Abstract
Background:
Respiratory swallowing coordination is regarded as one of the several mechanisms by which the airway is protected from aspiration during swallowing. A lack of reciprocity between respiration and swallowing has been indicated as one of the mechanisms that can lead to aspiration and pneumonia. Since chronic obstructive pulmonary disease (COPD) is a pulmonary condition, we have hypothesized that there would be deficits observed in respiratory-swallow coordination in individuals with COPD. Hence, the present study was planned to investigate the respiratory-swallow coordination in individuals with COPD.
Methods:
Thirty-two individuals with the diagnosis of COPD and 32 normal controls were recruited for the study. Respiratory coordination for swallowing was measured using Kay Digital Swallowing Workstation. The specific swallowing tasks were recorded for each individual which was dry swallow, thin liquid swallow, and thick liquid swallow.
Results:
The results revealed that there was a significant difference between individuals with COPD and normal controls indicating that swallow apnea duration is prolonged in individuals with COPD. It was also observed that expiration-inspiration is the predominant pattern, followed by expiration-expiration, inspiration-expiration, and inspiration-inspiration in individuals with COPD when compared to predominant expiration-expiration swallow in normal controls followed by expiration-inspiration, inspiration-expiration, and inspiration-inspiration.
Conclusion:
The results of the present study gave an insight into the pattern of respiratory-swallowing coordination in individuals with COPD.
KEY WORDS: Chronic obstructive pulmonary disease, respiratory-swallow coordination, swallow apnea
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is a disease, characterized by repeated airflow obstruction that is usually progressive and is associated with an enhanced chronic inflammatory response within the airways and the lung to noxious particles or gases.[1] This would reduce the airflow to the lungs, causing problems such as wheezing, breathing difficulty, and cough. This may possibly affect swallowing also. As the patients with COPD have reduced ventilator capacity, the coordination between breathing and swallowing can be severely disrupted, which in turn poses serious health risks.
According to Dozier, dysphagia affects at least 12% of patients in acute care hospitals and more than 50% of those in chronic care settings.[2] The presence of dysphagia is associated with aspiration-induced chest infections and increases the risk of serious respiratory consequences such as pneumonia. Identification of the patient at risk of aspiration is important from a clinical viewpoint. Abnormalities impacting functional swallowing status and presenting an aspiration risk for patients with COPD include reduced laryngeal elevations with delayed laryngeal closure, reduced laryngeal-pharyngeal sensation, impaired pharyngeal clearance, cricopharyngeal dysfunction, and gastroesophageal reflux disease.[3] We concluded that the risk for aspiration in the COPD population is not limited to the presence of valleculae residue, and this cannot be seen as an isolated factor in an attempt to explain swallowing alterations in this population. Even though studies have addressed the relationship between COPD and oropharyngeal swallowing, results are favoring oropharyngeal dysphagia only during the exacerbated conditions of COPD as reported by O'Kane and Groher.[4] However, limited studies exist on respiratory-swallowing coordination during the stable state of COPD individuals, and hence, the present study is planned to investigate the respiratory-swallow coordination in individuals with COPD.
METHODS
This study followed the cross-sectional control group design. The participants were divided into two groups within the age range of 18–65 years. Group 1 consisted of 32 individuals with the diagnosis of COPD. The diagnosis of COPD was performed by an experienced physician in the field of pulmonary medicine based on the signs, symptoms, and lung function tests. All the types of COPD were included in this group. Group 2 consisted of 32 age- and gender-matched normal controls. The exclusion criteria for Group 2 considered were the history of respiratory, speech, and swallowing problems.
Instrumentation
All swallowing measurements were performed using the Kay Digital Swallowing Workstation and Swallowing Signals Laboratory {Model 7120, Kay PENTAX, Montvale, NJ, USA}. It is a computer-integrated system for the simultaneous measurement of surface electromyography, nasal airflow monitoring, and cervical auscultation.
Procedure
Each participant was made to sit on a comfortable chair. The respiratory-swallowing coordination was assessed using the Kay Digital Swallowing Workstation connected to swallowing signal laboratory hardware {Model 7120; PENTAX Medicals}. The calibrated nasal catheter was positioned at the entrance of nares. Two tasks considered were thin liquid swallow and thick liquid swallow with 5 ml and 10 ml quantity. Respiratory information (inhalation/exhalation) displayed as a line tracing was recorded for all swallowing attempts. Swallow apnea as well as the respiratory phase where the swallow apnea occurs was measured for each volume and consistency of the bolus. Vertical cursors were superimposed at the onset and offset of the swallowing apnea, and the duration of apnea was measured. Descriptive statistics was conducted to obtain mean and standard deviation (SD) of swallow apnea in both group of participants. One-way repeated measures ANOVA was employed to compare the significance of difference between the means of both groups for swallow apnea duration across the bolus consistency and volume. Percentage of swallows occurring in different phases of respiration was also analyzed.
