Abstract
Many different materials are available for grafting during surgery for Peyronie's disease (PD). To study the outcomes associated with the use of a lyophilized bovine pericardium graft (Peri-Guard®) to repair tunical defects in patients with PD, descriptive study of 43 patients with disabling penile curvature was performed. Curvature was measured before and after the intervention using a standardized procedure. Surgical technique was plaque excision and grafting of the tunical defect carried out by a single surgeon. A lyophilized bovine pericardium patch was used for grafting. We measured the change in penile curvature and length, the ability to perform successful sexual intercourse without further pharmacological or surgical treatment, and the satisfaction with treatment. Follow-up data were available for a total of 41 patients. Median age was 50 years (IQR 48–52); mean follow-up time was 14 ± 6 months. Complete penile straightening was achieved in 33 patients (80.5%) and five patients (12.2%) had curvature under 20°. Three months after surgery and stretching therapy, mean (s.d.) flaccid penile length increased from 11.2 ± 2.8 cm to 12.1 ± 2.9 cm (P = 0.062). Seventy-five percentage of patients reported being able to achieve successful intercourse without further treatment. Eighty-five percentage of patients reported to be satisfied with the treatment. There was no evidence of tissue rejection or infection, and only four patients suffered an adverse event. Plaque excision and grafting of the tunical defect with lyophilized bovine pericardium seems to be a safe and effective treatment for patients with PD.
Keywords: penile curvature, pericardium patch, Peyronie's disease, surgical treatment
INTRODUCTION
Peyronie's disease (PD) has been defined as a fibrotic wound-healing disorder of the tunica albuginea.1 Causes of PD include blunt penile trauma and trauma incurred during sexual intercourse though up to 70% of the condition is idiopathic.2 Characteristic features of the condition include penile curvature, penile plaques, hourglass defects, penile hinging/instability, and penile shortening3 and it is often associated with erectile dysfunction (ED). The curvature of the penis itself and the pain associated with erections can cause difficulties with sexual intercourse4 and loss of penile length and inability to have intercourse lead to a considerable psychological burden for the patient, with a negative impact on quality of life.5,6,7 Studies have estimated prevalence rates ranging from approximately 3% to 9%8,9,10,11 and have shown that prevalence increases with age.
Several pharmacological treatments exist to treat PD but have shown variable degrees of success.12 Surgery is therefore still considered the gold standard for definitive treatment in stable patients with penile deformity leading to impaired sexual function.13 The aim of surgery should be to allow the patient to resume his normal sexual relationship.14 Current treatment algorithms indicate that, in men with curvatures over 60° and good erectile function, who are willing to risk a higher rate of postoperative erectile dysfunction, tunical incision, preferably with grafting, and offers an excellent surgical option.14 For use in this type of procedure, a wide range of graft options are available, including autologous, nonautologous, and processed animal grafts, though evidence currently does not conclusively support the use of one type of graft over another.3
The aim of the present paper is to present our experience with the use of a lyophilized bovine pericardium graft (Peri-Guard®, Synovis Surgical Innovations) to repair tunical defects in a cohort of 43 patients with PD. Outcomes assessed were ability to perform successful sexual intercourse, improvements in curvature, change in penile length, and satisfaction with treatment.
MATERIALS AND METHODS
This was a prospective, descriptive study performed from January 2010 to June 2014 in a total of 43 patients with disabling penile curvature that interfered with sexual intercourse. Patients were accepted for surgery and included in the study if they had stable PD for >6 months, were <55 years of age, had no more than one risk factor for erectile function (diabetes mellitus [DM], high blood pressure, vasculopathy, obesity, high cholesterol, high triglycerides), testosterone >350 ng dl−1, a score on the Sexual Health Inventory for Men (SHIM) ≥24, and penile curvature >65°. A total of 114 patients did not meet the inclusion criteria for many different reasons (older patients, not enough curvature, two or more risk factors, etc.) (Figure 1). Curvature was measured before and after the intervention using a standardized procedure applied by the same technician. Informed consent was obtained from all patients included in this study.
