Abstract
Background:
Dupuytren disease (DD) is a fibroproliferative disorder of the palmar fasciae causing extension deficit and impaired hand function. Treatment with injection of collagenase clostridium histolyticum (CCH) is a nonsurgical treatment method. The aim of this study was to evaluate the difference in efficiency and recurrence at 12-month follow-up when treating metacarpophalangeal (MP) and proximal interphalangeal (PIP) joints with CCH. None of the patients had received previous treatments of their condition.
Methods:
This study is a prospective study of a consecutive series of patients with DD presenting with an extension deficit greater than 20° affecting the MP or PIP joint.
Results:
We found a mean reduction in extension deficit of 47° (91%) for MP joints and 47° (76%) for PIP joints. Full correction (max 5° deficit) was achieved in 76% of MP and 28% of PIP joints. Skin rupture was seen in 34% of treatments. The 1-year relapse rate was 15% for MP and 67% for PIP joints. The reduction in quickDASH score was only statistically significant for MP joints at 1 year. Eighty-one percent of all patients reported being satisfied or very satisfied. No major adverse events were recorded.
Conclusion:
Excellent results can be achieved in the treatment of MP-joint contractures, whereas the success rate is significantly lower and recurrence rate is greater for PIP joints.
Dupuytren disease (DD) is a slowly progressing fibroproliferative disorder of the palmar fasciae. Characteristic thickening of the skin, nodules, and cords causes a progressive extension deficit resulting in impaired hand function. DD is very common among Caucasians and their Northern European descendants.1
Traditionally, the preferred method of treatment has been surgical procedures such as percutaneous needle fasciectomy, limited fasciectomy, or dermofasciectomy with or without skin grafting. Surgical procedures are associated with intraoperative risk of damage to nerves, arteries, and tendons.2 Postoperative risks include infection, hematomas, and impaired wound healing. With multiple surgical interventions in the same area, the risks increase, as do the demands on the surgeon’s skills and patience.
A nonsurgical treatment with an injection of collagenase clostridium histolyticum (CCH) has been offered in recent years. This enzyme degrades and weakens a part of the cord into which it has been injected, and after injection of local anesthetics and manipulation, the extension deficit is released or diminished.
Since the introduction of CCH to the Danish market in 2011, several studies describing the effect have been published.3,4 The anatomical differences in contractures affecting the proximal interphalangeal (PIP) joint and the metacarpophalangeal (MP) joint have been suggested as a cause of different treatment potential.5
The aim of this study was to evaluate the difference in efficiency and recurrence when treating MP and PIP joints with CCH in patients with primary DD.
METHODS
Study Design and Patient Population
A prospective cohort study was conducted on a consecutive series of patients with primary DD treated at Odense University Hospital from July 2011 to the end of December 2013. The patients received no previous surgical treatment or CCH injections and were thus classified as primary DD patients. All research was carried out in compliance with the Declaration of Helsinki. The study was approved by the Danish Data Protection Agency and the regional ethics committee. All patients agreed to participate in the study, provided written informed consent, and were free to be excluded from the study at any time.
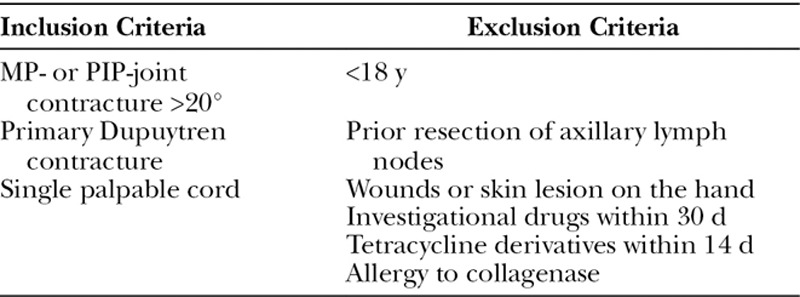
All patients presented with >20° extension deficit over one joint and a palpable cord (see Table 1). The primary endpoint was a reduction in extension deficit to 0° to 5° of full extension for a joint. PIP- and MP-joint extension deficits were evaluated separately. Secondary endpoints included patient-reported hand function using the Disabilities of the Arm, Shoulder and Hand (quickDASH) questionnaire, patient satisfaction, and recurrence of extension deficit and occurrence of adverse events after a 12-month follow-up period.
