Summary:
The magnetic intramedullary lengthening nail is an innovative technology that allows for creative ways to treat difficult problems. The lengthening option has revolutionized femur fracture management with bone loss and malunion therapy. The compression version of this nail has provided a gradual method to compress nonunions and difficult fractures that may obviate the need for many current uses of external fixation. Three cases are presented in this manuscript demonstrating a new paradigm in the management of bone loss/shortening of the tibia and femur, and recalcitrant nonunions.
Key Words: internal lengthening nail, PRECICE UNYTE, compression nail, nonunion, malunion
The magnetic intramedullary (IM)-lengthening nail has rapidly gained popularity in the pediatric orthopedic community.1,2 Although this technique is just as effective in adults with posttraumatic limb shortening,3 the orthopedic trauma community has been slow to integrate the intramedullary lengthening nail (ILN) into fracture care. Perhaps the inconstant experience with the ISKD (Intramedullary Skeletal Kinetic Distractor; Orthofix, Lewisville, TX) discouraged surgeons from using any ILN.4 The newer technology realized in the magnetic-actuated version of the ILN has made this implant extremely reliable.5 In the field of trauma, the ILN is typically used for tibia or femur lengthening after a malunion.6 Deformity can be corrected simultaneously through the osteotomy site to both realign and lengthen the femur without negative effects on the regenerate.7 This may also be performed in the tibia, but the risks are higher (compartment syndrome, peroneal nerve injury, delayed union). Ideal timing for lengthening in acute trauma with bone loss is not established.
A further innovation has been the internal compression nail (ICN) which is the same implant (ILN) used differently: to compress fracture fragments. The ILN is predistracted 10 mm in its sterile packaging, is inserted into the bone, and is then compressed externally. This has potentially powerful applications in acute fracture care, nonunion repair, and ankle/knee fusion surgery. Improvements in compression technology for IM nails before ICN have provided strong compression intraoperatively8 but have not allowed for any postoperative compressibility. Until recently, the only way to achieve postoperative compression was with an external fixator. The ICN offers the advantages of internal fixation with the dynamic dimension of external fixation, specifically postoperative compressibility. The question remains: which fractures and nonunions need to be treated with an ICN, and which can heal with simpler implants?
Why switch to an ILN or ICN when the current system of external fixation, now with hexapod technology, is so effective? Part of the answer to this question is the obvious benefit of not having to wear an external fixator. When compared with external fixation, the ILN provides a lower complication rate9 and greater patient comfort.10 The absence of pin sites means no pin infections, which has positive implications for a reduced need for antibiotics, less antibiotic resistance, and less damage to the intestinal microbiota. Greater patient comfort is primarily a function of less pain. A reduction in the need for narcotic medication by switching to internal fixation may reduce opioid abuse and opioid-related death, now national priorities.11 Studies have shown that femur lengthening with the ILN has produced the fastest healing seen with bone healing indices superior to historical controls using external fixation.6,12 External fixation requires specialized clothing or the modification of existing clothing, makes travel more difficult, and causes damage to a patient's home, inconveniences that are avoided with an all-internal technique.
This manuscript presents a new way of thinking about common problems faced in orthopedic trauma surgery while improving results and the patient experience.