Figure 1.
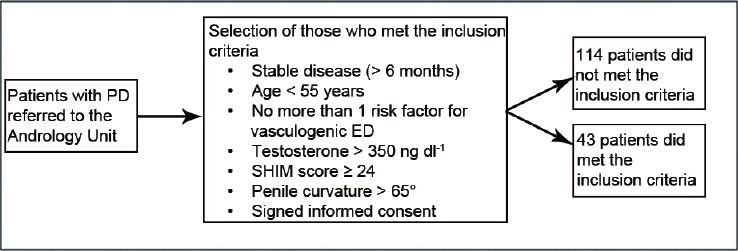
Distribution of the patients.
The preoperative evaluation included history and physical examination and administration of a validated questionnaire (Sexual Health Inventory for Men [SHIM]15) to evaluate the erectile function. Penile length was measured using the technique described by Wessells et al.16 With the patient in the supine position, the glans was grasped and pulled to full stretch at 90° from the plane of the body. A rigid ruler was used by pressing down on the suprapubic fat pad to the pubic bone, and the penis was measured dorsally to the corona or meatus depending on physician preference.
In all patients, grafting was carried out using a lyophilized bovine pericardium patch (Peri-Guard® Synovis Surgical Innovations). Plaque excision and grafting of the tunical defect were performed by a single surgeon.
Surgical procedures and technique
Once patients had demonstrated at least 6 months of stable disease, and after checking curvature by photography or induction with prostaglandin injection (20 μg), the SHIM was administered to verify good erectile function. Patients meeting inclusion criteria were then admitted on the day of surgery, which was performed under spinal anesthesia. Cefazolin (2 g, iv) was administered as antibiotic prophylaxis; anti-thrombosis prophylaxis was not used. A 16 Fr Foley catheter was placed in the sterile field and the penis was degloved using a subcoronal incision (Figure 2). The neurovascular bundle was carefully dissected using a bipolar scalpel when necessary and was released with scissors and a cold scalpel to avoid damage to blood vessels and nerves (Figure 3). Subsequently, an erection was induced by injecting saline into the corpus cavernosum to characterize the severity of curvature and plaque dimensions. Plaques were marked and excised in their entirety using the geometric technique described by Egydio et al.17 (Figure 2). Care was taken to avoid injury to underlying cavernosal tissue. After the neurovascular bundle was freed and the plaque excised (Figure 3), the pericardial graft material was soaked in abundant saline solution for at least 5 min to ensure thorough cleansing before being cut to a size 2–3 mm larger than the defect (Figure 4) and secured using a synthetic absorbable sterile surgical suture at the corners and the intercavernous septum (Figure 5). A continuous suture was then performed using monofilament synthetic absorbable surgical suture 4-0 with the penis maximally stretched throughout. Patch fitting and correction of the curvature was checked (Figures 6 and 7). Additional minor plications were occasionally used to ensure the minimum possible degree of curvature. The overlying layers of penile fascia were closed one by one and a light pressure dressing was applied for 4 days, at which point it was changed and a new one applied for a further 4 days.
Figure 2.
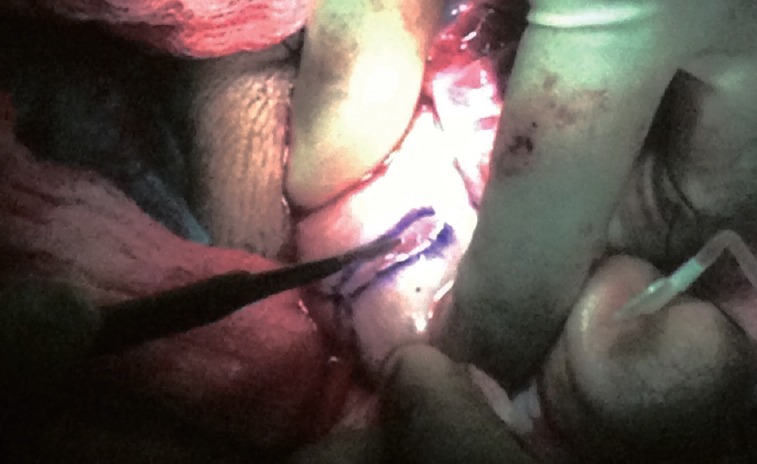
The tunica albuginea of the corpora cavernosa is revealed where the incision was made to correct the curvature.
