Abstract
Cervical cancer usually presents in advanced stages and is treated with chemoradiation. About 15–20 % patients present with local recurrence after chemoradiation. Radical surgical resection is the only treatment modality offering long term survival benefit in recurrent cervical cancer. The most common surgical option for these patients is pelvic exenteration. Radical hysterectomy may be done for patients with a small centrally located recurrence in the cervix with no infiltration of adjacent structures. The aim of this study was to evaluate the morbidity and survival outcome following radical hysterectomy and pelvic exenteration for recurrent cancer cervix. We retrospectively reviewed the medical records of our patients who underwent surgery for cancer cervix recurrence from January 2010 to December 2014. The postoperative morbidity was considered early if it happened in the initial 30 days of surgery and late if it occurred after 30 days. All patients were followed up till February 2015. Survival analysis was done using Kaplan- Meir method. Between January 2010 and December 2014, 20 patients with recurrent cervical cancer underwent radical surgical resection. The median age of the study group was 43 years (range 28–63 years). Seventeen patients had squamous cell carcinoma and 3 had adenocarcinoma. 13 underwent pelvic exenteration and 7 patients underwent radical type 2 hysterectomy with bilateral pelvic lymphnode dissection. In the exenteration group, 8 patients had anterior exenteration, 4 had total exenteration and one had posterior exenteration. Urinary diversion was done by ileal conduit in 8 patients, double barrel colostomy in two and wet colostomy in two patients. There were no immediate postoperative deaths. Operating time, blood transfusions needed and hospital stay was more in the exenteration group compared to radical hysterectomy patients. After pelvic exenteration post-operative complications were seen in 76.9 % of which the most common was of the urinary tract including 3 patients with pyelonephritis, 5 had renal insufficiency and 2 patients developed urinary fistulae. Post-operative morbidity was lower in radical hysterectomy patients. There were two patients in the hysterectomy group who developed vault recurrence while none in the exenteration group had local recurrence. The median follow up time was 19 months (range 9–53 months).Three year overall survival for the entire cohort was 43 %. Median survival time for the exenteration group was 28 months which was significantly higher than 14 months for the radical hysterectomy group. This study shows that radical surgical resection is feasible with good survival outcome and acceptable morbidity in recurrent cancer cervix patients. Radical hysterectomy can be done in selected patients but pelvic exenteration has better long-term survival but with the potential for both short- & long-term complications.
Keywords: Cancer cervix recurrence, Pelvic exenteration, Salvage surgery, Morbidity, Salvage hysterectomy
Introduction
Cervical cancer still continues to be one of the major tumour burdens of developing countries. Worldwide incidence of cervical cancer is 16.2 per 100 000 and mortality rate is 9 per 100 000 [1]. In India 132,000 new cases diagnosed and 74,000 deaths annually accounting to nearly 1/3rd of the global cervical cancer deaths. The majority of cervical cancer patients presents in advanced stages and receive chemo radiation for their primary treatment. But 15–30 % recur after completion of primary treatment [2]. In majority of patients the recurrence occurs in the initial two years of treatment and in approximately 50%of patients the recurrence is localized to pelvis [3]. For these patients chemotherapy has been tried with very little effect. Chemotherapy is not effective in a previously irradiated pelvis and the role of chemotherapy is essentially palliative [4]. So in the last 60 years radical surgery has come up with providing certain selected patients with local recurrence of cervical cancer with a real chance of cure.
The most common surgical option available for patients with central recurrence of cervical cancer is pelvic exenteration. Pelvic exenteration is a radical surgical procedure in which pelvic organs including uterus, ovaries, vagina, urinary bladder and rectum are removed en bloc followed by surgical reconstruction. This is an ultra-radical surgery associated with significant morbidity and mortality and is performed when the patient has no alternating treatments to cure her. Radical hysterectomy may be an option for patients with a small centrally located recurrence in the cervix or vaginal fornices with no infiltration of adjacent structures [5]. The data on exenteration dates back to 1948 when Brunswig published his first case series. Since then there has been many publications in western literature but there is an extreme paucity of literature from developing countries. In this background we decided to look into our own experience with surgery for recurrent cervical cancers.
Aim
The aim of the study was to assess the impact of salvage surgery on survival and morbidity in our patients with recurrent cervical cancer who received chemoradiation as primary treatment.
