Abstract
Rationale: Several intensive care unit (ICU) organizational practices have been associated with improved patient outcomes. However, the uptake of these evidence-based practices is unknown.
Objectives: To assess diffusion of ICU organizational practices across the state of Pennsylvania.
Methods: We conducted two web-based, cross-sectional surveys of ICU organizational practices in Pennsylvania acute care hospitals, in 2005 (chief nursing officer respondents) and 2014 (ICU nurse manager respondents).
Measurements and Main Results: Of 223 eligible respondents, nurse managers from 136 (61%) medical, surgical, mixed medical-surgical, cardiac, and specialty ICUs in 98 hospitals completed the 2014 survey, compared with 124 of 164 (76%) chief nursing officers in the 2005 survey. In 2014, daytime physician staffing models varied widely, with 23 of 136 (17%) using closed models and 33 (24%) offering no intensivist staffing. Nighttime intensivist staffing was used in 37 (27%) ICUs, 38 (28%) used nonintensivist attending staffing, and 24 (18%) had no nighttime attending physicians. Daily multidisciplinary rounds occurred in 93 (68%) ICUs. Regular participants included clinical pharmacists in 68 of 93 (73%) ICUs, respiratory therapists in 62 (67%), and advanced practitioners in 37 (39%). Patients and family members participated in rounds in 36 (39%) ICUs. Clinical protocols or checklists for mechanically ventilated patients were available in 128 of 133 (96%) ICUs, low tidal volume ventilation for acute respiratory distress syndrome in 54 of 132 (41%) ICUs, prone positioning for severe acute respiratory distress syndrome in 37 of 134 (28%) ICUs, and family meetings in 19 of 134 (14%) ICUs. Among 61 ICUs that responded to both surveys, there was a significant increase in the proportion of ICUs using nighttime in-ICU attending physicians (23 [38%] in 2005 vs. 30 [49%] in 2014; P = 0.006).
Conclusions: The diffusion of evidence-based ICU organizational practices has been variable across the state of Pennsylvania. Only half of Pennsylvania ICUs have intensivists dedicated to the ICU. Variable numbers use clinical protocols for life-saving therapies, and few use structured family engagement strategies. In contrast, the diffusion of non–evidence-based practices, including overnight ICU attending physician staffing, is increasing. Future research should focus on promoting implementation of organizational evidence to promote high-quality ICU care.
Keywords: intensive care units, personnel staffing, clinical protocols, multidisciplinary communication, patient-centered care
There is increasing evidence linking organization factors and protocols to intensive care unit (ICU) patient outcomes. Observational studies have shown that staffing ICUs with nurses with higher levels of training and certification (1–3), higher nurse-to-bed ratios (1, 4), involvement of intensivist physicians in the care of all ICU patients (5–7), daily interprofessional rounds, and use of daily checklists (1, 7–10) are all associated with superior patient outcomes. Randomized clinical trials have demonstrated mortality benefits from clinical protocols for lung-protective mechanical ventilation strategies (11, 12), ventilator liberation (13), and management of sedative medications (13, 14). Several studies have shown the lack of a need for in-hospital nighttime intensivist staffing in closed ICUs (1, 4, 6, 15–17).
The uptake of this evidence base is increasingly supported by professional organizations such as the American College of Critical Care Medicine Task Force (18) and the Leapfrog Group (19, 20), as well as other key stakeholders. However, barriers to uptake have also been identified, including cost, loss of control, lack of leadership, and lack of ramifications for not implementing these structural and protocol changes, resulting in slow uptake, despite knowledge regarding the recommendations (21, 22).
Although there have been ICU-based studies performed (11, 15, 19, 20, 23–26), there have not been systematic attempts to examine diffusion of various ICU organizational practices within a geographically defined region. Therefore, we examined the patterns and trajectory of uptake across Pennsylvania ICUs so as to identify targets for future systems interventions that may improve care for the critically ill.
Some of the results of this study have been previously reported in the form of an abstract at the 2016 American Thoracic Society international conference (27).
Methods
Study Design and Population
We invited nurse managers of all 223 adult ICUs in all 169 acute care hospitals in the state of Pennsylvania to participate in a web-based survey.
Instrument Development and Administration
We created a draft instrument on the basis of previous surveys of ICU organization for content (23, 28). We then assembled two separate focus groups of attending and trainee intensivist physicians, with approximately 10 participants in each group, to provide feedback about the content, form, and structure. We further refined the instrument after a pilot test with 10 clinicians, including 6 ICU nurse leaders who would not be otherwise eligible to participate in the survey, 1 physician researcher with experience in survey design, and 3 nurse researchers.
The final instrument included 38 items and could be completed in approximately 10 to 15 minutes (see Appendix E1 in the online supplement) using the REDCap (Research Electronic Data Capture) electronic platform hosted at the University of Pennsylvania (29). Survey questions were divided into five categories: ICU organization, nurse staffing, physician staffing, staffing of other disciplines, and availability of clinical protocols.
We administered the survey from January to March 2014. We sent all eligible participants an invitation letter by mail, which included multiple means to access the survey (quick response code, web address, or request for an email link). Along with the invitation letter, we included a $20 bill (30). We sent nonrespondents postcards every 2 weeks for a total of 6 weeks after the initial invitation. At 8 weeks, we attempted to contact the nonresponding nurse managers directly by telephone to request their participation.
Additional Data Sources
We obtained hospital-level data from the American Hospital Association Annual Survey Database for fiscal year 2014, including total number of hospital and ICU beds, total number of hospital annual admissions, hospital ownership, affiliation with Accreditation Council for Graduate Medical Education programs, and resident-to-bed ratio. We used rural–urban continuum codes from the United States Department of Agriculture to evaluate urbanicity (31).
