Abstract
Erectile dysfunction (ED) is considered a condition with a broad range of etiologies. Obstructive sleep apnea (OSA) syndrome is one of the lesser studied risk factors for ED. We intend to summarize the current evidence on the relationship between OSA and sexual impairment, focusing on the results in terms of erectile function of the different therapies offered to OSA patients. A systematic review was conducted, selecting articles related to the physiology of OSA and ED, and to the treatments of OSA syndrome and their reported outcomes in erectile and sexual function. Higher prevalences of ED in the OSA groups have been published. However, whether this effect on the erectile function occurs in the entire range of OSA severities remains unclear. Several hypotheses were proposed to explain the physiology of this association. Continuous Positive Airway Pressure as a treatment for OSA patients with ED has achieved a significative improvement in the sexual parameters in most of the studies. Phosphodiesterase type 5 inhibitors (iPDE5) on demand are useful as a treatment for ED in this subgroup of patients, with high satisfaction rates. The surgical treatment for the OSA evidenced benefits over the erectile function, and the effect on the sexual satisfaction of the therapy using Mandibular Advancement Devices is still undefined.
Keywords: continuous positive airway pressure, erectile dysfunction, obstructive sleep apnea, operative surgical procedures, phosphodiesterase type 5 inhibitors
INTRODUCTION
Erectile dysfunction (ED) is considered a condition with a broad range of etiologies. Obstructive sleep apnea (OSA) syndrome, defined as a repetitive partial or complete collapse of the upper airway during sleep, is one of the lesser studied risk factors for ED. As identification and treatment of the causing factors of ED is recommended when feasible, knowledge of the outcomes regarding the sexual function in OSA patients is important for the urologist. A limited number of therapies have been used for OSA treatment, and the outcomes over the erectile and the sexual function of these therapies have been reported with different methodological approaches and using several measuring tools.
With the hypothesis of a benefit in terms of erectile function in the patients with OSA and ED treated for their ventilatory condition, we intend to identify and summarize the current published evidence in the relationship between OSA and sexual impairment in the male population and the results regarding erectile and sexual function of the different therapies offered to OSA patients.
MATERIALS AND METHODS
A systematic review was conducted and reported following the meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines.1 A search in the PubMed database was conducted and performed simultaneously by one urologist and one sleep medicine specialist, with the same specified strategy. The index terms used were “sleep apnea,” “obstructive sleep apnea,” “obstructive sleep apnea syndrome,” “erectile dysfunction,” “sexual function,” and “continuous positive airway pressure.” We included in our search all the studies published before 2015, including the earliest reports available in the database, either in urological journals or respiratory and sleep medicine ones. Papers published in languages other than English were excluded. All types of studies in our initial search were included. Reviewing the abstracts, papers related to the physiology of OSA and ED, and to the treatments of OSA syndrome and their reported outcomes in erectile and sexual function were selected. Bibliographies of the retrieved papers were also searched for any published papers not showed in the original PubMed search. For each selected report, a duplicated data extraction was performed by one urologist and one sleep medicine specialist, and the data were collected using a template.
Regarding the outcomes in the sexual and erectile function with the different OSA treatments, we described the design of the study, the patients and methods, and the results regarding the sexual function, and also the ventilatory outcomes when available. The main outcome measures of every individual study were identified and possible limitations or bias were addressed. When a conflict appeared between both reviewers regarding the information in one report, a third specialist was asked to clarify this question. We created tables to visually expose and compare the heterogeneity of the designs and outcomes available for each OSA treatment group.
RESULTS
Study selection
After a PubMed search, using a combination of the selected keywords, 176 articles were identified. From the original collection of abstracts, we excluded 110 for different reasons (i.e., focused on female population, original in other languages than English, general overviews of only one of the conditions or clearly not related with the topic of the search). The remaining 66 articles were selected and analyzed (Figure 1).
Figure 1.
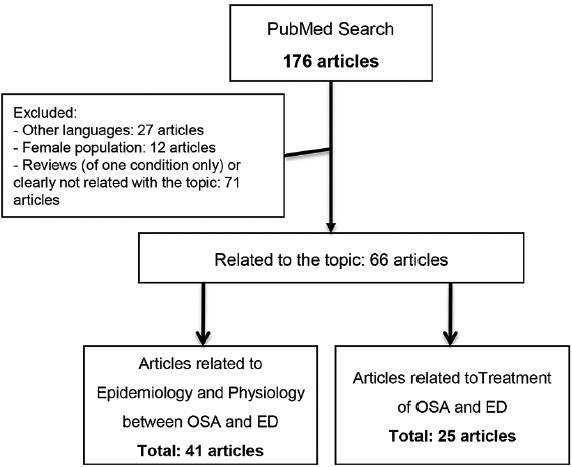
Selection of articles.
In our systematic review, we included the papers related with the epidemiology and the physiological hypothesis of the relationship between OSA and ED, and those related with the consequences on the erectile and sexual function of the treatments for OSA.
Evidence synthesis
Importance of ED
The prevalence of ED varies in different studies depending on age and the diagnostic tool used. In males aged 40–70 years old, according to Massachusets Male Aging Study (MMAS), ED is severe in 5.1%–15%, moderate in 17%–34% and mild in 17% of those studies.2 In worldwide studies ED varies between 2%–9% and 20%–30% in the 40–59 years old group, 20%–40% in the 60–69 years old group and 50%–75% in the 70–80 years old group.3 Currently, ED is considered a mixed condition, with both functional and organic causes2 and with a broad range of identified risk factors.2,3,4 One of the main risk factors, with direct consequences on respiratory system, is smoking, showing direct dose-response association with ED and statistically significant differences (adjusted odds ratio = 1.68; 95% CI: 1.03–2.30) in exposures ≥20 packs per year.5 Another related factor is the hormonal status, such as hypogonadism or androgen deficiency, which has a prevalence of 5.6% in males between 30 and 79 years old. Of these, 16% will develop ED.6 When managing ED, it is essential to address the cause of the dysfunction, as well as the psycho-social impact on the patient and his partner, using a therapeutic approach.7 At the same time, we should try to rule out etiologies of ED,8,9 focusing on comorbidities and possible modifiable causes.8 Many tools have been developed to aid the clinical interview with the patient and their partner, to assess the presentation, severity and the response to any treatment given.8,9 In most cases, these diagnostic tools are self-administered questionnaires, of which, the most widely used are the International Index of Erectile Function (IIEF),10 and the Male Sexual Health Questionnaire (MSHQ).11
