Abstract
A multi-center, randomized, double-blind, placebo-controlled study was conducted with 158 subjects who were randomized to placebo or avanafil 50, 100, and 200 mg on demand for 8 weeks to evaluate the safety, tolerability, and efficacy of avanafil in the treatment of erectile dysfunction (ED) in Korean men. The primary outcome was the erectile function (EF) domain score of the International Index of Erectile Function (IIEF) questionnaire. Secondary outcomes included changes in the scores of IIEF questions 3 and 4 (IIEF Q3, Q4) from baseline, changes in all domain scores in the IIEF from baseline, Sexual Encounter Profile questions 2–5 (SEP2–5), the Global Efficacy Assessment Question (GEAQ), and the number of subjects whose EF domain score at the 8th week visit was ≥ 26. After 8 weeks of treatment, the dose groups except avanafil 50 mg scored significantly higher on the IIEF-EF domain from baseline than the placebo group. The changes from baseline in the avanafil group in IIEF Q3 (all doses) and Q4 (200 mg alone) were higher than the placebo group. The differences between avanafil and placebo groups were significant in SEP2 (100 and 200 mg) and SEP3–5 (200 mg). The differences in the GEAQ “Yes” response were also significant in the avanafil 100 and 200 mg groups. Regarding the ratio of normal EF at the end of the study, avanafil 200 mg differed significantly from the placebo. Most treatment-associated adverse events were mild and resolved spontaneously. This is a clinical trial study and was registered at www.ClinicalTrials.gov (Identifier: NCT02477436).
Keywords: Erectile Dysfunction, Phosphodiesterase 5 Inhibitors, Penile Erection
Graphical Abstract
INTRODUCTION
Erectile dysfunction (ED) is defined as a persistent inability to attain and/or maintain an erection for satisfactory sexual intercourse (1). ED can occur for a variety of reasons (2-4). Typically, it can be classified as having a neurogenic, psychogenic, or endocrinologic basis. However, for the most part, reduction of penile blood supply is understood as the most basic mechanism of its development (5).
Oral phosphodiesterase type 5 (PDE5) inhibitors are currently the most widely used drugs and are recommended in the guidelines of various medical associations as the standard initial treatment for ED (6,7). Since the development of sildenafil, several PDE5 inhibitors have been developed and used. Many comparative studies have been conducted on their efficacy, which is generally similar (8). However, because the pharmacokinetic properties of each drug and the specificity for PDE5 isoenzyme differ slightly for each drug, it is also known that the efficacious time period after drug administration and their side effects also differ slightly (9).
When avanafil was developed, it was expected to have a rapid onset time and high selectivity for PDE5. Avanafil is a potent PDE5 inhibitor with a Tmax of 30–45 minutes and a half-life of 3–5 hours (10,11). Avanafil is known to have a higher selectivity for PDE5 than other PDE5 inhibitors. This characteristic of avanafil differs from that of sildenafil, vardenafil, and tadalafil, which all involve some inhibitory activity on other PDE enzymes (PDE1, PDE6, and PDE11) (10,11).
Avanafil also has advantages in terms of its rapid effects after administration. Because it is effective 15–30 minutes after ingestion, it eliminates the inconvenience of patients having to wait a considerable time before attempting sexual intercourse (12). This will alleviate patients' concerns about time and is expected to have positive effects from a psychological point of view, further enhancing the drug's efficacy. Despite these advantages of avanafil, it is the most recently developed PDE5 inhibitor and still lacks comprehensive clinical support. Furthermore, most studies on avanafil have focused on the currently used doses of 100 and 200 mg, so data on the efficacy of 50 mg are lacking (13). Therefore, we evaluated the safety and efficacy of all 3 dose levels of avanafil in Korean men with ED.
MATERIALS AND METHODS
Methods
Study design
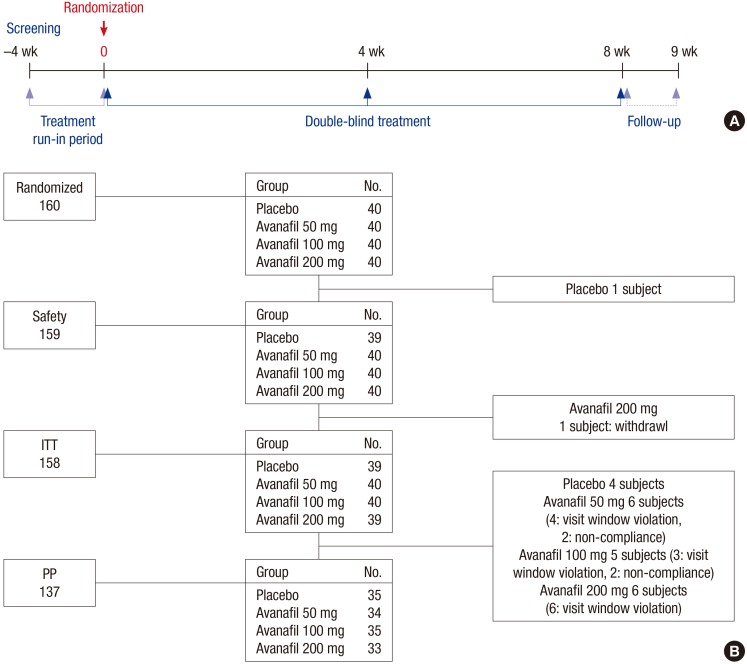
The screening test for the suitability of each subject was performed at least 4 weeks before administration of the investigational product (visit 1). At visit 2, the International Index of Erectile Function (IIEF) (14) was evaluated and the subject's diary, given to each subject at the time of the screening visit, was collected and reviewed. To be enrolled, a subject must have had at least 4 sexual intercourse events, on separate days, and a failure rate over 50% (question 4). Randomization numbers were given to patients who were judged to be suitable for the study, and a 4-week supply of investigational product (avanafil 50, 100, or 200 mg, or placebo) was provided; they were provided with more product on a subsequent visit. Patients were instructed to take the investigational products for 8 weeks on an ‘as needed’ basis, –30 minutes prior to sexual intercourse, and not to exceed one dose per day during the trial. They were also advised to avoid excessive eating and drinking 2 hours before and 2 hours after taking the investigational product (Fig. 1A). During the 8‑week treatment period, patient tolerance and responses to the study drug were assessed by the investigator every 4 weeks (visits 3, 4). Patients who needed a follow-up visit due to safety issues visited the hospital 1 or 2 weeks after the post-therapy visit.