Linkage to Historical Survey Data
We linked the survey results to those from a survey in 2005 of hospital Chief Nursing Officers of PA hospitals (Appendix E2) (23, 32) to determine longitudinal trends in ICU organization factors. Questions common to the two surveys included those related to ICU capacity, daytime intensivist staffing, overall staffing, and multidisciplinary care. Hospitals that were common between the surveys and reported single ICUs were included for comparison. Hospitals that were common but differed in numbers of ICUs were explored further for types of patients cared for in each ICU. Three authors (R.K., V.M., M.P.K.) came to a consensus as to which ICUs matched between the two studies, excluding those that did not match.
Statistical Analyses
For all ICUs, we compared hospital characteristics between responders and nonresponders using Wilcoxon rank sum tests and chi-square tests as appropriate. For cases in which a single hospital had both responding and nonresponding ICUs, the hospital contributed data to both groups. For responding ICUs, we summarized survey responses using standard summary statistics. For items that were shared among both the 2005 and 2014 surveys, we compared responses using two-sample Student t tests and chi-square tests as appropriate.
We performed all analyses using STATA version 14.1 (StataCorp LP, College Station, TX). The study was approved by the Institutional Review Board of the University of Pennsylvania (Philadelphia, PA). The 2005 survey was approved by the Institutional Review Board of the University of Pittsburgh.
Results
Baseline Characteristics
Among 223 eligible ICUs in 154 hospitals, nurse managers completed the survey for 136 (61%) ICUs in 98 (64%) hospitals, compared with 124 of 164 (76%) chief nursing officers in the 2005 survey (32). Among the 141 (92%) hospitals for which American Hospital Association data were available, responding ICUs were more likely to be located in teaching hospitals than nonteaching hospitals, although these differences did not achieve statistical significance (Table 1). Table 2 summarizes the general characteristics of the 136 responding ICUs.
Table 1.
Hospital characteristics of responding and nonresponding intensive care units using external data
| Organization Characteristic | Responding ICUs (n = 129) | Nonresponding ICUs (n = 77) | P Value |
|---|---|---|---|
| No. of hospitals* | 92 | 63 | — |
| Total hospital beds, median (IQR) | 308 (150–493) | 228 (138–382) | 0.09 |
| Total hospital annual admissions, median (IQR) | 13,136 (5,508–25,201) | 10,112 (3,271–18,928) | 0.1 |
| Total ICU beds,† median (IQR) | 34 (12–61) | 26 (10–53) | 0.3 |
| Hospital ownership, n (%) | 0.9 | ||
| Not for profit | 111 (86) | 66 (86) | |
| For profit | 18 (14) | 11 (14) | |
| Accreditation Council for Graduate Medical Education programs, n (%) | 78 (61) | 40 (52) | 0.2 |
| Resident-to-bed ratio, median (IQR) | 0.07 (0–0.26) | 0.01 (0–0.13) | 0.07 |
| Metropolitan, n (%) | 110 (85) | 64 (83) | 0.7 |
Definition of abbreviations: ICU = intensive care unit; IQR = interquartile range.
Only includes hospitals for which American Hospital Association data were available (129/136 responders, 77/87 nonresponders); 14 hospitals include both responding and nonresponding ICUs and are included in both comparison groups.
Missing: 14 responding ICUs, 8 non-responding ICUs.
Table 2.
General intensive care unit characteristics as reported in the survey
| Organization Characteristic | ICUs (n = 136) |
|---|---|
| ICU operational beds, median (IQR) | 12 (9.5–18.5) |
| ICU annual admissions, median (IQR) | 1,050 (500–2,000) |
| ICU type | |
| General patients (mixed medical/surgical patients) | 78 (57) |
| General medical patients | 25 (18) |
| Cardiac patients (medical and surgical) | 14 (10) |
| General surgical patients | 11 (8) |
| Specialty patients (neurological, burn, or trauma patients only) | 8 (6) |
| ICU services | |
| Mechanical ventilation | 136 (100) |
| Vasopressor administration | 136 (100) |
| Targeted temperature management | 100 (74) |
| Continuous renal replacement therapy | 93 (68) |
| Extracorporeal membrane oxygenation | 25 (18) |
Definition of abbreviations: ICU = intensive care unit; IQR = interquartile range.
Data presented as n (%) unless otherwise noted.
ICU Staffing
Nurse staffing varied across responding ICUs (Table 3). One hundred twenty-one (89%) ICUs reported having dedicated nurse managers. Twenty-eight of 119 (24%) nurse managers managed more than one ICU. Similarly, 30 (22%) ICUs reported regular care from clinical nurse specialists. Six (4%) ICUs used at least one licensed practical nurse and seven (5%) used at least one nurse practitioner, in addition to registered nurses. Seventy-seven (57%) ICUs had at least one nurse with a Master’s degree. Only 18 (13%) ICUs had no nurses with critical care certification. A majority of ICUs, 89 (65%), allowed the maximum nurse patient assignment to be three or higher. The typical nurse-to–mechanically ventilated patient ratio was 1:2 (in 129 [95%] ICUs).
Table 3.