Methods and Materials
We performed a retrospective study of 20 consecutive patients with recurrent cervical cancer who underwent salvage surgery at our institution from January 2010 to Dec. 2014.
Patient demographics, details of primary treatment, disease free interval and surgical parameters including type of surgery, reconstruction techniques, duration of surgery, blood transfusions given and associated complications were assessed. Treatment prior to surgery consisted of external beam pelvic radiotherapy in doses ranging from 40 Gy to 46 Gy in 20 to 23 fractions and concurrent weekly low dose Cisplatin in a dose of 40 mg/m2. Brachytherapy was given by High dose rate intracavitory treatment with 7Gy in 3 sittings. Patients were referred for surgery with biopsy proven recurrent tumour. Disease free interval was calculated from the date of completion of primary treatment to the date of recurrence. MRI was done to assess the local extension of disease extent in all patients. PET CT was done to rule out distant metastasis in 8 patients. Patients with tumour confined to cervix and tumour size less than 2 cm underwent Radical hysterectomy, Piver type 2 with bilateral pelvic node dissection. Patients with more extensive disease underwent pelvic exenteration. Pelvic exenterations were classified as anterior, posterior and total. In anterior exenteration, urinary bladder was removed along with the reproductive tract while in posterior exenterations, rectosigmoid colon was removed with uterus and vagina. Total exenteration combined anterior and posterior exenterations.The post-operative morbidity was considered early if it happened in the initial 30 days of surgery and late if it occurred after 30 days. All patients were followed up till February 2015. Follow up information included the date of last follow-up or death and the disease status at the time of last follow-up. Survival analysis was done using Kaplan- Meir method.
Results
Between January 2010 and December 2014, 1244 patients were treated in the institution for cancer cervix. 20.82 % had stage I, 30.54 % had stage II, 42.62 % had stage III, 5.06 % had stage IV and 0.96 % had no documentation of stage. Chemoradiation was the treatment given to all locally advanced cases and radical surgery for early disease. Patients who presented with residual or recurrent tumour after chemoradiation were biopsied and those with good performance status and localized central recurrences in were considered for salvage surgery.
Twenty three patients with recurrent cervical cancer underwent surgical exploration in this time period. Three patients with inoperable were excluded from the study. The reason for inoperability was paraaortic nodal metastasis in two patients and pelvic side wall involvement in one patient.
Twenty patients who underwent radical surgical resection were included in the study. The median age of the study group was 43 years (range 28–63 years).The most common stage at initial presentation was FIGO stage IIB. Seventeen patients had squamous cell carcinoma and three had adenocarcinoma. Thirteen underwent pelvic exenteration and seven patients underwent radical type two hysterectomy with bilateral pelvic lymphnode dissection. The patient characteristics are described in Table 1. In the exenteration group eight patients had anterior exenteration, four had total exenteration and one had posterior exenteration. Urinary diversion was done by ileal conduit in eight patients, double barrel colostomy in two and wet colostomy in two patients. All patients in the exenteration group had R0 resections. One patient in the radical hysterectomy group had disease extending to the resected margins. None of the patients received adjuvant treatment.
Table 1.
Patient characteristics
| Pelvic exenteration | Radical hysterectomy | |
|---|---|---|
| No of patients | 13 | 7 |
| Age | 43 Range − 28-63 years |
46 Range 41–56 |
| Histology | ||
| Squamous cell carcinoma | 10 | 7 |
| Adeno carcinoma | 3 | |
| FIGO Stage | ||
| IB | 4 | 3 |
| II A | 2 | 2 |
| IIB | 6 | 2 |
| III A | 1 | |
| Disease free interval (mean) | 27.07 months | 11.5 months |
| Range 7- 37 months | Range 3–15 months | |
There were no immediate postoperative deaths. The mean operating time was higher in exenteration group than radical hysterectomy group (340 Vs 150 min).The mean number of blood transfusions needed in exenteration patients was 3.2units compared to 1.5 units in radical hysterectomy patients. The mean hospital stay was also more in the exenteration patients (13.3 Vs 9.2 days). After pelvic exenteration post-operative complications were seen in 76.9 % of which the most common was of the urinary tract. Three patients developed pyelonephritis, 5 had renal insufficiency which manifested by deranged renal function, one patient underwent dialysis for the same. 2 patients developed urinary fistulae needing re exploration. In the radical hysterectomy group other than bladder atony and repeated urinary tract infections one patient developed ureterovaginal fistula which required laparotomy and fistula repair. Preoperative factors including age of the patient, stage of disease and disease free interval did not increase morbidity after salvage surgery.
