Supplemental Digital Content is available in the text.
Summary:
Surgical osteotomy guides created by computer-aided design/computer-aided manufacturing (CAD/CAM) have been developed and are now widely used in maxillofacial reconstruction. However, there are no standard procedures for dealing with an intraoperative change in defect size. We report on a case in which we used our CAD/CAM guides to deal with an intraoperative change in defect size in a maxillary reconstruction. We planned the maxillary reconstruction using a free fibula flap because of left maxillary sinus cancer in a 73-year-old man. In Japan, we cannot use commercially supplied CAD/CAM guides because these have not been approved by the government. We created novel CAD/CAM guides by using free software and a low-cost 3D printer. We performed model surgery to check the accuracy of the design and to prebend the titanium plates before the operation. The actual defect in the maxilla was found to be smaller than that used in preoperative planning. It was therefore necessary to rearrange the fibular segments and to rebend the plates. Comparison between the preoperative and postoperative 3D images showed that the deviation was 2–4 mm. In case that the CAD/CAM guides become inapplicable because of an intraoperative change in defect size, rearranging both the ends of set-up fibular segments and rebending the plates in situ allows us to deal with the situation. However, because extra time is needed to rearrange and rebend, the total operation and flap ischemic times are not shortened.
BACKGROUND
Surgical osteotomy guides created by computer-aided design/computer-aided manufacturing (CAD/CAM) are now used in the reconstruction of the jaw bone.1–7 However, there are no standard procedures for dealing with an intraoperative change in defect size, and CAD/CAM guides may not always be applicable as planned.
In Japan, it is impossible to use commercially supplied CAD/CAM guides because these have not been approved by the government.8 Therefore, we have created novel surgical CAD/CAM guides using software and a low-cost 3D printer.
Numajiri et al.8 previously reported that surgical guides created using our method allow the accurate reconstruction of mandibles with less than 2.4 mm deviation. The material used to create our guides was polylactic acid, which is used frequently in common plastics. We removed the guide completely. Therefore, we consider that the risk of toxicity by polylactic acid is extremely low in our applications. The use of our guides in this operation was approved by our Institutional Review Board. We informed the patients about the use of the guides and obtained their consent.
We report a case in which we used our unique CAD/CAM guides and dealt with an intraoperative change in defect size during a maxillary reconstruction.
CASE PRESENTATION
A 73-year-old man was diagnosed with maxillary sinus cancer and referred to our department for reconstruction. We planned the maxillary reconstruction using a free fibula flap.
We simulated the maxillary reconstruction virtually, and we designed several guides (Fig. 1). We manufactured the guides using a 3D printer and performed model surgery to check the accuracy of our uniquely designed guides and to prebend the titanium plates (see figure, Supplemental Digital Content 1, which displays a model surgery and prebending of the titanium plates, http://links.lww.com/PRSGO/A424).
Fig. 1.
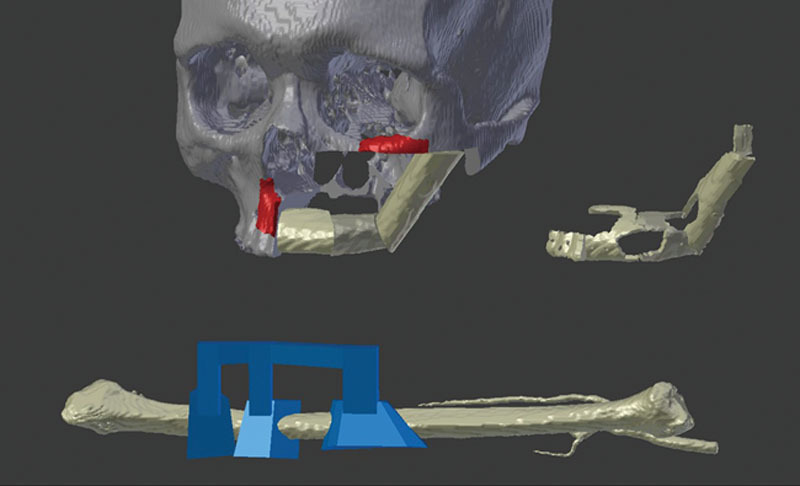
Virtual planning. Cutting guides, maxillary reconstruction, socket and fibular guide.
