Abstract
Background
Sufferers from bulimia nervosa (BN) and binge eating disorder (BED) underestimate the severity risk of their illness and, therefore, postpone seeking professional help for years. Moreover, less than one in five actually seek professional help and only 50% respond to current treatments, such as cognitive behavioral therapy (CBT). The impetus for the present trial is to explore a novel combination treatment approach adapted from physical exercise- and dietary therapy (PED-t). The therapeutic underpinnings of these separate treatment components are well-known, but their combination to treat BN and BED have never been previously tested. The purpose of this paper is to provide the rationale for this new treatment approach and to outline the specific methods and procedures.
Methods
The PED-t trial uses a prospective randomized controlled design. It allocates women between 18 and 40 years (BMI range 17.5–35.0) to groups consisting of 5–8 members who receive either CBT or PED-t for 16 weeks. Excess participants are allocated to a waiting list control group condition. All participants are assessed at baseline, post-treatment, 6, 12 and 24 months’ post-follow-up, respectively, and monitored for changes in biological, psychological and therapy process variables. The primary outcome relates to the ED symptom severity, while secondary outcomes relates to treatment effects on physical health, treatment satisfaction, therapeutic alliance, and cost-effectiveness. We aim to disseminate the results in high-impact journals, preferable open access, and at international conferences.
Discussion
We expect that the new treatment will perform equal to CBT in terms of behavioral and psychological symptoms, but better in terms of reducing somatic symptoms and complications. We also expect that the new treatment will improve physical fitness and thereby, quality of life. Hence, the new treatment will add to the portfolio of evidence-based therapies and thereby provide a good treatment alternative for females with BN and BED.
Trial registration
Prospectively registered in REC the 16th of December 2013 with the identifier number 2013/1871, and in Clinical Trials the 17th of February 2014 with the identifier number NCT02079935.
Keywords: Eating disorders, RCT, Physical exercise, Dietary therapy, CBT, Treatment outcome, Physical fitness, Bone mineral density, Resistance exercise
Background
The present paper reports on an ongoing, new treatment for bulimia nervosa (BN) and binge eating disorders (BED). Binge eating disrupts normal eating patterns and introduces vicious circles of fasting and binging that causes a chaotic energy intake. Also, binge eating causes an energy surplus, which those with BN compensate for by purging, eg. vomiting, using laxatives, diuretics, or enemas, misusing medications or exercising in an extreme or rigid manner, all which can change body metabolism. It is noteworthy that such changes may also be the result of physical inactivity, which is frequently observed particularly among sufferers from BED.
Binge eating and compensatory behaviors can raise the medical severity of BN and BED by means of hypokalemia, that may elicit inter-current infections as well as cardiac complications, diseases or arrest, or it may affect glucose, insulin and lipid levels that increases the risk of type-2 diabetes [1–5]. A combination of rigid exercising and eating may over time inflict chronic low energy availability and raise the risk for low bone mineral density, and ultimately osteoporosis [6, 7]. The non-medical severity comprises personal and familial burdens. A slightly raised standardized mortality rate is due to both medical and non-medical burdens [8–10]. According to a recent systematic review, the societal health care costs range from €888–18,283 for BN and €1762–2902 for BED [8–10].
Most sufferers do not acknowledge the clinical severity and the medical and non-medical risks of eating disorders (ED), as 80–94% of people with BN and BED never seek professional help or delay it 4–5 years [11–15]. Effective treatment of BN and BED is considerably hampered by this incongruence, which may be circumvented by offering treatment options outside the contexts of traditional health services or improving access to such options. Among those who do enter treatment, a protracted course of illness is typically seen among every third patient [16]. Important reasons are early drop-out due to a failure to engage patients into treatment and lack of rapid symptom changes or symptom coping, thereby lowering patients’ motivation and self-efficacy [17].
In most treatment guidelines, cognitive-behavioral therapy (CBT) is regarded as the treatment-of-choice for BN [18]. Clinical targets in CBT include weakening the strength of core beliefs about low self-worth and compensatory beliefs about the need to control food intake, body weight and shape. Use of stimulus-control procedures to reduce the frequency of disordered eating, ie. bingeing and/or purging [19] is also central. Studies, systematic reviews and meta-analyses show promising effects of CBT for BED, and intermediate effects for BN, but the methodological quality of studies is low to moderate [20–22] even when often observed comorbid conditions are incorporated in the treatment [23–25]. New treatment approaches are called for because up to 50% of patients do not respond to CBT, even when the therapy is especially designed for ED [26].
Guided physical exercise (PE) may facilitate regulation of negative emotions [27], yet guided PE is rarely used in clinics [28] due to a fear of reinforcing the excessive exercise used to compensate for bingeing. A previous randomized controlled trial has shown that guided PE is as effective as CBT in alleviating BN symptoms [29]. The present study aims to replicate and expand on these findings.
Dietary therapy (DT) and counseling alone to correct the chaotic eating pattern has unclear empirical support [5, 30], but one review indicate some support to a possible additive effects of DT with CBT [31]. The present trial is the first one to examine the additive effects of DT and PE (PED-t) compared to CBT alone, and using a group therapy format.
Therapeutic alliance is an important moderator (or even mediator) of treatment effects in general; however, for EDs its impact is less understood [18, 32, 33]. High treatment expectations and installment of hope seems to predict treatment alliance in anorexia nervosa, but the relationship is uncertain for BN and BED [34]. Recent literature reviews have shown inconsistent findings across ED diagnoses, treatments, patient age groups and time (eg. early, mid or late) of assessment [31, 35, 36]. We hence included measures of alliance and group climate after every CBT and PED-t session to study the temporal order between these factors and response in both treatment arms [31].
Hypotheses and predictions
This trial will test six hypotheses:
1) Comparison of treatment arms: a) PED-t and CBT have comparable effects in terms of less symptoms of eating pathology, b) both perform better than a wait-list control group in reducing binge eating and/or purging, and c) both improve dietary intake.
2) Compared with CBT, the PED-t intervention produces a more rapid treatment response.
3) By improving physical strength and endurance, body composition, bone mass, and the nutritional and hormonal status, PED-t will surpass CBT in reducing the number and severity of medical complications.
4) Positive early changes in therapeutic alliance scores and group cohesiveness partly mediate effects of PED-t and CBT.
5) PED-t surpasses CBT in terms of a lower dropout rate and higher patient satisfaction with treatment.
6) The direct treatment costs are comparable for PED-t and CBT, but the indirect costs of PED-t are expected to be lower.
We predict that the PED-t combination will serve as an effective treatment method for BN and BED because the preoccupations of exercise and diets are transformed away from being ED-symptoms and toward functional coping and self-regulative activities. We also predict that the treatment effect of PED-t will be rapid and strong, defined according to a systematic review and meta-analysis [37], and the best empirically derived predictors of sustained remission at 6 and 12 months follow-up [38, 39] ie. as a 25% reduction in depression scores and ≤3 binge eating episodes a week during the first four weeks of treatment. Given that our novel treatment (PED-t) targets clinical features that occupy the sufferers’ minds, we expect a high level of treatment engagement, motivation and compliance. Such accomplishments may facilitate a stronger therapeutic alliance [40].
Methods and design
This randomized controlled trial includes three groups: participants are randomized to either the CBT or the PED-t treatment group, while participants having to wait represent the control group condition. After 16–20 weeks, these are randomized to either treatment arm. The treatments are delivered to groups consisting of 5–8 participants. It includes 20 therapy sessions stretching across 16 weeks. All outcome variables are measured five times: pre, post, 6, 12 and 24 months (Fig. 1). Mediator/moderator data (ie. therapy process variables) are collected after each treatment session, which yields excellent statistical power for conducting growth curve modeling, nuanced mediation or moderation analyses.
