Abstract
Background:
In India, Janani Shishu Suraksha Karyakaram (JSSK) was launched in the year 2011 to assure cashless institutional delivery to pregnant women, including free transport and diet.
Objective:
To assess the impact of JSSK on institutional delivery.
Materials and Methods:
A record review was done at the primary health care facility in Faridabad district of Haryana from August 2010 to March 2013. Focus group discussion/ informal interviews were carried out to get an insight about various factors determining use / non-use of health facilities for delivery.
Results:
Institutional delivery increased by almost 2.7 times (197 Vs 537) after launch of JSSK (p < 0.001). For institutional deliveries, the most important facilitator as well as barrier was identified as ambulance service under JSSK and pressure by elders in the family respectively.
Conclusions:
JSSK scheme had a positive impact on institutional deliveries. It should be supported with targeted intervention designed to facilitate appropriate decision-making at family level in order to address barriers to institutional delivery.
Keywords: Institutional delivery, JSSK, primary care, rural India
Introduction
Promotion of Institutional delivery is one of the most important interventions in India with a high maternal and neonatal mortality rate.[1,2] A Nation-wide survey reports 73% institutional deliveries in the year 2009.[3] Important reasons for home deliveries documented were lack of felt need for delivery at health facility, and high cost of the hospital services in India.[4] Factors affecting care seeking include economic status, parental education, high out of pocket (OOP) expenditure in hospitalization, and lack of or unaffordable transport facilities.[5,6,7]
Conditional cash transfer scheme, named Janani Suraksha Yojana (JSY) was introduced in India in the year 2005, with a strategy is to link cash assistance to institutional delivery.[5] Due to JSY, institutional deliveries across the country have increased but with a few limitations such as high OOP expenditure especially for purchase of the drugs, and transport, incurred by families.[6]
In the view of these limitations, Government of India introduced Janani Shishu Suraksha Karyakram (JSSK) scheme in June 2011. Under this scheme; delivery, caesarian section, drugs and consumables, diagnostics, diet during stay (up to 3 days for normal delivery and 7 days for caesarian section), provision of blood, and transport between home to health institution is provided free of cost. The cash less service benefits are also extended to the newborn till 30 days after birth.[7] In the state of Haryana, JSSK scheme was launched in September 2011.[8] This study deals with impact assessment of JSSK on utilization of delivery services at a Primary Health Centre, in Faridabad district of Haryana.
Materials and Methods
This was a facility and community based cross-sectional study, consisting of both quantitative and qualitative components, carried out at the Primary Health Centre, Chhainsa. The study area was a part of Comprehensive Rural Health Services project, Ballabgarh, of All India Institute of Medical Sciences; New Delhi.[9] Study facility provides round the clock delivery services to catchment area consisting of approximately 47,000 rural inhabitants (year 2012). In the study area, JSSK scheme was launched in December 2011. Comparison was made for a period of 16 months before (August 2010-November 2011) and after the implementation of JSSK in the study area (December 2011-March 2013). We extracted data of all deliveries conducted in 32 months from the hospital records in the format of Microsoft excel. Information about various socio-demographic factors and distance between woman's village and study facility was also retrieved from these records. The proportions and means were compared through chi-square and t-test respectively using STATA 12.1.
Focus group discussions (FGD) and informal discussions were carried out to get insight about factors determining utilization of JSSK services and place of delivery. Two FGDs each were carried out among women who had delivered at the hospital, and at home during the period of January 2013-March 2013. FGDs were conducted in two villages, one within five kilometer range- Chhainsa and another which was more than five kilometers away from the study facility- Atali. FGD guide was prepared consisting of domains such as reason for choice of place of delivery, community perception about various services under JSSK scheme; suggestions for improvement of delivery services. Qualitative data was analyzed manually by free listing of responses, domain identification followed by coding of responses. Qualitative data was triangulated with quantitative data to make an assessment of reality by synthesizing multiple sources of information.