Fig. 1.
Study schedule (A) and patient disposition (B).
ITT = intent-to-treat, PP = per protoccol.
Subjects
Inclusion criteria were: male subject aged 19–70 with history of ED for at least 6 months; a stable, monogamous relationship with a female partner; a partner who was not pregnant or lactating and was using contraception; judged as suitable from the screening test; consent to participate in the clinical study in writing; at least 4 attempts at sexual intercourse on separate days during the 4-week run-in period with a failure rate over 50%; and a score of 11–25 in the EF domain of IIEF during the 4-week run-in period.
Men with the following conditions were excluded from the study: spinal cord injury, radical prostatectomy, anatomical deformity of the penis, ED due to neurogenic or endocrine cause (e.g., hyperprolactinemia, low serum testosterone levels), uncontrolled major psychiatric disorder, significant neurological abnormalities, a history of alcoholism or substance abuse, hepatic dysfunction or renal dysfunction, uncontrollable diabetes, proliferative diabetic retinopathy, stroke, transient ischemic attacks, myocardial infarction, heart failure, unstable angina or fatal arrhythmia, serious hypotension (systolic blood pressure/diastolic blood pressure [SBP/DBP] less than 90/50 mmHg in a sitting position), uncontrollable severe hypertension (SBP/DBP over 170/100 mmHg in a sitting position), hematological disorders, or a serious gastrointestinal (GI) bleeding disorder within 1 year. Subjects were also ineligible if they had been receiving regular treatment with nitrates, anticoagulants (except for low-dose aspirin), androgens, anti-androgens, inhibitor of cytochrome P450 3A4, anticancer chemotherapy, or trazodone. Patients with a history of an anaphylactic reaction to a PDE5 inhibitor, unsuccessful use of a PDE5 inhibitor, or having taken other agent(s) in a clinical trial within 30 days were also excluded. Concomitant use of another ED treatment was forbidden.
Outcome measures
The primary efficacy variable was the change in the EF domain scores of the IIEF questionnaire from baseline, calculated by comparing total scores from questions 1–5 and 15 from the IIEF questionnaire (14).
Secondary efficacy measures included changes in questions 2–5 of the Sexual Encounter Profile (SEP2: Were you able to insert your penis into your partner's vagina?; SEP3: Did your erection last long enough for you to have successful intercourse?; SEP4: Were you satisfied with the hardness of your erection?; SEP5: Were you satisfied overall with this sexual experience) from baseline, changes in other domain scores of the IIEF from baseline, change in scores of the IIEF questions 3 and 4 (IIEF Q3, Q4) from baseline, patient responses to the Global Efficacy Assessment Question (GEAQ: Has the treatment you have been taking during the last 4 weeks improved your erections?), and the number of subjects whose EF domain score at the 8th week visit was ≥ 26.
Adverse events (AEs) were classified as undesirable and unexpected signs, symptoms, diseases, and accidents arising after administration throughout the study period. Safety assessments included laboratory tests (hematology, clinical biochemistry, blood coagulation test, and urinalysis), vital signs (blood pressure and heart rate), physical examination, 12-lead electrocardiogram recordings, and patient reports of AEs.
Safety evaluation
AEs and adverse drug reactions: Differences between the placebo group and the avanafil groups were compared using χ2 or Fisher's exact test. AEs reported in study subjects are presented according to the World Health Organization (WHO) Adverse Reactions Terminology (WHOART) system organ classes. Adverse drug reactions related to the investigational product were compared using the same method.
Statistical analysis
For randomization, the ‘proc plan’ procedure in the SAS software (ver. 9.1; SAS Institute, Cary, NC, USA) was used. Using a block randomization method, subjects were divided randomly into avanafil 50, 100, and 200 mg and placebo: 4 groups in a 1:1:1:1 ratio. Regarding the definition of the evaluation population, the maximum efficacy evaluation population included subjects who satisfied the inclusion criteria, took the investigational product at least once, visited the hospital after taking the investigational product, and who provided results for the efficacy evaluation. The safety evaluation population consisted of subjects who made a visit after taking the investigational product once or more and who provided follow-up safety results.
