Abstract
Smoking is a well-known risk factor of reproductive health. However, the effect of paternal smoking on fertility has been less extensively examined. We conducted a cross-sectional study in a mountainous area of South-West China to assess the effect of male smoking on couples’ fertility. A total of 8200 couples aged 18–49 years in the study area were invited to participate in the study. An in-person interview was performed to collect demographic characteristics of the couples, and husbands’ life style factors including smoking and drinking habits. Information on time to pregnancy (TTP) was collected retrospectively. Infertility was defined as failure to achieve clinical pregnancy after regular unprotected intercourse for ≥12 months. Logistic regression model was used to estimate the association between male smoking and infertility. A total of 7025 couples were included in the final analysis. After adjusting for potential confounders, the couples were more likely to suffer from infertility if the husbands smoked (adjusted odds ratio [aOR] =1.28, 95% CI: 1.08–1.52) before the first pregnancy. After the analyses were performed according to husbands’ smoking duration, an increased risk started at a relatively longer smoking duration of 5–10 years (aOR = 1.58, 95% CI: 1.26–1.99) and a stronger association (aOR = 3.34, 95% CI: 2.45–4.56) was observed in the group of ≥10 years. Similar patterns were found for the number of cigarettes smoked per day and the total amount of cigarettes smoked. From our findings, we conclude that male smoking may have an adverse impact on couples’ infertility.
Keywords: cross-sectional study, infertility, male smoking
INTRODUCTION
Infertility, one critical component of reproductive health, has been defined as failure to achieve clinical pregnancy after regular unprotected intercourse for 12 months or more.1 The prevalence of infertility has been increasing globally, and the number of couples affected by infertility has reached 48.5 million in 2010.2
Smoking is a well-known risk factor of reproductive health.3,4,5 Given a large number of smokers worldwide as well as the reproductive toxicity induced by cigarette smoking in animal studies,6 there have been growing concerns that smoking may lead to reduced fecundity in human. Currently, available evidence suggested a causal association between maternal smoking and reduced fertility.7,8,9,10,11 However, the effect of paternal smoking on fertility has been less extensively examined, although the well-established association between male smoking and semen quality makes this effect biologically plausible.5,12,13,14,15,16,17,18 Some investigators reported that paternal smoking had an adverse effect on fecundity,10,19,20,21 but this was not confirmed by others.22,23,24,25,26 Furthermore, those studies showing no association between male smoking and fecundity lacked sufficient sample size or detailed information on male smoking.22,24,26 Therefore, we conducted a population-based study in a remote mountainous area of China to assess the effect of male smoking on fertility.
METHODS
Study population and subjects
From November 2011 to August 2012, a cross-sectional study was conducted in Sandu Shui Autonomous County of Guizhou province, which is in a mountainous area of South-West China, with a predominantly rural population. A total of 8200 couples aged 18–49 years who had been married for more than 12 months were invited to participate in the study and 7846 couples were enrolled (response rate: 95.7%). After an exclusion of 645 couples who did not answer the key questions, 96 couples who had been trying to have a baby for <1 year until the initiation of our investigation, and 80 couples who were remarried, a total of 7025 couples were included in this study. The study was approved by Ethics Committees of Shanghai Institute of Planned Parenthood Research, and written informed consent was obtained from all participants.
Data collection
An in-person interview was performed by trained interviewers. Participated couples provided information on their sociodemographic characteristics, including dates of birth, nationalities, educational levels, and current occupations. The husbands were asked about their smoking and drinking habits. We defined smoking as consuming at least 1 cigarette per day for more than 6 months and drinking as consuming alcohol beverages (beer, wine, and liquor) at least once a week for more than 6 months. Detailed information on smoking including current or previous smoking, age at starting smoking, the number of cigarettes smoked per day, and the duration of smoking (recorded as years) was obtained from those who smoked.