Intensive care unit nurse staffing
| ICU Staffing Characteristic | ICUs (n = 136) |
|---|---|
| Dedicated nurse manager | 121 (89) |
| Clinical nurse specialist provides care regularly | 30 (22) |
| Nursing licensure levels (any present) | |
| LPN | 6 (4) |
| RN | 136 (100) |
| NP | 7 (5) |
| Nursing education levels | |
| ADN | 123 (90) |
| BSN | 136 (100) |
| MSN | 77 (57) |
| Nursing specialty certification in critical care | |
| All nurses | 3 (2) |
| Some nurses | 115 (85) |
| None | 18 (13) |
| Maximum patient assignment* | |
| 2 | 47 (35) |
| 3 | 83 (61) |
| ≥4 | 6 (4) |
Definition of abbreviations: ADN = associates degree in nursing; BSN = bachelor of science in nursing; ICU = intensive care unit; LPN = licensed practical nurse; MSN = master of science in nursing; NP = nurse practitioner; RN = registered nurse.
Data presented as n (%).
95% reported the typical nurse-to–mechanically ventilated patient ratio during weekday, daytime hours to be 1:2.
Table 4 summarizes patterns of physician staffing across responding ICUs. One hundred six (78%) ICUs had dedicated physician directors. Sixty-one (45%) ICUs had high-intensity daytime intensivist staffing. An attending physician (either intensivist or nonintensivist) was available during nighttime hours in 75 (55%) ICUs. Twenty-three (17%) ICUs utilized remote patient monitoring, or tele-ICUs, which were staffed by intensivists in 14 (61%), nonintensivist attendings in 7 (30%), and nurses in 16 (70%). Remote monitoring was used during weekday daytime hours in 10 (44%) ICUs, weekday nighttime hours in 11 (48%) ICUs, weekend daytime hours in 8 (35%) ICUs, and weekend nighttime hours in 8 (35%) ICUs. Seventy-nine of 134 (59%) ICUs routinely had fellows or residents participate in patient care.
Table 4.
Intensive care unit physician staffing
| ICU Staffing Characteristic | ICUs (n = 136) |
|---|---|
| Dedicated physician ICU director | 106 (78) |
| Daytime intensivist staffing model | |
| Primary responsibility for all patients on admission | 23 (17) |
| Primary attending or consults on all patients by ICU policy/guideline | 38 (28) |
| Consults on certain patients by policy/guideline and on other patients only when requested by an attending physician | 20 (15) |
| Consults on patients only when requested by the primary attending physician | 21 (15) |
| No intensivist is available | 33 (24) |
| Tele-ICU | 1 (1) |
| Senior-most clinician available in person overnight | |
| Intensivist attending physician | 37 (27) |
| Nonintensivist attending physician | 38 (28) |
| Resident, fellow, or other trainee | 27 (20) |
| Advanced practitioner | 8 (6) |
| No physician or physician-equivalent clinician, but physicians from other parts of the hospital | 24 (18) |
| No physician or physician equivalent is available in person | 2 (2) |
| Patient monitoring by tele-ICU | 23 (17) |
| Trainees routinely participate in patient care* | 79 (59) |
Definition of abbreviation: ICU = intensive care unit.
Data presented as n (%).
Missing: two ICUs.
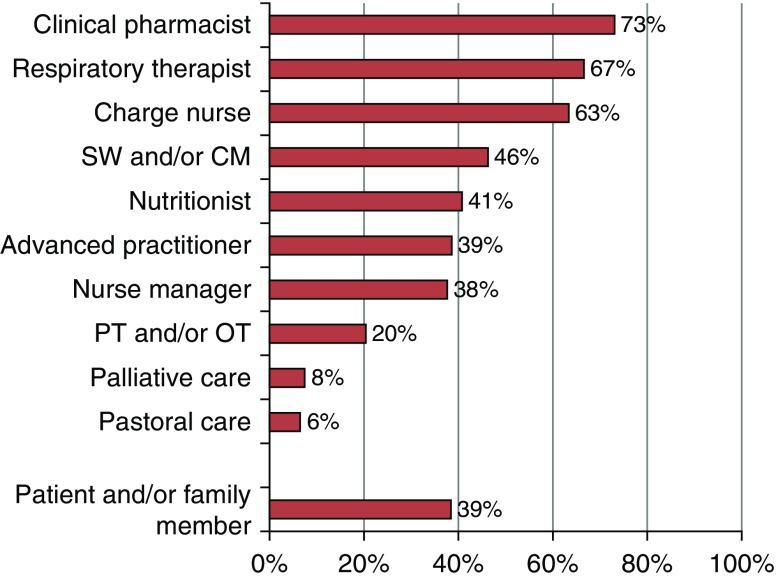
In addition to physicians and bedside nurses, care providers who provided care regularly (on at least 3 days weekly) are summarized in Table 5. Daily team rounds at least 5 days weekly occurred in 93 (68%) ICUs. Regular participants in rounds are shown in Figure 1. The patient and/or a family member participated in rounds in 36 (39%) ICUs.
Table 5.
Multidisciplinary care
| ICU Clinician | Clinicians Providing Care on a Regular Basis (≥3 d weekly) (n = 136) |
|---|---|
| Respiratory therapists | 133 (98) |
| Social workers and/or case managers | 129 (95) |
| Physical therapists and/or occupational therapists | 121 (89) |
| Nutritionists | 115 (85) |
| Clinical pharmacists | 102 (75) |
| Advanced practitioners | 77 (57) |
| Pastoral care | 74 (54) |
| Palliative care | 71 (52) |
Definition of abbreviation: ICU = intensive care unit.
Data presented as n (%).
Figure 1.
Participants present on daily team rounds (in addition to physician and bedside nurse) (n = 93). CM = case manager; OT = occupational therapist; PT = physical therapist; SW = social worker.