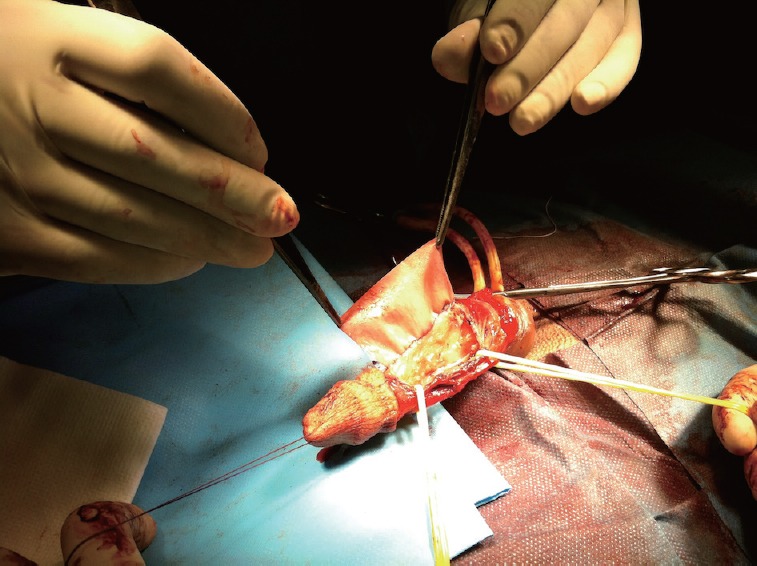
Figure 3.
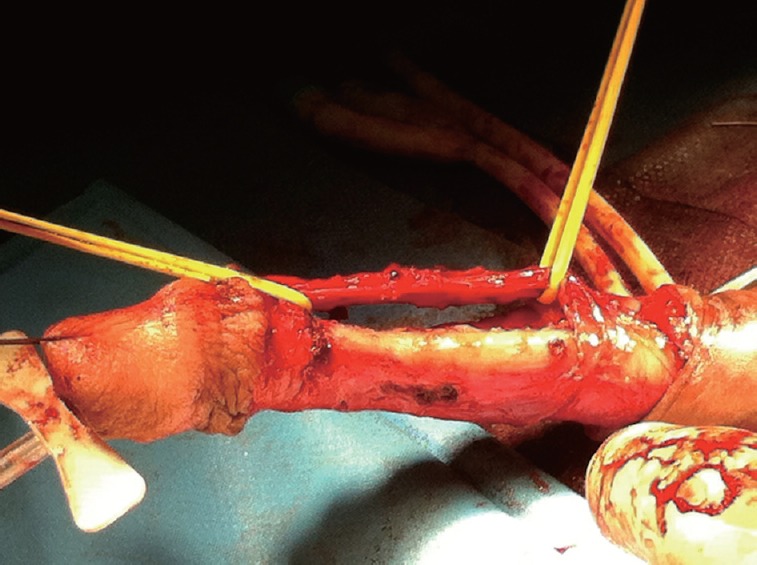
The penis with the neurovascular bundle completely raised and the fibrotic plaque completely removed from the dorsal side of the penis. Stretching the penis to confirm that there was no curvature through traction.
Figure 4.
