Abstract
Background:
Strategic investments and policy directives of the Indian Government has demonstrated highest degree of political commitment for maternal and child health care.
Objectives:
To evaluate the impact of the rise in institutional deliveries in India on perinatal mortality.
Methods:
Hospital delivery rate and perinatal mortality rate (PNMR), reported by Sample Registration System, Registrar General of India, on a representative sample was used. The correlation between relative change in hospital deliveries and PNMR was examined.
Results:
In rural areas of India, hospital deliveries have increased during 2005–2013 from 24.4 to 69.7% and PNMR has declined from 40 to 28 per 1000 births. At the state level, there was significant correlation between the rise in hospital delivery rate and decline in PNMR (r 0.4, p 0.04).
Conclusions:
Decline in perinatal rates can be attributed to India's strategic initiatives in health policy and planning for increasing deliveries in hospitals.
Keywords: institutional delivery, quality of care, mortality, maternal health, perinatal, policy
Introduction
India is making concerted efforts to attain United Nation's Millennium Development Goals (MDG). Under-five-child mortality rate is declining at a much higher rate than the global average.[1] Strategic investments and policy directives that the Indian Government has taken in last decade demonstrates highest degree of political commitment for maternal and child health (MCH) care.[2] National Health Mission with its wide ranging and comprehensive strategies like Janani Shishu Suraksha Karyakram (JSSK) and Janani Suraksha Yojana (JSY) have led to an upsurge in institutional deliveries.[3]
Most of the under-five-child deaths occur during the early neonatal period and several babies also die during birthing process resulting in high stillbirth rate. More than 0.7 million neonatal deaths occur in India every year.[1] Perinatal mortality rate (PNMR) is a very sensitive indicator of the prenatal, intrapartum, and early newborn care. The early neonatal component of the PNMR responds relatively quickly to programmatic interventions like care during delivery. Childbirth in a health institute is a cost-effective intervention to reduce PNMR, as the health facilities equipped with supplies and trained staff can provide high-quality services. This study was carried out to evaluate the impact of the rise in institutional deliveries in India on perinatal mortality.
Methodology