To evaluate initial comparability, discrete variables were compared using χ2 tests or Fisher's exact test, and successive variables were compared using analysis of variance (ANOVA) or the Kruskal-Wallis test.
The efficacy evaluation was performed using each of the following methods. Analysis of covariance (ANCOVA) was used to check whether there was a difference between 2 groups in changes of all domain scores in IIEF and success rate in SEP Q2–5. The differences in GEAQ and normal erectile function (IIEF-EF domain score ≥ 26) between groups were analyzed by χ2 tests. The efficacy results were analyzed using Dunnett's or Bonferroni's multiple comparison tests to check whether there was a significant difference between the placebo group and the avanafil groups. All statistical analyses were performed at a significance level of 5% and a test power of 80%, and were 2-sided.
The number of patients evaluated in this study was based on the results of a phase II clinical study involving Westerners (15). The number of subjects was calculated on the assumption that the avanafil 100 mg group would differ significantly in the EF domain. Considering the results of the Western study, the difference between the placebo group and the avanafil 100 mg group was fixed to 5 and standard deviation was fixed at 7.5. As a result, each group needed 36 subjects. However, the actual groups contained 40 subjects and the target number was fixed to 160, considering drop-outs. The α-error was 0.05 (2-tail test) and the β-error was 0.2.
Ethics statement
This multi-center, prospective, randomized, double-blinded, placebo-controlled, therapeutic exploratory clinical study was conducted at 8 centers in Korea in accordance with Good Clinical Practice (GCP) and International Conference on Harmonization guidelines (ICH), and was consistent with the ethical principles of the Declaration of Helsinki. Forms of the documents related with this clinical study, i.e., the study protocol and the informed consent form, were all reviewed and approved by Institutional Review Board of Pusan National University Hospital (No. PNUH 2007111). Written informed consent was obtained from each patient prior to randomization. [REMOVED HYPERLINK FIELD] The present clinical trial was registered at www.ClinicalTrials.gov (Identifier: NCT02477436).
RESULTS
Demographics
Of the 160 subjects, 158 were included in the intent-to treat (ITT) population and 137 subjects were included in the per protocol (PP) population, which were used for analyses of efficacy parameters (Fig. 1B). The mean patient age was 56.4 ± 7.8 years. At baseline, no clinically or statistically meaningful difference was found between the treatment groups with respect to demographic or clinical variables (Table 1).
Table 1. Baseline characteristics of patients (ITT population).
| Category | Placebo (n = 39) | Avanafil 50 mg (n = 40) | Avanafil 100 mg (n = 40) | Avanafil 200 mg (n = 39) | Total (n = 158) |
|---|---|---|---|---|---|
| Age, yr | |||||
| Mean (SD) | 56.7 (9.0) | 55.7 (7.6) | 57.2 (8.0) | 56.1 (6.7) | 56.4 (7.8) |
| Median | 58 | 57 | 59 | 57 | 58 |
| Min–Max | 29–69 | 41–67 | 33–69 | 42–67 | 29–69 |
| Smoking, No. (%) | |||||
| Yes | 10 (25.6) | 8 (20.0) | 8 (20.0) | 9 (23.1) | 35 |
| No | 29 (74.4) | 32 (80.0) | 32 (80.0) | 30 (76.9) | 123 |
| Alcohol, No. (%) | |||||
| Yes | 21 (53.9) | 27 (67.5) | 23 (57.5) | 21 (53.9) | 92 |
| No | 18 (46.2) | 13 (32.5) | 17 (42.5) | 18 (46.2) | 66 |
| EF domain | |||||
| Mean (SD) | 15.1 (3.0) | 16.0 (3.0) | 15.7 (3.0) | 16.0 (3.1) | 15.7 (3.0) |
| Median | 15 | 16 | 16 | 16 | 16 |
| Min–Max | 11–22 | 11–24 | 11–21 | 11–25 | 11–25 |
| Duration of ED, yr | |||||
| Mean (SD) | 5.9 (4.7) | 4.8 (4.0) | 5.2 (5.0) | 4.6 (3.4) | 5.1 (4.3) |
| Median | 5.0 | 4.0 | 3.1 | 3.5 | 4.0 |
| Min–Max | 0.6–20.0 | 0.6–14.2 | 0.8–23.0 | 0.8–15.0 | 0.6–23.0 |
| Etiology, No. (%) | |||||
| Organic origin | 13 (33.3) | 16 (40.0) | 14 (35.0) | 13 (33.3) | 56 |
| Mixed origin | 23 (59.0) | 22 (55.0) | 21 (52.5) | 22 (56.4) | 88 |
| Psychological origin | 3 (7.7) | 2 (5.0) | 5 (12.5) | 4 (10.3) | 14 |
| Previous treatment for ED, No. (%) | |||||
| None | 15 (38.5) | 22 (55.0) | 24 (60.0) | 24 (61.5) | 85 |
| Experienced | 24 (61.5) | 18 (45.0) | 16 (40.0) | 15 (38.5) | 73 |
| Concomitant diseases, No. (%) | |||||
| None | 6 (15.4) | 7 (17.5) | 6 (15.0) | 5 (12.8) | 24 |
| Yes | 33 (84.6) | 33 (82.5) | 34 (85.0) | 34 (87.2) | 134 |
There were no significant differences between the groups in all parameters.
