Abstract
Introduction
After sinus surgery, patients are commonly instructed to irrigate with saline irrigations with their heads over a sink and noses directed inferiorly (nose-to-floor). While irrigations can penetrate the sinuses in this head position, no study has assessed whether sphenoid sinus penetration can be improved by irrigating with the nose directed superiorly (nose-to-ceiling). The purpose of this study was to use a validated computational fluid dynamic (CFD) model of sinus irrigations to assess the difference in sphenoid sinus delivery of irrigations after irrigating in a nose-to-floor versus nose-to-ceiling head position.
Methods
Bilateral maxillary antrostomies, total ethmoidectomies, wide sphenoidotomies, and a Draf III frontal sinusotomy were performed on a single fresh cadaver head. CFD models were created from postoperative computed tomography maxillofacial scans. CFD modeling software was used to simulate a 120 mL irrigation to the left nasal cavity with the following parameters: flow rate 30 mL/s, angle of irrigation 20 degrees to the nasal floor, and either nose-to-floor or nose-to-ceiling head positioning.
Results
In the postoperative CFD models, the sphenoid sinuses were completely penetrated by the irrigation while in a nose-to-ceiling head position. However, no sphenoid sinus penetration occurred while in the nose-to-floor position. Other sinuses were similarly penetrated in both head positions, although the ipsilateral maxillary sinus was less penetrated in the nose-to-ceiling position.
Conclusion
CFD modeling demonstrated that the nose-to-ceiling head position was superior to the nose-to-floor position in delivering a 120 mL irrigation to the sphenoid sinuses.
Keywords: topical therapy for chronic rhinosinusitis, computational fluid dynamics, endoscopic sinus surgery, chronic rhinosinusitis
Introduction
Topical delivery to the paranasal sinuses is an active area of rhinologic research, with various microscopic and macroscopic factors of topical delivery being studied.1 Among macroscopic factors, optimizing the delivery and distribution of sinus irrigations has been one of the more heavily studied areas. Penetration of the paranasal sinuses by topical irrigations is minimal in unoperated sinuses, regardless of head position or delivery device.2 Prior studies have analyzed different head positions such as vertex-to-wall (nose-to-floor), vertex-to-ceiling (nose-to-wall), and vertex-to-floor, and how they affect topical sinus delivery. After sinus surgery, irrigation can be delivered to each of the sinuses in a nose-to-floor head position, provided high volume delivery devices (≥100 mL per side) are used.3 Generally studies have focused on optimizing irrigation delivery to the maxillary, ethmoid, and frontal sinuses, as these sinuses are more commonly involved with recalcitrant disease.2–10 Recalcitrant sphenoid sinus disease has received little attention in the literature, and therefore has an unknown incidence. No study has assessed how head position affects topical delivery to the sphenoid sinuses, nor whether this might benefit patients with recalcitrant sphenoid sinus disease. More specifically, no study has analyzed whether a nose-to-ceiling head position could improve topical delivery to the sphenoid sinuses. The purpose of this study was to use a validated computational fluid dynamic (CFD) model10 to compare the degree of sphenoid sinus penetration by irrigation after sinus surgery on a cadaver, in nose-to-floor versus nose-to-ceiling head positions.
Methods
One fresh cadaver head was obtained from the University of Pennsylvania morgue, and the study was approved by the University of Pennsylvania Institutional Review Board. Bilateral endoscopic sinus surgery was performed on the cadaver, including wide maxillary antrostomies, total ethmoidectomies, wide sphenoidotomies (complete removal of the anterior sphenoid faces), and a Draf III frontal sinusotomy. Four millimeter trephinations were made in the roofs of the sphenoid sinuses to allow placement of a 30° rigid nasal endoscope, such that clear views of the anterior faces of the sphenoid sinuses could be visualized and recorded during irrigation attempts. A NeilMed SinusRinse® squeeze bottle was filled with 240 mL of saline dyed with blue food coloring. Irrigations were performed by one experimenter while another held the endoscope in each of the sphenoid sinuses. The nozzle tip of the squeeze bottle was seated in the nasal vestibule, and the bottle was angled at approximately 20° to the nasal floor. Irrigation of 120 mL was performed to the left nasal cavity at a volume flow rate of 30 mL/s (120 mL per side over four seconds) in the nose-to-floor position only. Of note, cadaveric sinus irrigations were only assessed endoscopically in the nose-to-floor head position, as the head was not physically available for the nose-to-ceiling portion of the study. Other details of the cadaveric methodology can be found in a previously published paper by the authors.11 Next a postoperative computed tomography (CT) scan was obtained.
