Abstract
Angiomyofibroblastoma is a rare benign soft tissue tumor that arises predominantly in the female genital tract. It occurs less commonly in the scrotum, spermatic cord, and the retroperitoneum. Its diagnosis is based on specific histological and immunopathological features. However, the condition has never been previously described in the extremities. We present the first case report of angiomyofibroblastoma presenting as a slow-growing tumor in the foot of a 48-year-old lady.
Keywords: Angiomyofibroblastoma, Foot, Soft tissue tumor
Introduction
Angiomyofibroblastoma is a soft tissue neoplasm of mesenchymal group and most commonly affects the lower genital tracts of young women [1–3]. Rarely, this tumor affects inguinal and scrotal region in males and retroperitoneal region [1, 2, 4, 5]. The diagnosis of is based on specific histological features of spindle to epithelioid shape tumor cells and immuno-histochemical staining of desmin, CD68, ER was strongly positivity. The differential diagnosis includes angiomatoid fibrous histiocytoma, cellular angiofibroma, and other myxoid tumors. According to the review of literature, this tumor has never been previously described in the extremities. We report the first case of angiomyofibroblastoma presenting as a slow-growing tumor in the foot. We have emphasized the difficulty in making an accurate diagnosis of soft tissue tumor due to unusual location.
Case Presentation
A 48-year-old pre-menopausal lady presented with a 8-year history of a slow-growing right plantar foot mass. The mass was mildly painful on walking and interfered with shoe-wearing. There was no night pain or systemic symptoms. The mass was noticeably larger and became more painful during her menstrual periods. Clinical examination revealed a 7 × 6 cm firm lobulated soft tissue mass on the medial plantar aspect of the right foot (Fig. 1). The mass extended from the medial longitudinal arch laterally towards the fourth webspace. There was sensory hypoesthesia over the third toe. Motor power of toes and the rest of the foot were normal. The capillary refill and distal pulsations were unaffected. There were no other palpable masses elsewhere in the body.
Fig. 1.
Clinical photographs showing a firm lobulated soft tissue mass measuring 7 × 6 cm in the medial aspect of the left foot
The MRI of the right foot showed a T2 hyperintense, T1 isointense lobulated soft tissue mass arising from the plantar aspect of the midfoot with avid contrast enhancement (Fig. 2). It was extending between the first and fourth metatarsal bones and involving the fourth webspace. The dermal skin on plantar aspect was involved by the mass and the flexor digitorum tendons were displaced inferiorly. The tumor was closely related to branches of the medial plantar nerve. Biopsy was performed and the histopathological findings were suggestive of a spindle tumor cells resembling fibrohistiocytic/myofibroblastic type with ovoid bland vesicular nuclei without prominent nucleoli. There was no cytological atypia and a significant mitosis was absent.
Fig. 2.
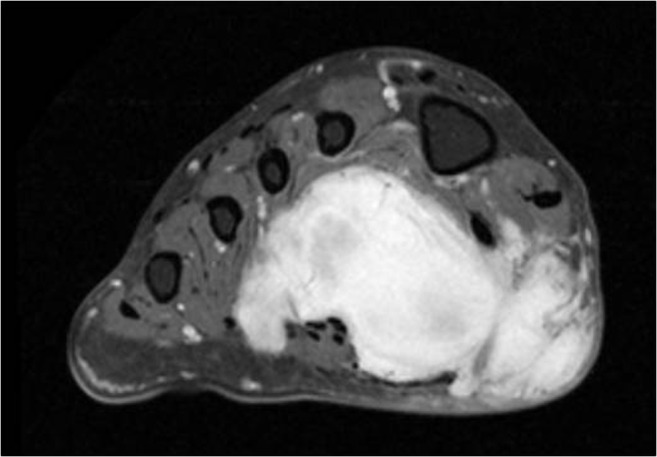
T2W MRI scans of the left foot demonstrating a T2 hyperintense tumor mass in the midfoot, displacing the flexor digitorum tendons inferiorly, closely related to branches of the medial plantar nerve, and involving the plantar skin
The patient underwent marginal excision of the tumor with preservation of the neurovascular bundles. Intra-operative findings were suggestive of soft lobulated tumor in plantar aspect of right foot with extensive infiltration between the neurovascular bundles, muscles, and tendons. Small branches of medial plantar nerve were found to entering the substance of the tumor, with larger branches wrapped around the tumor mass and its capsule. Neural branches which were seen entering the substance of the tumor were sacrificed, whereas other branches which were adherent to the capsule of the tumor were traced and dissected free. An ellipse of involved skin was excised with the tumor. After achieving homeostasis, the surgical site was closed primarily.
