Abstract
Background
Safety net and teaching hospitals are somewhat more likely to be penalized for excess readmissions, but the association of other hospital characteristics with readmission rates is uncertain and may have relevance for hospital-centered interventions.
Objective
To examine the independent association of 8 hospital characteristics with hospital-wide 30-day risk-standardized readmission rate (RSRR).
Design
Retrospective cross-sectional multivariable analysis
Subjects
US hospitals
Measures
Center for Medicare and Medicaid Services specification of hospital-wide RSRR from July 1, 2013 through June 30, 2014 with race and Medicaid dual-eligibility added.
Results
We included 6,789,839 admissions to 4,474 hospitals of Medicare fee-for-service beneficiaries aged over 64 years. In multivariable analyses, there was regional variation: hospitals in the Mid-Atlantic region had the highest RSRRs (0.98 percentage points higher than hospitals in the Mountain region, 95% CI 0.84–1.12). For-profit hospitals had an average RSRR 0.38 percentage points (95% CI, 0.24–0.53) higher than public hospitals. Both urban and rural hospitals had higher RSRRs than those in medium metropolitan areas. Hospitals without advanced cardiac surgery capability had an average RSRR 0.27 percentage points (95% CI, 0.18, 0.36) higher than those with. The ratio of registered nurses per hospital bed was not associated with RSRR. Variability in RSRRs among hospitals of similar type was much larger than aggregate differences between types of hospitals.
Conclusions
Overall, larger, urban, academic facilities had modestly higher risk-standardized readmission rates than smaller, suburban, community hospitals, although there was a wide range of performance. The strong regional effect suggests that local practice patterns are an important influence. Disproportionately high readmission rates at for-profit hospitals may highlight the role of financial incentives favoring utilization.
Keywords: readmissions, hospital quality, health service research, organizational structure, health care delivery
Introduction
Reducing hospital readmissions has become a major focus of payers, policymakers and hospitals. Numerous studies have demonstrated that a variety of patient characteristics are associated with readmission.1 Nevertheless, despite focusing on high risk patients, many hospitals and communities are still struggling to reduce readmission rates.
Hospital readmission rates vary even after risk-adjustment for patient characteristics,2–4 suggesting that healthcare system factors play a role in readmission outcomes. As Donabedian noted 30 years ago, quality outcomes are influenced by both structural aspects of care and processes of care.5 Some studies have shown that certain structural characteristics (such as being a teaching or safety net hospital) are associated with readmission risk for individual conditions,6,7 and that hospitals with more nurses have fewer readmissions.2,7,8 However, these studies have focused on care for specific medical conditions and have not examined readmissions for all patients; they also have not always simultaneously controlled for other hospital characteristics.
A clearer understanding of the influence of structural effects – that is, which types of hospitals are succeeding at achieving lower readmission rates in both the general hospital population and among specific types of patients – may help in designing strategies to reduce readmissions. We have, for example, previously found that lower volume hospitals on average have lower overall readmission rates than higher volume hospitals, suggesting that there may be an advantage to a smaller setting in terms of organizing transitional care effectively.9 Understanding the magnitude of hospital-level differences is also important from a clinical and policy perspective. Given that risk-standardized hospital readmission rates have a relatively narrow range of performance (nationally the difference between the 25th percentile hospital and the 75th percentile hospital-wide RSRR is only 0.9 percentage points), and that hospitals above the mean for certain conditions are subject to financial penalties, even clinically small differences may have implications for payment in the current policy environment.
The Center for Medicare & Medicaid Services (CMS) publicly reports risk-standardized hospital-wide readmission rates for older patients with Medicare fee-for-service insurance in US acute care hospitals using a measure developed by these investigators and endorsed by the National Quality Forum.4 The hospital-wide readmission measure includes more than 90% of older hospitalized patients, and also characterizes admissions according to the likely inpatient treatment team, such as surgery, cardiology or medicine. Accordingly, we based our investigation on this measure, adding risk adjustment for race and dual eligibility status, to explore the association of hospital financial, structural and operational characteristics with risk-standardized readmission rates overall and for individual specialty cohorts.