Fig. 1.
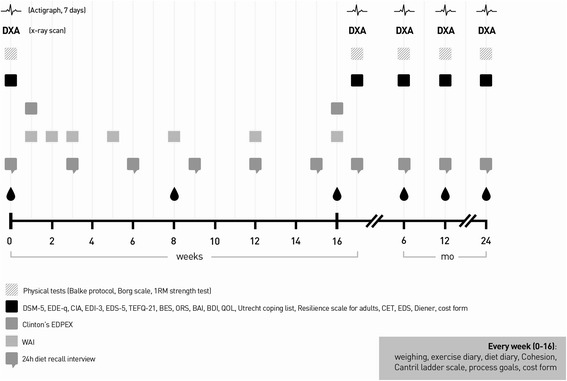
Overview of measures and measurement points. Abbreviations are explained by full name in Table 4
Treatment groups run through 2014–2016. The last follow up assessment is scheduled in December 2018. A detailed treatment manual for the new treatment method (PED-t) can be provided upon request. All treatment sessions are arranged at the Norwegian School of Sport Sciences in Oslo, Norway (NSSS).
Inclusion and exclusion criteria
Included are women aged 18–40 years with a BMI in the range of 17.5–35, a DSM-5 diagnosis of BN or BED with duration of at least 3 months, and with mild to severe symptoms (minimum one episode per week of compensatory behaviors or binge eating, respectively) [41]. A signed letter from the women’s general practitioner (GP) confirming their suitability for the study is required for final enrollment.
Women not eligible are those who are or plan to become pregnant during the study period and those who are competitive athletes. Also excluded are those with a concurrent severe axis I and/or axis II mental disorder obviously in need of other treatments options not focusing on the ED. To prevent effect diffusions we also excluded individuals who have received CBT for ED during the last two years before the trial.
Recruitment
Study- and contact information is distributed through GP’s, magazines and websites of the ED patient organizations, newspaper ads, national TV, social media, and posters.
Individuals calling by phone are informed about the project purpose, and for those who pass the inclusion criteria, a diagnostic screening is conducted using the Mini-International Neuropsychiatric Interview screening [42] and the Eating Disorder Examination (EDE-q) [41, 43, 44] (Fig. 2). Final inclusion is based on three written and signed declarations, ie, the informed consent by the woman to take part in the trial and the assessment procedures herein, a declaration of mutual secrecy about personal information revealed in the group treatment sessions, and a signed consent from their GP that they are medically fit to participate. These documents are returned personally upon the first visit to the NSSS.
Fig. 2.
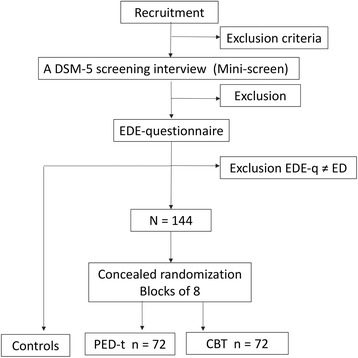
Recruitment, screening and randomization of participants
Randomization
The participants complete the baseline measures before randomization. We use block randomization of size eight (https://www.randomizer.org/) to ensure equal sized treatment arms. A project-independent fellow worker allocated eligible participants to either treatment arm according to a concealed randomization list. Researchers and test personnel in the study are blind with regard to group allocation, but due to the nature of the two treatment procedures, therapists and participants are obviously not blinded to the treatment allocation. The participants are informed about their group allocation after completing the baseline measures.
Safety procedures
A stop-procedure is activated if included subjects display a worsening of ED symptoms (eg. a BMI < 17.0 and/or rapid and significant weight loss of more than 3 kg from normal weight), severe depression or if severe osteoporosis is identified among those randomized to PED-t. Individuals excluded for any of these reasons are medically evaluated for admittance to health care services. Further: if participants report not to have been eating properly before exercise sessions in the PED-t groups, or if feeling ill, we tell the participant not to participate in the physical test or the exercise session that day. During the pre- and post-tests, if participants reports severe purging or restrictive eating in the days before, no physical tests will be performed. A defibrillator is available in the lab where physical tests are held, and a medical health care team is available next house if help is needed.
Statistical power and analyses
Analysis of covariance (ANCOVA) is used to raise statistical power. The effect size of the covariates is set to R 2 = 25%, alpha = .05 and 1-beta = .80. The CBT treatment effect for EDs using the Eating Disorder Examination Questionnaire is about d = 1.30 [45]. A small change (d = 0.30) in the wait-list condition requires 14 subjects in each group (total N = 28), but since the difference between the PED-t and CBT treatment conditions is of primary interest a non-inferiority margin of d = 0.45 is considered as clinically relevant [46]. This requires a sample size of 62 + 62 subjects, increasing to 72 + 72 when adjusting for the group therapy factor (intra-class correlation = .05, design factor 1.16). The longitudinal data will be analyzed using multilevel regression models to accommodate for dependency in the repeated data within subjects and within groups. The maximum likelihood procedure uses all information available, thus, handling dropout well. Multiple imputation will be used to impute missing values. Follow-up data is analyzed with mixed model regression to estimate correct between-group treatment effects adjusted for within-group variance components related to patients and groups. Moderator variables will be included to analyze whether any treatment effects are modified by variables as motivation, therapist alliance or group cohesiveness. If treatment arms do not differ in outcome, combined latent class growth curve modeling will be conducted to analyze reasons for individual differences at startup and in the rate of change across time.
Interventions
The physical exercise and the dietary therapy (PED-t)
Physical exercise
The PED-t is a treatment method particularly designed for BN and BED by our research group, and adheres to recent guidelines developed from systematic reviews to successfully use therapist guided physical exercise [47], and recommendations for a minimal training volume to accomplish a health benefit [48–51].
The intervention aims to (re)establish healthy eating and exercise routines, to change body ideals by focusing on the body’s functionality rather than body appearance and to provide knowledge about the harmful metabolic effects of swings between dieting and food craving. Education about harmful effects of unhealthy behavior is given and how basic and sports related nutritional needs may be balanced.
Three physical trainers and three dieticians conduct the intervention, all holding a master degree in sport sciences and having about three years of practice with supervised exercise. To qualify as a PED-t therapist the physical trainers hold a bachelor’s degree in physical exercise and health or exercise medicine.
The weekly training program in PED-t aims to establish a healthy volume of physical activities, emphasizing the training principles of progression and variation. The exercise program consists of three weekly exercise sessions, each of 40–60 min’ duration. Two sessions are resistance exercise of which one is supervised. The third exercise session consists of unsupervised pyramid interval running, involving shifts between intensive work-periods and active rest-periods with progressive duration (from one minute work period to 4 min of work period).
There are three reasons to focus on giving the participants experience with resistance exercise. First, regular resistance exercise may improve metabolism and bone mineral density, and increase muscular mass and strength [49, 52–54]. Change in body composition further increases the potential for improvement in energy metabolism, weight control and metabolic status [52, 55]. Second, the repeated bouts of supervised resistance exercise, involving technical guiding/corrections while lifting may improve body posture and awareness. Third, strength training involves easily coordinated movements, which may increase the likelihood of positive experience of mastery and weekly progression in performance. These bodily experiences during and after a period with exercise training, have potential to improve body image, self-perception, affect regulation and feeling of coping [56–60]. Intensive work periods, followed by active recovery periods, as practiced with interval training may improve cardiovascular health more effectively and with a lower risk compared to the extended exercise regimen often seen in ED [49, 61–64].