Based on previously published methods,11–13 postoperative CFD models were then created from the postoperative cadaveric CT scans. In brief, AMIRA® software (Visualization Sciences Group, Burlington, MA) was used to establish the interface between the nasal mucosa and air on the CT scans. The air space of the nasal cavity was filled with tetrahedral elements using ICEMCFD® software (Ansys, Inc., Canonsburg, PA). The final models were refined and corrected for errors. CFD modeling software was used to simulate 120 mL irrigations to the left nasal cavity with the following parameters: flow rate 30 mL/s (120 mL over four seconds), an angle of irrigation 20° to the nasal floor, and either a nose-to-floor or nose-to-ceiling head position (Figure 1). The simulations were carried out by a commercial CFD software, CFX® (Ansys, Inc., Canonsburg, PA), using a multiphase free surface method. The multiphase model served to define the interaction between different fluid phases: air and saline solution in this case. Videos and still images of the CFD simulations were created.
Figure 1.
Examples of the nose-to-ceiling (A) and nose-to-floor (B) head positions used during sinonasal irrigations.
Each of the experimenters then assigned grades to the CFD model simulations. Irrigation penetration of each of the paranasal sinuses was graded ipsilateral and contralateral to the side of irrigation. The following grading scale was used to classify and compare the degrees of sinus penetration by the irrigation: 0- no penetration, 1- minimal or slow filling, 2- complete or rapid filling. This grading scale was used to compare the postoperative CFD models of the nose-to-floor and nose-to-ceiling head positions. The grades given for sphenoid sinus penetration by the irrigations can be found in Table 1.
Table 1.
| CFD (Nose-to-Floor) | CFD (Nose-to-Ceiling) | |
|---|---|---|
| Sphenoid | Sphenoid | |
| Left, ipsilateral | 0 | 2 |
| Right, contralateral | 0 | 2 |
| Maxillary | Maxillary | |
| Left, ipsilateral | 2 | 1 |
| Right, contralateral | 1 | 1 |
| Ethmoid | Ethmoid | |
| Left, ipsilateral | 2 | 2 |
| Right, contralateral | 2 | 2 |
| Frontal | Frontal | |
| Left, ipsilateral | 2 | 2 |
| Right, contralateral | 2 | 2 |
Grading (0–2) and comparison of irrigation penetration into the sphenoid sinuses after surgery in the cadaver experiment and computational fluid dynamics model. The left nasal cavity was irrigated in this cadaver.