Methods
Study cohort
To construct the hospital study cohort, we first identified all discharges between July 1, 2013–June 30, 2014 from United States short-term acute care or critical access hospitals for patients over 65 years with Medicare fee-for-service insurance who qualified for the CMS hospital-wide readmission measure. This measure specifications have previously been described in detail.4,10 Briefly, it includes discharges for patients who were discharged alive, not against medical advice, and not transferred to another acute care hospital. The measure excludes discharges in which the patients were admitted for medical treatment of cancer or primary psychiatric disease. In addition, it excludes discharges of patients without one year of prior enrollment in Medicare FFS and/or one month of post-discharge enrollment, and all discharges from FFS-exempt cancer hospitals. Patients could have more than one eligible discharge during the study period. The initial study cohort was all hospitals that had at least 25 eligible discharges in the study period. Of these, we excluded those which could not be matched to the American Hospital Association (AHA) annual survey file for 2013 and those which could not be matched to National Center for Health Statistics regional classifications (largely, hospitals in US territories).
Study data
We used 2012–2014 Medicare inpatient claims data combined with the Medicare enrollment file to obtain data on discharges, 12-month comorbidity history, and outcomes.
Outcome measure
Our primary outcome was the hospital-specific all-condition risk-standardized 30-day unplanned readmission rate (RSRR). We excluded planned readmissions according to a previously-described algorithm that takes into account major procedures occurring during readmission and the principal diagnosis of the readmission.11,12 The RSRR is defined as the geometric mean of standardized readmission ratios (SRRs) for five mutually exclusive specialty cohorts, multiplied by the overall crude readmission rate.4,10 The specialty cohorts are surgery/gynecology, cardiorespiratory, cardiovascular, neurology and medicine. These are defined based on the clinical specialty most likely to be caring for the patient based on principal diagnosis or, in the case of the surgery/gynecology cohort, major in-hospital procedures.4,10 We calculated each SRR using a hierarchical logistic regression model, adjusting for age, race (African American vs. non-African American), dual-eligibility status (Medicaid eligible vs. not), principal diagnosis condition and 30 comorbidity indicators based on Part A claims during the year prior to admission. Comorbidities present only during the index admission are included if they are not likely to be in-hospital complications of care. Of note, the publicly-reported RSRR does not include race and dual eligibility risk variables. For this analysis, we added these variables to reduce the possibility that any hospital-level effects were due to unmeasured differences in patient populations. Each model includes a random effect for hospital. The standardized readmission ratio (SRR) for each hospital was calculated as the (sum of the predicted readmission risks)/(sum of the expected readmission risks), where the sums were over all patients in the hospital; predicted risk is predicted probability including the hospital specific random effect, while expected risk is the predicted probability when the random effect is zero. The RSRR for each hospital is then constructed as the geometric mean of the specialty cohort SRRs for that hospital.
Independent variables
We assessed eight hospital characteristics, identified from the 2013 AHA annual survey, and based on prior evidence of importance to hospital performance: safety net status (a public hospital, or a private hospital with a Medicaid caseload more than one standard deviation above the state average13),6,14 hospital ownership (not-for-profit, for-profit or public),7 teaching status (major teaching [member of Council of Teaching Hospitals], minor teaching hospital, non-teaching),6 availability of cardiac procedures (capable of cardiac bypass surgery, capable only of cardiac catheterization, not capable of either) as a proxy for overall advanced surgical or procedural capacity, metropolitan status (defined according to the National Center for Health Statistics classification15), geographic region (US Census Bureau division),16 bed size (divided by AHA into 8 categories with smallest 6–24 beds and largest 500 or more),6 and RN/bed ratio.2,7,8
Statistical analysis
We used standard descriptive statistics to describe mean RSRRs according to hospital characteristics. We then constructed a volume weighted linear regression model including all hospital characteristics simultaneously to determine the adjusted association of each with RSRR. In secondary analyses, we replicated the main model for each specialty cohort separately. To assess whether inclusion of race and DE status affected the results, we also replicated all models using RSRRs that omit those two variables, consistent with public reporting.
Results
Demographics
We identified 4,772 hospitals in total, of which 4,593 had at least 25 eligible cases; 4,474 of those could be matched to the AHA survey. These 4,474 hospitals discharged 6,789,839 eligible admissions. We identified 1,035,239 unplanned readmissions (15.2% of all discharges) and 74,876 planned readmissions (7.2% of all readmissions). The mean age was 78.3 (SD 8.29). A total of 3,843,413 (56.6%) discharges were of female patients, 642,817 (9.5%) were of African American patients, and 995,521 (14.7%) were of dual-eligible patients. The largest specialty cohort was medicine with 2,841,458 discharges, and the smallest was neurology with 429,605.