Hospital delivery rate and perinatal mortality rate reported by the Sample Registration System operated by the Registrar General of India on a representative sample was used for this study.[4] The relative change in hospital deliveries and PNMR was calculated for rural areas in each of the major states of India from year 2005 to 2013. The correlation between relative change in hospital deliveries and PNMR was examined using statistical package for social sciences, version 17. The study had 80% power at 5% significance level for finding out association between relative change in hospital deliveries and relative change in PNMR. The regression line was fitted for the increase in hospital deliveries and decline in perinatal mortality rate for 20 major states. Coefficient of variation was also calculated for fitted line to assess the impact of hospital deliveries on the reduction in perinatal mortality.
Results
In most of the Indian States, hospital deliveries in rural areas have increased substantially from 2005 to 2013. Whereas most states had significant decline in PNMR; Assam, Haryana, and Karnataka have only a marginal decline, but Jharkhand has shown no decline in PNMR during the same period [Table 1].
Table 1.
Time trends in hospital delivery and perinatal mortality in rural areas of India
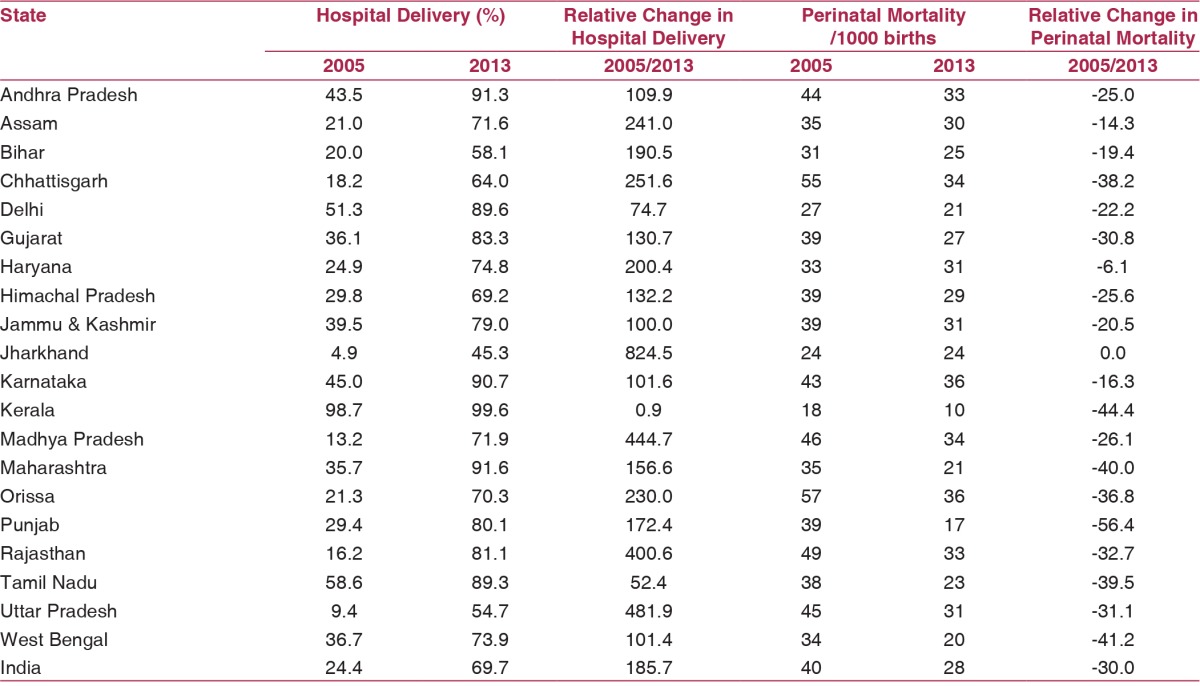
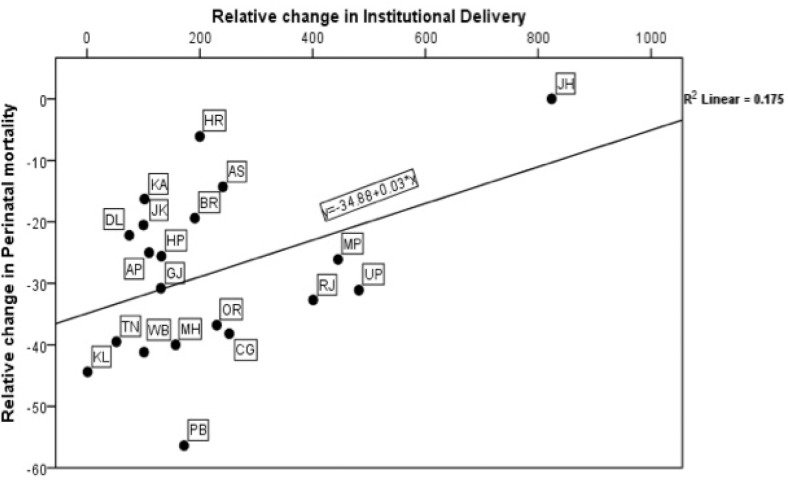
At the national level, in the rural areas, relative increase in hospital deliveries was 185.7% and relative decline in PNMR was 30%. The correlation between relative change in hospital delivery and PNMR in states was found to be significant (r = 0.42, 95% confidence interval; P = 0.04). A regression line fitted for relative change in perinatal mortality rate based on relative change in hospital deliveries revealed that 17.5% (R2 = 0.1751) of the variation in the decline of perinatal mortality could be explained by increase in hospital deliveries. [Figure 1].
Figure 1.
Relationship between relative change in institutional delivery with relative change in perinatal mortality in rural India, since 2005-2013. AP= Andhra Pradesh, AS=Assam, BR=Bihar, CG=Chhattisgarh, DL=Delhi, JH=Jharkhand, MP=Madhya Pradesh, OR=Orissa, RJ=Rajasthan, UP=Uttar Pradesh, HP=Himachal Pradesh, JK=Jammu & Kashmir, KA=Kamataka, KL=Kerala, TN=Tamil Nadu, GJ=Gujarat, HR=Haryana, MH=Maharashtra, PB=Punjab, WB=West Bengal
Discussion
An earlier analysis had revealed that a rise in hospital deliveries till 2008 did not have impact on perinatal mortality rates in rural areas of the country.[5] The unprecedented increase in hospital deliveries has occurred after 2008 and it has led to a significant decline in perinatal rates [Table 1], which can be attributed to India's strategic initiatives in health policy and planning for increasing deliveries in hospitals [Figure 1].