On histopathological examination, the tumor measured 5.0 × 6.4 × 3.0 cm (Fig. 3). The tumor had a thin capsule and cut section revealed a blood-filled central cystic space measuring 2.0 × 1.5 cm (which represents approximately one third of the diameter of the tumor). It is interesting to note that this cyst was not demonstrated in the pre-operative MRI. The central cystic space was surrounded by a tan-colored fibrous to myxoid solid tumor.
Fig. 3.
Macroscopic features of the tumor in cross-section
On microscopic examination, the tumor was surrounded by a fibrous pseudo-capsule (Fig. 4). There were spindle to epithelioid shape tumor cells resembling fibrohistiocytic/myofibroblastic type with ovoid bland vesicular nuclei without prominent nucleoli. There was abundant proliferation of small capillary-sized vascular channels in a loose edematous stroma. The tumor cells were concentrated around the blood vessels. Also, there were several areas of prominent blood-filled pseudo-angiomatoid cystic spaces. The periphery of the tumor showed lymphoplasmacytic infiltrate beneath the pseudo capsule. There was no cytological atypia and a significant mitosis was absent.
Fig. 4.
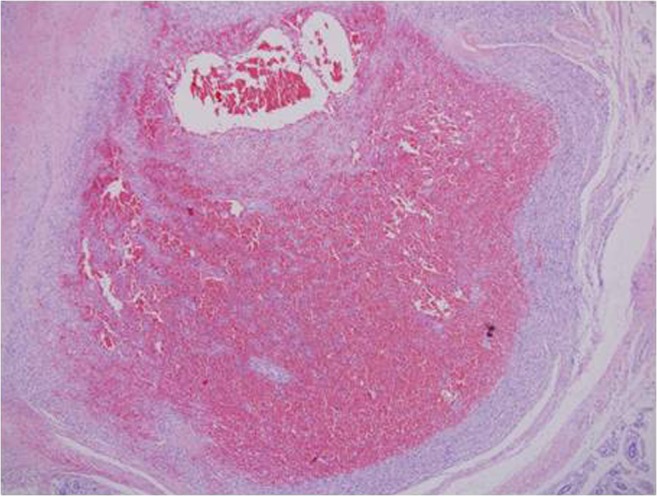
Microscopic features of the tumor
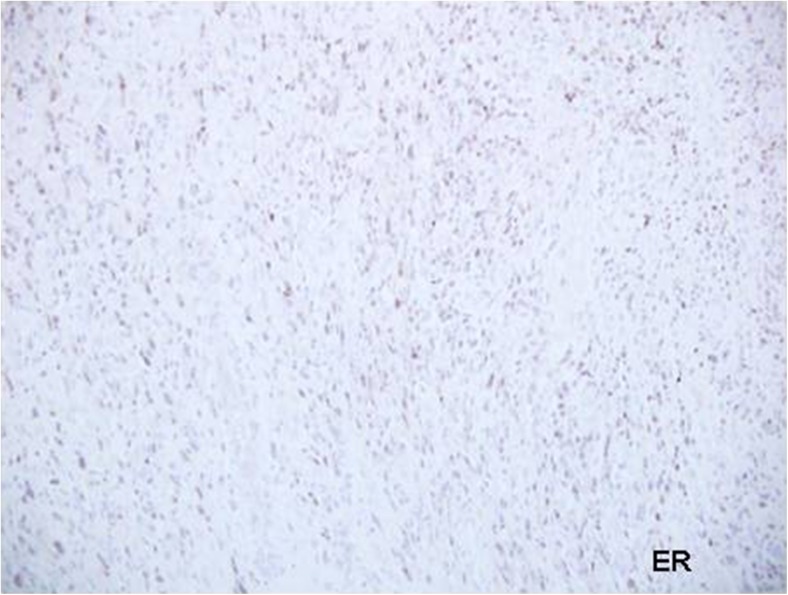
Immuno-histochemical staining showed strong and diffusely positive staining for desmin and CD68. ER was strongly positive whereas PR showed focal patchy positivity (Fig. 5). Other immuno-histochemical stains S100, SMA, myogenin, myo D1, H-caldesmon, CD31, CD34, AE1/3, and ALK were all negative. INI-1 showed intact expression. The proliferation index as measured by Ki-67 was low (<5 %). Due to the cystic and hemorrhagic nature of the tumor and positive expression for desmin, the differential diagnosis was between angiomatoid fibrous histiocytoma and angiomyofibroblastoma. FISH study to detect EWS rearrangement was negative. The diagnosis of angiomyofibroblastoma was made based on histopathological, immunohistochemistry and FISH study.
Fig. 5.
Immuno-histochemical staining showed strongly ER staining positive
Post-operatively, the patient recovered well. She was able to ambulate independently on full weight bearing 2 weeks later.
Discussion