Results
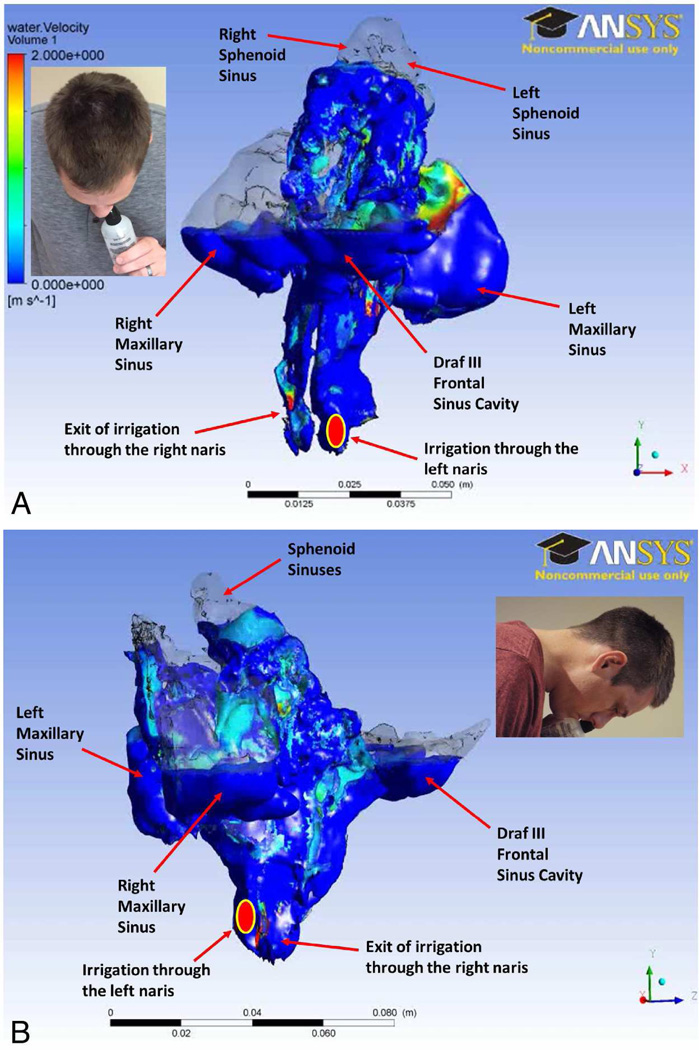
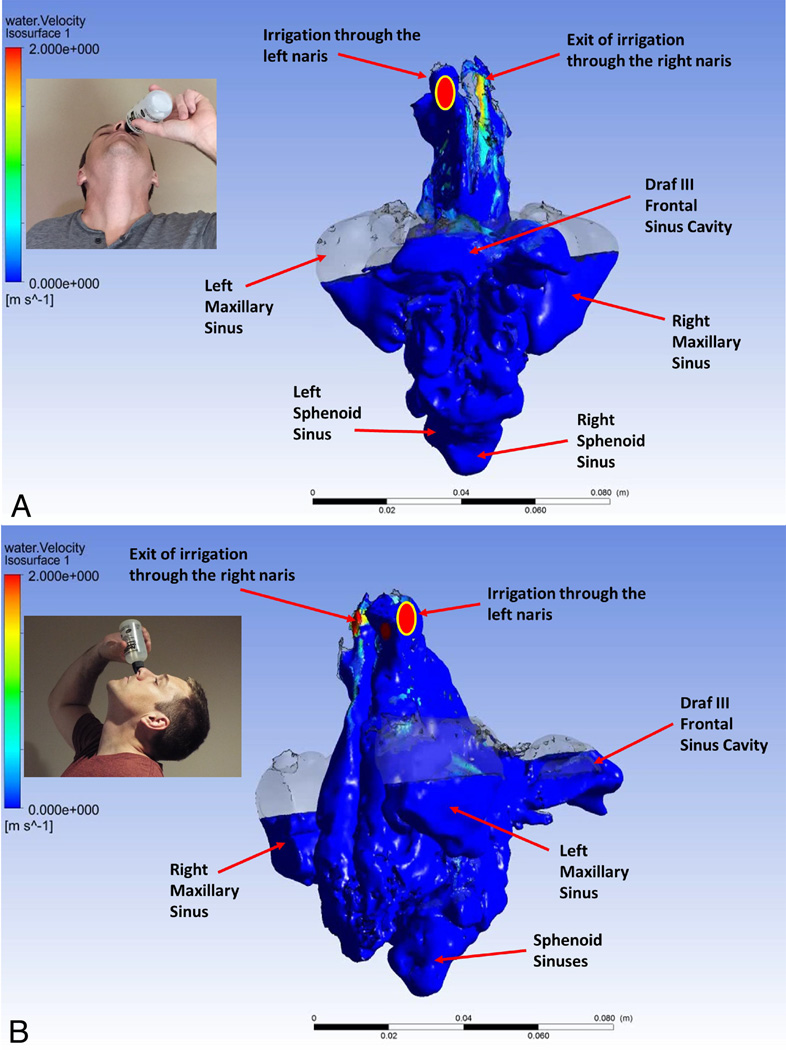
Based on the postoperative CFD model, the nose-to-ceiling head position resulted in complete penetration of sphenoid sinuses both ipsilateral and contralateral to the side of irrigation (Grade 2). Conversely, the nose-to-floor position resulted in no penetration of either of the sphenoid sinuses (Grade 0). Also based on the CFD models, irrigations penetrated the maxillary, ethmoid, and frontal sinuses to similar degrees in both the nose-to-floor and nose-to-ceiling head positions. One difference was that the anterior walls of the frontal and maxillary sinuses were not contacted in the nose-to-ceiling position, whereas the posterior walls in these sinuses were not contacted in the nose-to-floor position. Another difference was that the maxillary sinus ipsilateral to the side of irrigation received about half the irrigation filling (Grade 1) in the nose-to-ceiling positon compared with the ipsilateral maxillary sinus while in the nose-to-floor position (Grade 2). During endoscopic visualization of the cadaveric sphenoid sinuses in the nose-to-floor position, the sphenoid sinuses were not penetrated by the blue-dyed saline irrigation. The irrigation instead filled the maxillary, ethmoid, and frontal sinuses only. Representative still images of the postoperative CFD models are shown for the nose-to-floor (Figure 2) and nose-to-ceiling (Figure 3) head positions. Video clips of the CFD models for the nose-to-floor (Video 1) and nose-to-ceiling (Video 2) head positions, as well as a cadaver endoscopic video of the sphenoid sinuses during irrigations in the nose-to-floor head position (Video 3) are available for online viewing as video supplements.
Figure 2.
Representative still images of the sinonasal irrigation CFD model in the nose-to-floor head position after a Draf III procedure. Superior (A) and RIGHT sagittal (B) views of the simulated irrigation demonstrate that the sphenoid sinuses were never penetrated, whereas both maxillary and ethmoid sinuses, and the Draf III cavity were penetrated. The yellow-outlined red oval indicates that the left nasal cavity was irrigated. The smaller self-irrigation pictures demonstrate the nose-to-floor head position that was simulated for this model.