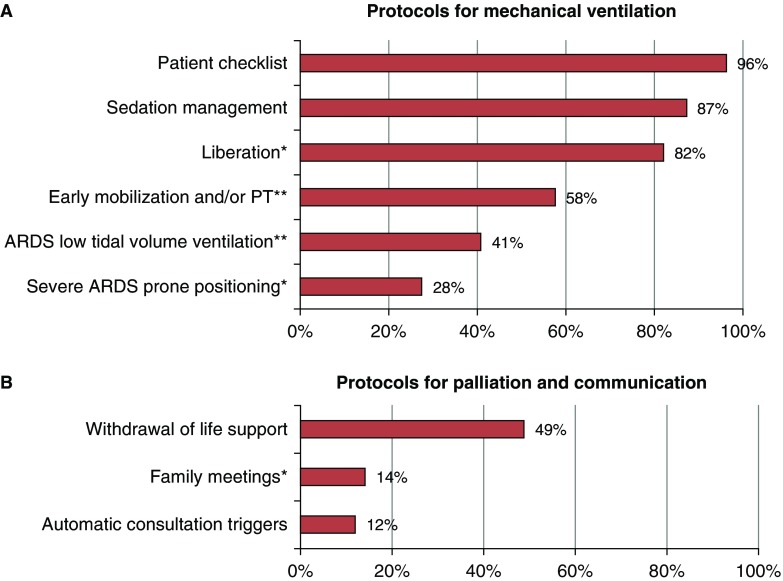
ICU Protocols
Overall, protocols or checklists for mechanically ventilated patients were used in 128 of 133 (96%) ICUs (Figure 2). Automatic triggers for palliative care consultation were used in 16 (12%) ICUs, and protocols for family meetings were used in 19 (14%) ICUs. Common elements included in family meeting protocols regarded the timing of the first and subsequent family meetings and triggers for the most severely ill patients.
Figure 2.
Presence of intensive care unit protocols (n = 133). *n = 134; **n = 132. ARDS = acute respiratory distress syndrome; PT = physical therapist.
Delirium was routinely measured in 83 of 132 (63%) ICUs. Of these, 70 (84%) used the Confusion Assessment Method for the ICU (33, 34), 2 (2%) used the Nursing Delirium Screening Scale (35), 3 (4%) used the Delirium Detection Score (36), and 7 (8%) used other scales, including the Intensive Care Delirium Screening Checklist (7%) (37); the remaining ICU reported using the Vanderbilt ABCDE delirium and safety bundle without specifying the delirium scale used (38).
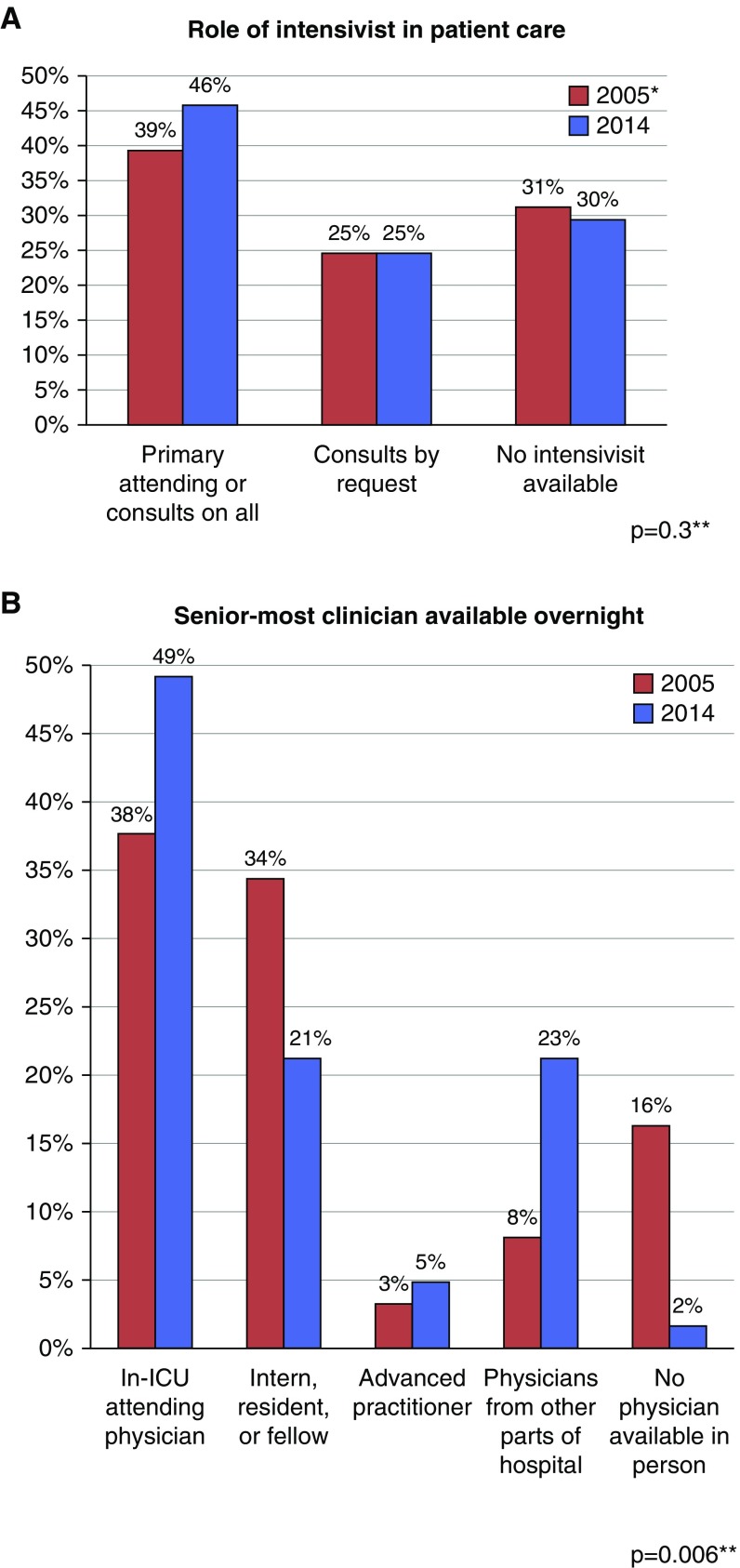
Temporal Trends in ICU Organization Factors
Data for 61 ICUs were available from both the 2005 and the 2014 surveys. There were no differences in the reported number of operational ICU beds (median, 12 [interquartile range (IQR), 8–16] in 2005 vs. 12 [IQR, 8–16] in 2014; P = 0.98), the proportion with daily multidisciplinary rounds (39 of 60 [65%] in 2005 vs. 39 of 61 [64%] in 2014; P = 0.9), or the proportion reporting the availability of a case manager (54 [89%] in 2005 vs. 57 [93%] in 2014; P = 0.3), palliative care (27 of 59 [46%] in 2005 vs. 31 of 61 [51%] in 2014; P = 0.6), or pastoral care (26 of 57 [46%] in 2005 vs. 32 of 61 [52%] in 2014; P = 0.5) between the study periods. There was also no significant change in the role of intensivists in patient care; however, there was increased coverage during nighttime hours by in-hospital physicians, with a shift of coverage from trainees to attending physicians (P = 0.006) (Figure 3).