SD = standard deviation, ITT = intent-to-treat, Min = minimum, Max = maximum, ED = erectile dysfunction, EF = erectile function.
Primary efficacy outcome variables
EF domain in IIEF questionnaire
The change from baseline in total EF domain scores in each dosage group was statistically significant (P < 0.001). In multiple comparisons, the dosage groups except for avanafil 50 mg differed significantly from the placebo group (Table 2).
Table 2. Mean change from baseline in the IIEF domain score.
| IIEF domains | Placebo (n = 39) | Avanafil 50 mg (n = 40) | Avanafil 100 mg (n = 40) | Avanafil 200 mg (n = 39) | |
|---|---|---|---|---|---|
| EF | Responses (8 wk) | 18.6 (7.6) | 20.7 (5.5) | 22.6 (5.9) | 25.3 (4.1) |
| Change from baseline | 3.2 (1.4, 5.1) | 4.9 (3.1, 6.7) | 6.8 (5.0, 8.6)† | 9.1 (7.3, 11.0)† | |
| Intercourse satisfaction | Responses (8 wk) | 8.5 (2.8) | 9.3 (2.3) | 9.8 (3.3) | 11.2 (2.9) |
| Change from baseline | 2.4 (1.5, 3.3) | 3.0 (2.2, 3.9) | 3.4 (2.5, 4.2) | 4.9 (4.0, 5.8)† | |
| Orgasmic function | Responses (8 wk) | 5.8 (2.8) | 6.8 (2.4) | 7.3 (2.4) | 8.4 (1.7) |
| Change from baseline | 0.7 (−0.03, 1.5) | 1.7 (1.0, 2.5) | 2.1 (1.3, 2.8)* | 3.1 (2.3, 3.8)† | |
| Sexual desire | Responses (8 wk) | 5.8 (2.0) | 6.6 (1.6) | 6.9 (2.0) | 7.6 (1.6) |
| Change from baseline | 0.9 (0.3, 1.4) | 1.4 (0.8, 1.9) | 1.4 (0.9, 1.9) | 2.1 (1.5, 2.6)* | |
| Overall satisfaction | Responses (8 wk) | 5.3 (2.2) | 5.9 (1.8) | 6.1 (2.3) | 7.4 (1.7) |
| Change from baseline | 1.0 (0.3, 1.6) | 1.6 (1.0, 2.2) | 1.8 (1.2, 2.5) | 3.1 (2.4, 3.7)† | |
| Question 3 | Responses (8 wk) | 3.4 (1.5) | 4.1 (1.2) | 4.3 (1.0) | 4.8 (0.5) |
| Change from baseline | 0.2 (−0.1, 0.5) | 0.8 (0.5, 1.2)* | 1.0 (0.7, 1.3)* | 1.4 (1.0, 1.7)† | |
| Question 4 | Responses (8 wk) | 2.7 (1.5) | 2.6 (1.4) | 3.1 (1.6) | 3.7 (1.3) |
| Change from baseline | 1.1 (0.7, 1.6) | 1.1 (0.6, 1.5) | 1.5 (1.0, 1.9) | 2.1 (1.6, 2.6)* |
All values are expressed as mean (SD) and number (95% CI).
EF = erectile function, IIEF = International Index of Erectile Function, SD = standard deviation, CI = confidence interval.
*P < 0.05; †P < 0.001, vs. placebo.
Secondary efficacy outcome variables
IIEF domains other than EF
IIEF domain scores were similar at baseline, but the avanafil groups had significantly higher endpoint IIEF scores across all IIEF domains compared with the placebo group (Table 2).
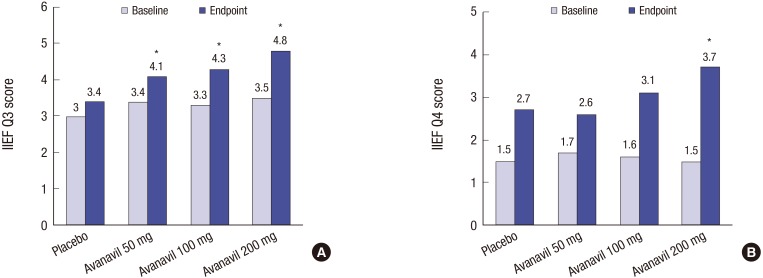
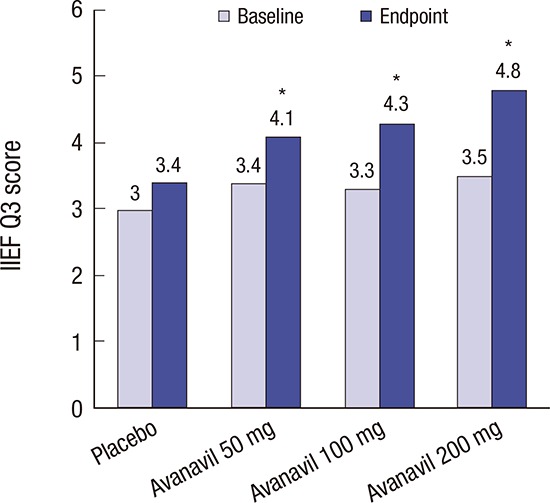
IIEF Q3 and Q4
The change from baseline in IIEF Q3 scores in each dose group was statistically significant (P < 0.001). In multiple comparisons, all dose groups of avanafil differed significantly from the placebo group (Fig. 2A).