The physical strength-training program intends to improve maximal strength and growth. It is divided into five microcycles with both linear and daily variation in training load [65]. Linear progression involves increased intensity and reduction of training volume over a period of time, with the objective to increase maximal strength. Each week consists of one supervised heavy load, and one unsupervised medium load session. In the former, the number of repetition maximum (RM) increases progressively during the 16 weeks, while in the medium load session, relative load is kept constant at 10RM.
The exercises in the resistance exercise program are squats in smith-machine, lunges with dumbbells, seated dumbbell shoulder press, bench press, latissimus pulldown and seated row in cable machine. The intensity and work periods in the interval running program, follows a traditional pyramid structure performed with progressive interval periods and active rest periods, and then repeated in reverse. After a 10 min warm up, the interval periods are initiated by the first work period of 1 min and a 30 s active rest period (lower intensity), followed by the next work periods of 2 and 3 min and their corresponding rest periods of 60 and 90 s respectively. During the last six weeks, an extra interval period adds to the program with 4 min of work and 2 min of active rest (Table 1).
Table 1.
Overview of the exercise module of the PED-t treatment arm
| SUPERVISED EXERCISE | UNSUPERVISED EXERCISE | |||
|---|---|---|---|---|
| Week | Microcycle | Resistance exercise | Interval running | Resistance exercise |
| 1–3 | 1 | 10 RM | Pyramid interval | 10 RM |
| 4–7 | 2 | 8 RM | Pyramid interval | 10 RM |
| 8–11 | 3 | 6 RM | Pyramid interval | 10 RM |
| 12–14 | 4 | 4 RM | Pyramid interval | 10 RM |
| 15–16 | 5 | 2 RM | Pyramid interval | 10 RM |
Resistance load is given as number of repetition maximum (RM)
During the mid-period (week 8–11) a supervised fourth, weekly group exercise session is introduced, leading the participants to do both the resistance exercise sessions unsupervised. The intention of introducing the participants to the fourth, additional exercise sessions is to inspire them to find a variety of training modalities that can improve physical fitness and promote training joy. Further, the intention with the group sessions is also to make them more experienced in exercising together with others, supervised by an instructor. The four sessions are Total body Resistance eXercise (TRX), suspension training or Cat slide exercise, one boot camp session, one indoor cycling class, and one combat inspired session.
Dietary therapy
The dietary therapy consists of three modules (Table 2), aiming to re-establish healthy dietary routines through weekly lectures, and on discussions related to the weekly topics and the experiences by the participants. Between every session, the participants register the meals they are consuming (pen and paper), and work on individual tasks related to dietary routines (increase number of meals per day, increase volume of food in each meal, improve the composition of the meal etc.).
Table 2.
Overview of the content of the dietary module of the PED-t treatment arm
| Module | Therapy session | Targets | Main content |
|---|---|---|---|
| 1 | 1–5 | Dietary routines & structure | Meal frequency |
| Portion size | |||
| Eating situation | |||
| Exercise theory | |||
| Repetition and summary | |||
| 2 | 6–17 | Nutritional knowledge & practical skills | Energy needs |
| Daily routines | |||
| Nutrients | |||
| Nutritional labels | |||
| Impulsive food shopping | |||
| Exercise theory | |||
| Sports nutrition | |||
| Repetition and summary | |||
| 3 | 18–20 | Summary of future plans | Reflections, repetition and summary |
| Presenting a personal plan for the future (exercise, diet, daily routines) |
The cognitive behavioral therapy (CBT)
Our manual-based CBT has a group format, and rests on the transdiagnostic model of generic core ED-pathology across ED-diagnoses [45]. The treatment runs through four stages (Table 3). All sessions are videotaped and coded according to a CBT manual adherence form [66]. Psychologists who are experienced with CBT and EDs run the CBT treatment.
Table 3.
Overview of the cognitive behavior therapy (CBT) module
| Stages | Therapy session | Targets | Main content |
|---|---|---|---|
| 1 | 1–4 | Engagement, preparation and early behavior change | Educate about the nature of CBT and how the therapist and the participants work together |
| Engage the participants in the treatment. | |||
| Develop a case formulation for each participant. | |||
| Strategies to take control over the behavioral symptoms of BN and BED | |||
| 2 | 5–6 | Monitoring and evaluating progress and barriers to change | A detailed review of progress so far, and to identify barriers to change |
| 3 | 7–16 | Modifying the core pathology of ED | Reduce the over-evaluation of weight and shape |
| Address extreme dieting, binge eating, and purging | |||
| 4 | 17–20 | Consolidating change and relapse prevention | Secure that progress is maintained after treatment end |
Measures and variables
Standardized instruments with good psychometric quality and high clinical utility are included throughout. Count variables measure physical injury and illness [67], and the number of participants meeting DSM-5 criteria for BN or BED [41], respectively. Psychological measures comprise both positive and negative clinical features (Table 4). Since variables of the same measurement domain (eg., eating pathology) will likely be highly multicolinear, these variables will not be combined in the same regression analysis.
Table 4.
Overview of the psychological measures in the PED-t trial
| Eating Disorder Examination-Questionnaire (EDE-q) [95] | Binge Eating Scale (BES) [96] |
|---|---|
| Clinical Impairment Assessment (CIA) [95] | Beck Anxiety Inventory (BAI) [97] |
| Eating Disorder Inventory-3 (EDI-3) [98] | Three-Factor Eating Questionnaire (TFEQ-21) [99] |
| Eating Disturbance Scale (EDS) [100] | Beck Depression Inventory (BDI) [101] |
| Subjective well-being scale [102] | Cantril’s Ladder Scale [103] |
| Utrecht Coping List [104] | Resilience Scale for Adults [105] |
| Outcome Rating Scale (ORS) [106] | Oslo Sports Trauma Research Center questionnaire on health problems (OSTRC) [67] |
Biological measures acknowledged as gold standard methods for assessing physical fitness as well as body composition and bone health [68–70] are used. They comprise changes in blood pressure, serum ferritin, total, high, and low cholesterol, respectively, triglycerides, Apo A, Apo B, vitamin D, folic acid, leptin, insulin CTX-1 and PTH, estradiol, progesterone, TSH, T3, T4, FSH, LH, and cortisol. Also included are objective measures of physical activity (ActigrapgGT3X) [71], a cardio pulmonary exercise test (CPET) to screen for aerobic physical fitness (an incremental modified Balke protocol and Borg Scale) [72–74], muscular strength (1RM test on three selected events -squats, bench press, seated row) [69], resting metabolic rate, bone mineral density (BMD), body fat and lean body weight. Body composition is measured using dual-energy x-ray absorptiometry (DXA) (Lunar iDXA, GE Healthcare, enCORE Software, Version 14.10.022) performing a three site scan (lumbar L2-L4, femoral neck, −trochanter and –shaft, and whole body scan) and analysis procedure according to the guidelines for best practice [75]. Physical tests and DXA-measurements are conducted in the lab at the NSSS, and blood samples are collected by qualified lab personnel and stored frozen until analyzed in a certified lab.
Reasons for physical exercise is measured using the Exercise Dependence Scale [76], and the Compulsive Exercise Test [77]. Throughout the 20 weeks of the physical and dietary therapy, program a training diary records intensity, type of training, and time. Dietary intake and energy/nutrient status is measured through a 24-h diet-recall interview (pre, week 3, 6, 9, 12, 16 and post), weight change (pre/post and separate weekly weigh-ins). Blood samples are taken in week 0, 8, and 17, respectively.