Hospital characteristic results
The mean composite hospital RSRR was 15.23 (SD 0.80). The lowest specialty cohort mean RSRR was 10.96 for surgery/gynecology and the highest was 19.35 for cardiorespiratory conditions (Table 1).
Table 1.
Mean and median SRR overall and by specialty cohort
| Cohort | Hospitals with at least 25 cases (N) | Mean SRR | Std Dev | Lower Quartile | Median | Upper Quartile |
|---|---|---|---|---|---|---|
| All condition | 4474 | 15.23 | 0.80 | 14.76 | 15.17 | 15.63 |
| Medicine | 4445 | 16.87 | 1.16 | 16.14 | 16.78 | 17.47 |
| Surgery/gynecology | 3884 | 10.96 | 0.71 | 10.58 | 10.91 | 11.29 |
| Cardiorespiratory | 4371 | 19.35 | 1.26 | 18.56 | 19.24 | 20.04 |
| Cardiovascular | 4294 | 13.77 | 0.52 | 13.55 | 13.74 | 13.98 |
| Neurology | 4279 | 13.01 | 0.57 | 12.75 | 12.96 | 13.22 |
Hospitals were majority non-safety net (70.3%), non-teaching (74.0%), did not have advanced cardiac procedure capability (60.3%), and were relatively evenly geographically dispersed (Table 2). Overall, major teaching hospitals (mean RSRR 15.87) and mid-Atlantic hospitals (mean RSRR 15.75) had the highest RSRRs, while hospitals in the Mountain region (mean RSRR 15.00) and Pacific regions (mean RSRR 15.02) and those in small or medium metropolitan regions (mean RSRR 15.07) had the lowest RSRRs.
Table 2.
Characteristics and mean RSRRs of included hospitals (N=4,554)
| Characteristic | N Obs (%) | Mean (Std Dev) |
|---|---|---|
| Safety net status | ||
| Non-safety net hospital | 3147 (70.3%) | 15.21 (0.82) |
| Safety net hospital | 1327 (29.7%) | 15.28 (0.73) |
| Ownership | ||
| Not for profit | 2694 (60.2%) | 15.21 (0.81) |
| For profit | 806 (18.0%) | 15.29 (0.87) |
| Public | 974 (21.8%) | 15.25 (0.67) |
| Teaching status | ||
| Major teaching | 252 (5.6%) | 15.87 (1.03) |
| Minor teaching hospital | 912 (20.4%) | 15.18 (0.88) |
| Non-teaching | 3310 (74.0%) | 15.20 (0.73) |
| Cardiac procedure capacity | ||
| CABG capability | 1100 (24.6%) | 15.24 (0.96) |
| Cardiac catheterization capability | 677 (15.1%) | 15.27 (0.84) |
| Neither | 2697 (60.3%) | 15.22 (0.71) |
| Metropolitan status | ||
| Large central metropolitan | 731 (16.3%) | 15.46 (1.02) |
| Large fringe metropolitan | 664 (14.8%) | 15.37 (0.85) |
| Medium metropolitan | 686 (15.3%) | 15.07 (0.87) |
| Small metropolitan | 461 (10.3%) | 15.07 (0.80) |
| Micropolitan | 822 (18.4%) | 15.15 (0.68) |
| Non-core (rural) | 1110 (24.8%) | 15.23 (0.55) |
| Census region | ||