Fig. 2.
Effects of avanafil on reponses to IIEF Q3 (A) and IIEF Q4 (B) score at 8 weeks after the start of treatment.
IIEF = International Index of Erectile Function, IIEF Q3 = International Index of Erectile Function questions 3, IIEF Q4 = International Index of Erectile Function questions 4.
*P < 0.05 vs. placebo.
The change from baseline in the score of IIEF Q4 in each dose group was statistically significant (P = 0.008). In multiple comparisons, avanafil 200 mg differed significantly from the placebo (Fig. 2B).
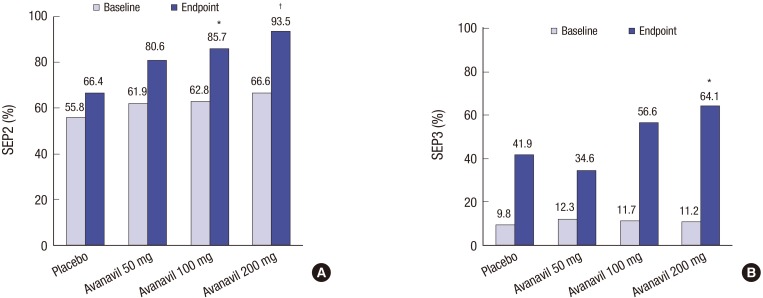
SEP 2–5
SEP 2 success rates were 66.4%, 81.7%, 86.5%, and 93.5% for the placebo, avanafil 50, 100, and 200 mg, respectively. The change from baseline in SEP 2 success rate in each dose group was statistically significant (P = 0.001). In multiple comparisons, avanafil 100 and 200 mg differed significantly from the placebo (Fig. 3A).
Fig. 3.
Effects of avanafil on reponses to the SEP2 (A) and SEP3 (B) at 8 weeks after the start of treatment.
SEP2 = Sexual Encounter Profile question 2, SEP3 = Sexual Encounter Profile question 3.
*P < 0.05 vs. placebo, †P < 0.001 vs. placebo.
SEP 3 success rates were 41.9%, 34.3%, 56.3%, and 64.1% for the placebo, avanafil 50, 100, and 200 mg, respectively. The change from baseline in SEP 3 success rate in each dose group was statistically significant (P = 0.002). In multiple comparisons, avanafil 200 mg differed significantly from the placebo (Fig. 3B). The changes from baseline in SEP 4 and 5 success rates in each dose group were statistically significant. In multiple comparisons, avanafil 200 mg differed significantly from the placebo.
GEAQ
GEAQ improvement rates for the placebo, avanafil 50, 100, and 200 mg were 38.5%, 55%, 75%, and 89.5%, respectively. The dosage groups except for avanafil 50 mg differed significantly from the placebo in multiple comparisons.
Ratio of normal EF
The total score of the EF domain at completion of administration was classified as ‘normal’ for ≥ 26 and ‘abnormal’ for < 26. The ratios of normal EF for the placebo, avanafil 50, 100, and 200 mg were 20.5%, 20.0%, 40.0%, and 59.0%, respectively. Avanafil 200 mg differed significantly from the placebo (P = 0.001).
Safety and tolerability
In total, 159 subjects who took at least one dose were included in the safety analysis of avanafil. Most AEs were mild in severity, and no serious AE was reported during the study or follow-up period (Table 3). No clinically significant changes in laboratory tests, electrocardiogram, or blood pressure were observed in either group.
Table 3. Incidence of adverse drug reactions by WHOART system organ class.