Table 1.
Inclusion and Exclusion Criteria
Treatment
Three experienced hand surgeons performed all treatments in the same clinical setting. If the patient received anticoagulating therapy, the need for bridging with heparin before injection was assessed before treatment. Injections were given to correct flexion deformities one joint at a time. For patients with both MP and PIP contractures, 2 treatments were given with an interval of at least 30 days between injections. MP joints were treated before PIP joints, and patients were involved in prioritizing the order of fingers treated. Injection and manipulation technique was not altered during the study. The examiner was the treating surgeon at all times.
Day 1
The quickDASH score was recorded, and the passive extension deficits of the MP, PIP, and distal interphalangeal joints were measured using a goniometer. Extension deficits were measured relative to neutral in all joints. All surgeons were instructed in the use of CCH, and injections were carried out according to the product label guidelines and as described by Hentz.6
After injection, a soft dressing was applied.
Day 2
Major and minor adverse events and the need for pain medication were assessed. If no spontaneous rupture had occurred, 5 to 10 ml of lidocaine (either 10 or 20 mg/ml) was injected before manipulation. Residual extension deficit was recorded using a goniometer, the occurrence of skin tears was noted, and the need for additional follow-up assessed. A nonadhesive dressing was applied, and patients were educated in wound care. All patients were given a removable forearm-based splint to be worn at night for 4 months. The splint kept the treated finger in extension. Patients received instruction on performing finger exercises at home.
One-year Follow-up
At least 12 months after treatment, quickDASH scores, extension deficits, complications, and recurrences were recorded by the treating surgeon. Patient satisfaction at 1 year was recorded.
Statistical Methods and Definitions
Data were entered under quality-assured procedures using the EpiData Software (www.epidata.dk, EpiData Classic, Odense, Denmark) and were analyzed using Stata (www.stata.com—v14, StataCorp LLC, College Station, Tex.). All differences were calculated as intraindividual and joint-specific excluding the quickDASH scores, which were recorded at patient level. All confidence intervals (CIs) were 95% and calculated according to type of estimate (proportion, means). Intraindividual changes over time in goniometric measurements were tested with a paired t test, crosstabulations with chi-square. A 0°–5° extension deficit was defined as successful treatment result in accordance with previous studies,7–9 and recurrence defined as more than 20° of relapse in extension deficit in the treated joint.10 Patient satisfaction was measured on a 5-point ordinal scale (“very satisfied,” “quite satisfied,” “neither satisfied/nor dissatisfied,” “quite dissatisfied,” “very dissatisfied”). The patient’s specific reason for satisfaction or dissatisfaction was not noted.
Material
During the 30-month inclusion period, 340 patients with Dupuytrens Contracture were referred to the department. Of the patients treated, 88% received CCH injection. A total of 235 CCH treatments were given to 212 individuals (195 male and 40 female treatments, see Fig. 1 and Table 2).
Fig. 1.
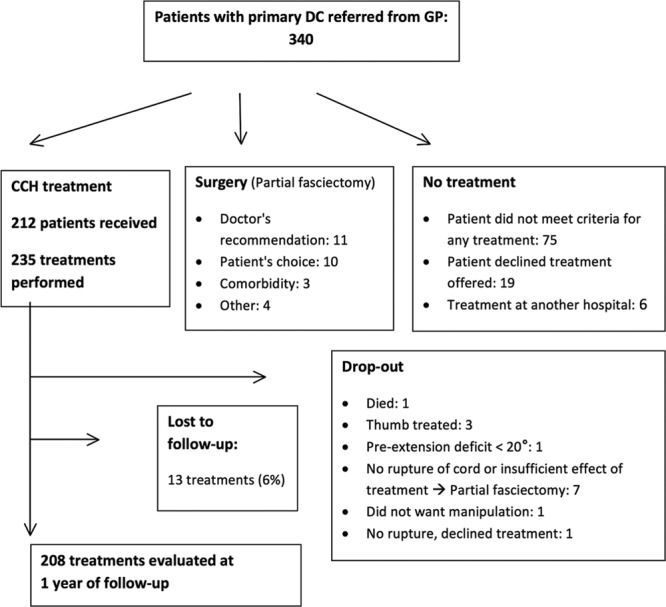
Flowchart accounting for all patients referred to our department with DD. GP; general practitioner.