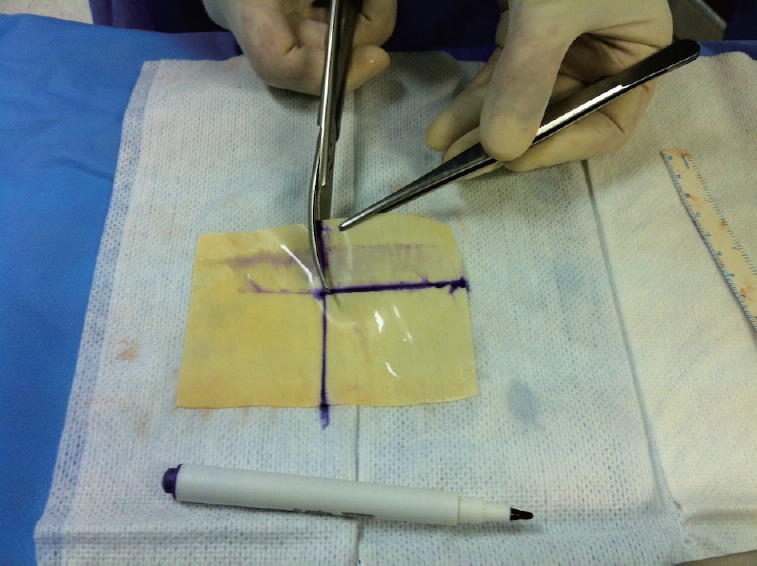
In the sterile field, and after washing in abundant saline solution, the lyophilized bovine pericardium patch was measured to provide a patch 2-3 mm larger than the defect.
Figure 5.
The patch was sutured to the penis using absorbable suture.
Figure 6.
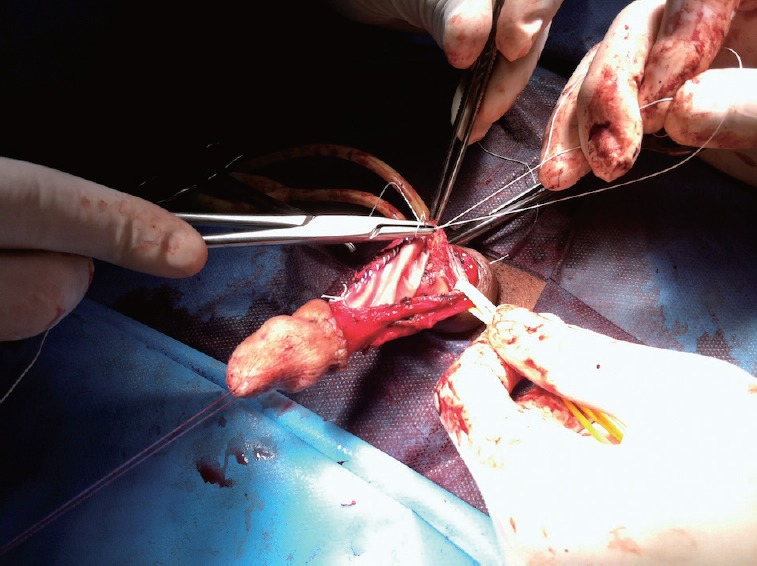
The patch was closed as tightly as possible to prevent blood leakage in the early stages of the postoperative period.
Figure 7.

The correction of curvature was checked.
Patients continued prescribed antibiotics for 7–10 days after the intervention and were instructed to abstain from intercourse for 6 weeks. They were also prescribed 5 mg daily of tadalafil to be taken at night for 3 months. Patients were further instructed to use a vacuum device without the constricting ring for 10 min, 3 times per day, starting approximately 2 weeks postoperatively for 3 months.
Baseline data collected included demographic characteristics, plaque location (ventral, dorsal, lateral), angle of curvature, co-morbidities, and the SHIM. Patch size was recorded during the intervention and surgical outcomes assessed were degree of curvature, penile size, capacity to perform successful intercourse with or without concomitant treatment (PDE-5i, alprostadil, penile prosthesis), and complications classified as: necrosis, ischemia, edema, infection, loss of sensation, or others. Capacity to perform successful intercourse was assessed using question three of the Sexual Encounter Profile (SEP), i.e., “Did your erection last long enough for you to have successful intercourse?” Satisfaction with the procedure was assessed by asking the patient whether he would be willing to undergo the intervention again. Multivariate analysis was used to determine whether there was a relationship between patch size and erectile dysfunction or between any of the other variables recorded and the need for additional treatment for erectile dysfunction.