| Category | Placebo (n = 39) | Avanafil 50 mg (n = 40) | Avanafil 100 mg (n = 40) | Avanafil 200 mg (n = 40) | Total (n = 159) |
|---|---|---|---|---|---|
| ADR case, % | 4 (10.3) | 3 (7.5) | 4 (10.0) | 5 (12.5) | 16 (10.1) |
| ADR event (event/subject) | 7 (0.18) | 5 (0.13) | 5 (0.13) | 6 (0.15) | 23 (0.14) |
| WHOART system organ class | |||||
| Cardiovascular, general | 2 (0.05) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 2 (0.01) |
| Blood pressure increased | 2 (0.05) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 2 (0.01) |
| Center & peripheral nervous system | 1 (0.03) | 3 (0.08) | 1 (0.03) | 2 (0.05) | 7 (0.04) |
| Dizziness | 0 (0.00) | 0 (0.00) | 1 (0.03) | 0 (0.00) | 1 (0.01) |
| Headache | 1 (0.03) | 1 (0.03) | 0 (0.00) | 2 (0.05) | 4 (0.03) |
| Migraine | 0 (0.00) | 2 (0.05) | 0 (0.00) | 0 (0.00) | 2 (0.01) |
| Gastro-intestinal system | 0 (0.00) | 0 (0.00) | 1 (0.03) | 0 (0.00) | 1 (0.01) |
| Heartburn | 0 (0.00) | 0 (0.00) | 1 (0.03) | 0 (0.00) | 1 (0.01) |
| Hearing and vestibular | 0 (0.00) | 0 (0.00) | 1 (0.03) | 0 (0.00) | 1 (0.01) |
| Tinnitus | 0 (0.00) | 0 (0.00) | 1 (0.03) | 0 (0.00) | 1 (0.01) |
| Liver and biliary system | 3 (0.08) | 1 (0.03) | 0 (0.00) | 0 (0.00) | 4 (0.03) |
| ALT increased | 1 (0.03) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 1 (0.01) |
| AST increased | 1 (0.03) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 1 (0.01) |
| Bilirubin increased | 0 (0.00) | 1 (0.03) | 0 (0.00) | 0 (0.00) | 1 (0.01) |
| GGT increased | 1 (0.03) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 1 (0.01) |
| Vascular (extracardiac) | 1 (0.03) | 1 (0.03) | 2 (0.05) | 3 (0.08) | 7 (0.04) |
| Flushing | 1 (0.03) | 1 (0.03) | 2 (0.05) | 3 (0.08) | 7 (0.04) |
| Vision | 0 (0.00) | 0 (0.00) | 0 (0.00) | 1 (0.03) | 1 (0.01) |
| Ocular hyperemia | 0 (0.00) | 0 (0.00) | 0 (0.00) | 1 (0.03) | 1 (0.01) |
WHOART = World Health Organization (WHO) Adverse Reactions Terminology, ADR = adverse drug reactions, ALT= alanine transaminase, AST = aspartate aminotransferase, GGT = gamma-glutamyl transferase.
DISCUSSION
Currently, the basis of ED treatment is PDE5 inhibitors (7). Since the development of sildenafil, PDE5 inhibitors have been used as the first-line treatment for ED, regardless of the cause (6). There have been many reports of using PDE5 inhibitors to treat various types of ED and varying degrees of ED (8). Although PDE5 inhibitors are efficacious for the treatment of ED, high rates of treatment discontinuation have also been reported, ranging from 14.0%–80.4% (16). Reasons for treatment discontinuation include lack of efficacy, AEs, fear about AEs, an unnatural forced drug-induced erection, and the inconvenience of waiting for the drug's onset of action (17). If first-line ED therapy, such as PDE5 inhibitors, is not sufficient for patient satisfaction, a second-line therapy is needed. The most commonly used second-line therapy is intracavernous injection (7,18), which has a success rate of –70%–85% (18). However, poor treatment compliance and ensuing high dropout rates (41%–68%) have been reported (19,20). Thus, there is a continuing need for the development and improvement of new PDE5 inhibitors for ED. One reason for reduced therapeutic efficacy of oral PDE5 inhibitors is that patients do not adequately follow the medication counseling, such as drug dosing time; another is that some patients are overly concerned about side effects that may occur when taking the medication (21). Given this, avanafil may reduce the inconvenience regarding dosing time because its onset of efficacy is very soon after administration, and it is also advantageous in terms of side effects due to its high selectivity for PDE5 (10,11). Based on our results, we recommended taking the trial drug, avanafil, 30 minutes before sexual intercourse, which leads to a significant improvement in EF in terms of the primary and secondary outcomes. However, in previous studies with other PDE5 inhibitors, the study drug was usually taken 1–2 hours before attempting sexual intercourse (8). In a previous study, Mulhall et al. (12) reported that for all time intervals from dose to sexual attempt (15 minutes or less through > 360 minutes), the avanafil group had significantly higher proportions of successful responses in terms of vaginal penetration (SEP2), intercourse (SEP3), and overall sexual experience vs. the placebo. In particular, after dosing with 100 or 200 mg avanafil, 36.4% of sexual attempts (SEP3) at 15 minutes or less were successful vs. 4.5% for the placebo. Of all attempts made from 16–30 minutes and from 31–60 minutes after dosing, SEP3 success rates for the avanafil groups were 30.2% and 29.5% vs. 7.7% and 11.3% for the placebo, respectively. These results are consistent with the results of the present study, where patients experienced significant improvement in EF when taking avanafil 30 minutes prior to sexual activity.
As summarized in Table 3, avanafil treatment was well tolerated with no major differences in the incidence of AEs leading to discontinuation between the avanafil and placebo groups. The reasons for drop-out in some patients in this study were withdrawal of consent, visit window violation, and non-compliance (no or insufficient number of sexual attempts).