Wives’ reproductive histories were also collected, including whether they have been pregnant and the outcome of each pregnancy. Those who had been pregnant were asked “How many months did it take you to conceive for each pregnancy?” with an answer list of <6 months, 6–11 months, 12–24 months, and >24 months. Those who had never been pregnant were asked to record the number of months since they had been trying to conceive. We defined infertility as waiting time to pregnancy (TTP) ≥12 months of the first pregnancy for those who had got pregnancy and time of trying to conceive ≥12 months for those who had never been pregnant. In the current study, we used the first pregnancy of each couple for identification of infertility because the later pregnancies had more chances of suffering from confounding.27 Wives’ age at menarche and regularity of menstrual cycle were also collected.
Statistical analysis
All statistical analyses were performed using SAS software (version 9.1, SAS Institute Inc., Cary, NC, USA). All P values were calculated by two-sided tests and were considered statically significant if P < 0.05.
Infertility rates were calculated according to sociodemographic characteristics. Logistic regression model was used to estimate odds ratio (OR) and its 95% confidence interval (CI) of infertility associated with husbands’ smoking after adjustment for potential confounders including wives’ age at planning pregnancy, education level, and age at menarche, as well as husbands’ occupation and drinking status. The confounders were chosen because of their potential influence on infertility, as indicated elsewhere.28 Chi-square test for trend was used to examine the dose-response relationship between husbands’ smoking and infertility, according to the duration of smoking, number of cigarettes smoked per day, and the total amount of cigarettes.
To reduce the confounding effect of age on the association between male smoking and infertility, we restricted the analysis to couples who had their first pregnancy before 30 years old since their fecundity was less variable. We also performed subgroup analyses among couples whose first pregnancy ended with live birth, as well as those with live birth and TTP <24 months, who were assumed to be in good health status, to attenuate the impact of individual's health condition that may cause infertility. To eliminate the influence of drinking alcohol on infertility, we repeated the above analysis in those with nondrinking husbands.
RESULTS
In the current study, there were 52 couples who had never conceived, of the remainders, 5131 (73.58%) couples spent <6 months to get pregnant, 1093 (15.67%) couples waited for 6–12 months and others (10.74%) spent more than 12 months. There were 2689 (38.3%) husbands who had smoked before their wives conceived, and 801 (11.40%) couples who were infertile. A majority of couples (85.4% for wives and 65.2% for husbands) married before 25 years old. Most of the couples are of Shui nationality (57.8% for wives and 59.2% for husbands), followed by Bouyei (23.8% for wives and 26.0% for husbands), Miao (11.9% for wives and 10.9% for husbands), Han nationality (5.4% for wives and 3.6% for husbands), and others. Most of the couples (75.7% for wives and 70.4% for husbands) worked as farmers and had an education level of elementary school or middle school (91.1% for wives and 85.0% for husbands).
Table 1 shows the infertility rate according to characteristics of the couples. Couples with Nationality of Miao, with education level of preschool, or with wives’ marriage age ≥31 years had slightly higher infertility rates. We observed a trend that infertility rate increased with age at menarche. A higher infertility rate was also observed among couples with husbands smoking or drinking before their wives became pregnant (13.8% and 14.3%, respectively) when compared with those with husbands who did not smoke or drink (9.9% and 9.9%, respectively). In addition, the infertility rate of the couples with husbands never smoking at home (15.1%) was slightly higher than those with husbands smoking at home (13.9%).
Table 1.