Figure 3.
Temporal trends in intensive care unit (ICU) physician staffing. *5% reported “Other”; **chi-square test.
Discussion
This study describes the diffusion of recommendations and scientific evidence regarding ICU organizational factors and assesses temporal trends in organizational models across a diverse group of hospitals. Despite the literature linking specific ICU organizational structures with superior patient outcomes, and professional society recommendations from the American College of Critical Care Medicine Task Force (18) and the Leapfrog Group (19, 20), among others, adoption of these structures remains incomplete. Having at least some nurses with critical care certification and high nurse-to-patient ratio for mechanically ventilated patients has been nearly universally adopted. However, nearly one-third of ICUs have no regular availability of intensivists. A quarter of ICUs have no dedicated clinical pharmacists, despite studies demonstrating a reduction in medication errors (39) and downstream benefits to patient outcomes (40). Fewer than half of ICUs have clinical protocols for lung-protective ventilation (12) and prone positioning in ARDS (41).
Policies for structured family engagement are also uncommon. Only a quarter of ICUs engage patients and family members in daily team rounds, and even fewer have guidelines regarding family meetings. Although the evidence of benefit from family engagement is limited (42), family engagement is consistent with principles of autonomy and patient-centered care and expert recommendations for patient and family support in the ICU (43).
The most notable change in ICU organization over the past 10 years is in nighttime physician coverage. Compared with 2005, the same ICUs in 2014 more commonly used physicians in the ICU at night. These changes occurred despite evidence suggesting that nighttime intensivist staffing does not improve patient survival or perhaps other outcomes (1, 6, 16, 23, 44).
Why is there incomplete adoption of some evidence-based organizational practices and guideline recommendations but at the same time increases in some practices against high-quality evidence? This question remains unanswered, but there may be several factors at play. Previous literature cites high costs, lack of leadership, and lack of accountability as barriers to evidence uptake, particularly to what may be perceived to be large organizational changes (21, 22). On the other hand, although acknowledging that nighttime intensivists do not save lives on a population level, in the era of patient safety, hospitals may be willing to invest in this staffing practice to save the individual marginal lives, using the principle of “rule of rescue” rather than utilitarianism. In addition, anecdotes of poor outcomes may compel health systems to intervene despite the lack of benefit in the literature, or hospital administrators may be compelled to compete with their local markets in being able to advertise the most “advanced services.” Future work should seek to better understand these and other drivers of organizational decisions (22), methods to overcome barriers to evidence uptake, and alternative staffing solutions that may be as effective (45).
Strengths and Limitations
This study has several strengths. It includes a large and organizationally diverse population of ICUs. The response rate is high compared with other studies of health care providers (46–49). Although there were some differences among responders and nonresponders, there was an overrepresentation of academic ICUs, which are more likely to have dedicated intensivists and interprofessional rounds. Therefore, the prevalence of these organizational factors, if anything, is overestimated. As the prevalence of these staffing practices was still quite low compared with the universal recommendations, the true proportions may be even lower than our findings suggest. To our knowledge, this is the first study to evaluate temporal trends of organizational practices in a diverse group of ICUs.
However, the results must also be interpreted in the context of the study limitations. First, data from the 2014 survey reflect the views of ICU nurse managers. As shown in a prior study, nurse managers and physicians often answer the same objective and subjective questions differently (50). Furthermore, regardless of respondent, there is always a risk that survey responses may not reflect actual practice (51, 52). However, surveys are more feasible than other means (such as direct observation or site visits) to obtain these data on a large population of hospitals, and prior organizational research has utilized similar methods (1, 2, 7). We chose to study this population specifically because there were dedicated nurse managers in the vast majority of ICUs and because these were the most consistent staff present in these ICUs (21).
Second, the 2014 survey elicited information on the presence of clinical protocols but did not specify what is contained in them, how they are operationalized, and how they are followed. However, we did not believe that any data we could obtain on protocol adherence by self-report would be reliable (51, 52). Third, the question regarding nursing licensure captured the presence of any single nurse with a particular licensure in that ICU rather than the proportion of nurses with each licensure, which has different implications for outcomes and organizational practices.
Finally, in our longitudinal comparison, questions were asked of different populations (ICU nurse managers in the 2014 survey vs. chief nursing officers of the hospitals surveyed in 2005), using different phrasing and survey questions, and were limited to a subset of the ICUs in the surveys, making comparability and applicability limited. However, we avoided comparing subjective measures and focused on objective measures between the two studies.