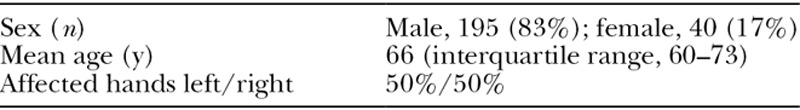
Table 2.
Sex, Age, and Side Treated (n = 235 Treatments)
The majority of the patients received 1 treatment (90%). Eighteen patients received 2 treatments (8%), and 4 patients received 3 treatments (2%). A total of 208 patients were seen at an average of 15 months of follow-up.
A total of 14 patients were listed as dropouts. No relation to joints, finger, or other patient-related factors could be identified. One patient declined manipulation and administration of local anesthetics and asked to be excluded on day 2. One died from circumstances unrelated to DD and CCH treatment. Thumbs were excluded as they are considered anatomically incomparable with the ulnar digits (n = 3). Seven patients (2.9%) were excluded from the 1-year relapse statistics because they had undergone surgery within 1 year of the primary treatment. Indication for surgery was absence of cord rupture or the patient being unsatisfied with an only partial release of the extension deficit.
An attempt was made to contact patients lost to follow-up. Reasons for not participating were either geographical or caused by severe, unrelated illness. According to the national electronic patient files, none of these 13 patients received surgical treatment at the 1-year follow-up.
RESULTS
Spontaneous rupture of the cord was recorded in 5% of treatments. For all treated MP joints, the initial extension deficit was 51° (95% CI: 48–54), and the mean improvement in the extension deficit was 47°, corresponding to a 91% reduction in the extension deficit.
For all treated PIP joints, the initial extension deficit was 62° (95% CI: 57–66), and the mean improvement in the extension deficit was 47°, corresponding to a 76% reduction in the extension deficit (see Fig. 2).
Fig. 2.
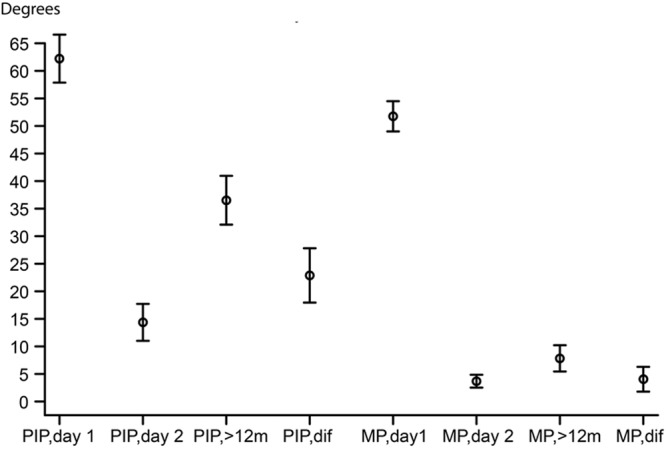
Improvement in passive extension deficit from day 1 to immediately after treatment and after 1 year of follow-up (mean extension deficits with 95% CIs). Day 1, extension deficit, before treatment; day 2, extension deficit, immediately after manipulation; 12m, extension deficit, at 1-year follow-up; MP, dif, mean, difference in extension deficit from day 2 to 1-year follow-up; PIP, dif, mean difference in extension deficit from day 2 to 1-year follow-up.
With a successful result defined as an extension deficit of 5° or less, we found an average success rate of 76% (95% CI: 68–82) for MP joints and 28% (95% CI: 17–40) for PIP joints. The success rate with CIs for each joint can be seen in Figures 3, 4.
Fig. 3.
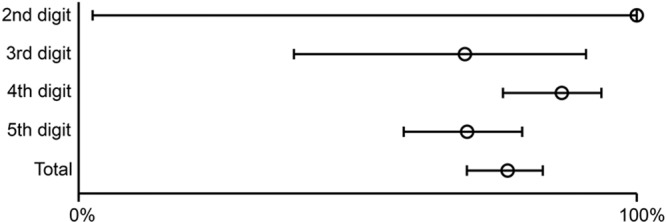
Proportion of MP joints that reached clinical success, defined as a less than or equal to 5° passive extension deficit after manipulation with 95% CIs.
Fig. 4.