The infertility rate in relation to the characteristics of the couples
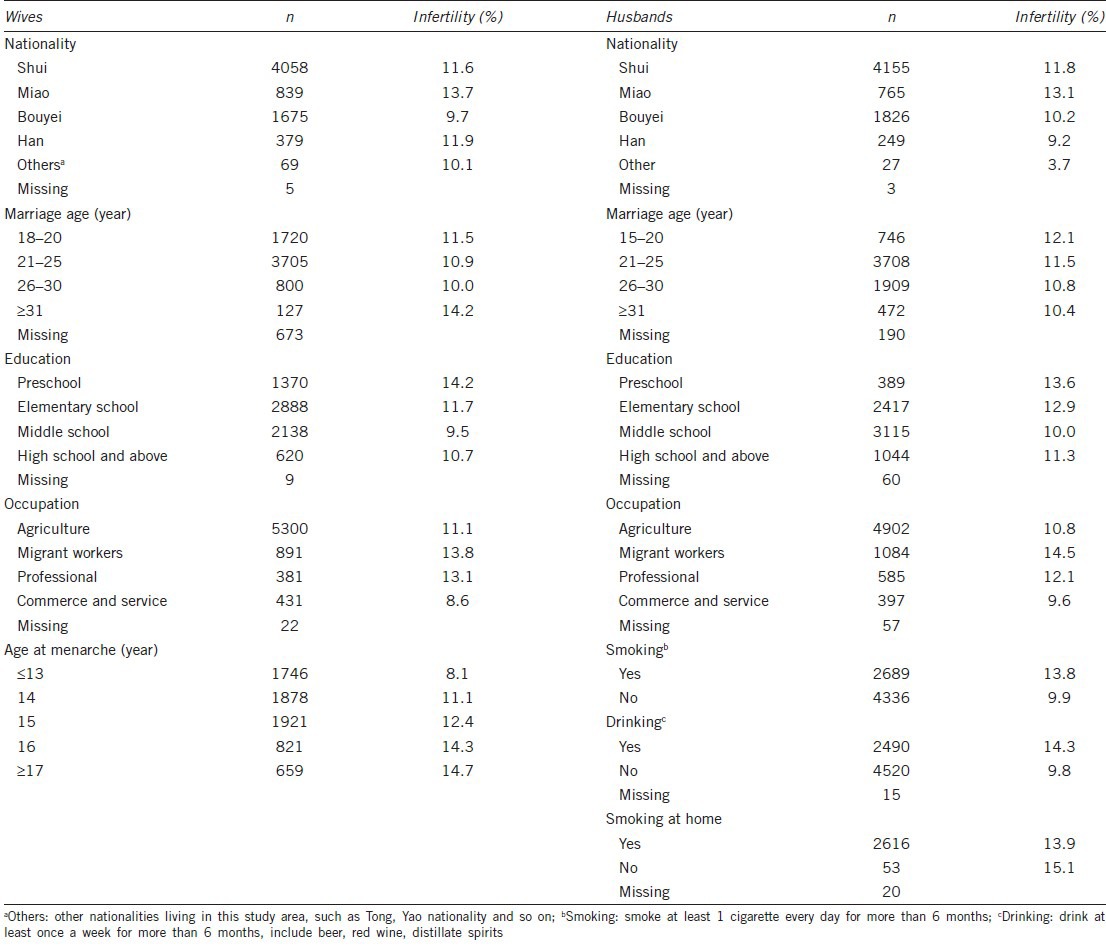
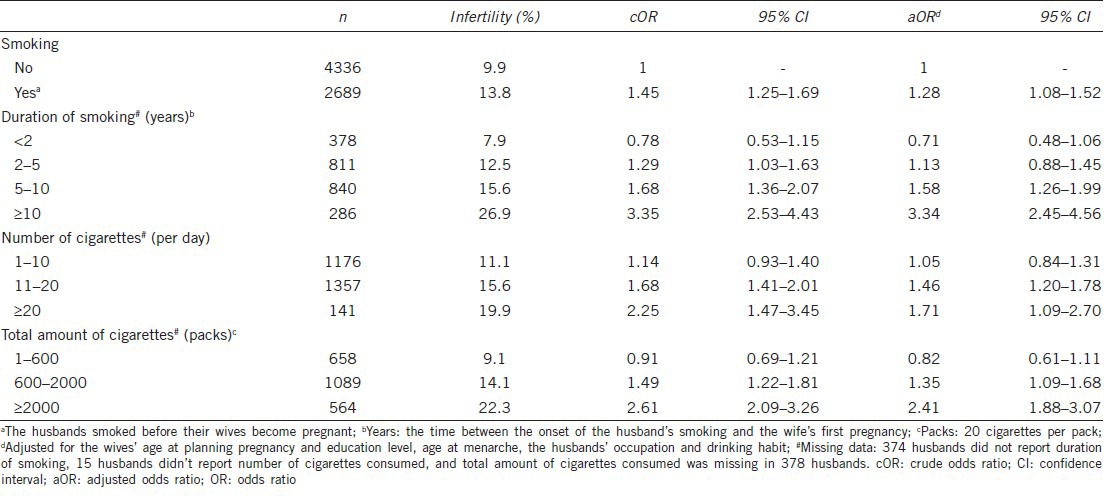
Table 2 shows the risks for infertility of couples according to husbands’ smoking characteristics. After adjusting for potential confounders, the couples with smoking husbands were more likely to suffer from infertility than those with nonsmoking husbands (OR = 1.28, 95% CI: 1.08–1.52). When the analyses were performed by husbands’ smoking duration, an increased risk started at a relatively longer smoking duration of 5–10 years (aOR = 1.58, 95% CI: 1.26–1.99) and a stronger association (aOR = 3.34, 95% CI: 2.45–4.56) was observed in the group of ≥10 years. Similar patterns were found for the number of cigarettes smoked per day and total amount of cigarettes smoked. The increased risks started at groups of 11–20 cigarettes smoked per day (aOR = 1.46, 95% CI: 1.20–1.78) and 600–2000 packs totally smoked (aOR = 1.35, 95% CI: 1.09–1.68), and stronger associations were observed in the groups of ≥20 cigarettes per day (aOR = 1.71, 95% CI: 1.01–2.70) and ≥2000 packs totally smoked (aOR = 2.41, 95% CI: 1.88–3.07). There were clear trends of increased risk of infertility with increased smoking years (P for trend <0.001), number of cigarettes smoked per day (P for trend <0.001), and the total consumption of cigarettes (P for trend < 0.001).
