Summary
Background
Cone beam computed tomography (CBCT) has become a reliable adjunctive tool for both diagnosis and treatment planning in the field of dentistry. There are numerous advantages of CBCT over 2D imaging techniques (OPG). There is a need to evaluate the changing trend of preference and purpose of utilisation of these imaging modalities by dental practitioners.
This study was carried out to evaluate and compare the purpose and preference of utilisation of CBCT and OPG by various dental practitioners in their clinical practice.
Material/Methods
A retrospective, cross-sectional study was carried out on CBCT and OPG data of 620 different cases treated by different dental practitioners from imaging centres in the twin cities of Telangana (Hyderabad & Secunderabad). For comparisons, we used the Mann-Whitney U test (Z test).
Results
The analysis of data showed that among the dental practitioners OPG was more commonly ordered by general dentists (31%) followed by prosthodontists (30%), whereas CBCT was more advocated by general dental practitioners (25%) followed by OMFS (23%).
OPG preference was greater for fixed partial denture planning (FPD) 59%, whereas CBCT was highly preferred for implant planning 61%.
Conclusions
The present study showed that general dentists preferred OPG and CBCT compared to other dental practitioners, and OPG was advocated for FPD planning, whereas CBCT was advocated for implant planning. Moreover, and it was found that there had been a drastic increase in the preference of CBCT over OPG in recent times.
MeSH Keywords: Cone-Beam Computed Tomography; Imaging, Three-Dimensional; Radiography, Panoramic
Background
Cone beam computed tomography (CBCT) scanners were introduced fifteen years ago as an adaptive technology to meet the demand for three-dimensional (3D) information regarding craniofacial imaging [1,]. A widespread interest in CBCT imaging developed as a result of its varied applications in dentistry for implant planning, orthodontic treatment planning, impactions, evaluation of cysts, tumours etc. [2]. The present study was performed to analyse the purpose of utilisation and preference of CBCT and OPG by dental practitioners in the twin cities (Hyderabad & Secunderabad).
Material and Methods
The database of 620 CBCT and OPG examinations performed over a period of 3 months was collected with the consent of referring dentists and managing directors of seven diagnostic centres in the twin cities (Hyderabad & Secunderabad).
Inclusion criteria
The centres containing both OPG and CBCT equipment were included.
All data, irrespective of age and sex, were included in the study.
Exclusion criteria
The centres containing only OPG or only CBCT equipment were excluded from the study
Results
Out of 620 cases, CBCT constituted 89.9% (557) while (OPG) 10.1% (63) of all examinations (Figure 1). The analysed data showed the following percentages of different dental practitioners who advised OPG (N=63) – general dentists, 31% (20), prosthodontists, 30% (19), OMFS, 15% (9), orthodontist, 7% (5), periodontists, 7% (5), endodontists, 6% (3) and pedodontists, 3% (2) (Figure 2).
Figure 1.
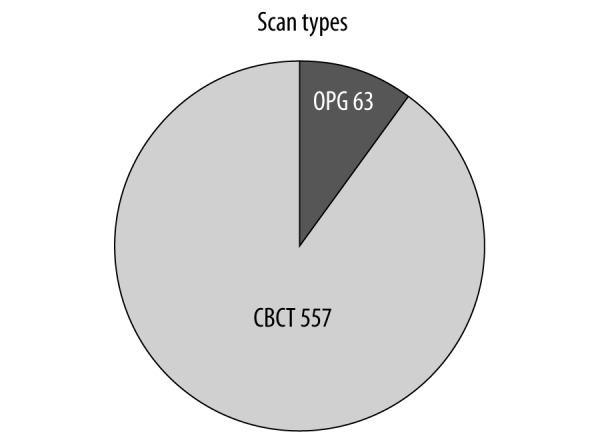
Relative contribution of OPG and CBCT data (OPG=63, CBCT=557). Sample of 620 cases were studied.
Figure 2.