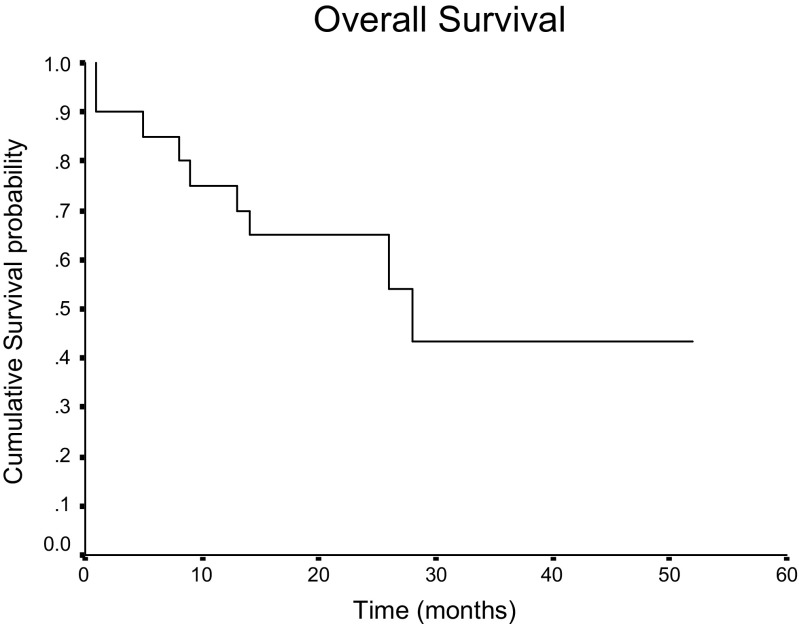
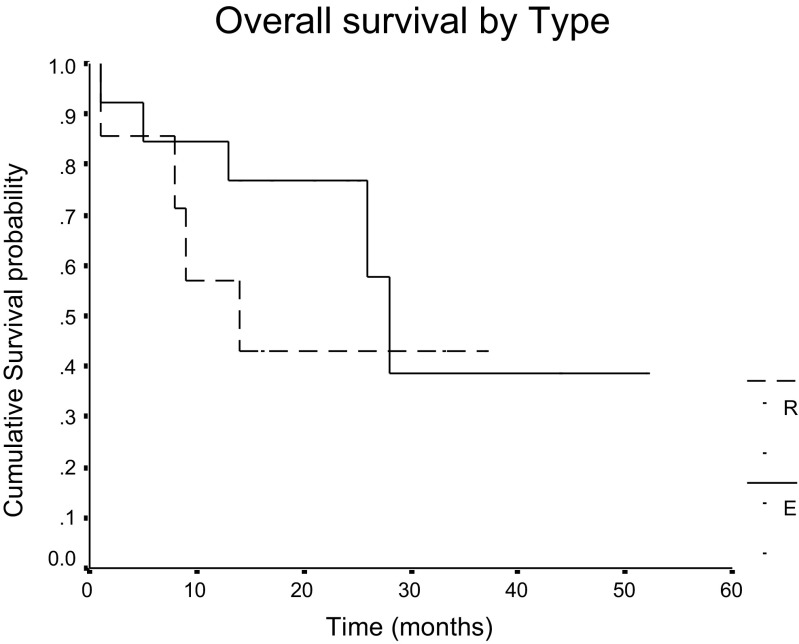
There were two patients in the hysterectomy group who developed vault recurrence including one who was margin positive in her salvage surgery while none in the exenteration group had local recurrence. The median follow up time was 19 months (range 9–53 months).Three year overall survival for the entire cohort was 43 % (Fig.1). Median survival time for the exenteration group was 28 months which was significantly higher than 14 months for the radical hysterectomy group (Fig. 2).
Fig. 1.
Overall survival of patients who underwent radical surgical resection
Fig. 2.