Table 2.
ORs of infertility among couples according to husbands smoking characters
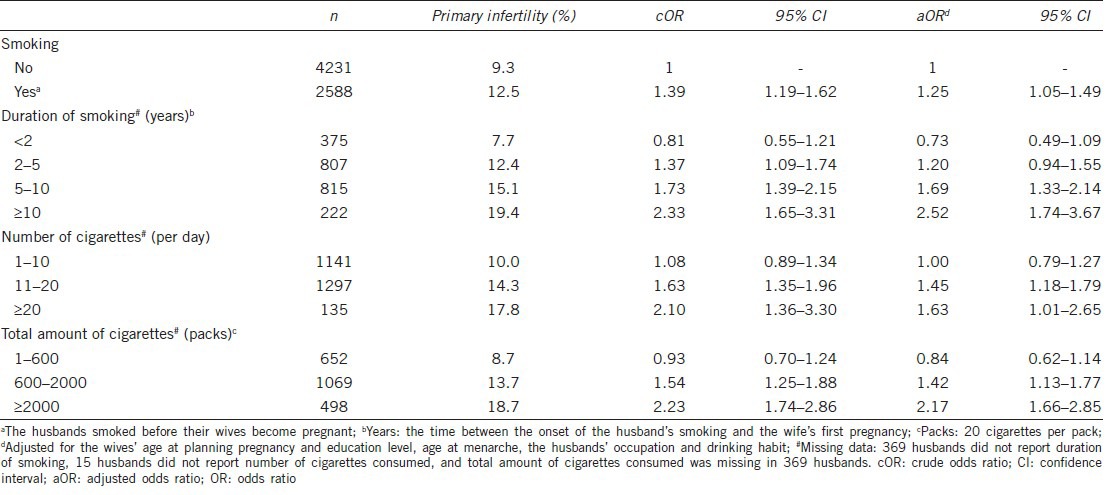
When we repeated the above analyses by restricting to couples who had their first pregnancy before 30 years old, the trend that infertility rate increased with increasing consumption of cigarettes persisted and the odds ratio of infertility for each sub-category of smoking characteristics did not essentially change (Table 3). Similar results were observed when we restricted the analysis to couples whose first pregnancy ended with live births, as well as to those with live births and TTP <24 months. We also did a subgroup analysis after excluding those who had never been pregnant (52 women) and found similar results. To further examine whether the observed association also existed among those with nondrinking husbands, we repeated the above analysis after excluding the couples with drinking husbands. Despite a markedly reduced sample size, the associations between male smoking and couples’ infertility persisted (data not shown).