| East North Central | 700 (15.7%) | 15.18 (0.79) |
| East South Central | 375 (8.4%) | 15.42 (0.75) |
| Mid-Atlantic | 384 (8.6%) | 15.75 (1.01) |
| Mountain | 366 (8.2%) | 15.00 (0.69) |
| New England | 176 (3.9%) | 15.32 (0.80) |
| Pacific | 489 (10.9%) | 15.02 (0.73) |
| South Atlantic | 661 (14.8%) | 15.35 (0.87) |
| West North Central | 649 (14.5%) | 15.10 (0.60) |
| West South Central | 674 (15.1%) | 15.14 (0.71) |
| Bed size | ||
| 6 – 24 beds | 485 (10.8%) | 15.10 (0.47) |
| 25 – 49 beds | 1016 (22.7%) | 15.17 (0.60) |
| 50 – 99 beds | 746 (16.7%) | 15.14 (0.70) |
| 100 – 199 beds | 930 (20.8%) | 15.21 (0.85) |
| 200 – 299 beds | 533 (11.9%) | 15.28 (0.92) |
| 300 – 399 beds | 316 (7.1%) | 15.37 (0.98) |
| 400 – 499 beds | 176 (3.9%) | 15.32 (0.95) |
| 500 or more | 272 (6.1%) | 15.69 (1.11) |
| Nursing/bed ratio, mean (SD) | ||
| Quartile 1 (0.04–0.77) | 1064 (23.8%) | 15.24 (0.67) |
| Quartile 2 (0.78–1.19) | 1136 (25.4%) | 15.27 (0.75) |
| Quartile 3 (1.20–1.65) | 1144 (25.6%) | 15.21 (0.85) |
| Quartile 4 (1.66–6.67) | 1127 (25.2%) | 15.21 (0.90) |
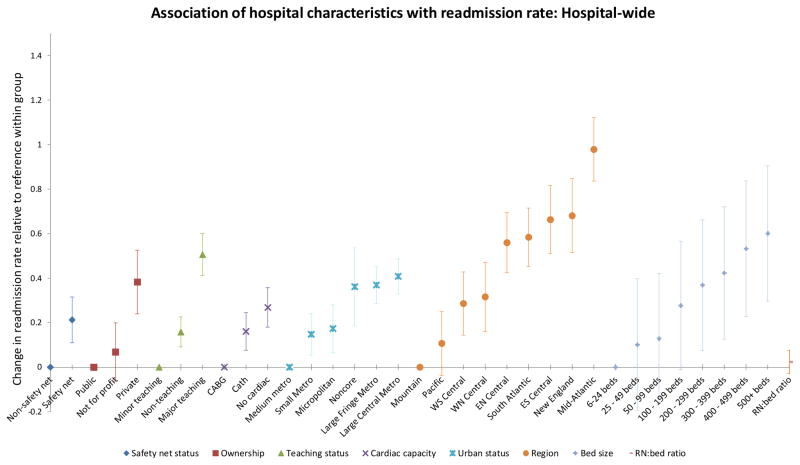
All hospital characteristics were also significantly associated with RSRR in multivariable analysis (Table 3, Figure 1). In multivariate analysis, RSRRs varied most by region, with hospitals in the mid-Atlantic region having RSRRs on average 0.98 percentage points higher than those in the Mountain region (95% CI, 0.84–1.12): 1 excess readmission per 102 discharges. Hospital RSRRs also varied significantly by population density: hospitals in either large metropolitan regions or in more rural areas had significantly higher RSRRs than hospitals in medium metropolitan areas (counties in metropolitan statistical areas with populations of 250,000 to 999,999). Major teaching hospitals had an average RSRR 0.35 percentage points higher than non-teaching hospitals (95% CI, 0.24–0.46; 1 excess readmission for every 286 discharges), and 0.51 percentage points higher than minor teaching hospitals (95% CI, 0.41, 0.60; 1 excess readmission for every 196 discharges). Safety net hospitals had an average RSRR 0.21 percentage points higher than non-safety net hospitals (95% CI, 0.11–0.32; 1 excess readmission for every 476 discharges), but for profit hospitals had an average RSRR 0.38 percentage points higher than public hospitals (95% CI, 0.24–0.53; 1 excess readmission for every 263 discharges). Nursing staff ratio was not associated with RSRR.
Table 3.