RESULTS
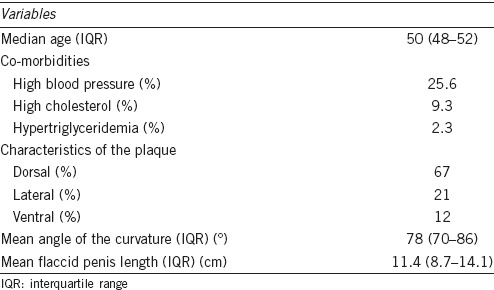
Median patient age was 50 years (IQR 48–52). High blood pressure was the most frequent co-morbidity (11/43 patients), followed by high cholesterol (4/43), diabetes mellitus (2/43), and hypertriglyceridemia (1/43). Plaque location was dorsal in 29 patients (67%), lateral in 9 (21%), and ventral in 5 (12%). The angle of curvature varied from 65° to 95°, with a mean of 78 ± 8°. Mean patch size was 12.8 ± 5.2 cm2. Mean flaccid penis length before the intervention was 11.4 ± 2.7 cm. The preoperative variables of the patients are resumed in Table 1.
Table 1.
Preoperative variables of the patients
Patients were followed up for a mean of 14 ± 6 months. Two patients were lost to follow-up as they returned to their countries of origin after the operation. The outcomes presented, therefore, refer to the remaining 41 patients. The results are summarized in Table 2. By the end of follow-up, pharmacologically induced erection showed that complete penile straightening was achieved in 33 patients (80.5%), 5 had a curvature of <20° (12.2%), and 3 had a curvature of >20° (7.3%). Two weeks after surgery, mean flaccid penile length was 11.2 ± 2.8 cm and 3 months later, after stretching therapy with the vacuum device, it was 12.1 ± 2.9 cm. The differences in penis length from baseline at both these time points were not statistically significant (P = 0.18 and 0.062, respectively).
Table 2.
Clinical outcomes after surgery
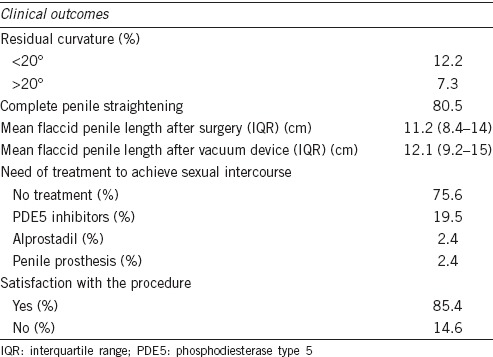
In order to achieve successful intercourse during follow-up, as assessed using question 3 of the SEP questionnaire, 31 of 41 patients (75.6%) did not require any further treatment, 8/41 (19.5%) required PDE5 inhibitors, 1 (2.4%) required alprostadil, and one patient (with diabetes mellitus) required a penile prosthesis (Table 2).
In terms of satisfaction with the procedure, 35 of 41 patients (85.4%) stated that they would elect to have the surgery again, while six said they would not (one patient with penile prosthesis, one patient who required alprostadil, three patients with curvature >20°, and one patient who reported finding the procedure too time-consuming).
There was no evidence of tissue rejection or infection. One patient suffered ischemia of the glans, one penile edema, and two reported a loss of sensation. There was no relationship between patch size and erectile function assessed using SHIM responses nor any relationship between any of the other variables assessed and the need for additional treatment for erectile function. There was no evidence of patch retraction in any of the patients.