CASE 1
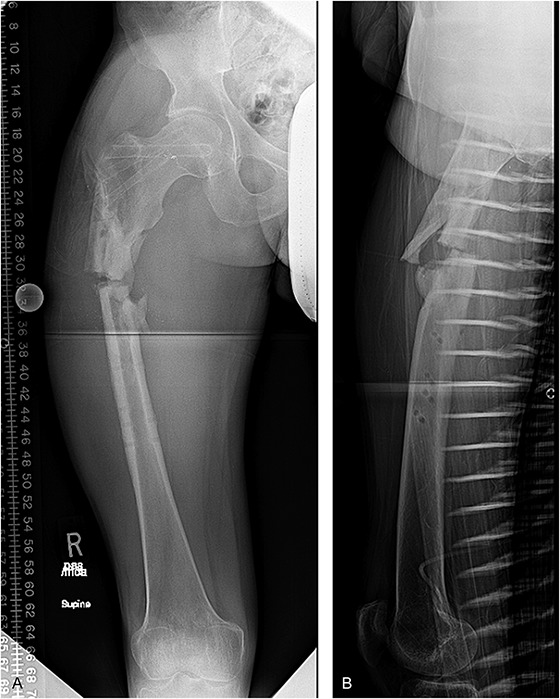
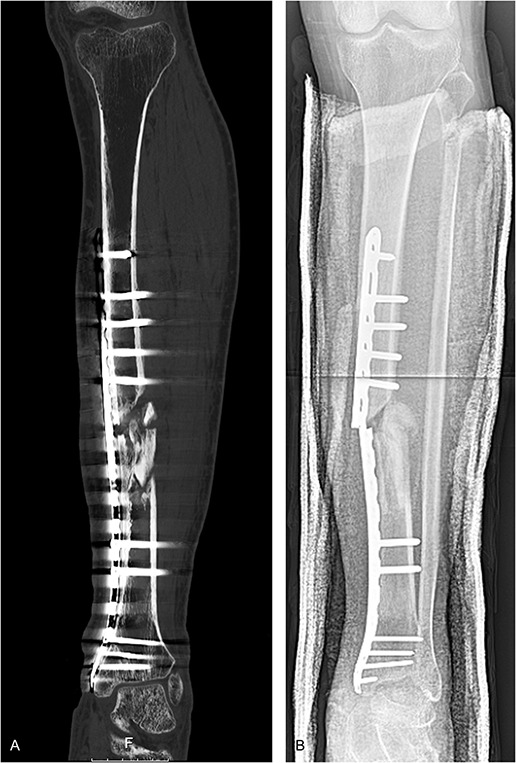
A 26-year-old female was a driver in a head-on collision at moderate speed in an urban setting. She had no medical problems, except obesity (BMI 34.3), and sustained a displaced, closed, right tibial plateau fracture (Schatzker 6)13 and an open middiaphyseal fracture (Gustilo-Anderson grade IIIA)14 with a 14 cm transverse laceration, contamination, and bone loss. She was stabilized with fracture debridement, temporary external fixation, and vacuum assisted wound coverage (Figs. 1A, B). A CT scanogram showed a 5 cm leg length discrepancy.
FIGURE 1.

A and B, CT reconstructions allowed for intraarticular surgical planning.
The trauma team performed a delayed open reduction and plating of the plateau fracture and felt that internal fixation of the diaphyseal fracture was not ideal due to the severity of the soft tissue injury. During the same procedure, a hexapod external fixator was placed, and the diaphyseal fracture bone ends were acutely shortened and compressed, which assisted with the wound closure. Continued compression was applied postoperatively to aid in fracture healing (Figs. 2A, B).
FIGURE 2.
A and B, AP and lateral radiographs.
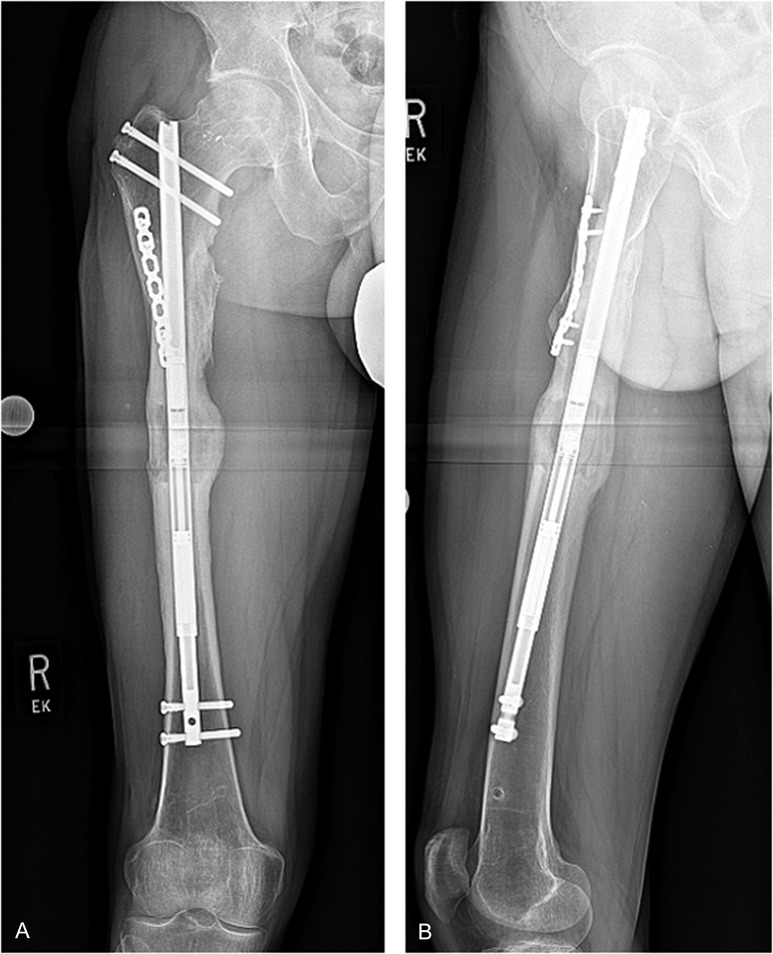
Options for recovering the 5 cm of bone loss included modification of the external fixator by adding an additional ring and performing a lengthening osteotomy, or use of the ILN, to achieve the same length restoration. The patient had a large leg at baseline and now had additional swelling with pin irritation. She was not tolerating the external fixator very well due to pain. She would likely not tolerate a lengthening procedure with pins and wires cutting through the skin. She remained nonweight-bearing for 10 weeks due to the tibial plateau fracture. The tibia fracture was then followed with monthly radiographs, and the frame (external fixator) was removed after 97 days. She recovered for another 3 months with progressive weight-bearing. After the sixth postoperative month, the proximal tibial hardware was removed, tibia and fibula osteotomies were performed, and the PRECICE (NuVasive Specialized Orthopedics, Aliso Viejo, CA) ILN was inserted. The use of internal fixation after circular external fixation put the patient at risk for a deep infection. Insertion of an IM nail at the time of frame removal after femoral lengthening with external fixation was found to carry a 7% infection rate despite the average time in the frame of 184 days.15 The lengthening and then nailing technique (LATN)16 discusses conversion from external to internal fixation, and carries a very low infection rate. This patient never had a deep or superficial infection, pin loosening, or nonunion, making internal lengthening a low-risk option (Figs. 3A, B).
FIGURE 3.