Prevalence of OSA and relationship with ED
Obstructive Sleep Apnea (OSA) syndrome was reported for first time in 1966,12 and it was defined by the American Association of Sleep Medicine (AASM) as a repetitive partial or complete collapse of the upper airway during sleep that results in disruptions of normal sleep architecture and arterial blood desaturations.13 OSA is estimated to affect at least 2%–4% of the adult population, with a consistent 2-fold risk for males compared to females.14 Furthermore, approximately one in four adults is at risk of experience excessive somnolence or other OSA-related symptoms.15,16 OSA is associated with a number of comorbidities, namely: systemic hypertension, coronary artery disease, stroke, congestive heart failure, atrial fibrillation, increased motor vehicle accident rate, sleepiness, impaired quality of life, increased mortality and erectile dysfunction, and others.17
A relationship between sleep disturbances and ED was first noticed in 1977 by Guilleminault et al.18 and further detailed by Schmidt and Wise in 1981.19 Since then, higher prevalences of ED in the OSA groups have been published in numerous studies,20,21,22,23,24,25 depending on the diagnostic tool used. The prevalence of ED is as high as 69%,26,27,28 with poorer sexual function in OSA patients compared with control patients matched for comorbidities and age.23,25,29,30,31 This growing evidence leads to the recommendation in some papers of asking the patients about sleep disturbances,25,32,33,34 or even snoring35 during ED assessment. In a survey study, snoring was associated with complaints of ED and with an organic ED diagnosis,36 while OSA has been clearly named as an independent risk factor for ED,37 with positive correlation between both entities.38 In OSA patients, the lower O2 saturation was a significant predictor (P = 0.01) of the presence of ED.34 Despite this data, it remains unclear if this effect on the erectile function occurs in the entire range of OSA severities or only in the moderate and severe OSA patients.21,23,25,28,30,34
Physiological hypothesis of the relationship between OSA and ED
The physiological basis of the association between OSA and ED is still a controversial subject since the first papers describing the possible hypothesis in 1984.39 This relationship is deeper than the simple impairment of sexual function due to depressed mood, daytime somnolence, and sleepiness caused by OSA.40 Studies of OSA and ED patients treated with antidepressant therapy showed no improvement on erectile function despite their depression scale results being restored.38
One theory focuses on the sleep fragmentation related to OSA and a lack in Rapid Eye Movement (REM) periods during rest time. During REM sleep time, physiological erections appear to help maintain erectile function through cavernosal tissue oxygenation.27,30 Another theory states that the ED is related to changes in the hormonal axis caused by sleep pattern changes associated with OSA.41 These hormonal changes have been correlated with a lack of libido and sexual desire.42 Impairment of the hypotalamus-pituitary-gonadal regulatory system leads to a decrease in the release of testosterone,42,43 with low testosterone levels being related to the degree of hypoxemia while sleeping.43 This suppression of testosterone and sex hormone-binding globulin (SHBG) in OSA patients is independent of age and obesity,43 and is reversed after 3 months of nasal Continuous Positive Airways Pressure (CPAP) therapy44 or after surgical treatment.43 Testosterone replacement therapy in patients with untreated OSA is contraindicated based on current evidence.45,46
Norepinephrine release may also have an effect over erectile functions in OSA patients, as levels are increased during the sympathetic predominant state that follows every apneic episode.47
A transient hypoxic environment, as in OSA, can also affect changes to erectile function in itself, evidenced by a significant (P = 0.05) decrease in nocturnal tumescence registers in healthy subjects who underwent hypoxia for a short period of time.48 Likewise, in other studies, it has been proven that hypoxia leads to neural changes,49 with evidence of significant (P = 0.007) impairment in pudendal nerve transmission and bulbocavernosus reflex, another possible explanation for loss of erectile function in OSA patients.50
A differing hypothesis focuses on a common presentation of ED within a proinflammatory state caused by OSA.51,52 This state can lead to ED by itself or through other coexisting pathologies.31,53 There is growing evidence on the development of ED with a vascular etiology in an environment with an excess of free-radicals54 and, in some studies conducted on OSA patients, an impairment of endothelial related vasodilatation mechanisms was seen.55 Likewise, using animal models, low levels of nitric oxide synthase, produced by the endothelium as part of the pathway for vasodilatation, are measured in a hypoxic environment,56 while other proinflammatory markers are increased, leading to low levels of nitric oxide.57,58 In a more practical approach, these decreased levels of nitric oxide and its derivatives in plasma samples were found to be increased by short- (1 or 2 nights) and long-term (1.5 months) CPAP therapy.58,59
Treatments for OSA and impact of erectile function
Introduction
OSA is a chronic disease that requires long-term multidisciplinary management. According to the clinical guidelines of the AASM, pneumatic splinting of the upper airway by CPAP is the treatment of choice for mild, moderate and severe OSA and should be offered as an option to all patients. Alternative therapies, such as mandibular advancement devices (MADs) and surgical treatments (uvulopalatopharyngoplasty, maxillomandibular advancement) may be offered depending on the severity of the OSA as well as the patient's anatomy, risk factors, and preferences.60 Success rates, which vary between individuals and treatment options, can be measured in terms of several polysomnographic features, symptoms, comorbidities, and quality of life. The vast array of outcome measures, together with the variability in individual's response to treatment, makes adequate interstudy comparisons difficult.
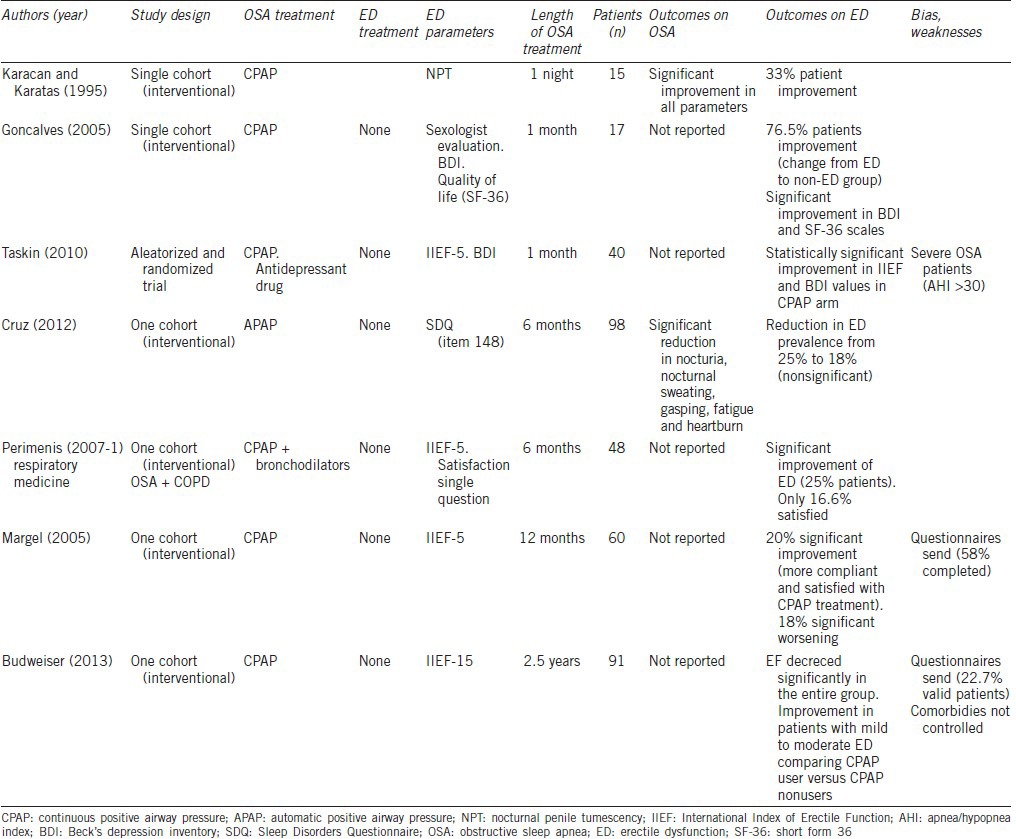
Continuous positive airway pressure (CPAP) (Table 1)
Table 1.
