingivally delivered simvastatin in the treatment of patients with chronic periodontitis: A randomized clinical trial. J Periodontol. 2010;81:214–22. doi: 10.1902/jop.2009.090429. [DOI] [PubMed] [Google Scholar]
- 30.Grover HS, Kapoor S, Singh A. Effect of topical simvastatin (1.2 mg) on gingival crevicular fluid interleukin-6, interleukin-8 and interleukin-10 levels in chronic periodontitis – A clinicobiochemical study. J Oral Biol Craniofac Res. 2016;6:85–92. doi: 10.1016/j.jobcr.2015.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Marsh PD. Dental plaque as a microbial biofilm. Caries Res. 2004;38:204–11. doi: 10.1159/000077756. [DOI] [PubMed] [Google Scholar]
- 32.Hosny KM, Khames A, Elhady SS. Preparation and evaluation of simvastatin orodispersible tablets containing soy polysaccharide and potassium polacrillin as novel superdisintegrants. Int J Pharm Sci Res. 2013;4:3381–9. [Google Scholar]
- 33.Nseir W, Diab H, Mahamid M, Abu-Elheja O, Samara M, Abid A, et al. Randomised clinical trial: Simvastatin as adjuvant therapy improves significantly the Helicobacter pylori eradication rate – a placebo-controlled study. Aliment Pharmacol Ther. 2012;36:231–8. doi: 10.1111/j.1365-2036.2012.05161.x. [DOI] [PubMed] [Google Scholar]
- 34.Pankey GA, Sabath LD. Clinical relevance of bacteriostatic versus bactericidal mechanisms of action in the treatment of Gram-positive bacterial infections. Clin Infect Dis. 2004;38:864–70. doi: 10.1086/381972. [DOI] [PubMed] [Google Scholar]
- 35.Rosenberg DR, Andrade CX, Chaparro AP, Inostroza CM, Ramirez V, Violant D, et al. Short-term effects of 2% atorvastatin dentifrice as an adjunct to periodontal therapy: A randomized double-masked clinical trial. J Periodontol. 2015;86:623–30. doi: 10.1902/jop.2015.140503. [DOI] [PubMed] [Google Scholar]
- 36.Haffajee AD, Yaskell T, Socransky SS. Antimicrobial effectiveness of an herbal mouthrinse compared with an essential oil and a chlorhexidine mouthrinse. J Am Dent Assoc. 2008;139:606–11. doi: 10.14219/jada.archive.2008.0222. [DOI] [PubMed] [Google Scholar]
- 37.Bedran TB, Grignon L, Spolidorio DP, Grenier D. Subinhibitory concentrations of triclosan promote Streptococcus mutans biofilm formation and adherence to oral epithelial cells. PLoS One. 2014;9:e89059. doi: 10.1371/journal.pone.0089059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Elavarasu S, Suthanthiran TK, Naveen D. Statins: A new era in local drug delivery. J Pharm Bioallied Sci. 2012;4(Suppl 2):S248–51. doi: 10.4103/0975-7406.100225. [DOI] [PMC free article] [PubMed] [Google Scholar]