During the operation, the actual defect was found to be smaller than that used in preoperative planning because of the cancer progression and the effects of chemotherapy. It was therefore necessary to shave both ends of the 3 fibular segments and to rebend the plates (see figure, Supplemental Digital Content 2, which displays how the actual defect became smaller than preoperative planning, http://links.lww.com/PRSGO/A425).
A computed tomography scan was performed 1 week after surgery to determine the accuracy of the fibula insertion. The deviation between the postoperative and preoperative 3D images was 2–4 mm (Fig. 2). The postoperative images showed that the contour of the maxilla had been retained (Fig. 3; see figure, Supplemental Digital Content 3, which displays preoperative and postoperative views, http://links.lww.com/PRSGO/A426). In a follow-up after the operation, the patient did not consent to receive osseointegrated dental implants. However, because the number of remaining teeth was sufficient and the patient’s occlusal condition was maintained, he is able to eat a normal diet.
Fig. 2.
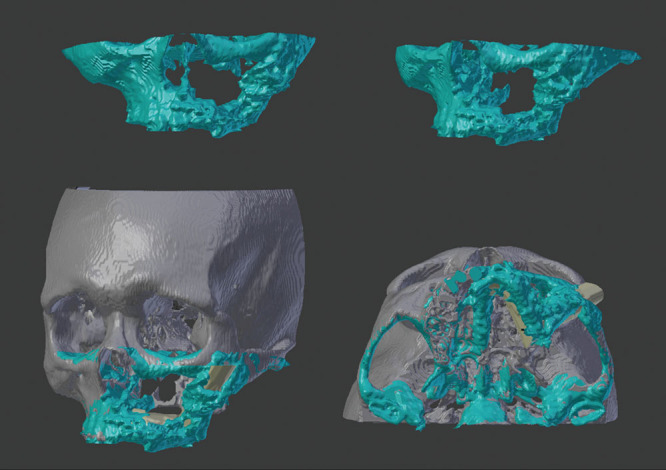
Postoperative 3D image of the reconstructed maxilla with the fibula flap and superimposed postoperative 3D and preoperative images.
Fig. 3.

Postoperative view.
DISCUSSION
Virtual planning and rapid prototyping are valuable and precise techniques in the extensive reconstruction of complicated anatomical sites.1–7
Preoperative virtual planning provides (1) an accurate estimate of the defect in the maxilla, (2) optimized planning for placement of the fibula fragment, and (3) optimized planning for the position and angle of the osteotomy of the fibula. Using CAD/CAM guides allows the surgeon to cut the fibula accurately and to perform an accurate reconstruction.3,4 Because the deviation between the postoperative and preoperative 3D images was only 2–4 mm, we considered that the reconstruction was accurate.
We performed model surgery using 3D entity models based on the preoperative planning. Model surgery allows the surgeon to simulate the actual operation and to prebend the plates. Using CAD/CAM guides and prebent plates can help to shorten the operation and flap ischemic times.5–7 However, the total operation and flap ischemic times did not differ from the averages for the same operation. We believe this was because of the extra time needed to shave the fibula and to rebend the plates to deal with the intraoperative change.
One of the most important points is that, during the operation, the maxilla defect can change from that used in the preoperative planning. Dealing with this situation using only CAD/CAM guides can complicate the operation. Although waiting to determine the defect size may allow the surgeon to deal with intraoperative change, a conventional operation without the CAD/CAM technique is usually required after oncological resection.
When dealing with a defect that is smaller, only the 2 ends of the fibular segments require modification, and the middle segment does not require modification because the end of the remaining maxilla overlaps with the end of the set-up fibula. A defect that is larger requires transplantation of a free bone graft from the disposed fibula, which has already been cut, to fill the gap between the 2 ends of the segments and the maxilla because a vascularized bone graft cannot be harvested in the same operation field (Fig. 4). When dealing with the intraoperative change, these processes can be complex, but the time required for these processes is shorter than that for the operation after oncological resection followed by the conventional method. Moreover, because only the 2 ends of the fibular segments require modification and the central portion can be reconstructed by using CAD/CAM guides, the reconstruction made using the partially adapted CAD/CAM guides is more accurate compared with that made using the conventional method through the entire procedure without CAD/CAM guides.
Fig. 4.