Comparing overall survival in exenteration patients with radical hysterectomy patients. R – Radical hysterectomy patients. E – Pelvic exenteration patients
Discussion
Local failure after radio therapy for cervical cancer is seen in about 10–15 % of early cervical cancer and 20–50 % of advanced cance [6, 7]. Survival of patients with recurrent cervical cancer is poor and the only treatment modality associated with long term survival benefit is radical surgical resection. In patients with small recurrent cancers confined to cervix radical hysterectomy is feasible. Larger recurrences which involve the adjacent organs are treated by pelvic exenteration which is en bloc resection of pelvic organs, followed by surgical reconstruction. The first series on exenteration was published by Brunshwig in 1948 [8]. At that time the mortality rates were very high and this surgery was criticized as a very brutal procedure. But now 60 years after Brunshwig, pelvic exenteration is accepted as a respected procedure potentially curative for patients with localized pelvic recurrences. The initial publications itself showed 5 year overall survival rate between 20 and 40 %.In the recently published literature the 5 year survival has increased to 50–60 % and morbidity and mortality rates have decreased [9–12]. This evolution in pelvic exenteration was made possible by meticulous operative techniques and intensive postoperative management which remains the corner stones in maximizing the success of this surgery. It is ideal to restrict this surgery for patients who have a real chance to get cured. Distant metastasis can be ruled out by Positron emission tomography (PET) scans which help in selecting an ideal patient for cervical cancer salvage surgery.
Post-operative complications are seen in 76.9 % of patients after total exenteration in our series while literature shows morbidity ranging from 32 and 84% [13–16]. There were no post-operative deaths in our patients in the first 30 days after surgery. In the study by Terán-Porcayo etal the post-operative mortality was higher in patients who had early recurrence but our study failed to show relationship between post-operative morbidity and disease free interval [17]. After radical hysterectomy patients had early recovery and complications were lesser compared to exenteration patients. Literature on radical hysterectomy for cervical cancer recurrence is scanty. The report by Maneo et all considered radical hysterectomy as an alternate procedure to exenteration in selected patients [18].
Our series showed survival figures similar to the reported data. Ramamurthy et al. reported a series of 50 patients who underwent pelvic exenteration of which 26 patients had recurrent cancer cervix. Their 5 year survival was 40.1% [19]. In the study by Durgatosh et al. on pelvic exenteration, 15 patients had recurrent cancer cervix with overall 3 year survival of 77.6 % and post-operative mortality of 10.4% [20].
The limitation of this study is that it is a retrospective cohort analysis; we relied mostly on medical records for documentation of postoperative complications and survival outcome. But this study clearly indicates that salvage surgery has a definite role in selected patients with cervical cancer recurrence with definite survival advantage and acceptable morbidity.
Conclusion
The results of this small series seem to justify an attempt to resection for centropelvic recurrences of cancer cervix whenever possible. Radical hysterectomy can be done in selected patients but pelvic exenteration has better long-term survival but with the potential for both short- & long-term complications.
References
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Esti-mates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 2.Chiva LM, Lapuente F, Cortijio LG, Martin AG, Rojo A, Gracia JF, et al. Surgical treatment of recurrent cervical cancer: state of the art and new achievements. Gynecol Oncol. 2008;110:S60–S66. doi: 10.1016/j.ygyno.2008.05.024. [DOI] [PubMed] [Google Scholar]