Angiomyofibroblastoma is a benign soft tissue tumor with well-circumscribed margins, prominent vascularity, and features suggestive of myofibroblastic differentiation. The condition more commonly affects females. It has been mostly reported in vulva or vaginal region in females, and the scrotum and spermatic cord in males [1–6, 8, 11–13]. It has also been reported to occur in the retroperitoneum and in the inguinal region. This condition was first described by Fletcher et al. in 1992 [3]. Our review of the literature reveals that this is the first reported case of angiomyofibroblastoma affecting the extremities.
Histologically, angiomyofibroblastoma is characterized by alternating cellularity, numerous capillary-sized vessels associated with oval or plump epithelioid stromal cells. The cells stain strongly positive for desmin with some positive expression for ER [9–11]. Other specific mesenchymal markers are usually negative [6].
An important differential diagnosis in our case was angiomatoid fibrous histiocytoma due to the cystic and hemorrhagic nature of the tumor and positive expression for desmin. Angiomatoid fibrous histiocytoma is a soft tissue tumor of intermediate malignancy. More than 90 % of cases of angiomatoid fibrous histiocytoma demonstrate positive EWS rearrangement. It is important to distinguish between angiomatoid fibrous histiocytoma and angiomyofibroblastoma because the former condition is a soft tissue tumor of intermediate malignancy, whereas the latter is a benign mesenchymal tumor. Complete excision of angiomyofibroblastoma alone is usually curative [14]. Radiotherapy and chemotherapy are not indicated in the treatment of this condition [6–11].
Conclusion
Angiomyofibroblastoma is classically described as a benign and slow-growing tumor which affects the predominantly the female genital tract. In conclusion, we present the first report of in the extremity. The histological features of angiomyofibroblastoma can be similar to that of angiomatoid fibrous histiocytoma. It is important to make this differentiation as the latter is a soft tissue tumor of intermediate malignancy. We found FISH examination for EWS rearrangement to be valuable in excluding angiomatoid fibrous histiocytoma.