One of the goals of the present study was to select the most appropriate dose among the 3 treatment options of avanafil. The results revealed that 100 and 200 mg avanafil both differed significantly from the placebo in almost all measures. Moreover, avanafil 100 and 200 mg did not differ from the placebo in terms of AEs, abnormal changes in clinical laboratory values, or changes in vital signs. However, in the case of avanafil 50 mg, we did not find a significant improvement compared with the placebo in the EF domain in the IIEF questionnaire, IIEF Q4, SEP2–5, or GEAQ. Except for our study, Goldstein's study (10) was the only clinical trial that evaluated the efficacy of avanafil 50 mg. They reported that following 12 weeks of avanafil treatment without food or alcohol restrictions, significant improvements in sexual function were observed with all 3 doses of avanafil compared with placebo. However, the 50 mg dose was inferior to the 100 and 200 mg doses, while the efficacy of the 100 and 200 mg doses was similar. Wang's study (22), which meta-analyzes 5 randomized controlled trials, including Goldstein's study (10), suggests that although all doses of avanafil are effective, practitioners should treat ED patients with avanafil at a starting dose of 100 mg, and then adjust the dosage on demand taking both effectiveness and safety into consideration. Based on the results of these clinical studies, the optimal doses of avanafil appear to be 100 and 200 mg in Korea and other countries.
Because avanafil is the most recently developed PDE5 inhibitor, relatively few clinical studies have been conducted on it. The present study was a multi-center study investigating the efficacy and safety of avanafil in the treatment of Korean patients with ED.
Although the findings of this study suggest that avanafil is absorbed rapidly with a fast onset of drug action and has acceptable efficacy and safety, some limitations should be noted. First, due to sociocultural differences among various populations with different ethnic origins, the efficacy and safety profile of avanafil observed in this study, which included Korean patients only, may differ somewhat for other ethnic groups. Second, because our patients were only enrolled at tertiary care centers, it could be argued that the findings only reflect the efficacy of avanafil in a select group of patients being managed by tertiary specialists. Third, the present study was designed to have a relatively short period of treatment: 8 weeks. Long-term data are therefore needed, as in other PDE5 inhibitor studies. A final limitation is that this study did not have a crossover design. In this study, the efficacy of avanafil was not assessed according to ED severity. Future studies of avanafil should also include difficult-to-treat patients with ED, such as those with diabetic ED and ED after prostate cancer surgery.
In conclusion, avanafil, taken as needed 30 minutes before sexual activity during an 8-week period, yielded significant improvements in EF, as measured by the IIEF, SEP, and GEAQ, in Korean patients with ED. Avanafil 100 and 200 mg yielded significant improvements compared with the placebo in most measures of efficacy. In terms of safety issues, avanafil 50, 100, and 200 mg did not differ from the placebo. Based on these results, we suggest that avanafil 100 and 200 mg may be useful therapeutic agents for patients with ED.
Footnotes
Funding: This study was sponsored by Choongwae Pharma Corporation (Protocol No. CWP-AVA-201).
DISCLOSURE: This study was sponsored by Choongwae Parma Corporation but the sponsor played no roles in the study design or in the collection, analysis, or interpretation of the data. The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Conceptualization: Park NC. Data curation: Park HJ. Formal analysis: Park HJ. Investigation: Kim SW, Kim JJ, Lee SW, Paick JS, Ahn TY, Park K, Park JK, Park NC. Writing - original draft: Park HJ. Writing - review & editing: Park HJ, Park NC.
References
- 1.Goldstein I, Lue TF, Padma-Nathan H, Rosen RC, Steers WD, Wicker PA. Oral sildenafil in the treatment of erectile dysfunction. Sildenafil Study Group. N Engl J Med. 1998;338:1397–1404. doi: 10.1056/NEJM199805143382001. [DOI] [PubMed] [Google Scholar]
- 2.Park JH, Cho IC, Kim YS, Kim SK, Min SK, Kye SS. Body mass index, waist-to-hip ratio, and metabolic syndrome as predictors of middle-aged men's health. Korean J Urol. 2015;56:386–392. doi: 10.4111/kju.2015.56.5.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Canat L, Canat M, Guner B, Gurbuz C, Caşkurlu T. Association between renal function, erectile function and coronary artery disease: detection with coronary angiography. Korean J Urol. 2015;56:76–81. doi: 10.4111/kju.2015.56.1.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ko K, Yang DY, Lee WK, Kim SW, Moon DG, Moon KH, Park NC, Park JK, Son HC, Lee SW, et al. Effect of improvement in lower urinary tract symptoms on sexual function in men: tamsulosin monotherapy vs. combination therapy of tamsulosin and solifenacin. Korean J Urol. 2014;55:608–614. doi: 10.4111/kju.2014.55.9.