A, The ILN was lengthened according to the following schedule: a 7-day latency, then nail distraction using an external magnet at 0.25 mm 4 times a day for 4 days, then slowing to 0.25 mm 3 times a day until completion of the desired length. She was followed every 14 days with physical examination and radiographs and was kept protective weight bearing at 50 lbs. B, The patient is close to the end of the distraction period.
She was fully consolidated after 7 months yielding a consolidation index of 1.4 months/cm. She recovered her length and full knee and ankle mobility. She did not suffer from any infection or complication, and her pain was well controlled with low-dose opioids during the lengthening process (Figs. 4A, B).
FIGURE 4.
A, This AP radiograph after 5.5 months show near-equal limb lengths and partial cortical bridging allowing full weight bearing. B, This lateral radiograph at 12 months shows full consolidation.
In summary, the ILN provided this patient with an excellent result and minimized postoperative discomfort. The infection risk was low. This approach required more time than an all-external technique, and will require the additional surgery of syndesmotic screw and ILN removal in the future.
CASE 2
A 35-year-old male sustained a refracture of the proximal femur while walking down the street. Two years earlier he was involved in a motor vehicle accident where his right proximal femur was fractured with comminution and was fixed with a plate and screws. His fracture healed, and the surgeon removed the hardware for what was believed to be hardware-related pain. Two months after hardware removal, his leg gave out. Radiographs revealed a proximal femur diaphyseal fracture with displacement through sclerotic bone (Figs. 5A, B). He was placed in traction and a CT scan, obtained for surgical planning, provided detail on the extent of poorly vascularized bone at the fracture site. The extent of bone resection would be determined intraoperatively by visualizing the bony vascularity.
FIGURE 5.
A and B, AP and lateral radiographs showing the fracture through thinned-sclerotic bone. Planning for the second surgery included plans for a resection of the poorly vascularized bone at the fracture site which would create a limb length discrepancy.
The knowledge that this patient would have a limb lengthening discrepancy in the future influenced the treatment selected for the refracture. The use of a blade plate to gain proximal bony union would later require either plate removal or the use of a retrograde ILN. To contain the surgical site to proximal femur, an IM nail was used to fix the fracture with augmentation using a unicortical locking plate. Nonviable bone was resected in surgery, and tissue cultures were negative (Fig. 6). While keeping the patient 30 lbs weight bearing, the fracture healed after 5 months.
FIGURE 6.