Table 3.
ORs of primary infertility among couples whose first pregnancy were before 30 years old
DISCUSSION
In the current study, we found that husbands’ smoking was associated with couples’ infertility. We also observed a dose-response relationship that the associations increased with the increasing years of smoking, number of cigarettes smoked per day, and the total consumption of cigarettes.
Previous studies also reported similar association between male smoking and delayed conception,10,19,20 while in other studies male smoking appeared to have little or no impact on fertility.22,23,24,25,26 Dunphy et al.24 examined the relationship between male smoking and fecundity in 330 couples attending an infertility clinic for the first time and found that the couple's fecundity was unrelated to the number of cigarettes smoked by the male partner. However, the clinic-based study design restricted the validity of the results. Besides, another study found cigarette smoking intake did not differ between 42 subfertile men and 121 fertile men.26 Nevertheless, the small sample size and incomplete information of cigarettes consumption may have limited power to examine the association. Baird and Wilcox25 also suggested that TTP was not affected by the husband's smoking. Another study conducted by Bolumar et al.22 also found no association between paternal smoking and fertility among more than 4000 couples. Whereas the information about male smoking habits in the above two studies were collected from female partners, and besides, detailed data regarding the amount and duration of male smoking were not analyzed in both studies.
The associations we observed in the current study were supported by previous studies on smoking and semen quality and sperm DNA damage. Although the results have not been consistent, most studies reported male smokers had lower semen quality in terms of the conventional semen characteristics (sperm concentration, semen volume, total count, motility, and morphology) compared with nonsmokers.5,12,13,14,15,16,17,18,29 And lowered semen quality has been found to be associated with infertility.30,31 Besides, a number of studies have observed severe sperm DNA damage in male smokers, which could be another cause of infertility, since DNA fragmentation might prevent oocyte fertilization or embryo development.32,33,34,35 However, before any conclusion can be made, we should take the effect of maternal active and passive smoking into account. We did not collect information on female smoking in the study. In China, very few women (2.4%) smoked, especially in women at reproductive age (15–24 years, 0.7%; 25–44 years, 1.6%),36 therefore, the observed association was less likely to be explained by female active smoking. Increased male smoking is likely to be associated with increased passive smoking exposure of the female partner. Hence the observed association could be due to either the effect of male smoking or his partner's passive smoking, or both. However, the couple's infertility rate increased with the duration of husband's smoking before their first pregnancy, which indicated the risk of infertility associated with the husband's smoking could not be totally explained by the wife's passive smoking. Moreover, one recent study found, among women with no history of active smoking, passive smoking appeared to have little effect on fecundability.37 Besides, in the rural area of China, most of the wives’ passive smoking occur at home,38 thus the expected infertility rate would be higher for couples with husbands smoking at home than those with husbands never smoking at home. However, we observed similar infertility rate among the two groups. Thus, a male-mediated effect of smoking on fertility in the present study is reassuring.
This study had the advantage of being population-based with a relatively large sample size, which ensured the statistical power and provided an opportunity to adjust for a number of potential confounders. We had collected detailed information on male smoking, such as number of cigarettes smoked per day, the starting age of smoking, and years of smoking, so that we could analyze the dose-response relationship between male smoking and infertility. Furthermore, our study was conducted in a remote mountainous area where the industry is less developed. Therefore, our findings were less likely to be confounded by unmeasured environmental risk factors originated from pollution.