DISCUSSION
Current treatment guidelines for Peyronie's disease recommend tunical incision, preferably with grafting, as an appropriate treatment option in men with curvatures over 60° and good erectile function.14 A wide variety of options are available for grafting materials though currently available materials can be classified into one of three types: autologous graft materials, allografts/xenografts, and synthetic grafts.18 At present, there is no clear evidence for selecting one type of graft material over another, though the ideal characteristics of any graft material include being easily manipulated, with high tensile strength, a low risk of infection, minimal inflammation, and low antigenicity risk, as well as being available in different sizes, and for a reasonable cost.19
In the present series, a lyophilized bovine pericardium patch was used for grafting. The outcomes achieved were highly satisfactory, with 75% of the patients treated not requiring any further treatment, either pharmacological or surgical, to achieve successful intercourse. Complete penile straightening was achieved in 80% of patients and penile length increased by approximately 1 cm though the difference was not statistically significant. These results compare favorably with the previous series. For example, Chun et al.20 in a comparison of dermal and cadaveric pericardial grafts used in a modified Horton-Devine procedure, reported that of 22 patients reporting successful coitus after the intervention, 15 (63%) needed assistance to achieve an erection which was sufficiently rigid for satisfactory coitus, which is a substantially higher proportion of patients requiring assistance than in this study. Eight patients also reported recurrent curvature. In the series reported by Kovac and Brock21 which had a substantially longer follow-up time, and which compared dermal, pericardial, and small intestinal submucosal grafting, self-reported resolution of penile curvature was recorded in 60% of dermal, 100% of Tutoplast, and 76.9% of Stratasis graft recipients; Stratasis patients also maintained presurgery length and rigidity to a greater extent than the other patients.
Leungwattanakij et al.22 also reported on the long-term follow-up of patients receiving a pericardial graft in surgery for Peyronie's disease. After a mean follow-up of 30 months, the three patients who had received prosthesis continued to report excellent sexual function. Of those who did not receive prosthesis, the patients with a small initial plaque size continued to do well while those with large plaque size reported difficulty maintaining an erection due to venous leakage. In our study, none of the variables studied, including patch size (which could serve as a proxy for plaque size, given that plaque size was not recorded), were associated with poorer outcomes in terms of sexual function and improvement in curvature, and only one patient required a penile prosthesis. Other similar series reported rates of 98%23 and 88%24 of patients with successful penile straightening and 30% with some degree of ED requiring pharmacological assistance for intercourse.23 Hellstrom and Reddy25 also reported resolution of penile curvature in all 11 patients studied, allowing for normal sexual function after a mean follow-up of 14 months.
As in this study, previous studies using pericardial grafts reported no evidence of tissue rejection, infection or other graft related adverse events; and those that included patient satisfaction as an outcome variable reported similarly high rates of satisfaction to the 85% of patients in the present series who stated that they would be willing to undergo the intervention again. The patch used has several advantages over other types of the patch including the fact that a further incision is not required to obtain and, because it is easy to use and does not require extensive preparation, its use helps expedite the surgical procedure. It is also not costly and, therefore, does not add substantially to the costs of the intervention.
Obviously, the high rates of successful outcomes and satisfaction with the procedure will be likely due to some extent to the fact that this is a carefully selected population. Only those patients meeting a set of quite strict criteria were scheduled for surgery. It remains to be seen whether relaxing those criteria would lead to poorer outcomes. On the other hand, the postintervention period in which patients are exhaustively monitored and controlled to ensure that they adhere appropriately to follow-up treatments is also crucial. Those treatments include 3 months of treatment with tadalafil 5 mg per 24 h, 3 times daily use of a vacuum device without a ring to produce erections lasting 5 s, and repeated mechanical traction using a penile extender; monitoring those treatments means that the patient's progress is carefully assessed and that patients are highly motivated and involved in their recovery. Those treatments likely played a role in the mean 1 cm of penis enlargement seen in this study, although the result was not statistically significant.