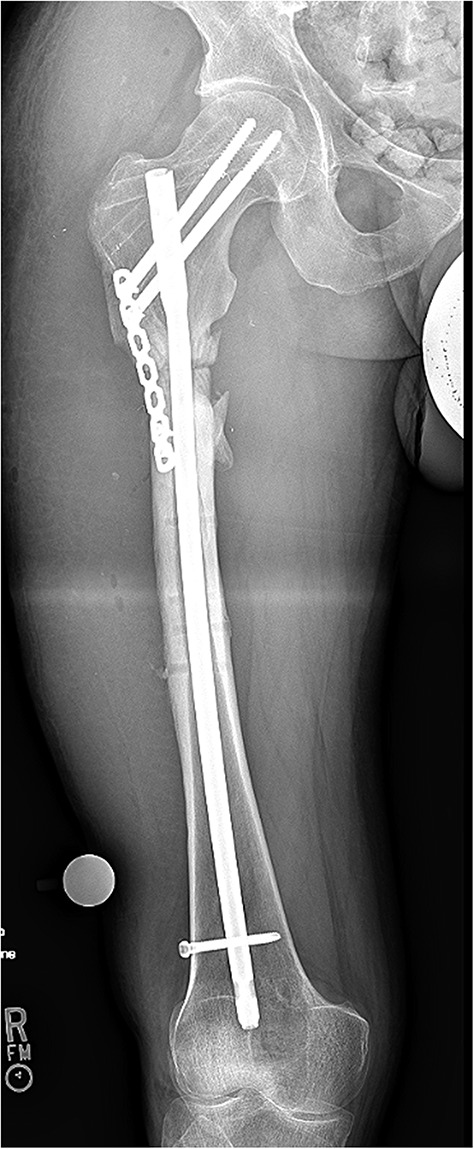
AP radiograph soon after fixation. A trochanteric IM nail was used through a piriformis entry point to prevent against varus angulation at the fracture site.
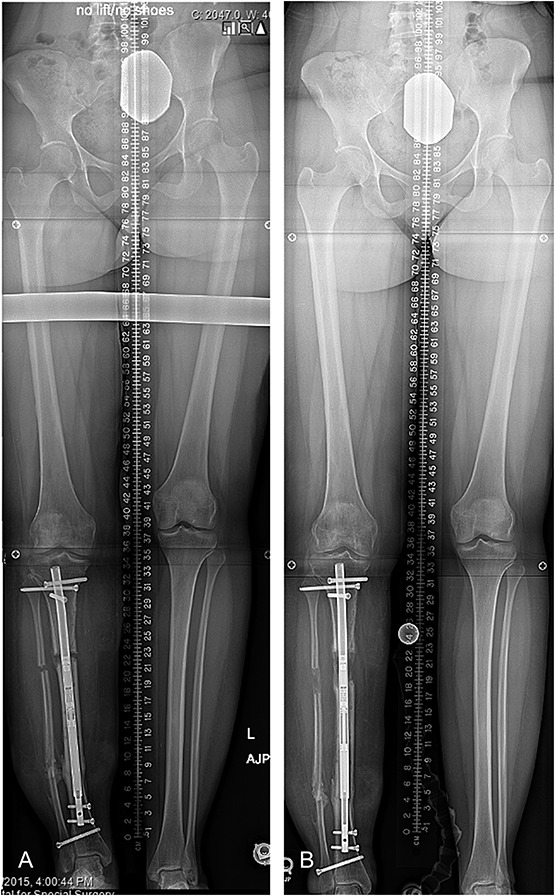
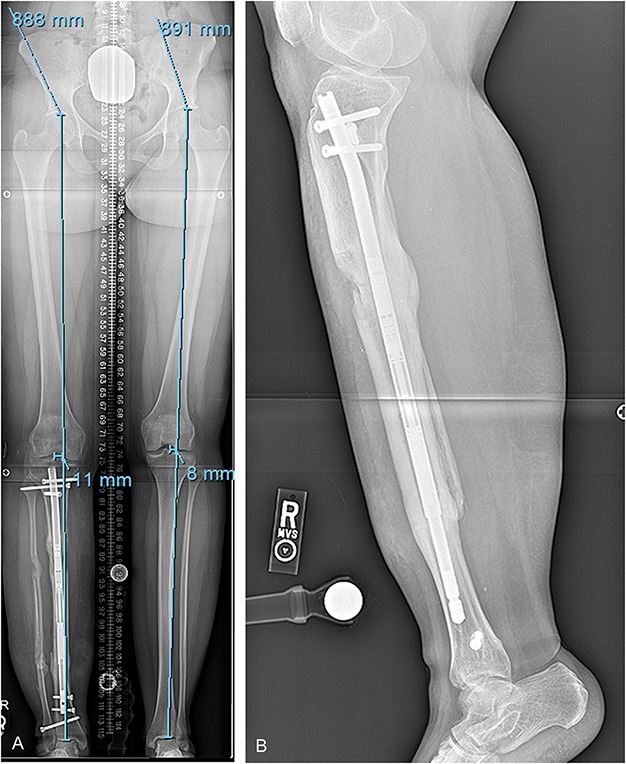
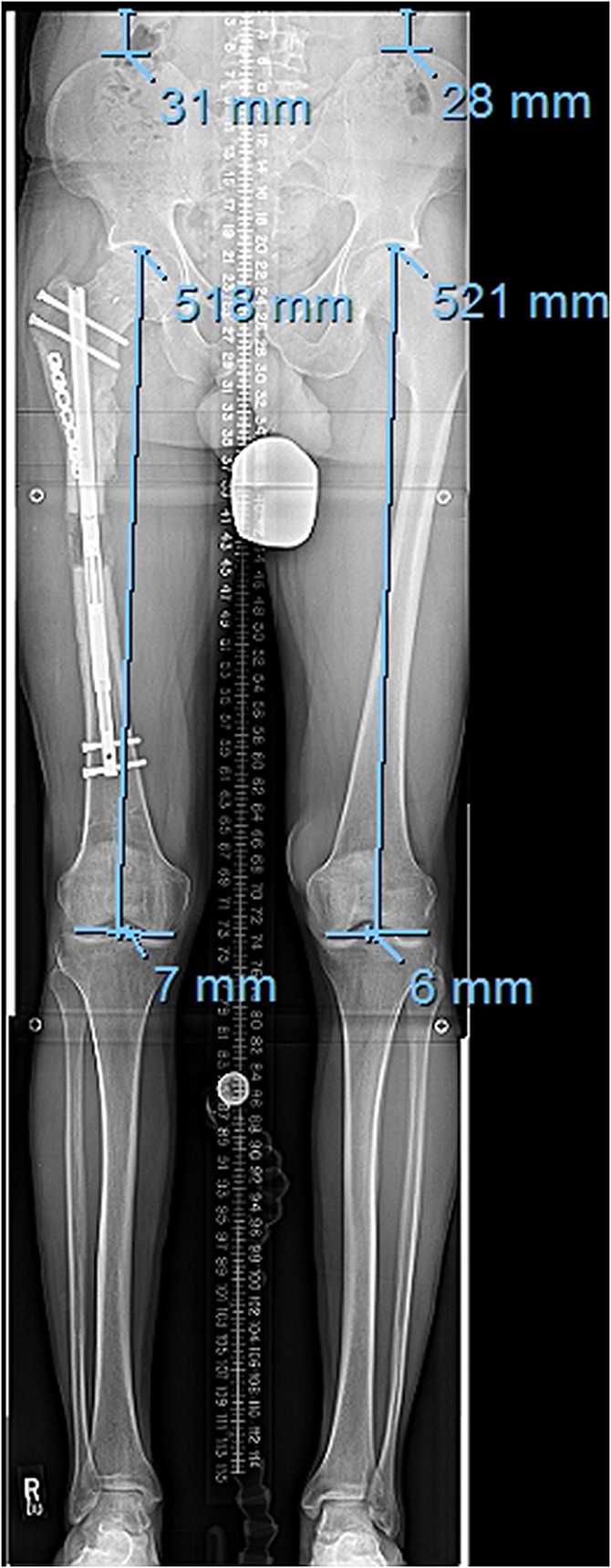
The preoperative planning for the ILN included creating an osteotomy distal to the unicortical plate in healthy bone, exchanging the reconstruction nail with a ILN, and retaining the unicortical plate (Fig. 7). The surgery was minimally invasive and used the same osseous passage for the PRECICE nail (Fig. 8). Once the desired length was achieved, bone consolidation ensued (Fig. 9). After 2.5 months, 2 cortices of bridging callous were seen on radiographs, and he was permitted full weight bearing (Figs. 10A, B). His consolidation index was 1.0 (4 months/4 cm).
FIGURE 7.