Patient satisfaction is measured using the “Expectations and experiences of ED-treatment” scale [78]. Qualitative approaches, such as in-depth interviews, may give additional insights into ED-patients’ perspectives and satisfaction with treatment [79, 80]. Therefore, a sufficient number of participants to meet data saturation criteria [81] are qualitatively interviewed about a) the immediate overall satisfaction with particular therapy sessions, the therapy process and outcomes, b) the recovery process; and c) the extent to which participants experience long-term treatment benefits. Interview data are analyzed in four steps within the framework of systematic text condensation [81]. Direct and indirect costs associated with treatment and follow-up are recorded prospectively.
Mediator variables comprise the “Working Alliance Inventory” [82] and the “Coerciveness” subscale from the “Therapeutic Factor Inventory” scale [83], both showing good psychometric qualities [84, 85].
Participants not continuing in the study will be compared to those who do continue by examining for differences in the pretest outcome measures.
Discussion
Support to our hypotheses and predictions will provide a platform for enlarging the portfolio of evidence-supported treatments for BN and BED. Enlarging this portfolio is a major achievement given the complex nature of these disorders. An important additional task is to examine which patient, treatment or common therapeutic factors that facilitate a stronger response to cognitive behavioral treatment versus dietary/physical therapy. By bringing ahead knowledge of who responds best to which kind of treatment, we may offer help to a larger proportion of sufferers of ED.
The present trial also offers a possibility of exploring generic therapeutic mechanisms, eg. therapeutic alliance, group cohesion or experience of universality among group members facilitating treatment effects. For EDs the impact of such mechanisms in CBT treatment is less understood [18, 31–33, 35, 36] in particular with respect to BN and BED [34], and for obvious reasons completely unknown with respect to the novel physical exercise and dietary treatment program. The exploring of the impact of such mechanisms imply a search for the mediation effects and when such effects occur during the course of treatment. This knowledge may pave the way for future research into the effects of treatment modules, the succession of modules and the possibility of shortening the treatment length without cutting down on treatment intensity.
In principle, as effective treatments can be unaffordable and intolerable, it is essential to capture the patient satisfaction aspects. The limited number of studies of patients’ satisfaction with treatment have used biased retrospective recalls of treatment modalities rather than methods [11, 86, 87]. In contrast, we use prospective quantitative and qualitative measures to study how satisfaction might be associated with pretreatment expectations, treatment elements, or generic factors in the two treatment arms.
The level of actual knowledge about the costs and benefits of treatments does not meet health authorities’ need to control the health budgets. A recent review located only one CBT study on EDs, also flawed by retrospective recall of direct costs only [8]. The present trial adds to the basis of knowledge by prospective recording of direct and indirect illness-related costs.
In recent years, dissemination has been highly at focus with respect to CBT [88], showing that CBT can be delivered by health professionals other than heavily trained and payed psychologists and psychiatrists. An affordable and tolerable new program with an equal or better effect than CBT would represent major societal benefits in the sense that the PED-t can be delivered by new groups of professionals, eg. exercise therapists and registered dietitians, hence a possibility of reaching out to new segments of those sufferers who are reluctant to seek help through the health care services.
However, a concern can be raised about treatment effectiveness, ie. how well the PED-t might perform in clinical settings. Two deviations from such settings should be mentioned, i.e. the failure to offer booster sessions to consolidate changes during treatment, and to exclude severe comorbid conditions frequently found among patients with BN and BED [89–93], notably anxiety, depression, personality disorders, and active substance abuse. Regrettably, on the other hand, a long waiting time before starting treatment would actually mirror real life clinical settings. The impact of such waiting time on drop-out rates from treatment does, however not seem relevant here as such impact is relevant mostly for patients with severe comorbid conditions [94].
Acknowledgements
The authors thank the participants as well as the research assistants in this project, particularly Tone Skomakerstuen, Line Rønningen, and Solveig Sørdal for production of the interval training program, and also Fredrik S. Kristiansen, Kethe M.E. Engen, Elisabeth Teinung, Karoline Underhaug, and Monika Halvorsen for exercise supervision, and Ane Korsvold and Hege Nymo Østgård for assistance in blood sampling and DXA analyses.
Funding
The PhD position is funded by the Norwegian Women’s Health organization, a non-profit organization being operative since 1896. Their policy is to support projects and science related to women’s health, based on funds collected through voluntary work by the organizational members. Operating funds are supported by the cooperative Universities behind this project (The Norwegian School of Sport Sciences, and UiT- The Arctic University of Norway), mainly by internal funds, and partly by an assigned fund from the Research Council of Norway. The Norwegian Osteoporosis association have donated funds for DXA scans with no further claims for commitment. Dairy sports recovery products have been supported by Tine Dairy Producer (Norway) as part of their charity funding activity, and ACTi graph monitors have been temporary supported by the Norwegian Directorate of Health, The University of Stavanger, the Department of Nutrition (University of Oslo), and Sogn & Fjordane University College. None of the sponsors are participating in the implementation of the project, and neither do they partake in any of the processes like data collection, analysis, interpretations, nor writing of the following papers.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed.
The Project group monitor the data gathering and filing process continuously. Data are handled and stored according to guidelines given by the Norwegian Regional Committees for Medical and Health Research Ethics. All data are de-identified. The identification numbers are stored electronically and separate from the clinical data. The list that maps ID numbers to the personal information will be erased when the project is finished, thus completely anonymizing the data during the current study. Data will for the future be held within the project group.
Authors’ contributions
This study is a multidisciplinary cooperation between experts in exercise medicine from the NSSS and the University College of Southeast Norway, and experts in nutrition from Oslo University Hospital and experts in psychology, CBT and methodology from the UiT- The Arctic University of Norway, and from the treatment and research institution Modum Bad. Dr. JSB provided the original research idea, and is responsible for project planning and -running together with ph.d.-student TFM, drs. GP, JR, and OF. Testing and running of the treatments are handled by the ph.d.-student (PED-T) and drs. TS and KV (CBT), supported by research assistants. Qualitative data are collected by another ph.d.-student (MB). Drs. GP and OF are chief responsible for the qualitative and quantitative data analyses, respectively. The ph.d. student TFM, drs. SBS and MS are responsible for planning and implementation of the physical exercise –and the dietary program. Ph.d student MB and dr. RW have contributed in the qualitative aspects of the study. JSB, JR and TFM wrote the main manuscript, OF managed the statistical description, TFM, SBS, TS, KV, and MS described the interventions and methods in the manuscript, MB, RW and GP contributed with the description of the qualitative aspects in the manuscripts, and all authors have approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The trial is approved by the Norwegian Regional Committee for medical and health research ethics identifier: 2013/1871 the 23rd of October 2013, and prospectively registered in Clinical Trials identifier: NCT02079935 the 17th of February 2014. All participants sign an informed consent delivered at the first visit on NSSS.