Most of the MCH schemes have prioritized health intervention to increase institutional care. The milestone achievement was the introduction of JSSK.[3] Free entitlements for women delivering in public health facilities, as well as for sick newborns and infants has been introduced, including free transport to health center, free diagnostics, free drugs, and free diet. These entitlements along with conditional cash transfers under JSY has led to a staggering 16.6 million women delivering in government and private accredited institutions every year.[3] Yet another e-initiative of web-enabled Mother and Child Tracking System has been introduced and more than 105 million pregnant women and children have been registered, who are regularly reached through call centers to ascertain utilization of health service delivery and to inquire about public satisfaction with the services.[3]
Moreover, facility-based newborn care has also been a novel strategic move by Government of India, wherein 548 special newborn care units, 1810 newborn stabilization units, and 14135 newborn care corners have been setup and many more are being added each year; and more than 470 dedicated MCH wings have been approved from 2011 to 2014.[1] More than 0.13 million health care providers have been trained in essential newborn care including resuscitation under Navjaat Shishu Suraksha Karyakram. More than 6,300 health personnel have been trained in facility-based newborn care to enrich their cognitive knowledge and to build psychomotor skills of the medical officers and staff nurses posted in special newborn care units in India.[1]
Large variations exist in institutional delivery rate and PNMR between states [Table 1]. Maternal and child death reviews, tracking of all deaths in the hospitals and simultaneously expanding it to community in which most births occur will help in sharper understanding of the preventable causes and their management. To ensure equitable health care and to bring about sharper improvements in health outcomes, a systematic effort to effectively address the intrastate disparities in health outcomes has been undertaken. At least 25% of districts in each state, 184 poorest performing districts all over the country, have been identified based on composite index of selected health indicators as High Priority Districts wherein the poorest, most vulnerable, and marginalized populations reside. These have been identified for intensification interventions through harmonized partner support and increased financial allocation.[3]
Indian government has increased investment in the health sector; however, there is a need to develop good quality health services. Various Common Review Missions and Joint Review Missions of National Rural Health have revealed that quality of care at most of delivery points in the country is a cause of concern.[6] Monitoring and supervision, which is an essential component of the interventions, needs improvement. Despite the fact that quality assurance cells are key component for quality service provision, these have not yet been constituted in many states.
To conclude, strategic investments in the rural areas of India have led to a surge in hospital deliveries, which has resulted in a significant decline in perinatal mortality during the last nearly a decade, but PNMR is still high (28/1000 births). For improved outcomes it is imperative that the strategies should aim to improve quality of antenatal and intrapartum care with timely referral. One of the major prerequisite for achieving the MDG-4 would be quality service provision.
Financial support and sponsorship
Nil
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The author(s) of the article are solely responsible for the content thereof. The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of any agency.
References
- 1.India Newborn Action Plan. New Delhi: Ministry of Health and Family Welfare, Government of India; 2014. [Last accessed on 2016 Feb 19]. Available from http://www.newbornwhocc.org/INAP_Final.pdf . [Google Scholar]
- 2.A Strategic Approach to Reproductive, Maternal, Newborn, Child and Adolescent Health (RMNCH+A) in India. New Delhi: Ministry of Health and Family Welfare, Government of India; 2013. [Last accessed on 2015 Feb 19]. Available from http://rmncha.in/upload/Content/101.pdf . [Google Scholar]
- 3.Five Years Achievements and New Initiatives. New Delhi: Ministry of Health and Family Welfare, Government of India; 2014. [Last accessed on 2015 Feb 19]. Available from http://nrhm.gov.in/images/pdf/media/publication/five-years-of-nhm-2009-2014/5_years_nhm_final.pdf . [Google Scholar]
- 4.Statistical Report 2013. New Delhi: office of Registrar General, India, Ministry of Home Affairs, Government of India; 2014. [Last accessed on 2016 Feb 22]. Sample Registration System. Available from http://www.censusindia.gov.in/vital_statistics/SRS_Reports_2013.html . [Google Scholar]
- 5.Singh SK, Kaur R, Gupta M, Kumar R. Impact of National Rural Health Mission on Perinatal Mortality in Rural India. Indian Pediatr. 2012;49:136–38. doi: 10.1007/s13312-012-0022-8. [DOI] [PubMed] [Google Scholar]
- 6.Common Review Mission Reports. New Delhi: Ministry of Health and Family Welfare, Government of India; 2015. [Last accessed on 2015 Feb 18]. Available from http://nrhm.gov.in/monitoring/common-review-mission.html . [Google Scholar]