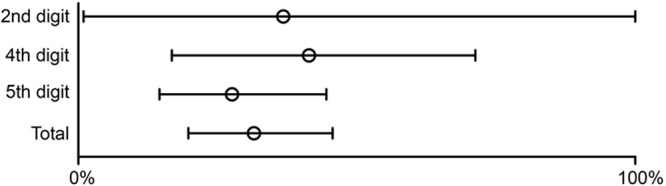
Proportion of PIP joints that reached clinical success, defined as a less than 5° passive extension deficit after manipulation with 95% CIs.
As a result of manipulation, 30% (n = 70) developed a skin tear, and of these treatments, 76% (n = 53) had a need for additional visits to the outpatient clinic. No infections were recorded. All skin tears healed within a few weeks.
Of all 208 treatments, 50% of patients reported the need to use over-the-counter medication for pain after the injection (acetaminophen or ibuprofen).
Follow-up at 12 Months
For MP joints, the mean relapse in the extension deficit was 4°, which was not statistically significant. For PIP joints, a significant relapse in extension deficit was 23°, which corresponds to a relapse of 49%. Recurrence (>20°) was seen in 67% (n = 12) of successfully corrected PIP joints (n = 18) and 15% (n = 19) of MP joints (n = 123) at >12 months of follow-up (see Table 3). The mean quickDASH score for MP joints was reduced from 17 (95% CI: 14–19) to 7 (95% CI: 5–9). No significant improvement in the quickDASH score was found for PIP joints. The majority (86%) of patients reported being either satisfied or very satisfied with the treatment at the 1-year follow-up for MP joints and 69% for PIP joint contractures. Minor adverse events were all mild and spontaneously resolved (Table 4). No major adverse events have been recorded to date (Table 5). To the authors’ knowledge, no patients have experienced severe adverse events to date.
Table 3.
Results of Treatment Immediately after Manipulation and at 1-year Follow-up for Individual Joints
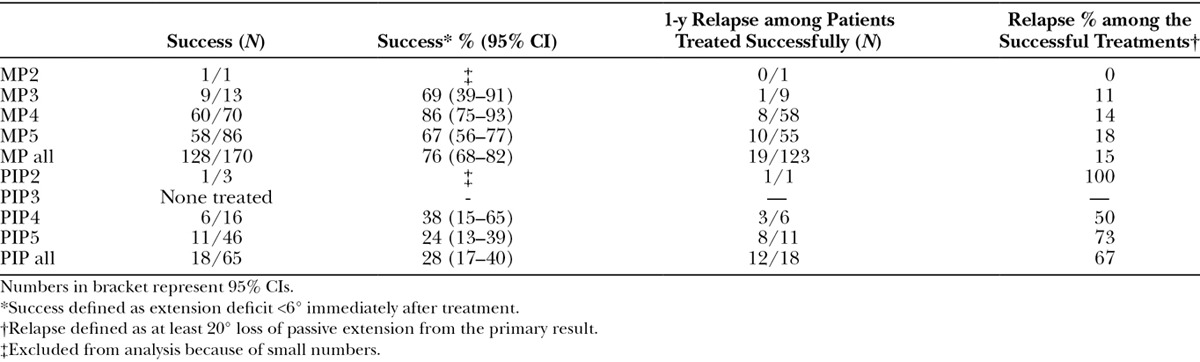
Table 4.
Minor Adverse Events
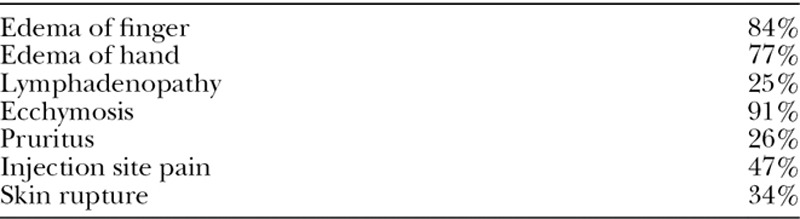
Table 5.
Major Adverse Events
DISCUSSION
The study demonstrates a large difference in treatment success and recurrence when treating MP joints and PIP joints. Treatment success was especially difficult to achieve in PIP joints, and relapse was more frequent compared with MP joints. Mild adverse events are frequent but acceptable. Patient satisfaction is high.