- 3.Hong JH, Tsai CS, Lai CH, Chang TC, Wang CC, Chou HH, et al. Recurrent squamous cell carcinoma after definitive radiotherapy. Int J Radiat Oncol Biol Phys. 2004;60:249–257. doi: 10.1016/j.ijrobp.2004.02.044. [DOI] [PubMed] [Google Scholar]
- 4.Cardon I, Van Gorp T, Amat F, Leunen K, Neven P, Vergot I. Chemotherapy for recurrent cervical cancer. Gynecol Oncol. 2007;107(1):S113–S118. doi: 10.1016/j.ygyno.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 5.Gadducci A, Tana R, Cosio S, Cionini L. treatment options in recurrent cervical cancer (review) Oncol Lett. 2010;1:3–11. doi: 10.3892/ol_00000001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Landoni F, Maneo A, Colombo A, et al. Randomised study of radical surgery versus radiotherapy for stage ib-iia cervical cancer. Lancet. 1997;350:535–540. doi: 10.1016/S0140-6736(97)02250-2. [DOI] [PubMed] [Google Scholar]
- 7.Kasamatsu T., Onda T., Yamada T., Tsunematsu R. Clinical aspects and prognosis of pelvic recurrence of cervical carcinoma. Int J Gynecol Obstet. 2005;89:39–44. doi: 10.1016/j.ijgo.2004.12.020. [DOI] [PubMed] [Google Scholar]
- 8.Brunschwig A. Complete excision of pelvic viscera for advanced carcinoma. Cancer 1948;1:177–183. [DOI] [PubMed]
- 9.Pawlik T.M., Skibber J.M., Rodriguez-Bigas M.A. Pelvic exenteration for advanced pelvic malignancies. Ann Surg Oncol. 2006;13:612–623. doi: 10.1245/ASO.2006.03.082. [DOI] [PubMed] [Google Scholar]
- 10.Hockel M., Dornhofer N. Pelvic Exenteration for Gynaecological Tumours: Achievements and Unanswered Questions. Lancet Oncol. 2006;7:837–847. doi: 10.1016/S1470-2045(06)70903-2. [DOI] [PubMed] [Google Scholar]
- 11.Peiretti M, Zapardiel I, Zanagnolo V, Landoni F, Morrow CP, Maggioni A. Management of recurrent cervical cancer: a review of the literature. Surg Oncol. 2012;21:e59–e66. doi: 10.1016/j.suronc.2011.12.008. [DOI] [PubMed] [Google Scholar]
- 12.Goldberg G.L., Sukumvanich P., Einstein M.H., Smith H.O., Anderson P.S., Fields A.L. Total pelvic exenteration: the albert einstein college of medicine montefiore medical center experience (1987 to 2003) Gynecol Oncol. 2006;101:261–268. doi: 10.1016/j.ygyno.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 13.Sharma S., Odunsi K., Driscoll D., Lele S. Pelvic exenterations for gynecological malignancies: twenty-year experience at roswell park cancer institute. Int J Gynecol Cancer. 2005;15:475–482. doi: 10.1111/j.1525-1438.2005.15311.x. [DOI] [PubMed] [Google Scholar]
- 14.Berek J.S., Howe C., Lagasse L.D., Hacker N.F. Pelvic exenteration for recurrent gynecologic malignancy: survival and morbidity analysis of the 45-year experience at UCLA. Gynecol Oncol. 2005;99:153–159. doi: 10.1016/j.ygyno.2005.05.034. [DOI] [PubMed] [Google Scholar]
- 15.Pawlik T.M., Skibber J.M., Rodriguez-Bigas M.A. pelvic exenteration for advanced pelvic malignancies ann. Surg Oncol. 2006;13:612–623. doi: 10.1245/ASO.2006.03.082. [DOI] [PubMed] [Google Scholar]
- 16.Höckel M. Ultra-radical compartmentalized surgery in gynaecological oncology. Eur J Surg Oncol. 2006;32:859–865. doi: 10.1016/j.ejso.2006.03.040. [DOI] [PubMed] [Google Scholar]
- 17.Terán-Porcayo M. A., Zeichner-Gancz I., Gomez del-Castillo R. A. C., Beltrán-Ortega A., Solorza-Luna G. “Pelvic exenteration for recurrent or persistent cervical cancer,”. Med Oncol. 2006;23(2):219–223. doi: 10.1385/MO:23:2:219. [DOI] [PubMed] [Google Scholar]
- 18.Maneo A, Landoni F, Cormio G, Colombo A, Mangioni C. Radical hysterectomy for recurrent or persistent cervical cancer following radiation therapy. Int J Gyne col Cancer. 1999;9(4):295–301. doi: 10.1046/j.1525-1438.1999.99037.x. [DOI] [PubMed] [Google Scholar]
- 19.R Ramamurthy, A Duraipandian, Morbidity and outcome of pelvic exenteration in locally advanced pelvic malignancies. Indian J Surg Oncol. 2012; 3(3): 231–235 [DOI] [PMC free article] [PubMed]
- 20.Pandey D, Zaidi S, Mahajan V, Kannan R. Pelvic exenteration: a perspective from a regional cancer center in India. Indian J Cancer. 2004;41(3):109–114. [PubMed] [Google Scholar]