Abbreviations
- ANCOVA
analysis of covariance
- BAI
Beck Anxiety Inventory
- BDI
Beck Depression Inventory
- BED
Binge eating disorder
- BES
Binge Eating Scale
- BMD
bone mineral density
- BMI
body mass index
- BN
Bulimia nervosa
- CBT
cognitive behavioral therapy
- CIA
clinical impairment assessment
- CTX-1
carboxy-terminal collagen crosslinks
- DSM-5
diagnostic and statistical manual of mental disorders, 5th edition
- DT
dietary therapy
- DXA
dual-energy x-ray absorptiometry
- ED
eating disorders
- EDE-q
Eating Disorder Questionnaire
- EDI-3
Eating Disorder Inventory, version 3
- EDS
Eating Disturbance Scale
- FSH
follicle-stimulating hormone
- GP
general practitioner
- LH
luteinizing hormone
- NSSS
Norwegian School of Sport Sciences
- ORS
Outcome Rating Scale
- OSTRC
Oslo Sport Trauma Research Center questionnaire on health problems
- PE
physical exercise
- PED-t
Physical exercise and dietary therapy
- PTH
Parathyroid hormone
- RM
repetition maximum
- T3
triiodothyronine
- T4
thyroxine
- TFEQ-21
Three Factor Eating Questionnaire, 21 items version
- TSH
thyroxine stimulating hormone
Contributor Information
Therese Fostervold Mathisen, Phone: +4795752818, Email: T.F.Mathisen@NIH.no.
Jan H. Rosenvinge, Email: jan.rosenvinge@uit.no
Gunn Pettersen, Email: gunn.pettersen@uit.no.
Oddgeir Friborg, Email: oddgeir.friborg@uit.no.
KariAnne Vrabel, Email: karianne.vrabel@modum-bad.no.
Solfrid Bratland-Sanda, Email: Solfrid.Bratland-Sanda@hit.no.
Mette Svendsen, Email: mette.svendsen@ous-hf.no.
Trine Stensrud, Email: Trine.stensrud@nih.no.
Maria Bakland, Email: maria.bakland@uit.no.
Rolf Wynn, Email: rolf.wynn@uit.no.
Jorunn Sundgot-Borgen, Email: jorunn.sundgot-borgen@nih.no.
References
- 1.Raevuori A, Suokas J, Haukka J, Gissler M, Linna M, Grainger M, Suvisaari J. Highly increased risk of type 2 diabetes in patients with binge eating disorder and bulimia nervosa. Int J Eat Disord. 2015;48(6):555–62. [DOI] [PubMed]
- 2.Sullivan PF, Gendall KA, Bulik CM, Carter FA, Joyce PR. Elevated total cholesterol in bulimia nervosa. Int J Eat Disord. 1998;23:425–432. doi: 10.1002/(SICI)1098-108X(199805)23:4<425::AID-EAT10>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 3.Monteleone P, Santonastaso P, Pannuto M, Favaro A, Caregaro L, Castaldo E, Zanetti T, Maj M. Enhanced serum cholesterol and triglyceride levels in bulimia nervosa: relationships to psychiatric comorbidity, psychopathology and hormonal variables. Psychiatry Res. 2005;134:267–273. doi: 10.1016/j.psychres.2004.06.019. [DOI] [PubMed] [Google Scholar]
- 4.Gendall KA, Joyce PR, Carter FA, McIntosh VV, Bulik CM. The effect of bulimia nervosa on plasma glucose and lipids. Physiol Behav. 2002;77:99–105. doi: 10.1016/S0031-9384(02)00829-6. [DOI] [PubMed] [Google Scholar]
- 5.Treasure J, Claudino AM, Zucker N. Eating disorders. Lancet. 2010;375:583–593. doi: 10.1016/S0140-6736(09)61748-7. [DOI] [PubMed] [Google Scholar]
- 6.Mountjoy M, Sundgot-Borgen J, Burke L, Carter S, Constantini N, Lebrun C, Meyer N, Sherman R, Steffen K, Budgett R, Ljungqvist A. The IOC consensus statement: beyond the female athlete triad--relative energy deficiency in sport (RED-S)s Br J Sports Med 2014;48:491–497. [DOI] [PubMed]
- 7.Melin A, Tornberg AB, Skouby S, Moller SS, Sundgot-Borgen J. Faber J. Aziz M, Sjodin A. Energy availability and the female athlete triad in elite endurance athletes. Scand J Med Sci Sports: Sidelmann JJ; 2014. [DOI] [PubMed] [Google Scholar]
- 8.Stuhldreher N, Konnopka A, Wild B, Herzog W, Zipfel S, Löwe B, König H-H. Cost-of-illness studies and cost-effectiveness analyses in eating disorders: a systematic review. Int J Eat Disord. 2012;45:476–491. doi: 10.1002/eat.20977. [DOI] [PubMed] [Google Scholar]
- 9.Simon J, Schmidt U, Pilling S. The health service use and cost of eating disorders. Psychol Med. 2005;35:1543–1551. doi: 10.1017/S0033291705004708. [DOI] [PubMed] [Google Scholar]
- 10.Ágh T, Covács G, Supina D, Pawaskar M, Herman BK, Voko Z, Sheehan DV. A systematic review of the health-related quality of life and economic burdens of anorexia nervosa, bulimia nervosa, and binge eating disorder. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity. 2016:1–12. [DOI] [PMC free article] [PubMed]
- 11.Rosenvinge JH, Klusmeier AK. Treatment for eating disorders from a patient satisfaction perspective: a Norwegian replication of a British study. Eur Eat Disord Rev. 2000;8:293–300. doi: 10.1002/1099-0968(200008)8:4<293::AID-ERV346>3.0.CO;2-4. [DOI] [Google Scholar]
- 12.Hoek HW, van Hoeken D. Review of the prevalence and incidence of eating disorders. Int J Eat Disord. 2003;34:383–396. doi: 10.1002/eat.10222. [DOI] [PubMed] [Google Scholar]
- 13.Reichborn-Kjennerud T, Bulik CM, Sullivan PF, Tambs K, Harris JR. Psychiatric and medical symptoms in binge eating in the absence of compensatory behaviors. Obes Res. 2004;12:1445–1454. doi: 10.1038/oby.2004.181. [DOI] [PubMed] [Google Scholar]
- 14.Wentz E, Gillberg C, Gillberg IC, Råstam M. Ten year follow up of adolescent onset anorexia nervosa: psychiatric disorders and overall functioning scales. J Child Psychol Psychiatry. 2001;42:613–622. doi: 10.1111/1469-7610.00757. [DOI] [PubMed] [Google Scholar]
- 15.Keski-Rahkonen A, Hoek HW, Susser ES, Linna MS, Sihvola E, Raevuori A, Bulik CM, Kaprio J, Rissanen A. Epidemiology and course of anorexia nervosa in the community. Am J Psychiatry. 2007;164:1259–1265. doi: 10.1176/appi.ajp.2007.06081388. [DOI] [PubMed] [Google Scholar]
- 16.Rosenvinge JH, Pettersen G. Epidemiology of eating disorders part II: an update with a special reference to the DSM-5. Adv Eat Disord Theory Res Pract. 2015;3:198–220. doi: 10.1080/21662630.2014.940549. [DOI] [Google Scholar]
- 17.Mahon J. Dropping out from psychological treatment for eating disorders: what are the issues? Eur Eat Disord Rev. 2000;8:198–216. doi: 10.1002/(SICI)1099-0968(200005)8:3<198::AID-ERV356>3.0.CO;2-3. [DOI] [Google Scholar]
- 18.Wilson GT, Grilo CM, Vitousek KM. Psychological treatment of eating disorders. Am Psychol. 2007;62:199. doi: 10.1037/0003-066X.62.3.199. [DOI] [PubMed] [Google Scholar]
- 19.Waller G. A trans-transdiagnostic model of the eating disorders: a new way to open the egg? Eur Eat Disord Rev. 2008;16:165–172. doi: 10.1002/erv.869. [DOI] [PubMed] [Google Scholar]
- 20.Hay P. A systematic review of evidence for psychological treatments in eating disorders: 2005-2012. Int J Eat Disord. 2013;46:462–469. doi: 10.1002/eat.22103. [DOI] [PubMed] [Google Scholar]
- 21.Spielmans GI, Benish SG, Marin C, Bowman WM, Menster M, Wheeler AJ. Specificity of psychological treatments for bulimia nervosa and binge eating disorder? A meta-analysis of direct comparisons. Clin Psychol Rev. 2013;33:460–469. doi: 10.1016/j.cpr.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 22.Vist G, Jung S, Straumann GH, Ding KY, Reinar LM. Cognitive behavior therapy compared to other psychotherapy for treatment of bulimia. Norwegian Directorate for Health, Norwegian Institute of Public Health, Knowledge Centre for the Health Services Department 2016. http://www.kunnskapssenteret.no/en/publications/Cognitive+behaviour+therapy+compared+to+other+psychotherapies+for+treatment+of+bulimia+nervosa. Accessed 20 Feb 2017.