Figure 3.
Representative still images of the sinonasal irrigation CFD model in the nose-to-ceiling head position after a Draf III procedure. Superior (A) and LEFT sagittal (B) views of the simulated irrigation demonstrate that the sphenoid sinuses were penetrated and completely filled by the irrigation. Both the maxillary and ethmoid sinuses, and the Draf III cavity were still penetrated. The yellow-outlined red oval again indicates that the left nasal cavity was irrigated. The smaller self-irrigation pictures demonstrate the nose-to-ceiling head position that was simulated for this model.
Discussion
While there is an unknown incidence of recalcitrant sphenoid disease, some patients do suffer from this, and this may be due to inadequate topical delivery to the sphenoid sinuses. Optimizing topical delivery to the sphenoid sinus, both for mechanical lavage and topical medication delivery, could benefit patients with recalcitrant sphenoid sinus disease. High volume topical irrigations have proven beneficial after sinus surgery both for mechanical debridement and for medication delivery. The nose-to-floor, nose-to-wall, and vertex-to-floor head positions have been discussed most commonly in the literature with respect to topical delivery, and allow for adequate penetration of each of the sinuses when using high volume irrigations. The findings from this study suggest that after sphenoidotomy, the nose-to-ceiling head position is an alternative to other classically described head positions for delivering topical irrigations to the sphenoid sinus.
Head positions such as the nose-to-floor, nose-to-wall, or vertex-to-floor leave the sphenoid sinus in a position requiring irrigation against gravity. This could decrease irrigation delivery and mucosal contact time within the sphenoid sinus. The nose-to-ceiling head position leaves the sphenoid sinus in a gravity-dependent position relative to the irrigation device, which should improve irrigation delivery to the sphenoid sinus for lavage, as well as mucosal contact time for topical medication absorption. The CFD models compared in this study support the hypothesis that placing the sphenoid sinus in a gravity-dependent nose-to-ceiling position can improve topical delivery to the sphenoid sinus.