Association of hospital characteristics with RSRR, multivariable analysis
| Characteristic | Parameter estimate (95% CI) | P value |
|---|---|---|
| Safety net status | <.0001 | |
| Safety net hospital | 0.21 (0.11, 0.32) | |
| Non-safety net hospital | REF | |
| Ownership | <.0001 | |
| Not for profit | 0.07 (−0.06, 0.20) | |
| For profit | 0.38 (0.24, 0.53) | |
| Public | REF | |
| Teaching status | <.0001 | |
| Major teaching | 0.51 (0.41, 0.60) | |
| Non-teaching | 0.16 (0.09, 0.23) | |
| Minor teaching hospital | REF | |
| Cardiac procedure capability | <.0001 | |
| Neither | 0.27 (0.18, 0.36) | |
| Cardiac catheterization capability | 0.16 (0.08, 0.25) | |
| CABG capability | REF | |
| Metropolitan status | <.0001 | |
| Small metropolitan | 0.15 (0.05, 0.24) | |
| Micropolitan | 0.17 (0.07, 0.28) | |
| Non-core (rural) | 0.36 (0.19, 0.54) | |
| Large Fringe Metro | 0.37 (0.29, 0.45) | |
| Large central metropolitan | 0.41 (0.33, 0.49) | |
| Medium metropolitan | REF | |
| Census region | <.0001 | |
| Pacific | 0.11 (−0.04, 0.25) | |
| West South Central | 0.29 (0.14, 0.43) | |
| West North Central | 0.32 (0.16, 0.47) | |
| East North Central | 0.56 (0.42, 0.69) | |
| South Atlantic | 0.58 (0.45, 0.71) | |
| East South Central | 0.66 (0.51, 0.82) | |
| New England | 0.68 (0.51, 0.85) | |
| Mid-Atlantic | 0.98 (0.84, 1.12) | |
| Mountain | REF | |
| Bed size | <.0001 | |
| 25 – 49 beds | 0.10 (−0.20, 0.40) | |
| 50 – 99 beds | 0.13 (−0.16, 0.42) | |
| 100 – 199 beds | 0.28 (−0.01, 0.57) | |
| 200 – 299 beds | 0.37 (0.08, 0.66) | |
| 300 – 399 beds | 0.42 (0.13, 0.72) | |
| 400 – 499 beds | 0.53 (0.23, 0.84) | |
| 500 or more | 0.60 (0.30, 0.91) | |
| 6 – 24 beds | REF | |
| Nursing/bed ratio | 0.02 (−0.03, 0.08) | 0.3699 |
Figure 1.
Difference in mean adjusted RSRR from reference level, multivariate model, overall. Error bars represent 95% confidence interval.
Analysis of hospital characteristic association with readmission rates when stratified by specialty cohort yielded very similar results overall, though with some notable exceptions (eFigure Panels A–E). Cardiac procedure capability was not a significant predictor in surgery patients. RN/bed ratio was a significant predictor for medicine, cardiovascular and neurology patients; however, increasing nurses per bed was associated with slight increases in readmission rate in medicine and neurology patients, and with slight decreases in cardiovascular patients (eTable A). Finally, analysis of hospital characteristic association with readmission rates without adding race and dual eligibility status (i.e. using the measure as publicly reported) did not materially change the results (eTables B, C).
Discussion
We identified a number of system-level characteristics that are associated with risk-standardized readmission rates in the general hospital population. Geographic variation was more marked than variation by hospital characteristics. Moreover, variation within hospitals of a particular type (i.e., non-profit hospitals) was generally larger than differences between types. Moreover, the magnitude of differences in readmission rates was relatively small: generally less than half a percentage point except for regional variation. Nonetheless, on an individual hospital basis, these differences may be meaningful from a reporting and policy standpoint given the current penalty structure and the narrow range of risk-standardized performance.
Consistent with many other studies of regional differences in outcomes, we observed substantial differences in readmission rates by geographic region.16 Other studies have demonstrated the importance of local practice patterns in readmission rates. For example, one such study found that propensity to admit is associated with readmission rates,17 suggesting that efforts to change local standards of practice may be important mechanisms of reducing readmission rates nationally. Another study found that increased numbers of primary care physicians in the locality was strongly related to lower hospital readmission rates, highlighting the importance of healthcare access and capacity.18 The regions with low readmission rates in this study are similar to regions found in other studies to have improved access and lower healthcare utilization in general.
Hospital readmission rates appear to have fallen significantly only after the announcement of financial penalties by Medicare for excess readmission rates, suggesting that hospitals are sensitive to financial incentives, and that insurers’ efforts to alter the business case for reducing readmissions have been a valuable policy lever.19–21 In this study, however, we found that for-profit hospitals had higher readmission rates than non-profit and public hospitals. This might suggest that the current penalty structure is insufficient to induce hospitals to avoid revenue-generating readmissions in order to avoid relatively small financial penalties.22,23 It might, however, also be a consequence of different quality of care at such hospitals. We cannot distinguish between the two potential explanations; however, a future study examining whether readmission rates at for-profit hospitals facing substantial penalties fall more rapidly than non-profit hospitals facing similar penalties would help to disentangle these effects.