Our findings should be interpreted in the light of limitations. First, TTP was retrospectively collected to define couples’ infertility, which may introduce recall bias. However, women have remarkably accurate long-term recall of TTP, on a group basis.39,40 A previous study found that TTP data obtained retrospectively was virtually identical to that obtained concurrently, with a median duration of recall of 14 years.40 Thus, the recall bias on infertility was probably minimal in the current study. Second, it is possible that smoking habit was under-reported since it is known to be unhealthy. However, infertility data were obtained from the wives while smoking information was obtained from the husbands, and the participants were not informed of the objectives of the present study. Thus, the misclassification on smoking information was most likely to be nondifferential which often bias the risk estimates toward null. Third, there may have been confounding from factors that we did not measure (e.g., other medical history or carcinogens exposure, etc.). Couples with medical history may tend to reduce their smoking, so the nonsmoker group may falsely include more couples who suffer from subfertility. This differential misclassification would bias the risk estimates towards null. Besides, our study was conducted in an area where the industry is less developed, and residents had few chances to expose to carcinogens. Therefore, our findings were less likely to be confounded by unmeasured carcinogens exposure and other environmental risk factors. Fourth, the study was conducted in one remote mountainous area in China, where the distribution of demographic characteristic and lifestyle factors were somewhat distinct from the general population. It should be cautious to generalize the findings to other populations.
CONCLUSIONS
Our study provides evidence that male smoking had an adverse impact on fertility. Therefore, it seems advisable to encourage the male to quit smoking before the attempt to conceive.
AUTHOR CONTRIBUTIONS
WY, HL, MHM participated in the study design and coordination and helped to draft the manuscript; JPC, XQL and YFR collected and analyzed the data; FY and LL performed the analyses and wrote the manuscript; CLZ and YY participated in the data collection. All authors read and approved the final manuscript.
COMPETING INTERESTS
The authors report no competing interests.
ACKNOWLEDGMENTS
This study was supported and funded by a grant from the National Basic Research Program of China (Grant No. 2009CB941700). The authors would like to thank all of the volunteers that assisted with this study and all of the participants as well as the staff in this study.
REFERENCES
- 1.Zegers-Hochschild F, Adamson GD, de Mouzon J, Ishihara O, Mansour R, et al. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril. 2009;92:1520–4. doi: 10.1016/j.fertnstert.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 2.Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. 2012;9:e1001356. doi: 10.1371/journal.pmed.1001356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Practice Committee of the American Society for Reproductive Medicine. Smoking and infertility. Fertil Steril. 2004;81:1181–6. doi: 10.1016/j.fertnstert.2003.11.024. [DOI] [PubMed] [Google Scholar]
- 4.Vine MF. Smoking and male reproduction: a review. Int J Androl. 1996;19:323–37. doi: 10.1111/j.1365-2605.1996.tb00523.x. [DOI] [PubMed] [Google Scholar]
- 5.Kumar S, Murarka S, Mishra VV, Gautam AK. Environmental and lifestyle factors in deterioration of male reproductive health. Indian J Med Res. 2014;140(Suppl 1):S29–35. [PMC free article] [PubMed] [Google Scholar]