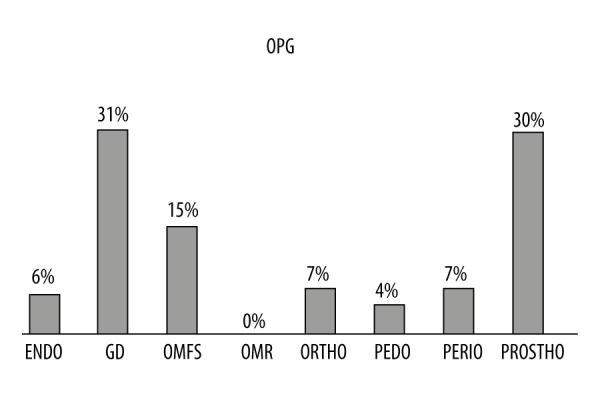
Percentage of different dental practitioners who ordered OPG.
The analysed data showed that among the dental practitioners who advised CBCT (N=557), general dentists comprised 25% (53), OMFS 23% (128), prosthodontists 18.5%(104), orthodontists 11.5% (64), endodontists 10% (53), periodontists 6.5% (36), oral radiologists 3.5% (20) and pedodontists 2% (11) (Figure 3).
Figure 3.
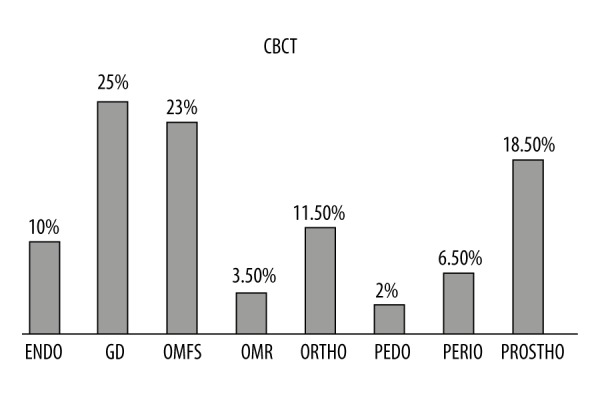
Percentage of different dental practitioners who ordered CBCT. Sample of 557 cases where CBCT was advised.
Among the 10.1% (N=63) of cases referred for (OPG), the purpose of OPG was FPD planning, 59% (34), periodontitis, 26% (15), impactions, 9% (5), orthodontic treatment planning, 5%(3), cysts, 3% (2), jaw fractures, 3% (2), root canal planning, 2% (1) and pre-implant planning, 2% (1) (Figure 4).
Figure 4.
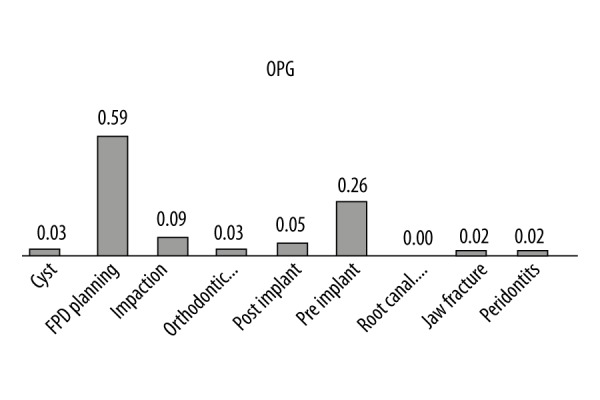
Different purposes for using OPG, in percentages. Sample of 63 cases where OPG was advised.
Among the 89.9% (N=557) of cases referred for CBCT, the purpose of CBCT was pre-implant planning, 42%(235), post-implant planning, 19%(111), impactions, 15%(86), root canal planning, 10% (55), orthodontic treatment planning, 5%(25), cysts, 4%(17), jaw fractures, 2% (13) and periodontitis, 2%(11) (Figure 5).
Figure 5.