Several studies have found an association between increased RN staffing ratios and reduced readmission rates, including a study of heart failure alone,7 a study of medical-surgical patients at a group of four hospitals,24 and a study of surgical patients in four states.8 By contrast, we did not find an association of nurse staffing ratios with readmission rates overall, and observed inconsistent effects within specialty cohorts that did not correlate well with expected nursing needs. It may be that the ways in which nurses are deployed in terms of delivering patient care and education are more important than the absolute ratio of nurses to patients.
On an unadjusted basis, hospitals with advanced cardiac surgery capability had higher readmission rates than those without. However, after adjustment for other hospital structural characteristics, we observed that readmission rates were substantially lower at hospitals with advanced cardiac surgery capability, perhaps because more experience with procedures improves outcomes. Surprisingly, however, this variable was not associated with reduced readmission risk in the surgery cohort, and even in the cardiovascular cohort, the effect size was smaller than in medicine and cardiorespiratory cohorts, whose patients generally do not undergo cardiac procedures. It is likely therefore that this variable is serving as a proxy for some other hospital characteristic, such as advanced radiology capacity, rather than as a causal factor.
A notable finding is that major teaching hospitals (representing <6% of the sample) had readmission rates 0.35 points higher on average than non-teaching hospitals and 0.51 points higher on average than minor teaching hospitals. Of note, variability among major teaching hospitals was even greater: the standard deviation of performance among major teaching hospitals was 1.03 points. Nonetheless, other studies have noted a disproportionate penalty rate among major teaching hospitals in the federal Hospital Readmission Reduction Program, a reflection of the policy relevance of even small differences.6 This small average difference may be a consequence of confounding unmeasured patient risk, for example from transferred patients. In this study, we did adjust for race and dual eligibility status, which are not included in the quality measurement, but could in part represent unmeasured clinical and social risk factors that may be distributed differently across hospitals.25–27 These differences could also be due to different care by trainees, who may not yet have an appreciation of the importance of transitions in care;28,29 and/or competing mortality risk, since teaching hospitals tend to be larger, and high volume centers generally have lower mean 30-day mortality.30,31 Previous studies, however, have not found strong associations between mortality and readmission rates.32
Our findings should be considered in light of study limitations. All our analyses are cross-sectional in nature and cannot establish causality; the characteristics we measured may be proxies for other, unmeasured, hospital characteristics and may not have any causal relationship with readmission. We could not account for all patient-level risk factors, including education, income, function, cognition, social support and other factors, which may differ systematically at different types of hospitals. We apply the risk-standardization approach used in public reporting, which creates more stable estimates for small hospitals and is more policy relevant, but makes it difficult to distinguish differences in performance by size. Finally, we use only fee-for-service Medicare data; results for managed Medicare, commercially-insured or younger patients may be different.
Overall, we find risk-standardized hospital-wide readmission rates to vary somewhat by hospital characteristics, with generally larger, urban, academic facilities faring worse than smaller, suburban, community hospitals. There was a strong regional effect, suggesting that local practice patterns are an important influence on hospital readmissions. However, differences within groups were relatively small.
Supplementary Material
Acknowledgments
Financial support: This work was performed under contract HHSM-500-2013-13018I-T0001 Modification 000002, entitled “Measure Instrument Development and Support,” funded by CMS, an agency of the US Department of Health and Human Services. This work was also supported by the Agency for Healthcare Research and Quality (R01HS022882). Drs. Horwitz and Ross were supported by the National Institute on Aging (K08 AG038336 and K08 AG032886, respectively) and by the American Federation for Aging Research through the Paul B. Beeson Career Development Award Program at the time this work was performed. Dr. Krumholz is supported by grant U01 HL105270-04 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute. No funding source had any role in the study design; in the collection, analysis, and interpretation of data; or in the writing of the report. The CMS reviewed and approved the use of its data for this work and approved submission of the manuscript.