References
- 1.Aytac B, Yalcinkaya U, Vuruskan H. Angiomyofibroblastoma-like tumor of the scrotum: a case report and review of literature. Turk Patoloji Dergisi. 2012;28:168–171. doi: 10.5146/tjpath.2012.01118. [DOI] [PubMed] [Google Scholar]
- 2.De Souza LR, Filho EC, Braga WP, Martins PT, De Nicola H. Angiomyofibroblastoma-like tumor of the inguinal canal. J Ultrasound Med. 2009;28:1269–1272. doi: 10.7863/jum.2009.28.9.1269. [DOI] [PubMed] [Google Scholar]
- 3.Fletcher CD, Tsang WY, Fisher C, Lee KC, Chan JK. Angiomyofibroblastoma of the vulva. A benign neoplasm distinct from aggressive angiomyxoma. Am J Surg Pathol. 1992;16:373–382. doi: 10.1097/00000478-199204000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Ito M, Yamaoka H, Sano K, Hotchi M. Angiomyofibroblastoma of the male inguinal region. Arch Pathol Lab Med. 2000;124:1679–1681. doi: 10.5858/2000-124-1679-AOTMIR. [DOI] [PubMed] [Google Scholar]
- 5.Jira H, Hammoudi Y, Ferlicot S, Droupy S, Eschwege P. Benoit G, et al. Scrotal Angiofibroblastoma Prog Uro. 2004;14:561–563. [PubMed] [Google Scholar]
- 6.Kairi-Vassilatou E, Dastamani C, Vouza E, Mavrigiannaki P, Hasiakos D, Kondi-Pafiti A. Angiomyofibroblastoma of the vulva: a clinicopathological and immunohistochemical analysis of a rare benign mesenchymal tumor. Eur J Gynaecol Oncol. 2011;32:353–355. [PubMed] [Google Scholar]
- 7.Magro G, Greco P, Alaggio R, Gangemi P, Ninfo V. Polypoid angiomyofibroblastoma-like tumor of the oral cavity: a hitherto unreported soft tissue tumor mimicking embryonal rhabdomyosarcoma. Pathol Res Pract. 2008;204:837–843. doi: 10.1016/j.prp.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 8.Modica G, Cajozzo M, Sciume C, Lupo F, Pisello F, Li Volsi F, et al. Scrotal angiomyofibroblastoma. Report of a case. Ann Ital Chir. 2001;72:361–363. [PubMed] [Google Scholar]
- 9.Nagai K, Aadachi K, Saito H. Huge pedunculated angiomyofibroblastoma of the vulva. Int J Clin Oncol. 2010;15:201–205. doi: 10.1007/s10147-010-0026-0. [DOI] [PubMed] [Google Scholar]
- 10.Nielsen GP, Rosenberg AE, Young RH, Dickersin GR, Clement PB, Scully RE. Angiomyofibroblastoma of the vulva and vagina. Mod Pathol. 1996;9:284–291. [PubMed] [Google Scholar]
- 11.Quintero C, Sasken H, Houck KL, Hernandez E. Angiomyofibroblastoma of the retroperitoneum: a case report. J Reprod Med. 2007;52:741–744. [PubMed] [Google Scholar]
- 12.Siddiqui MT, Kovarik P, Chejfec G. Angiomyofibroblastoma of the spermatic cord. Br J Urol. 1997;79:475–476. doi: 10.1046/j.1464-410X.1997.10831.x. [DOI] [PubMed] [Google Scholar]
- 13.Sims SM, Stinson K, McLean FW, Davis JD, Wilkinson EJ. Angiomyofibroblastoma of the vulva: a case report of a pedunculated variant and review of the literature. J Lower Genital Tract Dis. 2012;16:149–154. doi: 10.1097/LGT.0b013e318231217b. [DOI] [PubMed] [Google Scholar]
- 14.Tzanakis NE, Giannopoulos GA, Efstathiou SP, Rallis GE, Nikiteas NI. Angiomyofibroblastoma of the spermatic cord: a case report. J Med Case Rep. 2010;4:79. doi: 10.1186/1752-1947-4-79. [DOI] [PMC free article] [PubMed] [Google Scholar]