Outcomes of treatment with CPAP
CPAP is the most widespread and consolidated treatment for OSA patients, achieving a significative improvement in respiratory and neurological parameters evaluated by polysomnographic studies.61,62
The first report of improvement of erectile function in OSA patients treated with CPAP was published by Karacan and Karatas in 1995.63 This study was conducted on a cohort of patients diagnosed with OSA and sexual dysfunction, performing a polysomnographic test and a nocturnal penile tumescence (NPT) register in a basal state and after one night using CPAP devices. Previous reports evidenced alterations in NPT due to sleep disorders.33 This first study after CPAP treatment clearly showed an improvement on the ED parameters in one-third of patients.63 Despite the short time of CPAP treatment between tests and the absence of clinical assessment of satisfaction following NPT changes, this early report offers a first approach to the association between OSA and ED. It suggests that the severity of OSA and the patient's age are relevant factors which influence the improvement on rigidity with CPAP therapy.63
Since then, several studies have been conducted analyzing the changes in erectile function after different lengths of CPAP therapy, and in some cases adding other ED treatments as phosphodiesterase type 5 inhibitors (iPDE5)22,64,65,66 or testosterone67 to the positive airway pressure therapy.
Taskin et al.38 in a recently published randomized study, evidenced a statistically significant (P < 0.001) improvement in ED, using the validated IIEF questionnaire, after at least 1 month of CPAP treatment in a cohort of patients diagnosed with severe OSA. They compared CPAP therapy with an antidepressant drug (selective serotonin reuptake inhibitor) that only showed significantly (P = 0.001) benefit in Beck's depression inventory but not in IIEF-5.38
Goncalves et al. in a cohort of OSA patients assessed for ED by a sexologist interview, found an improvement in the sexual function status following 1 month of CPAP therapy in more than 75% of patients.34 This study also evidenced benefits in the quality of life of patients with OSA and ED treated with CPAP, with improvements valued as more important in this group than in the group of OSA patients without ED treated equally with CPAP. This study demonstrates that erectile alteration has a significant (P = 0.02) additional impairment on quality of life in OSA patients.34
In a recently published paper, Cruz et al. assessed the results of a cohort of moderate to severe OSA patients treated using nasal automatic positive airway pressure (APAP) for at least 6 months.68 Several parameters, including the presence of ED, were analyzed with the Sleep Disorders Questionnaire (SDQ). The prevalence of ED before therapy was 25%, and was reduced to 18%, without achieving statistical significance.68 One of the most important outcomes of this study is a lower ED prevalence when compared with that previous published, probably related with the lack of a targeted questionnaire for ED, and the absence of any adjustments regarding the severity of ED or OSA, leading to poor treatment outcomes.68
Perimenis et al. studied a group of patients diagnosed with Overlap Syndrome (Chronic obstructive pulmonary disease + OSA) and with concurrent ED, treated for 6 months with CPAP and bronchodilators, finding significant (P < 0.001) improvement in the individual results, that were measured with a validated tool (IIEF-5).69 They found that this improvement in the erectile function was related positively with age and the Apnea-Hypopnea Index (AHI), and negatively with ED duration. When patients were simply asked if they were satisfied with the effect of the respiratory over their sexual function, only 17% were satisfied. However this assessment was not made using a validated questionnaire.69
Margel et al.70 assessed the change in IIEF results on patients with OSA treated with at least 1 year of CPAP therapy. They found an improvement on sexual function in 20% of patients, correlated with adherence and satisfaction with CPAP treatment and with lower levels of baseline oxygen saturation. In this study, 18% presented worsening in the IIEF results, being less compliant and satisfied with the CPAP than the patients with improvement or unchanged erectile function. In this study, the low response rate of only 58% of patients who received the questionnaire could be a potential limitation for the results.
The beneficial effect of OSA treatment using CPAP therapy over erectile function seems to be maintained in the long-term, according to the results published by Budweiser et al.71 In their study, with an average follow-up above 3 years, the changes over the baseline erectile function, measured within IIEF subscales, showed a significant (P = 0.005) decrease in the entire group. However, in mild to moderate ED patients with good CPAP compliance, the erectile function improved over time, with significant differences (P = 0.014) compared with CPAP nonusers. In the multivariate regression model, only the age and the severity of OSA at diagnosis were predictive for EF impairment, with the regular use of CPAP failing to get statistical significance.71 Despite these interesting results, the conclusions of Budweiser's study should be carefully assessed, due to the limitations of a mail conducted survey with a low response rate (28%) and the lack of adjustment for body weight, medications or comorbidities.
Continuous positive airway pressure and iPDE5 (Table 2)
Table 2.
Outcomes of treatment with CPAP and iPDE5
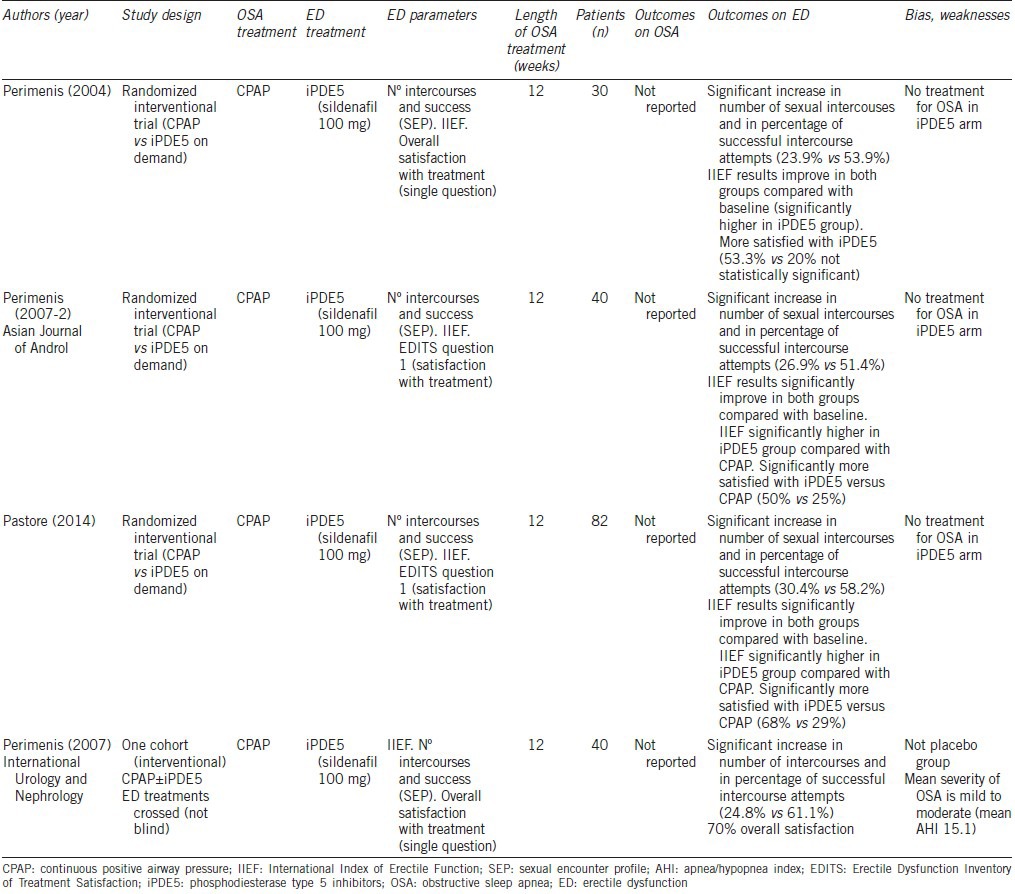