Even in light of these limitations, we believe the information in this study is still of vital importance. Despite prior ICU-based studies evaluating individual organizational practices (15, 19, 20, 23–26), all of the research to date has not increased evidence-based ICU management, and we do not yet understand why. Our study highlights this point across a wide geographical and diverse population for a broad range of organizational practices. Perceptions of clinician leaders are fundamental to understanding these barriers to evidence implementation to subsequently enact change. In addition, the longitudinal data provide novel insights into ICU organizational practices and highlight areas to focus future studies.
Conclusions
At a time when evidence and recommendations support the use of intensivist-led multidisciplinary ICU care, the diffusion of these ICU organizational practices has been variable and lacking. Only half of Pennsylvania ICUs have intensivists dedicated to the ICU; one-third do not have regular team rounds, clinical protocols for life-saving therapies are limited, and structured family engagement is rare. In contrast, the diffusion of non–evidence-based practices, including overnight ICU attending physician staffing, is increasing.
Future research should focus on better understanding barriers to implementation of evidence-based organizational practices, contributors to implementing non–evidence-based practices, testing strategies to improve evidence uptake, and consideration of alternative staffing practices (45), to promote high-quality ICU care.
Additional material
Supplementary data supplied by authors.
Footnotes
Supported by National Institutes of Health/NHLBI grants T32 HL007891 (R.K.) and K08 HL116771 (M.P.K.), and National Institutes of Health/National Institute on Aging grant K08 AG21921 for the 2005 survey (A.E.B.).
Author Contributions: All authors made substantial contributions to the conception or design of the study; the acquisition, analysis, or interpretation of data; and drafting or revising the manuscript.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Checkley W, Martin GS, Brown SM, Chang SY, Dabbagh O, Fremont RD, Girard TD, Rice TW, Howell MD, Johnson SB, et al. United States Critical Illness and Injury Trials Group Critical Illness Outcomes Study Investigators. Structure, process, and annual ICU mortality across 69 centers: United States Critical Illness and Injury Trials Group Critical Illness Outcomes Study. Crit Care Med. 2014;42:344–356. doi: 10.1097/CCM.0b013e3182a275d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boev C, Xue Y, Ingersoll GL. Nursing job satisfaction, certification and healthcare-associated infections in critical care. Intensive Crit Care Nurs. 2015;31:276–284. doi: 10.1016/j.iccn.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 3.Boyle DK, Cramer E, Potter C, Gatua MW, Stobinski JX. The relationship between direct-care RN specialty certification and surgical patient outcomes. AORN J. 2014;100:511–528. doi: 10.1016/j.aorn.2014.04.018. [DOI] [PubMed] [Google Scholar]
- 4.Sakr Y, Moreira CL, Rhodes A, Ferguson ND, Kleinpell R, Pickkers P, Kuiper MA, Lipman J, Vincent JL Extended Prevalence of Infection in Intensive Care Study Investigators. The impact of hospital and ICU organizational factors on outcome in critically ill patients: results from the Extended Prevalence of Infection in Intensive Care study. Crit Care Med. 2015;43:519–526. doi: 10.1097/CCM.0000000000000754. [DOI] [PubMed] [Google Scholar]
- 5.Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA. 2002;288:2151–2162. doi: 10.1001/jama.288.17.2151. [DOI] [PubMed] [Google Scholar]
- 6.Wilcox ME, Chong CA, Niven DJ, Rubenfeld GD, Rowan KM, Wunsch H, Fan E. Do intensivist staffing patterns influence hospital mortality following ICU admission? A systematic review and meta-analyses. Crit Care Med. 2013;41:2253–2274. doi: 10.1097/CCM.0b013e318292313a. [DOI] [PubMed] [Google Scholar]
- 7.Yoo EJ, Edwards JD, Dean ML, Dudley RA. Multidisciplinary critical care and intensivist staffing: results of a statewide survey and association with mortality. J Intensive Care Med. 2016;31:325–332. doi: 10.1177/0885066614534605. [DOI] [PubMed] [Google Scholar]
- 8.Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, Sexton B, Hyzy R, Welsh R, Roth G, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med. 2006;355:2725–2732. doi: 10.1056/NEJMoa061115. [DOI] [PubMed] [Google Scholar]
- 9.Weiss CH, Moazed F, McEvoy CA, Singer BD, Szleifer I, Amaral LAN, Kwasny M, Watts CM, Persell SD, Baker DW, et al. Prompting physicians to address a daily checklist and process of care and clinical outcomes: a single-site study. Am J Respir Crit Care Med. 2011;184:680–686. doi: 10.1164/rccm.201101-0037OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AHS, Dellinger EP, Herbosa T, Joseph S, Kibatala PL, Lapitan MC, et al. Safe Surgery Saves Lives Study Group. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360:491–499. doi: 10.1056/NEJMsa0810119. [DOI] [PubMed] [Google Scholar]