RESULTS
The present study was carried out to investigate the effect of COPD on swallow apnea duration and the respiratory phase where the swallow apnea occurred. Descriptive statistical analysis was employed to obtain mean and SD for swallow apnea duration across the groups, bolus consistency and bolus volume which is shown in Figure 1.
Figure 1.
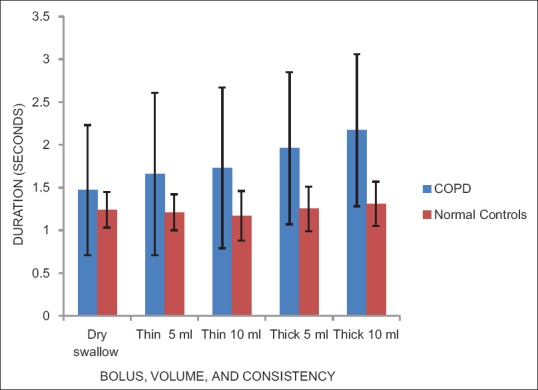
Swallow apnea duration in chronic obstructive pulmonary disease and normal controls
From the Figure 1, it can be inferred that individuals with COPD had longer swallow apnea duration in comparison to the normal group. Repeated measures ANOVA was performed with bolus consistency and bolus volume as within group variables and between-group variables.
The results of repeated measures ANOVA revealed that there was a significant main effect of the groups P = 0.00. Results also revealed that there was no significant main effect of bolus volume (F{1,71}= 2.253; P = 0.138), but there was a significant difference observed for bolus consistency (F{1,71}= 10.302; P = 0.002). The interaction of bolus volume versus group (F{1,71}= 1.994; P = 0.168), bolus consistency versus group (F{1,71}= 3.814; P = 0.055), bolus volume versus consistency (F{1,71} = 0.956; P = 0.331), and bolus volume versus bolus consistency versus group (F{1,71} = 0.017; P = 0.896) were not significant.
Since dry swallow was not performed with different bolus volumes and consistencies, independent t-test was performed between the two groups and the results revealed no significant difference between the groups (t{62}=1.618, P > 0.05).
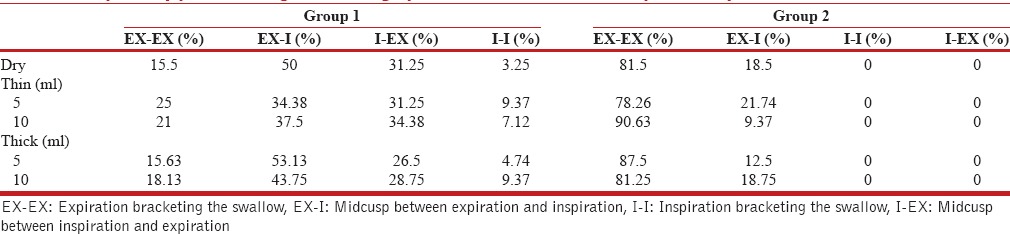
Respiratory phase during which swallowing apnea occurred was expressed in percentages across various food consistencies and volumes for both the groups of participants. The coding for various respiratory patterns during swallow apnea is shown below.
EX-EX – Expiration bracketing the swallow
EX-I – Midcusp between expiration and inspiration
I-I – Inspiration bracketing the swallow
I-EX – Midcusp between inspiration and expiration.
From Table 1, it can be observed that the predominant respiratory pattern exhibited by individuals with COPD was expiration-inspiration, followed by inspiration-expiration, expiration-expiration, and inspiration-inspiration. However, normal individuals exhibited predominantly expiration-expiration followed by expiration-inspiration. Similar trend was seen across all the bolus consistencies and bolus volume too. These findings suggest that the respiratory phase during swallow apnea is deviant in individuals with COPD when compared to normal controls.
Table 1.
Respiratory phase during swallowing apnea in chronic obstructive pulmonary disease and normal controls
DISCUSSION
Respiration and swallowing coordination is required to protect the airway from aspiration. This coordination may be disrupted in individuals with respiratory illness. In the present study, it was hypothesized that individuals with COPD have respiratory-swallowing incoordination when compared with normal controls. Hence, the present study investigated the respiratory-swallow coordination in individuals with COPD using nasal airflow module of digital swallowing workstation. Results revealed that majority of the swallows occurred was during expiration-inspiration phase followed by inspiration-expiration, expiration-expiration, and inspiration-inspiration in comparison to predominant expiration bracketing swallowing in normal adults.
Gross et al. have reported that COPD individuals swallowed solids during inhalation and had a higher rate of inhalation after swallowing semisolid food. They have attributed their findings to the reduced ventilator capacity.[5] Inhalation before swallowing suggests that the respiratory systems need for ventilation supersedes the swallowing. Martin-Harris concluded that patients attempting to maintain breathing activity as long as possible before the obligatory apneic pause, and trying to reestablish respiration quickly while eating semisolids and solids may present channeling of a bolus to the level of the pyriform sinuses and premature opening of the larynx during the latter stages of swallow.[6] The habitual and sometimes necessary mouth-breathing characteristics of COPD patients may lead to excessive dryness and adherence of thick and dry materials to the oropharyngeal tissues, with potential postswallow aspiration.