The descriptive nature of the present study is clearly a limitation in terms of ascribing the successful outcomes and lack of adverse events to a specific surgical approach or the use of one particular graft material. However, this study does add to the accumulating evidence regarding the highly satisfactory performance of pericardial graft materials in the surgical treatment of patients with PD. The number of patients included was likewise not large, though larger than some earlier series, and acceptable when considering that only one type of patch was studied. In future studies, it might also be interesting to include measures of overall quality of life to understand the impact of this type of intervention on a broader range of dimensions, including mood and well-being.
CONCLUSIONS
Plaque excision and grafting of the tunical defect with lyophilized bovine pericardium appeared to be a safe and effective treatment in this cohort of selected patients with PD.
AUTHOR CONTRIBUTIONS
The study was designed by JRO, who also put in contact the centers. The data were collected by JRO, BGG, JMP, CPM, SGB and EGC. In the writing collaborated JRO and BGG. The paper was revised by JRV and ARA.
COMPETING INTERESTS
All the authors declare no competing interests.
REFERENCES
- 1.Levine LA, Larsen SM. Surgery for Peyronie's disease. Asian J Androl. 2013;15:27–34. doi: 10.1038/aja.2012.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Levine LA, Burnett AL. Standard operating procedures for Peyronie's disease. J Sex Med. 2013;10:230–44. doi: 10.1111/j.1743-6109.2012.03003.x. [DOI] [PubMed] [Google Scholar]
- 3.Segal RL, Burnett AL. Surgical management for Peyronie's disease. World J Mens Health. 2013;31:1–11. doi: 10.5534/wjmh.2013.31.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schwarzer U, Sommer F, Klotz T, Braun M, Reifenrath B, et al. The prevalence of Peyronie's disease: results of a large survey. BJU Int. 2001;88:727–30. doi: 10.1046/j.1464-4096.2001.02436.x. [DOI] [PubMed] [Google Scholar]
- 5.Smith JF, Walsh TJ, Conti SL, Turek P, Lue T. Risk factors for emotional and relationship problems in Peyronie's disease. J Sex Med. 2008;5:2179–84. doi: 10.1111/j.1743-6109.2008.00949.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nelson CJ, Diblasio C, Kendirci M, Hellstrom W, Guhring P, et al. The chronology of depression and distress in men with Peyronie's disease. J Sex Med. 2008;5:1985–90. doi: 10.1111/j.1743-6109.2008.00895.x. [DOI] [PubMed] [Google Scholar]
- 7.Rosen R, Catania J, Lue T, Althof S, Henne J, et al. Impact of Peyronie's disease on sexual and psychosocial functioning: qualitative findings in patients and controls. J Sex Med. 2008;5:1977–84. doi: 10.1111/j.1743-6109.2008.00883.x. [DOI] [PubMed] [Google Scholar]
- 8.Sommer F, Schwarzer U, Wassmer G, Bloch W, Braun M, et al. Epidemiology of Peyronie's disease. Int J Impot Res. 2002;14:379–83. doi: 10.1038/sj.ijir.3900863. [DOI] [PubMed] [Google Scholar]
- 9.Rhoden EL, Teloken C, Ting HY, Lucas ML, Teodósio da Ros C, et al. Prevalence of Peyronie's disease in men over 50-y-old from Southern Brazil. Int J Impot Res. 2001;13:291–3. doi: 10.1038/sj.ijir.3900727. [DOI] [PubMed] [Google Scholar]
- 10.La Pera G, Pescatori ES, Calabrese M, Boffini A, Colombo F, et al. Peyronie's disease: prevalence and association with cigarette smoking. A multicenter population-based study in men aged 50-69 years. Eur Urol. 2001;40:525–30. doi: 10.1159/000049830. [DOI] [PubMed] [Google Scholar]