- 23.Groff SE. Is enhanced cognitive behavioral therapy an effective intervention in eating disorders? A review. J Evid Inf Soc Work. 2015:1–17. [DOI] [PubMed]
- 24.Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders: a "transdiagnostic" theory and treatment. Behav Res Ther. 2003;41:509–528. doi: 10.1016/S0005-7967(02)00088-8. [DOI] [PubMed] [Google Scholar]
- 25.Wilson GT, Wilfley DE, Agras WS, Bryson SW. Psychological treatments of binge eating disorder. Arch Gen Psychiatry. 2010;67:94–101. doi: 10.1001/archgenpsychiatry.2009.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pinna F, Sanna L, Carpiniello B. Alexithymia in eating disorders: therapeutic implications. Psychol Res Behav Manag. 2015;8:1. doi: 10.2147/PRBM.S52656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bratland-Sanda S, Martinsen EW, Rosenvinge JH, Ro O, Hoffart A, Sundgot-Borgen J. Exercise dependence score in patients with longstanding eating disorders and controls: the importance of affect regulation and physical activity intensity. Eur Eat Disord Rev. 2011;19:249–255. doi: 10.1002/erv.971. [DOI] [PubMed] [Google Scholar]
- 28.Bratland-Sanda S, Rosenvinge JH, Vrabel KA, Norring C, Sundgot-Borgen J, Ro O, Martinsen EW. Physical activity in treatment units for eating disorders: clinical practice and attitudes. Eat Weight Disord. 2009;14:e106–e112. doi: 10.1007/BF03327807. [DOI] [PubMed] [Google Scholar]
- 29.Sundgot-Borgen J, Rosenvinge JH, Bahr R, Schneider LS. The effect of exercise, cognitive therapy, and nutritional counseling in treating bulimia nervosa. Med Sci Sports Exerc. 2002;34:190–195. doi: 10.1097/00005768-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 30.Laessle RG, Beumont PJ, Butow P, Lennerts W, O'Connor M, Pirke KM, Touyz SW, Waadt S. A comparison of nutritional management with stress management in the treatment of bulimia nervosa. Br J Psychiatry. 1991;159:250–261. doi: 10.1192/bjp.159.2.250. [DOI] [PubMed] [Google Scholar]
- 31.Brauhardt A. De ZM, Hilbert a. The therapeutic process in psychological treatments for eating disorders: a systematic review. Int J Eat Disord. 2014;47:565–584. doi: 10.1002/eat.22287. [DOI] [PubMed] [Google Scholar]
- 32.Wampold BE. How important are the common factors in psychotherapy? An update World Psychiatry. 2015;14:270–277. doi: 10.1002/wps.20238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Horvath AO, Del Re AC, Flückiger C, Symonds D. Alliance in individual psychotherapy. Psychotherapy. 2011;48:9. doi: 10.1037/a0022186. [DOI] [PubMed] [Google Scholar]
- 34.Stiles-Shields C, Bamford BH, Touyz S, Le Grange D, Hay P, Lacey H. Predictors of therapeutic alliance in two treatments for adults with severe and enduring anorexia nervosa. J Eat Disord. 2016;4:1. doi: 10.1186/s40337-016-0102-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zaitsoff S, Pullmer R, Cyr M, Aime H. The role of the therapeutic alliance in eating disorder treatment outcomes: a systematic review. Eat Disord. 2015;23:99–114. doi: 10.1080/10640266.2014.964623. [DOI] [PubMed] [Google Scholar]
- 36.Tasca GA, Balfour L, Ritchie K, Bissada H. Developmental changes in group climate in two types of group therapy for binge-eating disorder: a growth curve analysis. Psychother Res. 2006;16:499–514. doi: 10.1080/10503300600593359. [DOI] [Google Scholar]
- 37.Linardon J, Brennan L, de la Piedad Garcia X. Rapid response to eating disorder treatment: a systematic review and meta-analysis. Int J Eat Disord. 2016;49(10):905–19. [DOI] [PubMed]
- 38.MacDonald DE, Trottier K, McFarlane T, Olmsted MP. Empirically defining rapid response to intensive treatment to maximize prognostic utility for bulimia nervosa and purging disorder. Behav Res Ther. 2015;68:48–53. doi: 10.1016/j.brat.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 39.Thompson-Brenner H, Shingleton RM, Sauer-Zavala S, Richards LK, Pratt EM. Multiple measures of rapid response as predictors of remission in cognitive behavior therapy for bulimia nervosa. Behav Res Ther. 2015;64:9–14. doi: 10.1016/j.brat.2014.11.004. [DOI] [PubMed] [Google Scholar]
- 40.Rector NA, Zuroff DC, Segal ZV. Cognitive change and the therapeutic alliance: the role of technical and nontechnical factors in cognitive therapy. Psychotherapy. 1999;36:320. doi: 10.1037/h0087739. [DOI] [Google Scholar]
- 41.American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5), 5.th edn. American Psychiatric Pub; 2013.
- 42.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The MINI-international neuropsychiatric interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- 43.Luce KH, Crowther JH. The reliability of the eating disorder examination- selfreport questionnaire version (EDE-Q) Int J Eat Disord. 1999;25:349–351. doi: 10.1002/(SICI)1098-108X(199904)25:3<349::AID-EAT15>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 44.Mond JM, Hay PJ, Rodgers B, Owen C, Beumont PJ. Validity of the eating disorder examination questionnaire (EDE-Q) in screening for eating disorders in community samples. Behav Res Ther. 2004;42:551–567. doi: 10.1016/S0005-7967(03)00161-X. [DOI] [PubMed] [Google Scholar]
- 45.Fairburn CG, Cooper Z, Doll HA, O'Connor ME, Bohn K, Hawker DM, Wales JA, Palmer RL. Transdiagnostic cognitive-behavioral therapy for patients with eating disorders: a two-site trial with 60-week follow-up. Am J Psychiatr. 2009;166:311–319. doi: 10.1176/appi.ajp.2008.08040608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fairburn CG, Bailey-Straebler S, Basden S, Doll HA, Jones R, Murphy R, O'Connor ME, Cooper Z. A transdiagnostic comparison of enhanced cognitive behaviour therapy (CBT-E) and interpersonal psychotherapy in the treatment of eating disorders. Behav Res Ther. 2015;70:64–71. doi: 10.1016/j.brat.2015.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cook B, Wonderlich SA, Mitchell J, Thompson R, Sherman R, McCallum K. Exercise in eating disorders treatment: systematic review and proposal of guidelines. Med Sci Sports Exerc. 2016;48:1408–1414. doi: 10.1249/MSS.0000000000000912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.WHO. Global recommendations on physical activity for health. 2010. http://apps.who.int/iris/bitstream/10665/44399/1/9789241599979_eng.pdf. Accessed 30 Jan 2017. [PubMed]
- 49.Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, Nieman DC, Swain DP. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 50.Nordic Council of Ministers. Nordic Nutrition Recommendations 2012 - integrating nutrition and physical activity. https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/806/Anbefalinger-om-kosthold-ernering-og-fysisk-aktivitet-IS-2170.pdf. Accessed 30 Jan. 2017.