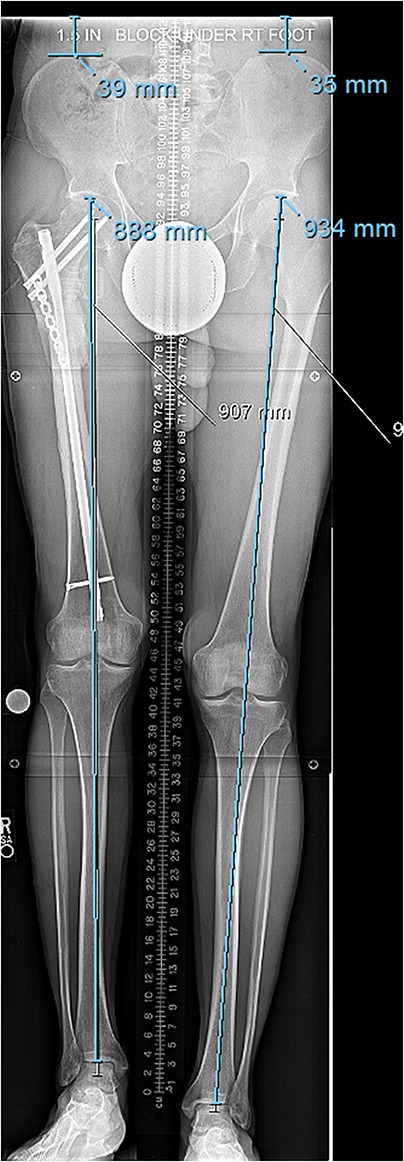
A long, standing, bipedal 51″ radiograph showed a 40–46 mm limb length discrepancy with the right side shorter.
FIGURE 8.
Lengthening ensued according to the following schedule: Four days of latency, distraction at 0.33 mm 4 times per day for 4 days, and then 0.33 mm 3 times per day for the remainder of the lengthening period. The patient was followed with bimonthly x-rays that showed normal regenerate ossification, and the distraction rate was not altered.
FIGURE 9.
A long-standing x-ray is obtained to confirm limb length and alignment at the end of distraction.
FIGURE 10.
A and B, These 8 months AP and lateral radiographs show final healing.
In summary, this case illustrates the use of an initial IM nail with the specific intention of later exchange nailing with the ILN. A trochanteric entry nail used in a piriformis entry point helped prevent varus at the fracture site.
CASE 3
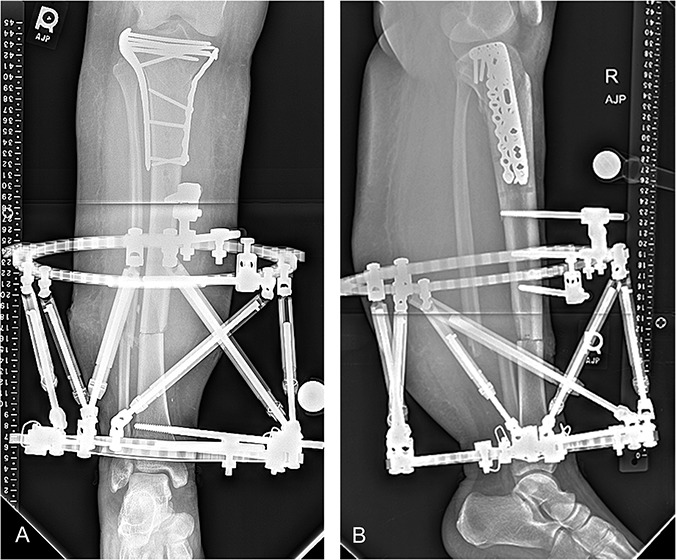
A 24-year-old male was injured in a motorcycle accident in Southeast Asia where he sustained an open, contaminated, grade 3A tibia fracture. He was treated in a major medical center in Thailand where he underwent open reduction and internal fixation. The skin over his anterior-medial leg was traumatized but viable, and was being managed by a plastic surgeon. His imaging showed a nonunion of the tibia and an intact fibula (Fig. 11A). His plate fractured soon after the CT scan (Fig. 11B). Due to the poor pretibial skin and suspected indolent infection he was treated with a bone debridement, hardware removal, and circular external fixation. An estimated 15 mm of bone was removed to leave only viable tissues. Intraoperative tissue cultures were all negative. The frame was compressed both intraoperatively (5 mm) and postoperatively (1 mm at each office visit) to provide an ideal environment for bone healing. He was encouraged to weight bear, as tolerated, which he could do after 6 weeks. He was followed at monthly intervals with slow progression of healing. At the 6-month visit, the nonunion had created some callus and the frame was noted to be loosening (Fig. 12). The decision was made to remove the frame and treat him in a cast (Fig. 13).