- 11.Mulhall JP, Creech SD, Boorjian SA, Ghaly S, Kim ED, et al. Subjective and objective analysis of the prevalence of Peyronie's disease in a population of men presenting for prostate cancer screening. J Urol. 2004;171:2350–3. doi: 10.1097/01.ju.0000127744.18878.f1. [DOI] [PubMed] [Google Scholar]
- 12.Shaw EJ, Mitchell GC, Tan RB, Sangkum P, Hellstrom WJ. The non-surgical treatment of Peyronie's disease: 2013 update. World J Mens Health. 2013;31:183–92. doi: 10.5534/wjmh.2013.31.3.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tan RB, Sangkum P, Mitchell GC, Hellstrom WJ. Update on medical management of Peyronie's disease. Curr Urol Rep. 2014;15:415. doi: 10.1007/s11934-014-0415-4. [DOI] [PubMed] [Google Scholar]
- 14.Wespes E, Hatzimouratidis K, Eardley I, Giuliano F, Hatzichristou D, et al. EAU guidelines on penile curvature. European Association of Urology. 2014 doi: 10.1016/j.eururo.2012.05.040. [DOI] [PubMed] [Google Scholar]
- 15.Cappelleri JC, Rosen RC. The Sexual Health Inventory for Men (SHIM): a 5-year review of research and clinical experience. Int J Impot Res. 2005;17:307–19. doi: 10.1038/sj.ijir.3901327. [DOI] [PubMed] [Google Scholar]
- 16.Wessells H, Lue TF, McAninch JW. Penile length in the flaccid and erect states: guidelines for penile augmentation. J Urol. 1996;156:995–7. [PubMed] [Google Scholar]
- 17.Egydio PH, Lucon AM, Arap S. Treatment of Peyronie's disease by incomplete circumferential incision of the tunica albuginea and plaque with bovine pericardium graft. Urology. 2002;59:570–4. doi: 10.1016/s0090-4295(01)01651-x. [DOI] [PubMed] [Google Scholar]
- 18.Lentz AC, Carson CC., 3rd Peyronie's surgery: graft choices and outcomes. Curr Urol Rep. 2009;10:460–7. doi: 10.1007/s11934-009-0073-0. [DOI] [PubMed] [Google Scholar]
- 19.Carson CC, Chun JL. Peyronie's disease: surgical management: autologous materials. Int J Impot Res. 2002;14:329–35. doi: 10.1038/sj.ijir.3900864. [DOI] [PubMed] [Google Scholar]
- 20.Chun JL, McGregor A, Krishnan R, Carson CC. A comparison of dermal and cadaveric pericardial grafts in the modified Horton-Devine procedure for Peyronie's disease. J Urol. 2001;166:185–8. [PubMed] [Google Scholar]
- 21.Kovac JR, Brock GB. Surgical outcomes and patient satisfaction after dermal, pericardial, and small intestinal submucosal grafting for Peyronie's disease. J Sex Med. 2007;4:1500–8. doi: 10.1111/j.1743-6109.2007.00453.x. [DOI] [PubMed] [Google Scholar]
- 22.Leungwattanakij S, Bivalacqua TJ, Reddy S, Hellstrom WJ. Long-term follow-up on use of pericardial graft in the surgical management of Peyronie's disease. Int J Impot Res. 2001;13:183–6. doi: 10.1038/sj.ijir.3900676. [DOI] [PubMed] [Google Scholar]
- 23.Levine LA, Estrada CR. Human cadaveric pericardial graft for the surgical correction of Peyronie's disease. J Urol. 2003;170:2359–62. doi: 10.1097/01.ju.0000091102.10849.95. [DOI] [PubMed] [Google Scholar]
- 24.Usta MF, Bivalacqua TJ, Sanabria J, Koksal IT, Moparty K, et al. Patient and partner satisfaction and long-term results after surgical treatment for Peyronie's disease. Urology. 2003;62:105–9. doi: 10.1016/s0090-4295(03)00244-9. [DOI] [PubMed] [Google Scholar]
- 25.Hellstrom WJ, Reddy S. Application of pericardial graft in the surgical management of Peyronie's disease. J Urol. 2000;163:1445–7. [PubMed] [Google Scholar]