- 51.Loveless MS, Ihm JM. Resistance exercise: how much is enough? Curr Sports Med Rep. 2015;14:221–226. doi: 10.1249/JSR.0000000000000149. [DOI] [PubMed] [Google Scholar]
- 52.Prabhakaran B, Dowling EA, Branch JD, Swain DP, Leutholtz BC. Effect of 14 weeks of resistance training on lipid profile and body fat percentage in premenopausal women. Br J Sports Med. 1999;33:190–195. doi: 10.1136/bjsm.33.3.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Martyn-St James M, Carroll S. Effects of different impact exercise modalities on bone mineral density in premenopausal women: a meta-analysis. J Bone Miner Metab. 2010;28:251–267. doi: 10.1007/s00774-009-0139-6. [DOI] [PubMed] [Google Scholar]
- 54.Chilibeck PD, Sale DG, Webber CE. Exercise and bone mineral density. Sports Med. 1995;19:103–122. doi: 10.2165/00007256-199519020-00003. [DOI] [PubMed] [Google Scholar]
- 55.Votruba SB, Horvitz MA, Schoeller DA. The role of exercise in the treatment of obesity. Nutrition. 2000;16:179–188. doi: 10.1016/S0899-9007(99)00264-6. [DOI] [PubMed] [Google Scholar]
- 56.Chmelo EA, Hall EE, Miller PC, Sanders KN. Mirrors and resistance exercise, do they influence affective responses? J Health Psychol. 2009;14:1067–1074. doi: 10.1177/1359105309342300. [DOI] [PubMed] [Google Scholar]
- 57.Moore JB, Mitchell NG, Bibeau WS, Bartholomew JB. Effects of a 12-week resistance exercise program on physical self-perceptions in college students. Res Q Exerc Sport. 2011;82:291–301. doi: 10.1080/02701367.2011.10599757. [DOI] [PubMed] [Google Scholar]
- 58.Taspinar B, Aslan UB, Agbuga B, Taspinar F. A comparison of the effects of hatha yoga and resistance exercise on mental health and well-being in sedentary adults: a pilot study. Complementary therapies in medicine. 2014;22:433–440. doi: 10.1016/j.ctim.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 59.Hale BS, Raglin JS. State anxiety responses to acute resistance training and step aerobic exercise across 8-weeks of training. J Sports Med Phys Fitness. 2002;42:108. [PubMed] [Google Scholar]
- 60.Focht BC. Pre-exercise anxiety and the anxiolytic responses to acute bouts of self-selected and prescribed intensity resistance exercise. J Sports Med Phys Fitness. 2002;42:217. [PubMed] [Google Scholar]
- 61.Bacon AP, Carter RE, Ogle EA, Joyner MJ. VO 2 max trainability and high intensity interval training in humans: a meta-analysis. PLoS One. 2013;8 doi: 10.1371/journal.pone.0073182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sloth M, Sloth D, Overgaard K, Dalgas U. Effects of sprint interval training on VO2max and aerobic exercise performance: a systematic review and meta-analysis. Scand J Med Sci Sports. 2013;23:e341–e352. doi: 10.1111/sms.12092. [DOI] [PubMed] [Google Scholar]
- 63.Fisher G, Brown AW, Brown MMB, Alcorn A, Noles C, Winwood L, Resuehr H, George B, Jeansonne MM, Allison DB. High intensity interval-vs moderate intensity-training for improving Cardiometabolic health in overweight or obese males: a randomized controlled trial. PLoS One. 2015;10 doi: 10.1371/journal.pone.0138853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hazell TJ, Hamilton CD, Olver TD, Lemon PW. Running sprint interval training induces fat loss in women. Appl Physiol Nutr Metab. 2014;39:944–950. doi: 10.1139/apnm-2013-0503. [DOI] [PubMed] [Google Scholar]
- 65.Kraemer WJ, Adams K, Cafarelli E, Dudley GA, Dooly C, Feigenbaum MS, Fleck SJ, Franklin B, Fry AC, Hoffman JR. American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2002;34:364–380. doi: 10.1097/00005768-200205001-00389. [DOI] [PubMed] [Google Scholar]
- 66.Barber JP, Liese BS, Abrams MJ. Development of the cognitive therapy adherence and competence scale. Psychother Res. 2003;13:205–221. doi: 10.1093/ptr/kpg019. [DOI] [Google Scholar]
- 67.Clarsen B, Roensen O, Myklebust G, Floerenes TW, Bahr R. The Oslo Sports Trauma Research Center questionnaire on health problems: a new approach to prospective monitoring of illness and injury in elite athletes. Br J Sports Med. 2013;bjsports-2012. [DOI] [PubMed]
- 68.Ackland TR, Lohman TG, Sundgot-Borgen J, Maughan RJ, Meyer NL, Stewart AD, Muller W. Current status of body composition assessment in sport: review and position statement on behalf of the ad hoc research working group on body composition health and performance, under the auspices of the I.O.C. Medical commission. Sports Med. 2012;42:227–249. doi: 10.2165/11597140-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 69.Maud PJ, Foster C. Physiological assessment of human fitness. 2. Human Kinetics: Champaign; 2006. [Google Scholar]
- 70.Lupash E. ACSM’s guidelines for exercise testing and prescription. 9. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health; 2014. [Google Scholar]
- 71.Ried-Larsen M, Brønd JC, Brage S, Hansen BH, Grydeland M, Andersen LB, Møller NC. Mechanical and free living comparisons of four generations of the Actigraph activity monitor. Int J Behav Nutr Phys Act. 2012;9:1. doi: 10.1186/1479-5868-9-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Edvardsen E. Hansen BrH, Holme IM, Dyrstad SM, Anderssen SA. Reference values for cardiorespiratory response and fitness on the treadmill in a 20-to 85-year-old population. CHEST Journal. 2013;144:241–248. doi: 10.1378/chest.12-1458. [DOI] [PubMed] [Google Scholar]
- 73.Borg G. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–81. doi: 10.1249/00005768-198205000-00012. [DOI] [PubMed] [Google Scholar]
- 74.Balke B, Ware RW. An experimental study of physical fitness of air force personnel. U S Armed Forces Med J. 1959;10:675–688. [PubMed] [Google Scholar]
- 75.Nana A, Slater GJ, Stewart AD, Burke LM. Methodology review: using dual-energy X-ray absorptiometry (DXA) for the assessment of body composition in athletes and active people. Int J Sport Nutr Exerc Metab. 2014; [DOI] [PubMed]
- 76.Hausenblas HA, Downs DS. How much is too much? The development and validation of the exercise dependence scale. Psychol Health. 2002;17:387–404. doi: 10.1080/0887044022000004894. [DOI] [Google Scholar]
- 77.Taranis L, Touyz S, Meyer C. Disordered eating and exercise: development and preliminary validation of the compulsive exercise test (CET) Eur Eat Disord Rev. 2011;19:256–268. doi: 10.1002/erv.1108. [DOI] [PubMed] [Google Scholar]
- 78.Clinton D. Expectations and experiences of treatment in eating disorders. Eat Disord. 2001;9:361–371. doi: 10.1080/106402601753454921. [DOI] [PubMed] [Google Scholar]