Looking for other therapeutic approaches for these patients, Perimenis et al. designed a trial based on the need for a combined therapy for both entities. They published a new study comparing CPAP treatment with CPAP and sildenafil 100 mg on demand for intercourse in a group of patients with mild to moderate OSA.22 Analyzing IIEF results, the number of intercourses and percentage of successful intercourses, they found 61.1% of success in the CPAP + Sildenafil arm, significantly (P < 0.001) higher than the 24.7% obtained in the CPAP only group. The overall satisfaction with the combined treatment, being assessed without a validated questionnaire, was 70% which was higher than that achieved with CPAP only.22
The same group attempted to clarify the importance of each part of this therapeutical approach and conducted two randomized trials comparing CPAP therapy versus Sildenafil 100 mg on demand in an OSA cohort of patients. After 3 months of treatment, they found an improvement when comparing with baseline characteristics in both groups. However, a significant (P < 0.001) increase in the number of sexual intercourses, the percentage of successful intercourse attempts and in IIEF results were achieved in the iPDE5 arm,64,65 being the benefit in the CPAP group statistically (P = 0.002) but probably not clinically significant. Overall satisfaction with the treatment was low with both therapies in the two trials, 20% CPAP versus 53.3% Sildenafil in the early one65 and 25% CPAP versus 50% Sildenafil in the second one,64 but was clearly higher in the group treated with iPDE5. In this latter study, a validated questionnaire (EDITS),72 was completed by the patients and also by their partners, showing a similar satisfaction rate (20% CPAP vs 50% Sildenafil), leading to the need for different therapeutic approaches.64
Using the data of those randomized controlled trials, Li et al. performed a meta-analysis, reaching the same conclusions, evidencing statistically significant differences toward the sildenafil group in terms of percentage of successful intercourse attempts (P < 0.0001), erectile function scores (P < 0.001) and satisfaction of the patient with the therapy for ED (P = 0.02).66
More recently, a new randomized study compared both treatments, focusing on patients with severe OSA. Using the same measuring tests, Pastore et al. found significant (P < 0.0001) improvement over baseline in IIEF-5 in CPAP and sildenafil 100 mg on demand. However when comparing the two arms, sildenafil group proved to be more effective in terms of successful attempts, IIEF-5 and EDITS results, reaching a satisfaction rate of 68%.73
Despite the good study design and the careful selection of patients, with very restrictive exclusion criteria, these studies showed a lack of description of the outcomes from the respiratory point of view. Since the ED appears to be associated with the OSA syndrome, the treatment only of the erectile problem means that the ventilatory dysfunction remains untreated, thus risking a worsening of the ED, and developing other comorbidities.
iPDE5 drugs in OSA patients
Despite the good results in Perimenis et al. trials, the treatment of OSA patients with ED using only iPDE5 is controversial due to the evidence of worsening the ventilatory events in cases diagnosed with severe OSA.64 Roizenblatt et al. in a double-blind, placebo-controlled, crossover study comparing Sildenafil 50 mg with placebo showed an increase in the AHI, and a worsening in oxygen saturation in those patients treated with iPDE5, without reporting the results in the sexual and erectile function.74 Neves et al. from the same group, evidenced not only a worsening in OSA respiratory data but also immediate cardiac effects due to autonomic system impairment in Sildenafil-treated patients with severe OSA.75 Since these two studies included only 13 severe untreated OSA patients, the external validation of the conclusions is compromised. As the authors suggested, it is premature to extrapolate these findings to all individuals before properly designed randomized, controlled trials on the effects of sildenafil and other iPDE5 on pulmonary gas exchange and hemodynamics are performed in patients with different severity of sleep-related breathing disorders.74
Continuous positive airway pressure and surgical treatment (Table 3)
Table 3.
Outcomes of treatment with CPAP and surgical correction and MAD
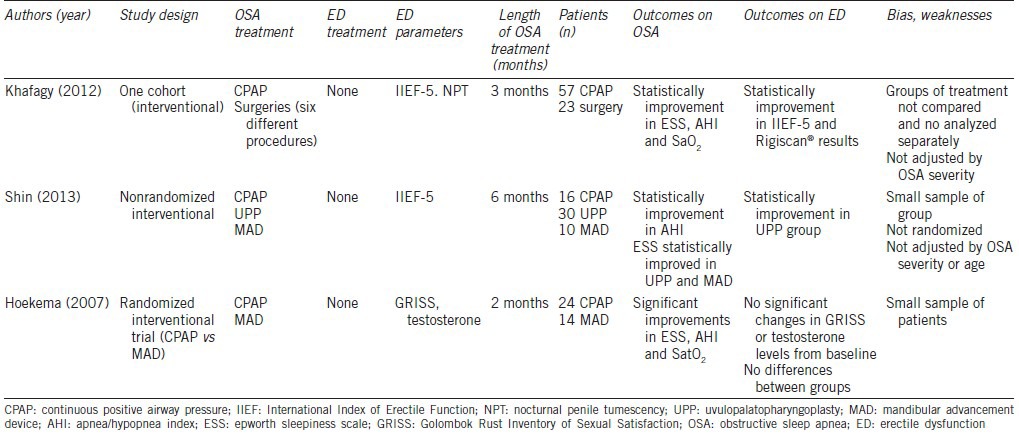
A recent study from Khafagy and Khafagy confirmed once more the benefits of OSA treatment over the erectile function. In this case, the benefit arises not only from medical therapy but also from surgical treatment in those patients with poor compliance with positive pressure treatments.20 They performed a trial, analyzing IIEF-5 results and nocturnal penile tumescence registered before and after 3 months of treatment in an heterogeneous cohort of OSA diagnosed patients treated with CPAP and an uvulopalatopharyngoplasty (UPP) plus adjunctive nasal surgeries. They found a statistically significant improvement in respiratory parameters (P < 0.001) and in both erectile function tests (P < 0.05).20 Unfortunately, a comparison between the two treatment arms was not performed, so the relative value of each kind of treatment remains uncertain.20
Surgical correction of OSA
Regarding the only surgical management of OSA and the implications over ED, it was first suggested by Guilleminault et al. in 1981 with a cohort of 49 male OSA patients treated with tracheostomy, a desperate, seldom-used surgical intervention that bypasses the upper airway granting an unobstructed inspiratory effort and a 100% cure rate. In this early report, 44% of patients reported initial difficulty with erections and ejaculation, with subsequent disappearance of symptoms after surgery in all of the patients except one, after a median follow-up of 31 months.76 Despite the lack of erectile function assessment validated tools, clinical interviews were performed with the patients pre- and post-treatment focused on several outcomes including sexual function, and the reported results were confirmed with interviews with their spouses.