The results from this study are discordant from some previous studies published on topical sinus delivery. Singhal et al. assessed 10 cadaver heads endoscopically while delivering 120 mL irrigations in three different head positions after performing sequentially larger openings to all the sinuses. They irrigated the heads in nose-to-floor (termed 90°) and nose-to-wall (termed 0°) positions, and a position in between which they termed the 45° position. For the sphenoid sinus, they showed that even in an unoperated state the sinus was penetrated, and penetration increased after sphenoidotomy. There were no significant differences in sphenoid sinus penetration between the three head positions tested.4 Abadie et al. compared the sinus distribution of seven different high and low volume topical delivery devices in seven cadaver heads. They performed maximal openings to each of the sinuses including a Draf III and wide sphenoidotomy, just as described in the current study. One of the high volume irrigation devices used was the 240 mL squeeze bottle used in the current study, but they did not specify the exact amount of irrigation used during each irrigation attempt. They irrigated the heads in a head-over-sink position (termed 45°). They assessed sinus penetration endoscopically as was done in the study by Singhal et al. They showed that the sphenoid sinus was maximally penetrated in this head position after sphenoidotomy using the 240 mL squeeze bottle.5 One possible explanation for the discrepant results between the current study and previous studies relates to potential variability in how cadaveric irrigations were performed. None of the previous studies reported the average irrigation flow rate nor the angulation of the bottle tip relative to the nasal floor. The flow rate of 30 mL/sec in the current study was based on the average time it took the authors to flush 120 mL through their nasal cavities, but this number is likely to vary between different people. If a faster flow rate was used in previous studies, perhaps this could explain why increased sphenoid sinus penetration was observed. Also in the current study, irrigations were directed 20° from the nasal floor and parallel to the septum. Perhaps different degrees of bottle angulation lead to variable penetration of the sphenoid sinus, and could explain discordance between the current study and previous studies.
Two other studies have actually showed lesser degrees of sphenoid sinus penetration by irrigations, lending support to the results from the current study showing improved sphenoid sinus delivery with a change in head position. Beule et al. performed Draf IIIs and wide endoscopic sinus surgery on 19 cadaver heads, and irrigated the heads with varying volumes of irrigation (50–200 mL) stained with fluorescein, methylene blue, or food coloring. They assessed the mucosal area of staining of each sinus after irrigation. They showed that about 20% of the sphenoid sinus was stained at all volumes of irrigations, whereas the maxillary, ethmoid, and frontal sinuses were each more significantly penetrated with increasing irrigation volumes to upwards of 60–70%. They irrigated heads in nose-to-floor and vertex-to-floor positions, but did not find differences in penetration between these positions.3 Chen et al. performed irrigations on five cadaver heads after varying degrees of surgical openings to each of the sinuses, including the sphenoid sinus. Heads were oriented with the nose facing 45° downward. They compared sinus penetration between a 240 mL squeeze bottle versus a pulsating irrigator. Irrigating 120 mL of fluorescein-stained saline, both devices delivered irrigations to the sphenoid sinus, however neither device achieved heavy penetration of the sphenoid sinus.6 Overall, published results to date with respect to the degree of sphenoid sinus penetration by high volume irrigations have been variable, and the factors responsible for this warrant further study in the future.
One major weakness with this study was that only one cadaver was studied, and therefore the results are difficult to generalize to patient populations. Variable anatomy, extents of surgery, and irrigation parameters may lead to different degrees of sphenoid sinus penetration by irrigations, and these factors can only be tested methodically with a larger sample size. However, an important purpose of this study was simply to show that irrigation delivery to the sphenoid sinus can be inadequate in a nose-to-floor head position, and a nose-to-ceiling position has the potential to improve delivery to the sinus. This finding alone is intriguing and warrants further study. Another weakness inherent to cadaver studies is that cadavers are not ideal representations of live patients. In addition to the absence of edema, polyps, and purulence to affect the distribution of irrigations in cadavers, live patients perform irrigations with variable head positions, flow rates, and bottle angulations. With these factors in mind, if there are variable findings in the literature with regard to degree of sphenoid sinus penetration under well-controlled conditions with reproducible irrigation flow rates, angles, and head positions, it is even more likely that live patients will have variable results. These variable results could mean some patients are not irrigating their sphenoid sinuses adequately.