The quickDASH questionnaire has limitations when evaluating patients with DD,11 and we were only able to show a significant improvement for treated MP joints. There is currently no alternative validated tool in Danish.
The study reflects the situation in clinical practice, with an emphasis on patient choice in regard to prioritizing treatment and in the use of patient-reported outcome measures to evaluate the efficiency of treatment. Of all patients treated (CCH or surgery), 88% were treated with CCH, including patients who could not be expected achieve a perfect result, because of a severe initial extension deficit. This may in part explain the high incidence of skin rupture. Another reason may be that we do not consider skin rupture problematic and do not seek to avoid it.
As a potential bias to our study, 7 patients with complete treatment failure were excluded, as described in the study design section. Including these patients in the statistics would have resulted in a 2% decrease in the overall success rate. Although none of the 13 patients lost to follow-up had undergone surgery according to the national patient files, this does not exclude the possibility of recurrence.
Our department was the first in the country to offer collagenase treatment, and therefore, patients from all over the country were initially treated. This is reflected in the number of patients lost to follow-up (n = 13). In particular, it was difficult for elderly patients with comorbidities to travel far distances for their follow-up visits.
Initially, patients had high expectations for the collagenase treatment and were at times discouraged when a residual extension deficit was present after treatment. As the study progressed, the treating surgeons became increasingly aware of the treatment effect and patient information and satisfaction improved accordingly.
Treatment failure in patients with long-lasting, severe contracture, especially of the PIP joints, can be due to tight collateral ligaments, volar plates, and/or joint capsule. It is well known from open surgical procedures that even removal of all Dupuytren’s tissue may not lead to any reduction in extension deficit in the PIP joint. The reason for this being that the contracture in chronic cases primarily lies in anatomical joint structures such as the accessory collateral ligaments and the volar plate.5
Absence of cord rupture can be due to incorrect injection technique, the injection of air or of inactive substances, or patient-related factors. Caution must be taken during the injection process and when handling the CCH.
Since the early landmark studies, several studies have proven CCH to be effective in the treatment of DD. Several of these previous studies addressed the efficacy of CCH for the MP and PIP joints and found results comparable to ours. Studying a total of 1080 treated joints and using the same criteria for success and relapse, Peimer et al.12 found that the majority of treated MP joints (70%) were successfully treated, whereas PIP joints (40%) were less prone to reach full extension. For successfully treated joints, a 27% relapse for MP joints and 56% relapse for PIP joints at 3 years of follow-up were reported. This multicenter study included a very large number of contributors and is not directly comparable to our single-center study, and yet it supports our finding that the success rate, when treating MP joints, is approximately 3 out of 4. The fact that our success rate when treating PIP joint is only 28% compared to Peimer’s 40% may be due to differences in patient selection. The fact that reported relapse rates for MP joints were much greater suggests that studies examining relapse frequencies must be long term.
Peimer et al.13 have published a series of 950 patients. Compared with our reported 1-year relapse rate of 15%, for MP joints, this study found a 39% 5-year relapse rate for MP joints, suggesting that a good initial result does not guarantee that relapse will not occur. Additionally, this study found a 66% 5-year relapse rate in PIP joints, which is comparable to our 67% relapse rate at 1 year. This may suggest that PIP joints relapse faster than MP joints.
Manning et al.14 treated 45 patients with a total of 50 injections and observed a 90% reduction in extension deficit for MP joints, which is very similar to our result of 93%. Witthaut et al.9 also reported similar results treating 879 joints and had a success rate of 70% for MP joints and 37% for PIP joints.
Other studies have addressed adverse events and have reported high incidences of mild adverse events. A study pooling 11 trials found a 0.3% rate of tendon injury, a 16% rate of skin rupture, a 77% rate of hematomas, a 0.1% rate of complex regional pain syndrome, and no nerve or vascular injury.15 In line with these results, we found a very low incidence of major adverse events (Tables 4, 5), although minor adverse events, including skin rupture, were common.
CCH is effective in reducing extension deficit caused by DD with acceptable adverse events. Patients should be properly counseled about the potential benefits and risks of treatment, and that for patients with extensive contractures of multiple joints, surgery may be a better choice.