In 1988, Santamaria et al. conducted a trial in 12 patients treated with UPP for OSA.43 They measured serum testosterone in OSA patients and snorers, finding statistically significant (P < 0.05) lower levels in the first group. Three months after UPP, a complete normalization of testosterone levels was reported, and a normal libido and sexual function was described in all the patients, with the resolution of erectile problems in all seven patients with previous impairment.43
Mandibular advancement devices (Table 3)
Recently, Shin et al. developed a comparative study between OSA surgical treatment with UPP and medical therapies, including CPAP and mandibular advancement devices (MADs).77 They reported a significant improvement in the erectile function of the UPP group (P = 0.039), but not in CPAP or MAD groups. The three treatment arms evidenced benefit regarding the quality of life tests outcomes, but only reached statistical significance (P = 0.040) in the MAD treated group. This paper presents important limitations, such a small sample of patients in each group (MAD: 10; CPAP: 16; UPP: 30), and bias due to the lack of randomization, which led to a different profile of severity of OSA and ED in each group with the conclusion of the relationship between the severity of ED and a better response to the treatment77 being controversial.
In another randomized controlled trial Hoekema et al. in 2007, analyzed the sexual function outcomes comparing OSA patients treated with CPAP or MAD.29 After 8 weeks of treatment, no statistically significant changes on sexual function results or on testosterone levels from baseline were observed in the two groups, but a significant correlation (r = −0.547; P < 0.001) was demonstrated between the severity of ED at baseline and the improvement after OSA treatment. Despite an adequate study design, several limitations arose, as they used a questionnaire uncommon in clinical practice (GRISS: Golombok Rust Inventory of Sexual Satisfaction), and there were a small number of patients with complete follow-up (MAP: 14; CPAP: 24) which could affect the conclusions of this trial.29
DISCUSSION
The relationship between OSA and ED was described more than 35 years ago and since then, this topic was approached in different investigations. Considering the multifactorial etiology of ED, and the variety of the diagnostic tools available, it is understandable of the wide range of prevalence of ED described in OSA population. Higher prevalences of ED in the OSA groups have been published, when compared control patients, matched for age and comorbidities. If this effect over the erectile function occurs in the entire range of OSA severities or only in severe cases remains controversial. Obesity, smoking, and androgen deficiency are conditions directly related with ED etiology that may act as confounding factors in OSA patients.
Regarding the bases linking both conditions, several hypothesis has been proposed to explain the physiology of this association. The first and more obvious one was related with the mood and the sleepiness caused by OSA. There are also clear evidences supporting the theory of hormonal changes related with the impaired sleep pattern and the hypoxic environment during apneic episodes. Recent studies suggest that ED in this context is caused by endothelial dysfunction, as part of a systemic proinflammatory state caused by OSA, and leading to decreased levels of nitric oxide.
CPAP is the treatment of choice for OSA patients. The effects over erectile and sexual function showed benefits after only one night of treatment and maintained in the long-term. These studies, based on cohorts of patients treated with CPAP therapy, evidenced an improvement on erectile function in around 30% of patients, with a broad range between 6% and 76%. As predictors for ED improvement, the patient's age, the severity of the OSA and the adherence to CPAP treatment were suggested, but not consistent in all the studies.
The best level of evidence in the relationship between OSA treatment and ED is comparing the CPAP and the iPDE5 (sildenafil), with one meta-analysis published in this topic and four well-designed randomized clinical trials. Sildenafil 100 mg on demand proved important improvement in erectile function tests (around 50%) compared with CPAP, also achieving better satisfaction results. In these trials CPAP alone also improved the erectile function around 20%. When both therapies were offered together, the higher overall satisfaction was achieved (70%). The combined approach with CPAP and Sildenafil ensures an adequate treatment for OSA, as there is some evidence regarding worsening in respiratory data and cardiac effects in severe OSA patients treated with iPDE5 only.
The published studies about erectile function outcomes after surgical treatment of OSA are very heterogeneous. The first reports showed promising outcomes with tracheostomy, a treatment currently seldom used. The UPP also showed benefit, but the measure of the outcomes in the papers was controversial, and the number of the patients included in the studies was small.
MAD is the less studied OSA treatment regarding the effects over the erectile function, but in a well-designed randomized trial, it failed to prove benefits.28
As limitations of our study, we performed a descriptive analysis of the published evidence, without any statistical comparison between groups of treatments or between individual studies. Heterogeneity between selected articles was found, with consequent differences in the level of evidence provided. We only selected reports published in English, but we will broaden our search including reports published in urological and also respiratory and sleep medicine journals in the future.
CONCLUSIONS
There is growing evidence of the risk of ED in OSA patients. Despite the lack of knowledge of the mechanisms of the sexual problems in these patients, there is a proven relationship between the severity of both entities. It seems to be reasonable to recommend asking about the sleep disorders during the erectile dysfunction clinical interview, due to the fact that the treatments of sleep disordered breathing will improve the sexual results, in particular, CPAP therapy. The iPDE5 on demand seems to be a good treatment for the ED in this cohort of patients, with the best outcomes and satisfaction rates when associated with CPAP therapy.
AUTHOR CONTRIBUTIONS
FCJ conceived the study, participated in the design, performed the database search and the review of selected articles, and drafted the manuscript. MFB participated in the study design, performed the database search and the review of selected papers, and helped to draft the manuscript. MG helped to draft the manuscript. JAPM helped to draft the manuscript. All authors read and approved the final manuscript.
COMPETING INTERESTS
All authors declare no competing financial interests.