- 11.Needham DM, Colantuoni E, Mendez-Tellez PA, Dinglas VD, Sevransky JE, Dennison Himmelfarb CR, Desai SV, Shanholtz C, Brower RG, Pronovost PJ. Lung protective mechanical ventilation and two year survival in patients with acute lung injury: prospective cohort study. BMJ. 2012;344:e2124. doi: 10.1136/bmj.e2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 13.Jakob SM, Lubszky S, Friolet R, Rothen HU, Kolarova A, Takala J. Sedation and weaning from mechanical ventilation: effects of process optimization outside a clinical trial. J Crit Care. 2007;22:219–228. doi: 10.1016/j.jcrc.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 14.Dale CR, Kannas DA, Fan VS, Daniel SL, Deem S, Yanez ND, III, Hough CL, Dellit TH, Treggiari MM. Improved analgesia, sedation, and delirium protocol associated with decreased duration of delirium and mechanical ventilation. Ann Am Thorac Soc. 2014;11:367–374. doi: 10.1513/AnnalsATS.201306-210OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kerlin MP, Harhay MO, Kahn JM, Halpern SD. Nighttime intensivist staffing, mortality, and limits on life support: a retrospective cohort study. Chest. 2015;147:951–958. doi: 10.1378/chest.14-0501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kerlin MP, Small DS, Cooney E, Fuchs BD, Bellini LM, Mikkelsen ME, Schweickert WD, Bakhru RN, Gabler NB, Harhay MO, et al. A randomized trial of nighttime physician staffing in an intensive care unit. N Engl J Med. 2013;368:2201–2209. doi: 10.1056/NEJMoa1302854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Soares M, Bozza FA, Angus DC, Japiassú AM, Viana WN, Costa R, Brauer L, Mazza BF, Corrêa TD, Nunes AL, et al. Organizational characteristics, outcomes, and resource use in 78 Brazilian intensive care units: the ORCHESTRA study. Intensive Care Med. 2015;41:2149–2160. doi: 10.1007/s00134-015-4076-7. [DOI] [PubMed] [Google Scholar]
- 18.Weled BJ, Adzhigirey LA, Hodgman TM, Brilli RJ, Spevetz A, Kline AM, Montgomery VL, Puri N, Tisherman SA, Vespa PM, et al. Task Force on Models for Critical Care. Critical care delivery: the importance of process of care and ICU structure to improved outcomes: an update from the American College of Critical Care Medicine Task Force on Models of Critical Care. Crit Care Med. 2015;43:1520–1525. doi: 10.1097/CCM.0000000000000978. [DOI] [PubMed] [Google Scholar]
- 19.Pronovost PJ, Needham DM, Waters H, Birkmeyer CM, Calinawan JR, Birkmeyer JD, Dorman T. Intensive care unit physician staffing: financial modeling of the Leapfrog standard. Crit Care Med. 2004;32:1247–1253. doi: 10.1097/01.ccm.0000128609.98470.8b. [DOI] [PubMed] [Google Scholar]
- 20.The Leapfrog Group[Accessed 2016. Nov 3.] Available from: http://www.leapfroggroup.org [Google Scholar]
- 21.Kahn JM, Matthews FA, Angus DC, Barnato AE, Rubenfeld GD. Barriers to implementing the Leapfrog Group recommendations for intensivist physician staffing: a survey of intensive care unit directors. J Crit Care. 2007;22:97–103. doi: 10.1016/j.jcrc.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 22.Moran J, Scanlon D. Slow progress on meeting hospital safety standards: learning from the Leapfrog Group’s efforts. Health Aff (Millwood) 2013;32:27–35. doi: 10.1377/hlthaff.2011.0056. [DOI] [PubMed] [Google Scholar]
- 23.Wallace DJ, Angus DC, Barnato AE, Kramer AA, Kahn JM. Nighttime intensivist staffing and mortality among critically ill patients. N Engl J Med. 2012;366:2093–2101. doi: 10.1056/NEJMsa1201918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kalhan R, Mikkelsen M, Dedhiya P, Christie J, Gaughan C, Lanken PN, Finkel B, Gallop R, Fuchs BD. Underuse of lung protective ventilation: analysis of potential factors to explain physician behavior. Crit Care Med. 2006;34:300–306. doi: 10.1097/01.ccm.0000198328.83571.4a. [DOI] [PubMed] [Google Scholar]
- 25.Needham DM, Colantuoni E, Mendez-Tellez PA, Dinglas VD, Sevransky JE, Dennison Himmelfarb CR, Desai SV, Shanholtz C, Brower RG, Pronovost PJ. Lung protective mechanical ventilation and two year survival in patients with acute lung injury: prospective cohort study. BMJ. 2012;344:e2124. doi: 10.1136/bmj.e2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ward NS, Afessa B, Kleinpell R, Tisherman S, Ries M, Howell M, Halpern N, Kahn J Members of Society of Critical Care Medicine Taskforce on ICU Staffing. Intensivist/patient ratios in closed ICUs: a statement from the Society of Critical Care Medicine Taskforce on ICU Staffing. Crit Care Med. 2013;41:638–645. doi: 10.1097/CCM.0b013e3182741478. [DOI] [PubMed] [Google Scholar]
- 27.Kohn R, Madden V, Kahn JM, Asch DA, Barnato AE, Halpern SD, Kerlin MP.Variation in intensive care unit organizational patterns: a state-wide analysis[abstract]. Am J Respir Crit Care Med 2016193A4698 [Google Scholar]
- 28.Kim MM, Barnato AE, Angus DC, Fleisher LA, Kahn JM. The effect of multidisciplinary care teams on intensive care unit mortality. Arch Intern Med. 2010;170:369–376. doi: 10.1001/archinternmed.2009.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ulrich CM, Danis M, Koziol D, Garrett-Mayer E, Hubbard R, Grady C. Does it pay to pay? A randomized trial of prepaid financial incentives and lottery incentives in surveys of nonphysician healthcare professionals. Nurs Res. 2005;54:178–183. doi: 10.1097/00006199-200505000-00005. [DOI] [PubMed] [Google Scholar]
- 31. United States Department of Agriculture. Economic Research Service Rural-Urban Continuum Codes [updated 2013 May 10; accessed 2016 Mar 3]. Available from: https://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx.