Footnotes
Conflicts of Interest: All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare that all authors have support from the Centers for Medicare & Medicaid Services for the submitted work. In addition, Dr. Ross is a member of a scientific advisory board for FAIR Health Inc. Dr. Krumholz chairs a cardiac scientific advisory board for UnitedHealth and is the recipient of research grants from Medtronic and Johnson&Johnson through Yale University. All other authors report no conflicts of interest.
References
- 1.Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306(15):1688–1698. doi: 10.1001/jama.2011.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tsai TC, Joynt KE, Orav EJ, Gawande AA, Jha AK. Variation in surgical-readmission rates and quality of hospital care. N Engl J Med. 2013;369(12):1134–1142. doi: 10.1056/NEJMsa1303118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berry JG, Toomey SL, Zaslavsky AM, et al. Pediatric readmission prevalence and variability across hospitals. JAMA. 2013;309(4):372–380. doi: 10.1001/jama.2012.188351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Horwitz LI, Partovian C, Lin Z, et al. Development and use of an administrative claims measure for profiling hospital-wide performance on 30-day unplanned readmission. Ann Intern Med. 2014;161(10 Suppl):S66–75. doi: 10.7326/M13-3000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Donabedian A. The quality of care. How can it be assessed? JAMA. 1988;260(12):1743–1748. doi: 10.1001/jama.260.12.1743. [DOI] [PubMed] [Google Scholar]
- 6.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. JAMA. 2013;309(4):342–343. doi: 10.1001/jama.2012.94856. [DOI] [PubMed] [Google Scholar]
- 7.Joynt KE, Jha AK. Who has higher readmission rates for heart failure, and why? Implications for efforts to improve care using financial incentives. Circ Cardiovasc Qual Outcomes. 2011;4(1):53–59. doi: 10.1161/CIRCOUTCOMES.110.950964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ma C, McHugh MD, Aiken LH. Organization of Hospital Nursing and 30-Day Readmissions in Medicare Patients Undergoing Surgery. Med Care. 2015;53(1):65–70. doi: 10.1097/MLR.0000000000000258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Horwitz LI, Lin Z, Herrin J, et al. Association of hospital volume with readmission rates: a retrospective cross-sectional study. BMJ. 2015;350:h447. doi: 10.1136/bmj.h447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Horwitz L, Partovian C, Lin Z, et al. [Accessed 28 August, 2013];Hospital-wide all-cause unplanned readmission measure: Final technical report. 2012 https://www.qualitynet.org/dcs/ContentServer?cid=1219069855273&pagename=QnetPublic%2FPage%2FQnetTier3&c=Page.
- 11.Horwitz LI, Partovian C, Lin Z, et al. [Accessed 3 June, 2015];Centers for Medicare & Medicaid Services Planned Readmission Algorithm – Version 2.1. 2013 http://hscrc.maryland.gov/documents/HSCRC_Initiatives/readmissions/Version-2-1-Readmission-Planned-CMS-Readmission-Algorithm-Report-03-14-2013.pdf.
- 12.Horwitz LI, Grady JN, Cohen DB, et al. Development and Validation of an Algorithm to Identify Planned Readmissions From Claims Data. J Hosp Med. 2015;10(10):670–677. doi: 10.1002/jhm.2416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ross JS, Cha SS, Epstein AJ, et al. Quality of care for acute myocardial infarction at urban safety-net hospitals. Health Aff (Millwood) 2007;26(1):238–248. doi: 10.1377/hlthaff.26.1.238. [DOI] [PubMed] [Google Scholar]
- 14.Gilman M, Adams EK, Hockenberry JM, Milstein AS, Wilson IB, Becker ER. Safety-net hospitals more likely than other hospitals to fare poorly under Medicare’s value-based purchasing. Health Aff (Millwood) 2015;34(3):398–405. doi: 10.1377/hlthaff.2014.1059. [DOI] [PubMed] [Google Scholar]
- 15.National Center for Health Statistics. [Accessed 2013, 6 Sept];NCHS Urban-Rural Classification Scheme for Counties. 2006 http://www.cdc.gov/nchs/data_access/urban_rural.htm.