The present study also evidenced prolonged apnea duration in individuals with COPD suggesting the compensatory mechanism for impaired respiratory-swallow coordination. Gross et al. revealed that in the COPD group, the duration of swallow apnea of swallows that occurred during the inhalation phase was significantly longer.[5] This prolongation could indicate the presence of a compensatory mechanism such as more time for recoil forces to generate higher swallow subglottic pressure or more time for the bolus to traverse the pharynx and enter the esophagus. Another study done by de Deus Chaves et al. has concluded that patients with COPD presented longer pharyngeal transit time (PTT) during the ingestion of 10 ml of the liquid consistency and during the ingestion of the paste consistency.[7]
Thus, aspiration is a likely complication following COPD. However, none of our participants exhibited cough while swallowing. This is due to the fact that all the individuals with COPD exhibited voluntary protective mechanism during swallowing such as prolonging the closure of airway, i.e., increased swallowing apnea duration as reported by Mokhlesi et al.[8] It is also interesting to note that none of the individuals with COPD exhibited any dysphagic symptoms. It is also possible that dysphagia in COPD patients may be exacerbated during the wheezing episodes. In this current study, the prolonged apnea duration exhibited by individual with COPD patients is considered to be compensatory mechanism for respiratory swallowing incoordination. This compensation need not to be considered as an impaired swallow and hence does not require any intervention. However, COPD individuals failing to exhibit such compensation require further detailed investigation and may be intervention too. Furthermore, bolus consistency showed a significant difference between the groups indicating that thicker liquids required longer swallow apnea duration than the thin liquids. This is because thin liquids flow at a faster rate, requiring reduced time for apnea duration than thick liquids which flow at a slower rate. However, bolus volume did not have any effect on respiratory-swallowing coordination in both the groups.
In nutshell, respiratory-swallowing incoordinations are observed during nasal airflow monitoring during swallowing in individuals with COPD. These deficits should further be correlated with videofluoroscopic evaluations to ascertain the nature of these deficits in a more objective way.
CONCLUSION
Findings suggest the presence of subtle dysphagic component in individuals with COPD and will assist the speech pathologist during the assessment of respiratory-swallow coordination in individuals with COPD. The present findings do suggest the need for dysphagia management in individuals with COPD which should be investigated in future studies. The findings also emphasize the need for tailor made management approaches for these COPD individuals depending on the nature of respiratory-swallowing incoordinations. Furthermore, our data should throw light on the efficacy of management approaches in these COPD individuals with respiratory-swallowing incoordination.
Financial support and sponsorship
Manipal Foundation, Manipal Universy.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.GOLD – The Global Initiative for Chronic Obstructive Lung Disease. 2016. [Last cited on 2016 Feb 19]. Available from: http://www.goldcopd.org/guidelines-global-strategy-for-diagnosis-management .
- 2.Dozier TS, Brodsky MB, Michel Y, Walters BC, Jr, Martin-Harris B. Coordination of swallowing and respiration in normal sequential cup swallows. Laryngoscope. 2006;116:1489–93. doi: 10.1097/01.mlg.0000227724.61801.b4. [DOI] [PubMed] [Google Scholar]
- 3.Cvejic L, Harding R, Churchward T, Turton A, Finlay P, Massey D, et al. Laryngeal penetration and aspiration in individuals with stable COPD. Respirology. 2011;16:269–75. doi: 10.1111/j.1440-1843.2010.01875.x. [DOI] [PubMed] [Google Scholar]
- 4.O'Kane L, Groher M. Oropharyngeal dysphagia in patients with chronic obstructive pulmonary disease: A systematic review. Rev CEFAC. 2009;11:449–506. [Google Scholar]
- 5.Gross RD, Atwood CW, Jr, Ross SB, Olszewski JW, Eichhorn KA. The coordination of breathing and swallowing in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2009;179:559–65. doi: 10.1164/rccm.200807-1139OC. [DOI] [PubMed] [Google Scholar]
- 6.Martin-Harris B. Optimal patterns of care in patients with chronic obstructive pulmonary disease. Semin Speech Lang. 2000;21:311–21. doi: 10.1055/s-2000-8384. [DOI] [PubMed] [Google Scholar]
- 7.de Deus Chaves R, Chiarion Sassi F, Davison Mangilli L, Jayanthi SK, Cukier A, Zilberstein B, et al. Swallowing transit times and valleculae residue in stable chronic obstructive pulmonary disease. BMC Pulm Med. 2014;14:62. doi: 10.1186/1471-2466-14-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mokhlesi B, Logemann JA, Rademaker AW, Stangl CA, Corbridge TC. Oropharyngeal deglutition in stable COPD. Chest. 2002;121:361–9. doi: 10.1378/chest.121.2.361. [DOI] [PubMed] [Google Scholar]