A few other concerns deserve mention. One concern with the nose-to-ceiling head position is that it may cause oropharyngeal penetration and perhaps even aspiration. The authors tested this head position on themselves, and irrigations reliably exited the contralateral nasal cavity without any oropharyngeal penetration. That said, this concern warrants further study to ensure patient safety, and the authors are studying this currently. An additional logistical concern is patient adherence. Irrigating in this head position requires standing in a bath or shower since the irrigation spills onto the patient’s body. This is less convenient for the patient compared to head-over-sink positions, but if it is more efficacious, the benefits should outweigh the inconvenience. Another concern relates to whether the nose-to-ceiling position allows for adequate topical delivery to the other sinuses, in addition to the sphenoid sinuses. In this study the maxillary, ethmoid, and frontal sinuses were still penetrated in the nose-to-ceiling head position, but this requires further investigation as well. If it were discovered that other sinuses were not as reliably penetrated in the nose-to-ceiling position, patients would need to irrigate in multiple head positions to ensure adequate delivery to all of the sinuses. However, perhaps the nose-to-ceiling position will be found to deliver topical irrigations adequately to all the sinuses, in which case patients could consider only using the nose-to-ceiling position.
Altogether, while various head positions can allow for sphenoid sinus penetration, there is conflicting evidence as to the extent of sphenoid sinus penetration and whether this could be improved with different head positions, irrigation flow rates, or bottle tip angulations. Topical delivery to the sphenoid sinus warrants further study to determine whether or not delivery to the sinus can be improved with different head positions, and whether this improved delivery leads to improved clinical outcomes.
Conclusions
Based on a CFD model of sinonasal irrigations, the nose-to-ceiling head position was more effective than the nose-to-floor position at delivering high volume saline irrigations to the sphenoid sinuses after sphenoidotomy. In patients with recalcitrant sphenoid sinus disease, nose-to-ceiling head positioning can be considered to improve mechanical lavage and medication delivery to the sphenoid sinus.
Supplementary Material
CFD model of the nose-to-floor head position after 120 mL saline irrigation. Use figure 2 as a diagram to orient you to the locations of the different sinuses in the video. Of note, the sphenoid sinus was not penetrated.
CFD model of the nose-to-ceiling head position after 120 mL saline irrigation. Use figure 3 as a diagram to orient you to the locations of the different sinuses in the video. Of note, the sphenoid sinus was penetrated.
Endoscopic view from within the sphenoid sinuses during left-sided irrigations of 120 mL of blue-dyed saline with the cadaver head in a nose-to-floor position. Note that the irrigation did not penetrate either sphenoid sinus, but instead pooled in the ethmoid and maxillary sinuses. The irrigation also reached the frontal sinus but that could not be visualized from this angle of view.
Acknowledgments
The authors would like to thank the University of Pennsylvania morgue, for their assistance in storing and handling the cadaveric specimens for the dissection portion of the study. Kai Zhao has grant funding through the NIH (NIDCD R01 DC013626). There are no other financial disclosures or other conflicts of interest to report for this study.
Footnotes
Conflicts of interest: None
Poster presentation at 2016 ARS Fall meeting (September 16–17, 2016, San Diego, CA)
Author Contributions: All authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Craig, Zhao, and Palmer. Acquisition of data: Craig, Zhao, and Palmer. Analysis and interpretation of data: Craig, Zhao, and Palmer. Drafting of the manuscript: Craig. Critical revision of the manuscript for important intellectual content: Craig, Zhao, and Palmer. Administrative, technical, and material support: Zhao, Palmer. Study supervision: Palmer.
Contributor Information
John R Craig, Dept. of Otolaryngology, Henry Ford Hospital, Detroit, MI.
James N Palmer, Dept. of Otolaryngology, University of Pennsylvania, Philadelphia, PA.
Kai Zhao, Dept. of Otolaryngology, Ohio State University, Columbus, OH.