- 16.Dartmouth Atlas Project, PerryUndem Research & Communications. The Revolving Door: A Report on US Hospital Readmissions. Robert Wood Johnson Foundation; 2013. [Accessed 11 Sep 2015]. http://www.rwjf.org/content/dam/farm/reports/reports/2013/rwjf404178. [Google Scholar]
- 17.Epstein AM, Jha AK, Orav EJ. The relationship between hospital admission rates and rehospitalizations. N Engl J Med. 2011;365(24):2287–2295. doi: 10.1056/NEJMsa1101942. [DOI] [PubMed] [Google Scholar]
- 18.Herrin J, St Andre J, Kenward K, Joshi MS, Audet AM, Hines SC. Community factors and hospital readmission rates. Health Serv Res. 2015;50(1):20–39. doi: 10.1111/1475-6773.12177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gerhardt G, Yemane A, Hickman P, Oelschlaeger A, Rollins E, Brennan N. Medicare readmission rates showed meaningful decline in 2012. Medicare and Medicaid Research Review. 2013;3(2):E1–E12. doi: 10.5600/mmrr.003.02.b01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carey K, Lin MY. Readmissions To New York Hospitals Fell For Three Target Conditions From 2008 To 2012, Consistent With Medicare Goals. Health Aff (Millwood) 2015;34(6):978–985. doi: 10.1377/hlthaff.2014.1408. [DOI] [PubMed] [Google Scholar]
- 21.Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, Observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016;374(16):1543–1551. doi: 10.1056/NEJMsa1513024. [DOI] [PubMed] [Google Scholar]
- 22.Burgess JF, Hockenberry JM. Can all cause readmission policy improve quality or lower expenditures? A historical perspective on current initiatives. Health Econ Policy Law. 2014;9(2):193–213. doi: 10.1017/S1744133113000340. [DOI] [PubMed] [Google Scholar]
- 23.Gilman M, Hockenberry JM, Adams EK, Milstein AS, Wilson IB, Becker ER. The Financial Effect of Value-Based Purchasing and the Hospital Readmissions Reduction Program on Safety-Net Hospitals in 2014: A Cohort Study. Ann Intern Med. 2015;163(6):427–436. doi: 10.7326/M14-2813. [DOI] [PubMed] [Google Scholar]
- 24.Weiss ME, Yakusheva O, Bobay KL. Quality and cost analysis of nurse staffing, discharge preparation, and postdischarge utilization. Health Services Research. 2011;46(5):1473–1494. doi: 10.1111/j.1475-6773.2011.01267.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Frick AP, Martin SG, Shwartz M. Case-mix and cost differences between teaching and nonteaching hospitals. Med Care. 1985;23(4):283–295. doi: 10.1097/00005650-198504000-00001. [DOI] [PubMed] [Google Scholar]
- 26.Goldfarb MG, Coffey RM. Case-mix differences between teaching and nonteaching hospitals. Inquiry. 1987;24(1):68–84. [PubMed] [Google Scholar]
- 27.Shahian DM, Liu X, Meyer GS, Normand SL. Comparing teaching versus nonteaching hospitals: the association of patient characteristics with teaching intensity for three common medical conditions. Acad Med. 2014;89(1):94–106. doi: 10.1097/ACM.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 28.Greysen SR, Schiliro D, Horwitz LI, Curry L, Bradley EH. “Out of sight, out of mind”: Housestaff perceptions of quality-limiting factors in discharge care at teaching hospitals. J Hosp Med. 2012 doi: 10.1002/jhm.1928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Greysen SR, Schiliro D, Curry L, Bradley EH, Horwitz LI. “Learning by Doing”-Resident Perspectives on Developing Competency in High-Quality Discharge Care. J Gen Intern Med. 2012 doi: 10.1007/s11606-012-2094-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taylor DH, Jr, Whellan DJ, Sloan FA. Effects of admission to a teaching hospital on the cost and quality of care for Medicare beneficiaries. N Engl J Med. 1999;340(4):293–299. doi: 10.1056/NEJM199901283400408. [DOI] [PubMed] [Google Scholar]
- 31.Allison JJ, Kiefe CI, Weissman NW, et al. Relationship of hospital teaching status with quality of care and mortality for Medicare patients with acute MI. JAMA. 2000;284(10):1256–1262. doi: 10.1001/jama.284.10.1256. [DOI] [PubMed] [Google Scholar]
- 32.Krumholz HM, Lin Z, Keenan PS, et al. Relationship between hospital readmission and mortality rates for patients hospitalized with acute myocardial infarction, heart failure, or pneumonia. JAMA. 2013;309(6):587–593. doi: 10.1001/jama.2013.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.