- 6.Dechanet C, Anahory T, Mathieu Daude JC, Quantin x, Reyftmann L, et al. Effects of cigarette smoking on reproduction. Hum Reprod Update. 2011;17:76–95. doi: 10.1093/humupd/dmq033. [DOI] [PubMed] [Google Scholar]
- 7.Zenzes MT. Cigarette smoking as a cause of delay in conception. Reprod Med Rev. 1995;4:189–205. [Google Scholar]
- 8.Olsen J, Rachootin P, Schiodt AV, Damsbo N. Tobacco use, alcohol consumption and infertility. Int J Epidemiol. 1983;12:179–84. doi: 10.1093/ije/12.2.179. [DOI] [PubMed] [Google Scholar]
- 9.Suonio S, Saarikoski S, Kauhanen O, Metsapelto A, Terho J, et al. Smoking does affect fecundity. Eur J Obstet Gynecol Reprod Biol. 1990;34:89–95. doi: 10.1016/0028-2243(90)90011-o. [DOI] [PubMed] [Google Scholar]
- 10.Olsen J. Cigarette smoking, tea and coffee drinking, and subfecundity. Am J Epidemiol. 1991;133:734–9. doi: 10.1093/oxfordjournals.aje.a115948. [DOI] [PubMed] [Google Scholar]
- 11.Alderete E, Eskenazi B, Sholtz R. Effect of cigarette smoking and coffee drinking on time to conception. Epidemiology. 1995;6:403–8. doi: 10.1097/00001648-199507000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Vogt HJ, Heller WD, Borelli S. Sperm quality of healthy smokers, ex-smokers, and never-smokers. Fertil Steril. 1986;45:106–10. doi: 10.1016/s0015-0282(16)49106-5. [DOI] [PubMed] [Google Scholar]
- 13.Chia SE, Ong CN, Tsakok FM. Effects of cigarette smoking on human semen quality. Arch Androl. 1994;33:163–8. doi: 10.3109/01485019408987820. [DOI] [PubMed] [Google Scholar]
- 14.Pasqualotto FF, Sobreiro BP, Hallak J, Pasqualotto EB, Lucon AM. Cigarette smoking is related to a decrease in semen volume in a population of fertile men. BJU Int. 2006;97:324–6. doi: 10.1111/j.1464-410X.2005.05906.x. [DOI] [PubMed] [Google Scholar]
- 15.Kunzle R, Mueller MD, Hanggi W, Birkhauser MH, Drescher H, et al. Semen quality of male smokers and nonsmokers in infertile couples. Fertil Steril. 2003;79:287–91. doi: 10.1016/s0015-0282(02)04664-2. [DOI] [PubMed] [Google Scholar]
- 16.Ramlau-Hansen CH, Thulstrup AM, Aggerholm AS, Jensen MS, Toft G, et al. Is smoking a risk factor for decreased semen quality? A cross-sectional analysis. Hum Reprod. 2007;22:188–96. doi: 10.1093/humrep/del364. [DOI] [PubMed] [Google Scholar]
- 17.Caserta D, Bordi G, Segni ND, D’Ambrosio A, Mallozzi M, et al. The influence of cigarette smoking on a population of infertile men and women. Arch Gynecol Obstet. 2013;287:813–8. doi: 10.1007/s00404-012-2643-5. [DOI] [PubMed] [Google Scholar]
- 18.Kovac JR, Khanna A, Lipshultz LI. The effects of cigarette smoking on male fertility. Postgrad Med. 2015;127:338–41. doi: 10.1080/00325481.2015.1015928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hull MG, North K, Taylor H, Farrow A, Ford WC. Delayed conception and active and passive smoking. The Avon Longitudinal Study of Pregnancy and Childhood Study Team. Fertil Steril. 2000;74:725–33. doi: 10.1016/s0015-0282(00)01501-6. [DOI] [PubMed] [Google Scholar]
- 20.Hassan MA, Killick SR. Negative lifestyle is associated with a significant reduction in fecundity. Fertil Steril. 2004;81:384–92. doi: 10.1016/j.fertnstert.2003.06.027. [DOI] [PubMed] [Google Scholar]
- 21.Sohrabvand F, Jafari M, Shariat M, Haghollahi F, Lotfi M. Frequency and epidemiologic aspects of male infertility. Acta Med Iran. 2014;53:231–5. [PubMed] [Google Scholar]
- 22.Bolumar F, Olsen J, Boldsen J. Smoking reduces fecundity: a European multicenter study on infertility and subfecundity. The European Study Group on Infertility and Subfecundity. Am J Epidemiol. 1996;143:578–87. doi: 10.1093/oxfordjournals.aje.a008788. [DOI] [PubMed] [Google Scholar]