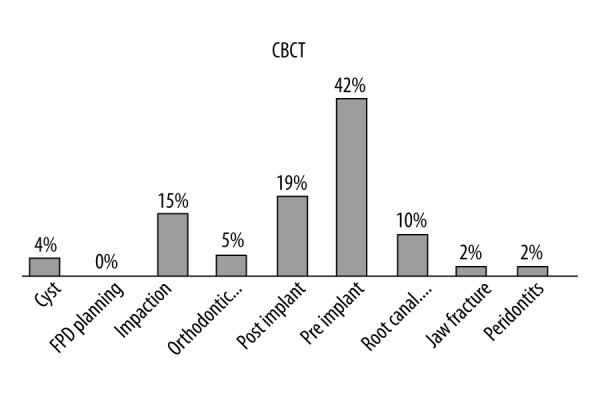
Different purposes for using CBCT, in percentages. Sample of 557 cases where CBCT was advised.
A statistically significant p value (<0.05) was obtained, showing that CBCT was preferred for implant planning (pre-implant planning, post-implant planning) followed by other purposes including impaction, root canal treatment planning, orthodontic treatment planning, cysts, jaw fractures and periodontitis. In contrast, OPG was preferred for FPD planning and bone evaluation in periodontitis (Table 1).
Table 1.
Preferential use of OPG and CBCT in different cases.
| OPG vs. CBCT | Z value | P Value | CBCT |
|---|---|---|---|
| Cyst | 4.12 | <.005 | ✓ |
| FPD planning | −5.67 | >.05 | × |
| Impaction + implant | 5.10 | <.005 | ✓ |
| Impactions | 6.89 | <.005 | ✓ |
| Jaw fracture | 3.74 | <.005 | ✓ |
| Ortho planning | 3.80 | <.005 | ✓ |
| Periodontitis | −0.82 | >.05 | × |
| Post implant | 10.54 | <.005 | ✓ |
| Pre implant | 14.94 | <.005 | ✓ |
| Root canal planning | 7.35 | <.005 | ✓ |
Discussion
The number of dentists who prefer digital radiography over conventional film radiography has increased in recent times [3]. Our study focused mainly on the purpose and preference of 3-D imaging (CBCT) compared to orthopantomogram (OPG) by dental practitioners in their clinical practice. Hence, this study was performed in order to evaluate the above-mentioned aspects. In our study, 10.1% (N=63) of dentists ordered OPG for both diagnosis and treatment. This is in line with a study conducted by Mioara Decusara et al., where out of 524 dentists, 403 (77%) thought that orthopantomogram was useful in a private dental practice, especially in cases requiring complex treatment, and that it did not expose the patient to unnecessary radiation [4].
In our study, 89.9% of dental specialists ordered CBCT., Among them, general dentists comprised 25%, OMFS 23%, prosthodontists 18.5%, orthodontists 11.5%, endodontists 10%, periodontists 6.5%, oral radiologists 3.5% and pedodontists 2%. This shows that the use of 3D imaging (CBCT) is popular among various dental practitioners, which is in line with the study performed by W. D Vos et al. in Belgium, where OMFS (41%) preferred CBCT scans followed by orthodontists (16%) [5]. In another study by Hol C et al., periodontists and oral and maxillofacial surgeons were the specialists who most frequently advised CBCT [6]. The advocacy of CBCT varies with the demographic variation in the type and prevalence of dental diseases, type of practice and the awareness of the 3D technology and its multiplanar imaging modality.
In the present study, OPG was advised most commonly for FPD planning, 59%, followed by periodontal bone evaluation, 26%, impactions, 9%, orthodontic treatment planning, 5%, cysts, 3%, jaw fractures, 3%, root canal planning, 2% and pre-implant planning, 2%. In a questionnaire study conducted by Mioara Decusara et al., 546 dental practitioners said that OPG is recommended as a useful tool for multiple carious lesions and endodontics, 78% (N=426), restorative and prosthetic treatment, 71.3% (N=389) orthodontics, 40% (N=218), periodontology, 38.1% (N=208), pre- and post-surgery, 32.1% (N =175), paediatric dentistry, 28% (N=153) and pre- and post-dental implants, 23% (N=127) [4].