REFERENCES
- 1.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283:2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 2.Lue TF. Physiology of penile erection and pathophysiology of erectile dysfunction. In: Wein AJ, Novick AC, Partin AW, Peter CA, editors. Campbell-Walsh Urology. 10th ed. Philadelphia: Saunders; 2011. pp. 688–720. [Google Scholar]
- 3.Francis ME, Kusek JW, Nyberg LM, Eggers PW. The contribution of common medical conditions and drug exposures to erectile dysfunction in adult males. J Urol. 2007;178:591–6. doi: 10.1016/j.juro.2007.03.127. [DOI] [PubMed] [Google Scholar]
- 4.Selvin E, Burnett AL, Platz EA. Prevalence and risk factors for erectile dysfunction in the US. Am J Med. 2007;120:151–7. doi: 10.1016/j.amjmed.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 5.Kupelian V, Link CL, McKinlay JB. Association between smoking, passive smoking, and erectile dysfunction: results from the Boston Area Community Health (BACH) Survey. Eur Urol. 2007;52:416–22. doi: 10.1016/j.eururo.2007.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Araujo AB, Esche GR, Kupelian V, O’Donnell AB, Travison TG, et al. Prevalence of symptomatic androgen deficiency in men. J Clin Endocrinol Metab. 2007;92:4241–7. doi: 10.1210/jc.2007-1245. [DOI] [PubMed] [Google Scholar]
- 7.Hatzichristou D, Rosen RC, Derogatis LR, Low WY, Meuleman EJ, et al. Recommendations for the clinical evaluation of men and women with sexual dysfunction. J Sex Med. 2010;7:337–48. doi: 10.1111/j.1743-6109.2009.01619.x. [DOI] [PubMed] [Google Scholar]
- 8.Wespes E, Eardley I, Giuliano F, Hatzichristou D, Hatzimouratidis J, et al. EAU Guidelines on Male Sexual Dysfunction: Erectile Dysfunction and Premature Ejaculation. 2013 doi: 10.1016/j.eururo.2010.02.020. [DOI] [PubMed] [Google Scholar]
- 9.Burnett AL. Evaluation and management of erectile dysfuntion. In: Wein AJ, Novick AC, Partin AW, Peter CA, editors. Campbell-Walsh Urology. 10th ed. Philadelphia: Saunders; 2011. pp. 721–48. [Google Scholar]
- 10.Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, et al. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–30. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 11.Rosen RC, Catania J, Pollack L, Althof S, O’Leary M, et al. Male sexual health questionnaire (MSHQ): scale development and psychometric validation. Urology. 2004;64:777–82. doi: 10.1016/j.urology.2004.04.056. [DOI] [PubMed] [Google Scholar]
- 12.Gastaut H, Tassinari CA, Duron B. Polygraphic study of the episodic diurnal and nocturnal (hypnic and respiratory) manifestations of the Pickwick syndrome. Brain Res. 1966;1:167–86. doi: 10.1016/0006-8993(66)90117-x. [DOI] [PubMed] [Google Scholar]
- 13.American Academy of Sleep Medicine. The International Classification of Sleep Disorders Revised Diagnostic and Coding Manual: Obstructive Sleep Apnea Syndrome. Westchester, IL: American Academy of Sleep Medicine; 2001. [Google Scholar]
- 14.Young T, Palta M, Dempsey J, Skatrud J, Weber S, et al. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–5. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 15.Hiestand DM, Britz P, Goldman M, Phillips B. Prevalence of symptoms and risk of sleep apnea in the US population: results from the national sleep foundation sleep in America 2005 poll. Chest. 2006;130:780–6. doi: 10.1378/chest.130.3.780. [DOI] [PubMed] [Google Scholar]
- 16.Duran J, Esnaola S, Rubio R, Iztueta A. Obstructive sleep apnea-hypopnea and related clinical features in a population-based sample of subjects aged 30 to 70 yr. Am J Respir Crit Care Med. 2001;163:685–9. doi: 10.1164/ajrccm.163.3.2005065. [DOI] [PubMed] [Google Scholar]
- 17.Kushida CA, Morgenthaler TI, Littner MR, Alessi CA, Bailey D, et al. Practice parameters for the treatment of snoring and obstructive sleep apnea with oral appliances: an update for 2005. Sleep. 2006;29:240–3. doi: 10.1093/sleep/29.2.240. [DOI] [PubMed] [Google Scholar]
- 18.Guilleminault C, Eldridge FL, Tilkian A, Simmons FB, Dement WC. Sleep apnea syndrome due to upper airway obstruction: a review of 25 cases. Arch Intern Med. 1977;137:296–300. [PubMed] [Google Scholar]
- 19.Schmidt HS, Wise HA., 2nd Significance of impaired penile tumescence and associated polysomnographic abnormalities in the impotent patient. J Urol. 1981;126:348–52. doi: 10.1016/s0022-5347(17)54520-6. [DOI] [PubMed] [Google Scholar]
- 20.Khafagy AH, Khafagy AH. Treatment of obstructive sleep apnoea as a therapeutic modality for associated erectile dysfunction. Int J Clin Pract. 2012;66:1204–8. doi: 10.1111/j.1742-1241.2012.02990.x. [DOI] [PubMed] [Google Scholar]
- 21.Margel D, Cohen M, Livne PM, Pillar G. Severe, but not mild, obstructive sleep apnea syndrome is associated with erectile dysfunction. Urology. 2004;63:545–9. doi: 10.1016/j.urology.2003.10.016. [DOI] [PubMed] [Google Scholar]
- 22.Perimenis P, Konstantinopoulos A, Karkoulias K, Markou S, Perimeni P, et al. Sildenafil combined with continuous positive airway pressure for treatment of erectile dysfunction in men with obstructive sleep apnea. Int Urol Nephrol. 2007;39:547–52. doi: 10.1007/s11255-006-9079-4. [DOI] [PubMed] [Google Scholar]
- 23.Shin HW, Rha YC, Han DH, Chung S, Yoon IY, et al. Erectile dysfunction and disease-specific quality of life in patients with obstructive sleep apnea. Int J Impot Res. 2008;20:549–53. doi: 10.1038/ijir.2008.39. [DOI] [PubMed] [Google Scholar]
- 24.Stannek T, Hurny C, Schoch OD, Bucher T, Munzer T. Factors affecting self-reported sexuality in men with obstructive sleep apnea syndrome. J Sex Med. 2009;6:3415–24. doi: 10.1111/j.1743-6109.2009.01486.x. [DOI] [PubMed] [Google Scholar]
- 25.Heruti R, Shochat T, Tekes-Manova D, Ashkenazi I, Justo D. Association between erectile dysfunction and sleep disorders measured by self-assessment questionnaires in adult men. J Sex Med. 2005;2:543–50. doi: 10.1111/j.1743-6109.2005.00072.x. [DOI] [PubMed] [Google Scholar]
- 26.Santos T, Drummond M, Botelho F. Erectile dysfunction in obstructive sleep apnea syndrome-prevalence and determinants. Rev Port Pneumol. 2012;18:64–71. doi: 10.1016/j.rppneu.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 27.Andersen ML, Santos-Silva R, Bittencourt LR, Tufik S. Prevalence of erectile dysfunction complaints associated with sleep disturbances in Sao Paulo, Brazil: a population-based survey. Sleep Med. 2010;11:1019–24. doi: 10.1016/j.sleep.2009.08.016. [DOI] [PubMed] [Google Scholar]