- 23.de Mouzon J, Spira A, Schwartz D. A prospective study of the relation between smoking and fertility. Int J Epidemiol. 1988;17:378–84. doi: 10.1093/ije/17.2.378. [DOI] [PubMed] [Google Scholar]
- 24.Dunphy BC, Barratt CL, von Tongelen BP, Cooke ID. Male cigarette smoking and fecundity in couples attending an infertility clinic. Andrologia. 1991;23:223–5. doi: 10.1111/j.1439-0272.1991.tb02542.x. [DOI] [PubMed] [Google Scholar]
- 25.Baird DD, Wilcox AJ. Cigarette smoking associated with delayed conception. JAMA. 1985;253:2979–83. [PubMed] [Google Scholar]
- 26.de Jong AM, Menkveld R, Lens JW, Nienhuis SE, Rhemrev JP. Effect of alcohol intake and cigarette smoking on sperm parameters and pregnancy. Andrologia. 2012;46:112–7. doi: 10.1111/and.12054. [DOI] [PubMed] [Google Scholar]
- 27.Olsen J. Options in making use of pregnancy history in planning and analysing studies of reproductive failure. J Epidemiol Community Health. 1994;48:171–4. doi: 10.1136/jech.48.2.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baird DD, Wilcox AJ, Weinberg CR. Use of time to pregnancy to study environmental exposures. Am J Epidemiol. 1986;124:470–80. doi: 10.1093/oxfordjournals.aje.a114417. [DOI] [PubMed] [Google Scholar]
- 29.Zhang JP, Meng QY, Wang Q, Zhang LJ, Mao YL, et al. Effect of smoking on semen quality of infertile men in Shandong, China. Asian J Androl. 2000;2:143–6. [PubMed] [Google Scholar]
- 30.Bonde JP, Ernst E, Jensen TK, Hjollund NH, Kolstad H, et al. Relation between semen quality and fertility: a population-based study of 430 first-pregnancy planners. Lancet. 1998;352:1172–7. doi: 10.1016/S0140-6736(97)10514-1. [DOI] [PubMed] [Google Scholar]
- 31.de Souza MB, England GC, Mota Filho AC, Ackermann CL, Sousa CV, et al. Semen quality, testicular B-mode and Doppler ultrasound, and serum testosterone concentrations in dogs with established infertility. Theriogenology. 2015;15; 84:805–10. doi: 10.1016/j.theriogenology.2015.05.015. [DOI] [PubMed] [Google Scholar]
- 32.Mostafa T. Cigarette smoking and male infertility. J Adv Res. 2010;1:179–86. [Google Scholar]
- 33.Horak S, Polanska J, Widlak P. Bulky DNA adducts in human sperm: relationship with fertility, semen quality, smoking, and environmental factors. Mutat Res. 2003;537:53–65. doi: 10.1016/s1383-5718(03)00051-2. [DOI] [PubMed] [Google Scholar]
- 34.Shi Q, Ko E, Barclay L, Hoang T, Rademaker A, et al. Cigarette smoking and aneuploidy in human sperm. Mol Reprod Dev. 2001;59:417–21. doi: 10.1002/mrd.1048. [DOI] [PubMed] [Google Scholar]
- 35.Dai JB, Wang Zx, Qiao ZD. The hazardous effects of tobacco smoking on male fertility. Asian J Androl. 2015 Apr 7; doi: 10.4103/1008-682X.150847. doi: 10.4103/1008-682X.150847. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li Q, Hsia J, Yang G. Prevalence of smoking in China in 2010. N Engl J Med. 2011;364:2469–70. doi: 10.1056/NEJMc1102459. [DOI] [PubMed] [Google Scholar]
- 37.Radin RG, Hatch EE, Rothman KJ, Mikkelsen EM, Sørensen HT, et al. Active and passive smoking and fecundability in Danish pregnancy planners. Fertil Steril. 2014;102:183–91.e2. doi: 10.1016/j.fertnstert.2014.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.He Q, Wang J, Zhu Y, Peng WJ. Prevalence of passive smoking among inland residents in China: a systematic analysis of 2000-2009 studies. Chin J Epidemiol. 2011;32:159–63. [PubMed] [Google Scholar]
- 39.Zielhuis GA, Hulscher ME, Florack EI. Validity and reliability of a questionnaire on fecundability. Int J Epidemiol. 1992;21:1151–6. doi: 10.1093/ije/21.6.1151. [DOI] [PubMed] [Google Scholar]
- 40.Joffe M, Villard L, Li Z, Plowman R, Vessey M. Long-term recall of time-to-pregnancy. Fertil Steril. 1993;60:99–104. doi: 10.1016/s0015-0282(16)56044-0. [DOI] [PubMed] [Google Scholar]