- 79.Pettersen G, Thune-Larsen KB, Wynn R, Rosenvinge JH. Eating disorders: challenges in the later phases of the recovery process. Scand J Caring Sci. 2013;27:92–98. doi: 10.1111/j.1471-6712.2012.01006.x. [DOI] [PubMed] [Google Scholar]
- 80.Pettersen G, Rosenvinge JH, Wynn R. Eating disorders and psychoeducation--patients' experiences of healing processes. Scand J Caring Sci. 2011;25:12–18. doi: 10.1111/j.1471-6712.2010.00783.x. [DOI] [PubMed] [Google Scholar]
- 81.Malterud K. Systematic text condensation: a strategy for qualitative analysis. Scand J Publ Health. 2012;40:795–805. doi: 10.1177/1403494812465030. [DOI] [PubMed] [Google Scholar]
- 82.Horvath AO, Greenberg LS. Development and validation of the working alliance inventory. J Couns Psychol. 1989;36:223. doi: 10.1037/0022-0167.36.2.223. [DOI] [Google Scholar]
- 83.Lese KP, MacNair-Semands RR. The therapeutic factors inventory: development of a scale. Group. 2000;24:303–317. doi: 10.1023/A:1026616626780. [DOI] [Google Scholar]
- 84.Rush AJ. Blacker D. Handbook of psychiatric measures: American Psychiatric Press Inc; 2008. [Google Scholar]
- 85.MacNair-Semands RR, Ogrodniczuk JS, Joyce AS. Structure and initial validation of a short form of the therapeutic factors inventory. Int J Group Psychother. 2010;60:245–281. doi: 10.1521/ijgp.2010.60.2.245. [DOI] [PubMed] [Google Scholar]
- 86.Rosenvinge JH, Pettersen G. Towards a comprehensive model of recovery, Relevant topics in Eating Disorders. In: Mental and Behavioural Disorders and Diseases of the Nervous System. Edited by Lobera IJ. InTech; 2012. p.
- 87.Paulson-Karlsson G, Nevonen L, Engström I. Anorexia nervosa: treatment satisfaction. J Fam Ther. 2006;28:293–306. doi: 10.1111/j.1467-6427.2006.00353.x. [DOI] [Google Scholar]
- 88.Shafran R, Clark DM, Fairburn CG, Arntz A, Barlow DH, Ehlers A, Freeston M, Garety PA, Hollon SD, Ost LG. Mind the gap: improving the dissemination of CBT. Behav Res Ther. 2009;47:902–909. doi: 10.1016/j.brat.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 89.Godart NT, Flament MF, Perdereau F, Jeammet P. Comorbidity between eating disorders and anxiety disorders: a review. Int J Eat Disord. 2002;32:253–270. doi: 10.1002/eat.10096. [DOI] [PubMed] [Google Scholar]
- 90.Welch E, Jangmo A, Thornton LM, Norring C, von Hausswolff-Juhlin Y, Herman BK, Pawaskar M, Larsson H, Bulik CM. Treatment-seeking patients with binge-eating disorder in the Swedish national registers: clinical course and psychiatric comorbidity. BMC psychiatry. 2016;16:1. doi: 10.1186/s12888-016-0840-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Rosenvinge JH, Martinussen M, Østensen E. The comorbidity of eating disorders and personality disorders: a metaanalytic review of studies published between 1983 and 1998. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity. 2000;5:52–61. doi: 10.1007/BF03327480. [DOI] [PubMed] [Google Scholar]
- 92.Friborg O, Martinussen M, Kaiser S, Øvergård KT, Martinsen EW, Schmierer P, Rosenvinge JH. Personality disorders in eating disorder not otherwise specified and binge eating disorder: a meta-analysis of comorbidity studies. J Nerv Ment Dis. 2014;202:119–125. doi: 10.1097/NMD.0000000000000080. [DOI] [PubMed] [Google Scholar]
- 93.Swanson SA, Crow SJ, Le Grange D, Swendsen J, Merikangas KR. Prevalence and correlates of eating disorders in adolescents: results from the national comorbidity survey replication adolescent supplement. Arch Gen Psychiatry. 2011;68:714–723. doi: 10.1001/archgenpsychiatry.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Carter O, Pannekoek L, Fursland A, Allen KL, Lampard AM, Byrne SM. Increased wait-list time predicts dropout from outpatient enhanced cognitive behaviour therapy (CBT-E) for eating disorders. Behav Res Ther. 2012;50:487–492. doi: 10.1016/j.brat.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 95.Fairburn CG. Cognitive behavior therapy and eating disorders. New York: The Guilford Press; 2008. [Google Scholar]
- 96.Freitas SR, Lopes CS, Appolinario JC, Coutinho W. The assessment of binge eating disorder in obese women: a comparison of the binge eating scale with the structured clinical interview for the DSM-IV. Eat Behav. 2006;7:282–289. doi: 10.1016/j.eatbeh.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 97.Beck, A. T. and Steer, R. A.Beck anxiety inventory manual
- 98.Garner DM. Eating disorder inventory-3 (EDI-3). Professional manual Odessa. Psychological Assessment Resources: FL; 2004. [Google Scholar]
- 99.Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985;29:71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- 100.Rosenvinge JH, Perry JA, Bjørgum L, Holte A. A new instrument measuring bulimia nervosa and disturbed eating patterns: development and validation of a 5-item scale. Eur Eat Disord Rev. 2001;9:123–132. doi: 10.1002/erv.371. [DOI] [Google Scholar]
- 101.Beck AT, Steer RA, Brown GK. Manual for the beck depression inventory-II. San Antonio, TX: Psychological Corporation. 1996;1:82.
- 102.Diener E. Assessing subjective well-being: progress and opportunities. Soc Indic Res. 1994;31:103–157. doi: 10.1007/BF01207052. [DOI] [Google Scholar]
- 103.Cantril H. The pattern of human concerns. New Brunswick: New Brunswick, N.J., Rutgers University Press; 1965. [Google Scholar]
- 104.Turner H, Bryant-Waugh R, Peveler R, Bucks RS. A psychometric evaluation of an English version of the Utrecht Coping List. Eur Eat Disord Rev. 2012;20(4):339–42. [DOI] [PubMed]
- 105.Friborg O, Hjemdal O, Rosenvinge JH, Martinussen M. A new rating scale for adult resilience: what are the central protective resources behind healthy adjustment? Int J Methods Psychiatr Res. 2003;12:65–76. doi: 10.1002/mpr.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Miller SD, Duncan BL, Brown J, Sparks JA, Claud DA. The outcome rating scale: a preliminary study of the reliability, validity, and feasibility of a brief visual analog measure. Journal of brief Therapy. 2003;2:91–100. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analysed.
The Project group monitor the data gathering and filing process continuously. Data are handled and stored according to guidelines given by the Norwegian Regional Committees for Medical and Health Research Ethics. All data are de-identified. The identification numbers are stored electronically and separate from the clinical data. The list that maps ID numbers to the personal information will be erased when the project is finished, thus completely anonymizing the data during the current study. Data will for the future be held within the project group.