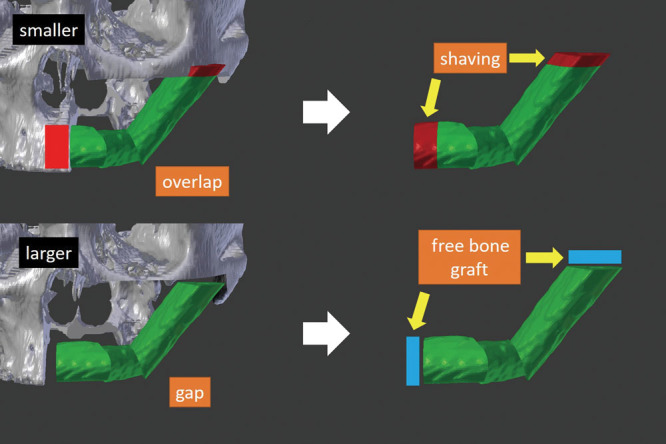
Detailed schema of modification. When a defect is smaller, shaving only the 2 ends of the fibular segments that overlap with the remaining maxilla is required. When a defect is larger, transplantation of a free bone graft to fill the gap is required. The central portion can be reconstructed by using CAD/CAM guides more accurately and more quickly than performing conventional freehand method through the entire procedure.
Because intraoperative amendments are performed according to the surgeon’s subjective view and experience, the reconstruction accuracy may be reduced. The CAD technique with a surgical navigation system allows the surgeon to reconstruct the mandible more accurately than with the freehand technique.9 Therefore, we consider that using a navigation system is helpful for accurate reconstruction when intraoperative amendments are needed because the navigation system can create the mirror image and reproduce the accurate positional relationships.
We did not use a navigation system in this patient because the change in the defect was small.
CONCLUSIONS
We used novel surgical osteotomy guides created by CAD/CAM for the maxillary reconstruction. Our unique guides allowed us to reconstruct the maxilla with a free fibula flap accurately.
Although the maxilla defect was smaller than expected and the CAD/CAM guides became inapplicable, we dealt with the situation by rearranging the bone and rebending the plates in situ. Because extra time is needed to rearrange and rebend, the total operation and flap ischemic times did not differ from the averages for the same operation in our hospital.
Supplementary Material
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Saad A, Winters R, Wise MW, et al. Virtual surgical planning in complex composite maxillofacial reconstruction. Plast Reconstr Surg. 2013;132:626–633.. [DOI] [PubMed] [Google Scholar]
- 2.Tarsitano A, Del Corso G, Ciocca L, et al. Mandibular reconstructions using computer-aided design/computer-aided manufacturing: a systematic review of a defect-based reconstructive algorithm. J Craniomaxillofac Surg. 2015;43:1785–1791.. [DOI] [PubMed] [Google Scholar]
- 3.Zhang WB, Wang Y, Liu XJ, et al. Reconstruction of maxillary defects with free fibula flap assisted by computer techniques. J Craniomaxillofac Surg. 2015;43:630–636.. [DOI] [PubMed] [Google Scholar]
- 4.Zheng GS, Wang L, Su YX, et al. Maxillary reconstruction assisted by preoperative planning and accurate surgical templates. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;121:233–238.. [DOI] [PubMed] [Google Scholar]
- 5.Wang YY, Fan S, Zhang HQ, et al. Virtual surgical planning in precise maxillary reconstruction with vascularized fibular graft after tumor ablation. J Oral Maxillofac Surg. 2016;74:1255–1264.. [DOI] [PubMed] [Google Scholar]
- 6.Hanasono MM, Jacob RF, Bidaut L, et al. Midfacial reconstruction using virtual planning, rapid prototype modeling, and stereotactic navigation. Plast Reconstr Surg. 2010;126:2002–2006.. [DOI] [PubMed] [Google Scholar]
- 7.Rustemeyer J, Sari-Rieger A, Melenberg A, et al. Comparison of intraoperative time measurements between osseous reconstructions with free fibula flaps applying computer-aided designed/computer-aided manufactured and conventional techniques. Oral Maxillofac Surg. 2015;19:293–300.. [DOI] [PubMed] [Google Scholar]
- 8.Numajiri T, Nakamura H, Sowa Y, et al. Low-cost design and manufacturing of surgical guides for mandibular reconstruction using a fibula. Plast Reconstr Surg Glob Open. 2016;4:e805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yu Y, Zhang WB, Liu XJ, et al. Three-dimensional accuracy of virtual planning and surgical navigation for mandibular reconstruction with free fibula flap. J Oral Maxillofac Surg. 2016;74:1503.e1–1503.e10.. [DOI] [PubMed] [Google Scholar]