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DeLay KJ, Haney N, Hellstrom WJ. Modifying risk factors in the management of erectile dysfunction: a review. World J Mens Health. 2016;34:89–100. doi: 10.5534/wjmh.2016.34.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ryu JK, Cho KS, Kim SJ, Oh KJ, Kam SC, Seo KK, Shin HS, Kim SW. Korean Society for Sexual Medicine and Andrology (KSSMA) guideline on erectile dysfunction. World J Mens Health. 2013;31:83–102. doi: 10.5534/wjmh.2013.31.2.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hatzimouratidis K, Amar E, Eardley I, Giuliano F, Hatzichristou D, Montorsi F, Vardi Y, Wespes E, European Association of Urology Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. Eur Urol. 2010;57:804–814. doi: 10.1016/j.eururo.2010.02.020. [DOI] [PubMed] [Google Scholar]
- 8.Yuan J, Zhang R, Yang Z, Lee J, Liu Y, Tian J, Qin X, Ren Z, Ding H, Chen Q, et al. Comparative effectiveness and safety of oral phosphodiesterase type 5 inhibitors for erectile dysfunction: a systematic review and network meta-analysis. Eur Urol. 2013;63:902–912. doi: 10.1016/j.eururo.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 9.Gresser U, Gleiter CH. Erectile dysfunction: comparison of efficacy and side effects of the PDE-5 inhibitors sildenafil, vardenafil and tadalafil--review of the literature. Eur J Med Res. 2002;7:435–446. [PubMed] [Google Scholar]
- 10.Goldstein I, McCullough AR, Jones LA, Hellstrom WJ, Bowden CH, Didonato K, Trask B, Day WW. A randomized, double-blind, placebo-controlled evaluation of the safety and efficacy of avanafil in subjects with erectile dysfunction. J Sex Med. 2012;9:1122–1133. doi: 10.1111/j.1743-6109.2011.02629.x. [DOI] [PubMed] [Google Scholar]
- 11.Jung J, Choi S, Cho SH, Ghim JL, Hwang A, Kim U, Kim BS, Koguchi A, Miyoshi S, Okabe H, et al. Tolerability and pharmacokinetics of avanafil, a phosphodiesterase type 5 inhibitor: a single- and multiple-dose, double-blind, randomized, placebo-controlled, dose-escalation study in healthy Korean male volunteers. Clin Ther. 2010;32:1178–1187. doi: 10.1016/j.clinthera.2010.06.011. [DOI] [PubMed] [Google Scholar]
- 12.Mulhall JP, Burnett AL, Wang R, McVary KT, Moul JW, Bowden CH, DiDonato K, Shih W, Day WW. A phase 3, placebo controlled study of the safety and efficacy of avanafil for the treatment of erectile dysfunction after nerve sparing radical prostatectomy. J Urol. 2013;189:2229–2236. doi: 10.1016/j.juro.2012.11.177. [DOI] [PubMed] [Google Scholar]
- 13.Kedia GT, Uckert S, Assadi-Pour F, Kuczyk MA, Albrecht K. Avanafil for the treatment of erectile dysfunction: initial data and clinical key properties. Ther Adv Urol. 2013;5:35–41. doi: 10.1177/1756287212466282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rosen RC, Cappelleri JC, Gendrano N., 3rd The International Index of Erectile Function (IIEF): a state-of-the-science review. Int J Impot Res. 2002;14:226–244. doi: 10.1038/sj.ijir.3900857. [DOI] [PubMed] [Google Scholar]
- 15.Hellstrom WJ, Freier MT, Serefoglu EC, Lewis RW, DiDonato K, Peterson CA. A phase II, single-blind, randomized, crossover evaluation of the safety and efficacy of avanafil using visual sexual stimulation in patients with mild to moderate erectile dysfunction. BJU Int. 2013;111:137–147. doi: 10.1111/j.1464-410X.2012.11267.x. [DOI] [PubMed] [Google Scholar]
- 16.Carvalheira AA, Pereira NM, Maroco J, Forjaz V. Dropout in the treatment of erectile dysfunction with PDE5: a study on predictors and a qualitative analysis of reasons for discontinuation. J Sex Med. 2012;9:2361–2369. doi: 10.1111/j.1743-6109.2012.02787.x. [DOI] [PubMed] [Google Scholar]
- 17.Ljunggren C, Hedelin H, Salomonsson K, Ströberg P. Giving patients with erectile dysfunction the opportunity to try all three available phosphodiesterase type 5 inhibitors contributes to better long-term treatment compliance. J Sex Med. 2008;5:469–475. doi: 10.1111/j.1743-6109.2007.00688.x. [DOI] [PubMed] [Google Scholar]
- 18.Leungwattanakij S, Flynn V, Jr, Hellstrom WJ. Intracavernosal injection and intraurethral therapy for erectile dysfunction. Urol Clin North Am. 2001;28:343–354. doi: 10.1016/s0094-0143(05)70143-9. [DOI] [PubMed] [Google Scholar]
- 19.Vardi Y, Sprecher E, Gruenwald I. Logistic regression and survival analysis of 450 impotent patients treated with injection therapy: long-term dropout parameters. J Urol. 2000;163:467–470. [PubMed] [Google Scholar]
- 20.Sundaram CP, Thomas W, Pryor LE, Sidi AA, Billups K, Pryor JL. Long-term follow-up of patients receiving injection therapy for erectile dysfunction. Urology. 1997;49:932–935. doi: 10.1016/s0090-4295(97)00079-4. [DOI] [PubMed] [Google Scholar]
- 21.Park NC, Kim TN, Park HJ. Treatment strategy for non-responders to PDE5 inhibitors. World J Mens Health. 2013;31:31–35. doi: 10.5534/wjmh.2013.31.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang H, Yuan J, Hu X, Tao K, Liu J, Hu D. The effectiveness and safety of avanafil for erectile dysfunction: a systematic review and meta-analysis. Curr Med Res Opin. 2014;30:1565–1571. doi: 10.1185/03007995.2014.909391. [DOI] [PubMed] [Google Scholar]