In the present study, CBCT was advised most commonly for implant planning (61%), which was in line with the study conducted by Arnheiter et al., in which the main reasons for CBCT referrals were dental implant planning (40%) and suspected surgical pathology (24%) [7].
Dental practitioners have a fair idea about the usefulness of CBCT in different fields of dentistry, but it is preferred in implant planning due to its advantage over conventional imaging systems, which could be because of its ability of 3D reconstructions in the craniofacial region [8].
OPG provides an excellent general overview of the dentition and the jaws. However, it has certain inherent limitations when used for pre- and post-implant assessment, including distortions in the horizontal plane, magnification in the vertical plane and the image is only a two-dimensional representation of a three dimensional entity. Hence, that is the reason why practitioners are using 3D imaging rather than 2D imaging with OPG [9]. With cone beam computed tomography, oral health professionals gain a highly accurate 3-D images of the patient’s anatomy from a single scan. These 3-D images allow practitioners to better diagnose and understand the true extent of dental disease and therefore they can provide more appropriate treatment for patients [10].
Conclusions
Cone beam computed tomography is a relatively advanced imaging technique with a profound potential in the field of dentistry. This fact is now being realized and accepted by dental professionals. This imaging technique has been globally developed and has become the most advanced, cost-effective imaging technique for diagnosing maxillofacial pathologies. Dental specialists should become more familiar with various CBCT machines, appropriate software and interpretations to accurately diagnose and treat oral and maxillofacial diseases.
References
- 1.Genevive Machado L. CBCT imaging – A boon to orthodontics. Saudi Dent J. 2015;27:12–21. doi: 10.1016/j.sdentj.2014.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Keerththana B, Arathy Srinivasan L. Awareness and attitude among dental professional towards CBCT. Journal of Dental and Medical Sciences. 2013;10:55–59. [Google Scholar]
- 3.Hellén-Halme K. Quality aspects of digital radiography in general dental practice. Swed Dent J Suppl. 2007;184:9–60. [PubMed] [Google Scholar]
- 4.Decusar M. Use of orthopantomogram in dental practice – a statistical study. International Journal of Medical Dentistry. 2011;1:389–92. [Google Scholar]
- 5.De Vos W, Casselman J, Swennen GR. Cone-beam computerized Tomography (CBCT) imaging of the oral and maxillofacial region: A systematic review of the literature. Int J Oral Maxillofac Surg. 2009;38:609–25. doi: 10.1016/j.ijom.2009.02.028. [DOI] [PubMed] [Google Scholar]
- 6.Hol C, Hellén-Halme K, Torgersen G, et al. How do dentists use CBCT in dental clinics? A Norwegian nationwide survey. Acta Odontol Scand. 2015;73(3):195–201. doi: 10.3109/00016357.2014.979866. [DOI] [PubMed] [Google Scholar]
- 7.Arnheiter C, Scarfe WC, Farman AG. Trends in maxillofacialcone-beam computed tomography usage. Oral Radiol. 2006;22:80–85. [Google Scholar]
- 8.Dölekoğlu S, Fişekçioğlu E, İlgüy M, İlgüy D. The usage of digital radiography and cone beam computed tomography among Turkish dentists. Dentomaxillofacial Radiol. 2011;40:379–84. doi: 10.1259/dmfr/27837552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ramakrishnan P, Shafi FM, Subhash A. A survey on radiographic prescription practices in dental implant assessment among dentists in Kerala, India. Oral Health Dent Manag. 2014;13(3):826–30. [PubMed] [Google Scholar]
- 10.Nehaanilpatil, Gadda R, Salvi R. Cone beam computed tomography: Adding the third dimensions. Journal of Contemporary Dentistry. 2012;2(3):84–88. [Google Scholar]