- 32.Lin CY, Farrell MH, Lave JR, Angus DC, Barnato AE. Organizational determinants of hospital end-of-life treatment intensity. Med Care. 2009;47:524–530. doi: 10.1097/MLR.0b013e31819261bd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, Truman B, Speroff T, Gautam S, Margolin R, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU) JAMA. 2001;286:2703–2710. doi: 10.1001/jama.286.21.2703. [DOI] [PubMed] [Google Scholar]
- 34.Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R, Speroff T, Gautam S, Bernard GR, Inouye SK. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) Crit Care Med. 2001;29:1370–1379. doi: 10.1097/00003246-200107000-00012. [DOI] [PubMed] [Google Scholar]
- 35.Gaudreau JD, Gagnon P, Harel F, Tremblay A, Roy MA. Fast, systematic, and continuous delirium assessment in hospitalized patients: the nursing delirium screening scale. J Pain Symptom Manage. 2005;29:368–375. doi: 10.1016/j.jpainsymman.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 36.Otter H, Martin J, Bäsell K, von Heymann C, Hein OV, Böllert P, Jänsch P, Behnisch I, Wernecke KD, Konertz W, et al. Validity and reliability of the DDS for severity of delirium in the ICU. Neurocrit Care. 2005;2:150–158. doi: 10.1385/NCC:2:2:150. [DOI] [PubMed] [Google Scholar]
- 37.Bergeron N, Dubois MJ, Dumont M, Dial S, Skrobik Y. Intensive Care Delirium Screening Checklist: evaluation of a new screening tool. Intensive Care Med. 2001;27:859–864. doi: 10.1007/s001340100909. [DOI] [PubMed] [Google Scholar]
- 38.Pandharipande P, Banerjee A, McGrane S, Ely EW. Liberation and animation for ventilated ICU patients: the ABCDE bundle for the back-end of critical care. Crit Care. 2010;14:157. doi: 10.1186/cc8999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Leape LL, Cullen DJ, Clapp MD, Burdick E, Demonaco HJ, Erickson JI, Bates DW. Pharmacist participation on physician rounds and adverse drug events in the intensive care unit. JAMA. 1999;282:267–270. doi: 10.1001/jama.282.3.267. [DOI] [PubMed] [Google Scholar]
- 40.Beardsley JR, Jones CM, Williamson J, Chou J, Currie-Coyoy M, Jackson T. Pharmacist involvement in a multidisciplinary initiative to reduce sepsis-related mortality. Am J Health Syst Pharm. 2016;73:143–149. doi: 10.2146/ajhp150186. [DOI] [PubMed] [Google Scholar]
- 41.Guérin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, Mercier E, Badet M, Mercat A, Baudin O, et al. PROSEVA Study Group. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 42.Cypress BS. Family presence on rounds: a systematic review of literature. Dimens Crit Care Nurs. 2012;31:53–64. doi: 10.1097/DCC.0b013e31824246dd. [DOI] [PubMed] [Google Scholar]
- 43.Davidson JE, Powers K, Hedayat KM, Tieszen M, Kon AA, Shepard E, Spuhler V, Todres ID, Levy M, Barr J, et al. American College of Critical Care Medicine Task Force 2004-2005, Society of Critical Care Medicine. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004-2005. Crit Care Med. 2007;35:605–622. doi: 10.1097/01.CCM.0000254067.14607.EB. [DOI] [PubMed] [Google Scholar]
- 44.Kerlin MP, Halpern SD. Nighttime physician staffing improves patient outcomes: no. Intensive Care Med. 2016;42:1469–1471. doi: 10.1007/s00134-016-4367-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kahn JM, Rubenfeld GD. The myth of the workforce crisis: why the United States does not need more intensivist physicians. Am J Respir Crit Care Med. 2015;191:128–134. doi: 10.1164/rccm.201408-1477CP. [DOI] [PubMed] [Google Scholar]
- 46.Asch DAJ, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50:1129–1136. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]
- 47.Halpern SD, Asch DA. Commentary: Improving response rates to mailed surveys: what do we learn from randomized controlled trials? Int J Epidemiol. 2003;32:637–638. doi: 10.1093/ije/dyg184. [DOI] [PubMed] [Google Scholar]
- 48.Halpern SD, Kohn R, Dornbrand-Lo A, Metkus T, Asch DA, Volpp KG. Lottery-based versus fixed incentives to increase clinicians’ response to surveys. Health Serv Res. 2011;46:1663–1674. doi: 10.1111/j.1475-6773.2011.01264.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kellerman SE, Herold J. Physician response to surveys: a review of the literature. Am J Prev Med. 2001;20:61–67. doi: 10.1016/s0749-3797(00)00258-0. [DOI] [PubMed] [Google Scholar]
- 50.Costa DK, Kuza CC, Kahn JM. Differences between nurse- and physician-assessed ICU characteristics using a standardized survey. Int J Qual Health Care. 2015;27:344–348. doi: 10.1093/intqhc/mzv062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Adams AS, Soumerai SB, Lomas J, Ross-Degnan D. Evidence of self-report bias in assessing adherence to guidelines. Int J Qual Health Care. 1999;11:187–192. doi: 10.1093/intqhc/11.3.187. [DOI] [PubMed] [Google Scholar]
- 52.Brunkhorst FM, Engel C, Ragaller M, Welte T, Rossaint R, Gerlach H, Mayer K, John S, Stuber F, Weiler N, et al. German Sepsis Competence Network (SepNet) Practice and perception--a nationwide survey of therapy habits in sepsis. Crit Care Med. 2008;36:2719–2725. doi: 10.1097/CCM.0b013e318186b6f3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.