- 28.Budweiser S, Enderlein S, Jorres RA, Hitzl AP, Wieland WF, et al. Sleep apnea is an independent correlate of erectile and sexual dysfunction. J Sex Med. 2009;6:3147–57. doi: 10.1111/j.1743-6109.2009.01372.x. [DOI] [PubMed] [Google Scholar]
- 29.Hoekema A, Stel AL, Stegenga B, van der Hoeven JH, Wijkstra PJ, et al. Sexual function and obstructive sleep apnea-hypopnea: a randomized clinical trial evaluating the effects of oral-appliance and continuous positive airway pressure therapy. J Sex Med. 2007;4:1153–62. doi: 10.1111/j.1743-6109.2006.00341.x. [DOI] [PubMed] [Google Scholar]
- 30.Teloken PE, Smith EB, Lodowsky C, Freedom T, Mulhall JP. Defining association between sleep apnea syndrome and erectile dysfunction. Urology. 2006;67:1033–7. doi: 10.1016/j.urology.2005.11.040. [DOI] [PubMed] [Google Scholar]
- 31.Szymanski FM, Filipiak KJ, Hrynkiewicz-Szymanska A, Grabowski M, Dabrowska-Kugacka A, et al. The high risk of obstructive sleep apnea – An independent risk factor of erectile dysfunction in ST-segment elevation myocardial infarction patients. J Sex Med. 2011;8:1434–8. doi: 10.1111/j.1743-6109.2010.02075.x. [DOI] [PubMed] [Google Scholar]
- 32.Jankowski JT, Seftel AD, Strohl KP. Erectile dysfunction and sleep related disorders. J Urol. 2008;179:837–41. doi: 10.1016/j.juro.2007.10.024. [DOI] [PubMed] [Google Scholar]
- 33.Pressman MR, DiPhillipo MA, Kendrick JI, Conroy K, Fry JM. Problems in the interpretation of nocturnal penile tumescence studies: disruption of sleep by occult sleep disorders. J Urol. 1986;136:595–8. doi: 10.1016/s0022-5347(17)44984-6. [DOI] [PubMed] [Google Scholar]
- 34.Goncalves MA, Guilleminault C, Ramos E, Palha A, Paiva T. Erectile dysfunction, obstructive sleep apnea syndrome and nasal CPAP treatment. Sleep Med. 2005;6:333–9. doi: 10.1016/j.sleep.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 35.Hanak V, Jacobson DJ, McGree ME, Sauver JS, Lieber MM, et al. Snoring as a risk factor for sexual dysfunction in community men. J Sex Med. 2008;5:898–908. doi: 10.1111/j.1743-6109.2007.00706.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Seftel AD, Strohl KP, Loye TL, Bayard D, Kress J, et al. Erectile dysfunction and symptoms of sleep disorders. Sleep. 2002;25:643–7. [PubMed] [Google Scholar]
- 37.Martin SA, Atlantis E, Lange K, Taylor AW, O’Loughlin P, et al. Predictors of sexual dysfunction incidence and remission in men. J Sex Med. 2014;11:1136–47. doi: 10.1111/jsm.12483. [DOI] [PubMed] [Google Scholar]
- 38.Taskin U, Yigit O, Acioglu E, Aricigil M, Toktas G, et al. Erectile dysfunction in severe sleep apnea patients and response to CPAP. Int J Impot Res. 2010;22:134–9. doi: 10.1038/ijir.2009.54. [DOI] [PubMed] [Google Scholar]
- 39.Semple PA, Graham A, Malcolm Y, Beastall GH, Watson WS. Hypoxia, depression of testosterone, and impotence in pickwickian syndrome reversed by weight reduction. Br Med J (Clin Res Ed) 1984;289:801–2. doi: 10.1136/bmj.289.6448.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Akashiba T, Kawahara S, Akahoshi T, Omori C, Saito O, et al. Relationship between quality of life and mood or depression in patients with severe obstructive sleep apnea syndrome. Chest. 2002;122:861–5. doi: 10.1378/chest.122.3.861. [DOI] [PubMed] [Google Scholar]
- 41.Luboshitzky R, Aviv A, Hefetz A, Herer P, Shen-Orr Z, et al. Decreased pituitary-gonadal secretion in men with obstructive sleep apnea. J Clin Endocrinol Metab. 2002;87:3394–8. doi: 10.1210/jcem.87.7.8663. [DOI] [PubMed] [Google Scholar]
- 42.Andersen ML, Tufik S. The effects of testosterone on sleep and sleep-disordered breathing in men: its bidirectional interaction with erectile function. Sleep Med Rev. 2008;12:365–79. doi: 10.1016/j.smrv.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 43.Santamaria JD, Prior JC, Fleetham JA. Reversible reproductive dysfunction in men with obstructive sleep apnoea. Clin Endocrinol (Oxf) 1988;28:461–70. doi: 10.1111/j.1365-2265.1988.tb03680.x. [DOI] [PubMed] [Google Scholar]
- 44.Grunstein RR, Handelsman DJ, Lawrence SJ, Blackwell C, Caterson ID, et al. Neuroendocrine dysfunction in sleep apnea: reversal by continuous positive airways pressure therapy. J Clin Endocrinol Metab. 1989;68:352–8. doi: 10.1210/jcem-68-2-352. [DOI] [PubMed] [Google Scholar]
- 45.Hanafy HM. Testosterone therapy and obstructive sleep apnea: is there a real connection? J Sex Med. 2007;4:1241–6. doi: 10.1111/j.1743-6109.2007.00553.x. [DOI] [PubMed] [Google Scholar]
- 46.Wittert G. The relationship between sleep disorders and testosterone in men. Asian J Androl. 2014;16:262–5. doi: 10.4103/1008-682X.122586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ziegler MG, Nelesen R, Mills P, Ancoli-Israel S, Kennedy B, et al. Sleep apnea, norepinephrine-release rate, and daytime hypertension. Sleep. 1997;20:224–31. doi: 10.1093/sleep/20.3.224. [DOI] [PubMed] [Google Scholar]
- 48.Verratti V, Di Giulio C, Berardinelli F, Pellicciotta M, Di Francesco S, et al. The role of hypoxia in erectile dysfunction mechanisms. Int J Impot Res. 2007;19:496–500. doi: 10.1038/sj.ijir.3901560. [DOI] [PubMed] [Google Scholar]
- 49.Mayer P, Dematteis M, Pepin JL, Wuyam B, Veale D, et al. Peripheral neuropathy in sleep apnea. A tissue marker of the severity of nocturnal desaturation. Am J Respir Crit Care Med. 1999;159:213–9. doi: 10.1164/ajrccm.159.1.9709051. [DOI] [PubMed] [Google Scholar]
- 50.Fanfulla F, Malaguti S, Montagna T, Salvini S, Bruschi C, et al. Erectile dysfunction in men with obstructive sleep apnea: an early sign of nerve involvement. Sleep. 2000;23:775–81. [PubMed] [Google Scholar]
- 51.Yamauchi M, Nakano H, Maekawa J, Okamoto Y, Ohnishi Y, et al. Oxidative stress in obstructive sleep apnea. Chest. 2005;127:1674–9. doi: 10.1378/chest.127.5.1674. [DOI] [PubMed] [Google Scholar]
- 52.Hoyos CM, Melehan KL, Phillips CL, Grunstein RR, Liu PY. To ED or not to ED - Is erectile dysfunction in obstructive sleep apnea related to endothelial dysfunction? Sleep Med Rev. 2015;20:5–14. doi: 10.1016/j.smrv.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 53.Szymanski FM, Puchalski B, Filipiak KJ. Obstructive sleep apnea, atrial fibrillation, and erectile dysfunction: are they only coexisting conditions or a new clinical syndrome? The concept of the OSAFED syndrome. Pol Arch Med Wewn. 2013;123:701–7. doi: 10.20452/pamw.2017. [DOI] [PubMed] [Google Scholar]