FIGURE 11.
A, A CT scan done 6 months after the injury showed an atrophic nonunion with canal blockage by bone fragments. B, Radiographs taken 2 weeks after the CT scan showed hardware failure.
FIGURE 12.
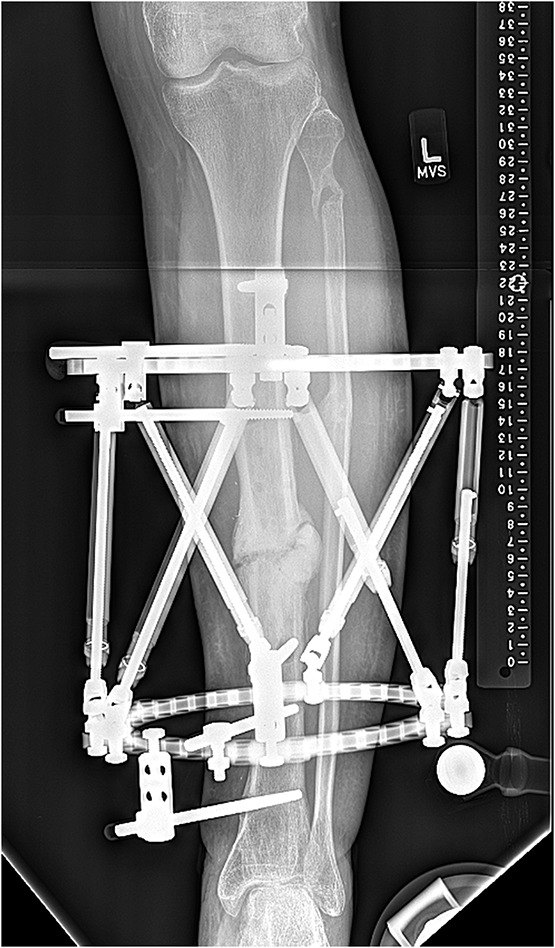
This AP radiograph taken 5.5 months after frame application showed callus formation.
FIGURE 13.

The radiograph at the time of frame removal showed widened pin holes and a hypertrophic partial union.
The tibia collapsed 6 weeks later in the cast. The treatment selected was the ICN. The nonunion was repaired percutaneously to avoid opening the chronically traumatized pretibial skin. The UNYTE ICN was compressed (Fig. 14). He was discharged 50% weight bearing. He was seen to have a purulent swelling on the next visit and was brought to the operating room for urgent debridement. The nonunion site was washed out, absorbable antibiotic beads were inserted, and the hardware was retained. Culture-specific antibiotics were given intravenously (Cefazolin for Methicillin Sensitive Staph Aureus) for 6 weeks, and suppressive oral antibiotics (Rifampin and Cephalexin) were continued for another 6 weeks. A CT scan, done 3 months after the ICN insertion, showed complete union of the posterior and lateral cortices. He could return to full weight bearing and low-impact activities. At latest follow-up (5 months post-ICN insertion) he had no pain, no signs of infection, and was off all antibiotics (Figs. 15A, B).
FIGURE 14.

Compression was done according to the following schedule: 2 mm postoperative day 1, 2 mm postoperative day 2, and 1 mm postoperative day 3. This protocol was invented to resemble the frame compression schedule we had become accustomed to.
FIGURE 15.
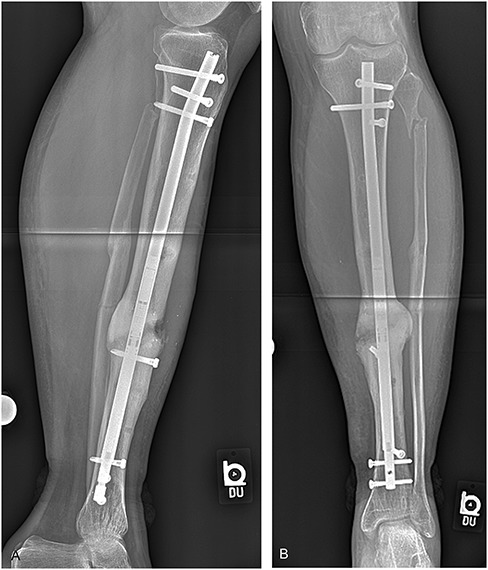
A and B, AP and lateral radiographs taken 6 months after ICN insertion show nearly full consolidation.