References
- 1.Harvey RJ, Schlosser RJ. Local drug delivery. Otolaryngol Clin North Am. 2009;42:829–845. doi: 10.1016/j.otc.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 2.Harvey RJ, Goddard JC, Wise SK, et al. Effects of endoscopic sinus surgery and delivery device on cadaver sinus irrigation. Otolaryngol Head Neck Surg. 2008;139:137–142. doi: 10.1016/j.otohns.2008.04.020. [DOI] [PubMed] [Google Scholar]
- 3.Beule A, Athanasiadis T, Athanasiadis E, Field J, Wormald PJ. Efficacy of different techniques of sinonasal irrigation after modified lothrop procedure. Am J Rhinol Allergy. 2009;23:85–90. doi: 10.2500/ajra.2009.23.3265. [DOI] [PubMed] [Google Scholar]
- 4.Singhal D, Weitzel EK, Lin E, et al. Effect of head position and surgical dissection on sinus irrigant penetration in cadavers. Laryngoscope. 2010;120:2528–2531. doi: 10.1002/lary.21092. [DOI] [PubMed] [Google Scholar]
- 5.Abadie WM, McMains KC, Weitzel EK. Irrigation penetration of nasal delivery systems: a cadaver study. Int Forum Allergy Rhinol. 2011;1(1):46–49. doi: 10.1002/alr.20002. [DOI] [PubMed] [Google Scholar]
- 6.Chen PG, Murphy J, Alloju LM, et al. Sinus penetration of a pulsating device versus the classic squeeze bottle in cadavers undergoing sinus surgery. Ann Otol Rhinol Laryngol. 2016 doi: 10.1177/0003489416671532. (epub) [DOI] [PubMed] [Google Scholar]
- 7.Grobler A, Weitzel EK, Buele A, et al. Pre- and postoperative sinus penetration of nasal irrigation. Laryngoscope. 2008;118:2078–2081. doi: 10.1097/MLG.0b013e31818208c1. [DOI] [PubMed] [Google Scholar]
- 8.Barham HP, Ramakrishnan VR, Knisely A, et al. Frontal sinus surgery and sinus distribution of nasal irrigation. Int Forum Allergy Rhinol. 2016;6(3):238–242. doi: 10.1002/alr.21686. [DOI] [PubMed] [Google Scholar]
- 9.Snidvongs K, Chaowanapanja P, Aeumjaturapat S, et al. Does nasal irrigation enter paranasal sinuses in chronic rhinosinusitis? Am J Rhinol Allergy. 2008;22:483–486. doi: 10.2500/ajr.2008.22.3221. [DOI] [PubMed] [Google Scholar]
- 10.Wormald PJ, Cain T, Oates L, et al. A comparative study of three methods of nasal irrigation. Laryngoscope. 2004;114:2224–2227. doi: 10.1097/01.mlg.0000149463.95950.c5. [DOI] [PubMed] [Google Scholar]
- 11.Craig JR, Zhao K, Doan N. Cadaveric validation study of computational fluid dynamics model of sinus irrigations before and after sinus surgery. Int Forum Allergy Rhinol. 2016 Apr;6(4):423–428. doi: 10.1002/alr.21677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhao K, Craig JR, Cohen NA, et al. Sinus irrigations before and after surgery – visualization through computational fluid dynamics simulations. Laryngoscope. 2015;00:000–000. doi: 10.1002/lary.25666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhao K, Scherer PW, Hajiloo SA, et al. Effect of anatomy on human nasal air flow and odorant transport patterns: implications for olfaction. Chem Senses. 2004;29:365–379. doi: 10.1093/chemse/bjh033. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
CFD model of the nose-to-floor head position after 120 mL saline irrigation. Use figure 2 as a diagram to orient you to the locations of the different sinuses in the video. Of note, the sphenoid sinus was not penetrated.
CFD model of the nose-to-ceiling head position after 120 mL saline irrigation. Use figure 3 as a diagram to orient you to the locations of the different sinuses in the video. Of note, the sphenoid sinus was penetrated.
Endoscopic view from within the sphenoid sinuses during left-sided irrigations of 120 mL of blue-dyed saline with the cadaver head in a nose-to-floor position. Note that the irrigation did not penetrate either sphenoid sinus, but instead pooled in the ethmoid and maxillary sinuses. The irrigation also reached the frontal sinus but that could not be visualized from this angle of view.