- 54.Vlachopoulos C, Rokkas K, Ioakeimidis N, Stefanadis C. Inflammation, metabolic syndrome, erectile dysfunction, and coronary artery disease: common links. Eur Urol. 2007;52:1590–600. doi: 10.1016/j.eururo.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 55.Kato M, Roberts-Thomson P, Phillips BG, Haynes WG, Winnicki M, et al. Impairment of endothelium-dependent vasodilation of resistance vessels in patients with obstructive sleep apnea. Circulation. 2000;102:2607–10. doi: 10.1161/01.cir.102.21.2607. [DOI] [PubMed] [Google Scholar]
- 56.Soukhova-O’Hare GK, Shah ZA, Lei Z, Nozdrachev AD, Rao CV, et al. Erectile dysfunction in a murine model of sleep apnea. Am J Respir Crit Care Med. 2008;178:644–50. doi: 10.1164/rccm.200801-190OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Liu K, Liu XS, Xiao L, Shang J, Li MC, et al. NADPH oxidase activation: a mechanism of erectile dysfunction in a rat model of sleep apnea. J Androl. 2012;33:1186–98. doi: 10.2164/jandrol.112.016642. [DOI] [PubMed] [Google Scholar]
- 58.Ip MS, Lam B, Chan LY, Zheng L, Tsang KW, et al. Circulating nitric oxide is suppressed in obstructive sleep apnea and is reversed by nasal continuous positive airway pressure. Am J Respir Crit Care Med. 2000;162:2166–71. doi: 10.1164/ajrccm.162.6.2002126. [DOI] [PubMed] [Google Scholar]
- 59.Schulz R, Schmidt D, Blum A, Lopes-Ribeiro x, Lucke C, et al. Decreased plasma levels of nitric oxide derivatives in obstructive sleep apnoea: response to CPAP therapy. Thorax. 2000;55:1046–51. doi: 10.1136/thorax.55.12.1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Epstein LJ, Kristo D, Strollo PJ, Jr, Friedman N, Malhotra A, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5:263–76. [PMC free article] [PubMed] [Google Scholar]
- 61.Mehta V, Vasu TS, Phillips B, Chung F. Obstructive sleep apnea and oxygen therapy: a systematic review of the literature and meta-analysis. J Clin Sleep Med. 2013;9:271–9. doi: 10.5664/jcsm.2500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Malhotra A, White DP. Obstructive sleep apnoea. Lancet. 2002;360:237–45. doi: 10.1016/S0140-6736(02)09464-3. [DOI] [PubMed] [Google Scholar]
- 63.Karacan I, Karatas M. Erectile dysfunction in sleep apnea and response to CPAP. J Sex Marital Ther. 1995;21:239–47. doi: 10.1080/00926239508414643. [DOI] [PubMed] [Google Scholar]
- 64.Perimenis P, Karkoulias K, Konstantinopoulos A, Perimeni PP, Katsenis G, et al. Sildenafil versus continuous positive airway pressure for erectile dysfunction in men with obstructive sleep apnea: a comparative study of their efficacy and safety and the patient's satisfaction with treatment. Asian J Androl. 2007;9:259–64. doi: 10.1111/j.1745-7262.2007.00085.x. [DOI] [PubMed] [Google Scholar]
- 65.Perimenis P, Karkoulias K, Markou S, Gyftopoulos K, Athanasopoulos A, et al. Erectile dysfunction in men with obstructive sleep apnea syndrome: a randomized study of the efficacy of sildenafil and continuous positive airway pressure. Int J Impot Res. 2004;16:256–60. doi: 10.1038/sj.ijir.3901219. [DOI] [PubMed] [Google Scholar]
- 66.Li x, Dong Z, Wan Y, Wang Z. Sildenafil versus continuous positive airway pressure for erectile dysfunction in men with obstructive sleep apnea: a meta-analysis. Aging Male. 2010;13:82–6. doi: 10.3109/13685530903406789. [DOI] [PubMed] [Google Scholar]
- 67.Zhuravlev VN, Frank MA, Gomzhin AI. Sexual functions of men with obstructive sleep apnoea syndrome and hypogonadism may improve upon testosterone administration: a pilot study. Andrologia. 2009;41:193–5. doi: 10.1111/j.1439-0272.2008.00914.x. [DOI] [PubMed] [Google Scholar]
- 68.Cruz IA, Drummond M, Winck JC. Obstructive sleep apnea symptoms beyond sleepiness and snoring: effects of nasal APAP therapy. Sleep Breath. 2012;16:361–6. doi: 10.1007/s11325-011-0502-4. [DOI] [PubMed] [Google Scholar]
- 69.Perimenis P, Karkoulias K, Konstantinopoulos A, Alchanatis M, Perimeni PP, et al. The impact of long-term conventional treatment for overlap syndrome (obstructive sleep apnea and chronic obstructive pulmonary disease) on concurrent erectile dysfunction. Respir Med. 2007;10:210–6. doi: 10.1016/j.rmed.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 70.Margel D, Tal R, Livne PM, Pillar G. Predictors of erectile function improvement in obstructive sleep apnea patients with long-term CPAP treatment. Int J Impot Res. 2005;17:186–90. doi: 10.1038/sj.ijir.3901268. [DOI] [PubMed] [Google Scholar]
- 71.Budweiser S, Luigart R, Jorres RA, Kollert F, Kleemann Y, et al. Long-term changes of sexual function in men with obstructive sleep apnea after initiation of continuous positive airway pressure. J Sex Med. 2013;10:524–31. doi: 10.1111/j.1743-6109.2012.02968.x. [DOI] [PubMed] [Google Scholar]
- 72.Althof SE, Corty EW, Levine SB, Levine F, Burnett AL, et al. EDITS: development of questionnaires for evaluating satisfaction with treatments for erectile dysfunction. Urology. 1999;53:793–9. doi: 10.1016/s0090-4295(98)00582-2. [DOI] [PubMed] [Google Scholar]
- 73.Pastore AL, Palleschi G, Ripoli A, Silvestri L, Maggioni C, et al. Severe obstructive sleep apnoea syndrome and erectile dysfunction: a prospective randomised study to compare sildenafil vs. nasal continuous positive airway pressure. Int J Clin Pract. 2014;68:995–1000. doi: 10.1111/ijcp.12463. [DOI] [PubMed] [Google Scholar]
- 74.Roizenblatt S, Guilleminault C, Poyares D, Cintra F, Kauati A, et al. A double-blind, placebo-controlled, crossover study of sildenafil in obstructive sleep apnea. Arch Intern Med. 2006;166:1763–7. doi: 10.1001/archinte.166.16.1763. [DOI] [PubMed] [Google Scholar]
- 75.Neves C, Tufik S, Chediek F, Poyares D, Cintra F, et al. Effects of sildenafil on autonomic nervous function during sleep in obstructive sleep apnea. Clinics (Sao Paulo) 2010;65:393–400. doi: 10.1590/S1807-59322010000400008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Guilleminault C, Simmons FB, Motta J, Cummiskey J, Rosekind M, et al. Obstructive sleep apnea syndrome and tracheostomy. Long-term follow-up experience. Arch Intern Med. 1981;141:985–8. [PubMed] [Google Scholar]
- 77.Shin HW, Park JH, Park JW, Rhee CS, Lee CH, et al. Effects of surgical vs. nonsurgical therapy on erectile dysfunction and quality of life in obstructive sleep apnea syndrome: a pilot study. J Sex Med. 2013;10:2053–9. doi: 10.1111/jsm.12128. [DOI] [PubMed] [Google Scholar]