In summary, the ICN was able to achieve the union that plating and circular fixation could not. The price was a deep infection which resolved with local treatment and nail retention. Most likely, the loose pin sites were contaminated and seeded the canal, despite a 6-weeks “frame holiday.” An antibiotic cement-coated nail could have been inserted to sterilize the canal before a staged ICN insertion.17 In my practice, the use of the ICN has been limited to recalcitrant nonunions where standard techniques have a high likelihood of failing.
Footnotes
A. T. Fragomen is a consultant for NuVasive, Smith and Nephew, and Synthes, where he works on physician education.
REFERENCES
- 1.Paley D. Precice intramedullary limb lengthening system. Expert Rev Med Devices. 2015;12:231–249. [DOI] [PubMed] [Google Scholar]
- 2.Rozbruch SR, Birch JG, Dahl MT, et al. Motorized intramedullary nail for the management of limb-length discrepancy and deformity. J Am Acad Orthop Surg. 2014;22:403–409. [DOI] [PubMed] [Google Scholar]
- 3.Baumgart R, Betz A, Schweiberer L. A fully implantable motorized intramedullary nail for limb lengthening and bone transport. Clin Orthop. 1997;343:135–143. [PubMed] [Google Scholar]
- 4.Lee DH, Ryu KJ, Song HR, et al. Complications of the skeletal kinetic distractor (ISKD) in distraction osteogenesis. Clin Orthop Relat Res. 2014;472:3852–3859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kirane Y, Fragomen A, Rozbruch SR. Precision of the PRECICE internal bone lengthening nail. Clin Orthop Rel Res. 2014;472:3869–3878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kucukkaya M, Karakoyun O, Erol MF. The importance of reaming the posterior femoral cortex before inserting lengthening nails calculation of the amount of reaming. J Orthop Surg Res. 2016;11:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karakoyun Ö, Küçükkaya M, Erol MF. Does lengthening after acute correction negatively affect bone healing during distraction osteogenesis? Acta Orthop Traumatol Turc. 2015;49:405–409. [DOI] [PubMed] [Google Scholar]
- 8.Fenton P, Qureshi F, Bejjanki N, et al. Management of non-union of humeral fractures with the stryker T2 compression nail. Arch Orthop Trauma Surg. 2011;131:79–84. [DOI] [PubMed] [Google Scholar]
- 9.Black SR, Kwon MS, Cherkashin AM, et al. Lengthening in congenital femoral deficiency: a comparison of circular external fixation and a motorized intramedullary nail. J Bone Joint Surg Am. 2015;97:1432–1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Landge V, Shabtai L, Gesheff M, et al. Patient satisfaction after limb lengthening with internal and external devices. J Surg Orthop Adv. 2015;24:174–179. [PubMed] [Google Scholar]
- 11.Kissin I. Opioid prescriptions for pain and epidemic of overdose death: can the dramatic reduction in anesthesia mortality serve as an example? J Pain Res. 2016;9:453–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Al-Sayyad MJ. Lower limb lengthening and deformity correction using the fitbone motorized nail system in the adolescent patient. J Pediatr Orthop B. 2012;21:131–136. [DOI] [PubMed] [Google Scholar]
- 13.Schatzker J, Mcbroom R, Bruce D. The tibial plateau fracture: the toronto experience 1968–1975. Clin Orthop Relat Res. 1979;138:94–104. [PubMed] [Google Scholar]
- 14.Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984;24:742–746. [DOI] [PubMed] [Google Scholar]
- 15.Abdelgawad AA, Jauregui JJ, Standard SC, et al. Prophylactic intramedullary rodding following femoral lengthening in congenital deficiency of the femur. J Pediatr Orthop. 2015. [epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 16.Rozbruch SR, Kleinman D, Fragomen A, et al. Limb lengthening and then insertion of an intramedullary nail. A case matched comparison. Clin Orthop. 2008;466:2923–2932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Conway J, Mansour J, Kotze K, et al. Antibiotic cement-coated rods: an effective treatment for infected long bones and prosthetic joint nonunions. Bone Joint J. 2014;96-B:1349–1354. [DOI] [PubMed] [Google Scholar]