A review by Eaton16 suggested that the recurrence of DD with CCH may be comparable to that with needle fasciotomy after 2 years of follow-up and greater than that with limited fasciectomy after 5 years of follow-up. Randomized controlled trials comparing CCH with needle fasciotomy and open fasciectomy will prove to be a great help in the future selection of treatment for DD.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Brenner P, Krause-Bergmann A, Van VH. [Dupuytren contracture in North Germany. Epidemiological study of 500 cases]. Unfallchirurg. 2001;104:303–311.. [DOI] [PubMed] [Google Scholar]
- 2.Foucher G, Medina J, Navarro R. Percutaneous needle aponeurotomy: complications and results. J Hand Surg Br. 2003;28:427–431.. [DOI] [PubMed] [Google Scholar]
- 3.Warwick D, Arner M, Pajardi G, et al. ; POINT X Investigators. Collagenase clostridium histolyticum in patients with Dupuytren’s contracture: results from POINT X, an open-label study of clinical and patient-reported outcomes. J Hand Surg Eur Vol. 2015;40:124–132.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hurst LC, Badalamente MA, Hentz VR, et al. ; CORD I Study Group. Injectable collagenase clostridium histolyticum for Dupuytren’s contracture. N Engl J Med. 2009;361:968–979.. [DOI] [PubMed] [Google Scholar]
- 5.Andrew JG. Contracture of the proximal interphalangeal joint in Dupuytren’s disease. J Hand Surg Br. 1991;16:446–448.. [DOI] [PubMed] [Google Scholar]
- 6.Hentz VR. Collagenase injections for treatment of Dupuytren disease. Hand Clin. 2014;30:25–32.. [DOI] [PubMed] [Google Scholar]
- 7.Coleman S, Gilpin D, Kaplan FT, et al. Efficacy and safety of concurrent collagenase clostridium histolyticum injections for multiple Dupuytren contractures. J Hand Surg Am. 2014;39:57–64.. [DOI] [PubMed] [Google Scholar]
- 8.Peimer CA, Skodny P, Mackowiak JI. Collagenase clostridium histolyticum for Dupuytren contracture: patterns of use and effectiveness in clinical practice. J Hand Surg Am. 2013;38:2370–2376.. [DOI] [PubMed] [Google Scholar]
- 9.Witthaut J, Jones G, Skrepnik N, et al. Efficacy and safety of collagenase clostridium histolyticum injection for Dupuytren contracture: short-term results from 2 open-label studies. J Hand Surg Am. 2013;38:2–11.. [DOI] [PubMed] [Google Scholar]
- 10.Felici N, Marcoccio I, Giunta R, et al. Dupuytren contracture recurrence project: reaching consensus on a definition of recurrence. Handchir Mikrochir Plast Chir. 2014;46:350–354.. [DOI] [PubMed] [Google Scholar]
- 11.Forget NJ, Jerosch-Herold C, Shepstone L, et al. Psychometric evaluation of the Disabilities of the Arm, Shoulder and Hand (DASH) with Dupuytren’s contracture: validity evidence using Rasch modeling. BMC Musculoskelet Disord. 2014;15:361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peimer CA, Blazar P, Coleman S, et al. Dupuytren contracture recurrence following treatment with collagenase clostridium histolyticum (CORDLESS study): 3-year data. J Hand Surg Am. 2013;38:12–22.. [DOI] [PubMed] [Google Scholar]
- 13.Peimer CA, Blazar P, Coleman S, et al. Dupuytren contracture recurrence following treatment with collagenase clostridium histolyticum (CORDLESS [collagenase option for reduction of Dupuytren long-term evaluation of safety study]): 5-year data. J Hand Surg Am. 2015;40:1597–1605.. [DOI] [PubMed] [Google Scholar]
- 14.Manning CJ, Delaney R, Hayton MJ. Efficacy and tolerability of day 2 manipulation and local anaesthesia after collagenase injection in patients with Dupuytren’s contracture. J Hand Surg Eur Vol. 2014;39:466–471.. [DOI] [PubMed] [Google Scholar]
- 15.Peimer CA, Wilbrand S, Gerber RA, et al. Safety and tolerability of collagenase Clostridium histolyticum and fasciectomy for Dupuytren’s contracture. J Hand Surg Eur Vol. 2015;40:141–149.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eaton C. Evidence-based medicine: Dupuytren contracture. Plast Reconstr Surg. 2014;133:1241–1251.. [DOI] [PubMed] [Google Scholar]