Results
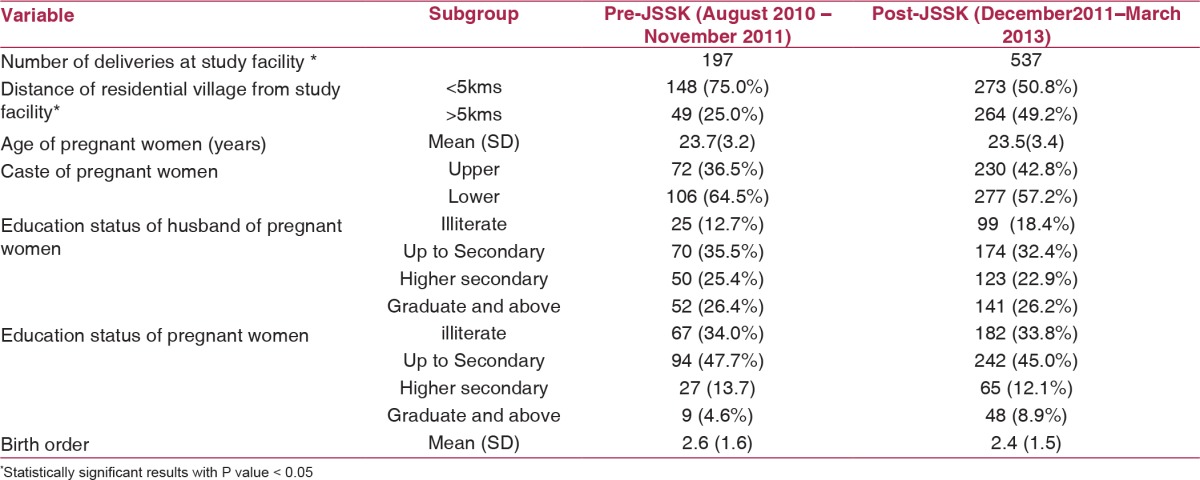
During the study period (August 2010-March 2013), a total of 734 deliveries took place at the study facility. Out of these, 197 (26.8%) took place before and 537 (73.2%) after implementation of JSSK (1st December 2011). This amounted to 2.7 times increase in the number of deliveries across the study period and was statistically significant (p < 0.001). Differences in socio-demographic characteristics among those who delivered before and after the launch of the scheme were statistically non-significant, except for place of residence of women (> 5 kilometers from study facility) (p value < 0.001, df = 1) [Table 1].
Table 1.
Baseline characteristics of study subjects, before and after the launch of JSSK
Qualitative study results
FGD conducted among women who had a hospital delivery revealed that difficulty in maintaining cleanliness at home during childbirth was identified as a reason for hospital delivery, and not availability of ambulance service.
“To maintain purity and hygiene at home we prefer deliveries in hospital” (A 20 years old respondent)
Respondents came to know about free diet services only during their hospital stay. However due to the cultural norm, a few women did not take solid foods for up to 6-11 days post-delivery.
FGD and Informal discussions among women who had hospital delivery in a village > 5 kilometers away from study facility revealed accessibility and round the clock availability of ambulance was the most important facilitator for institutional delivery. Cordial behavior of ambulance staff, punctuality of ambulance services and availability of cashless services under JSSK scheme were identified as facilitator factors too. Ambulance service also ensured timely referral in emergency situations.
“At the time of deliveries, we tell ASHA (village level volunteer) and they call ambulance any time we can go” (A 20 years old respondent)
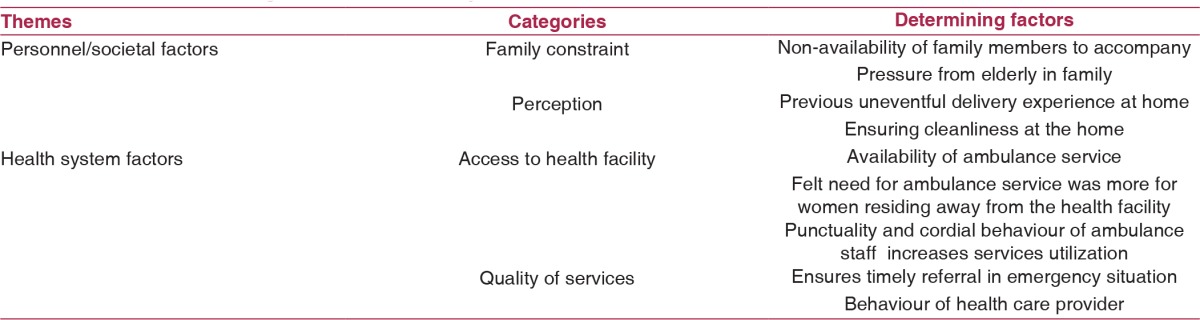
Harsh behavior by health care providers during earlier childbirth in hospitals, or non-availability of a family member who could accompany the pregnant women to health facility, traditional practices, assurance from local birth attendant (dai) for normal delivery at home, family member's preference for home delivery, and previous experience of uneventful home delivery were the common reasons for home delivery reported by respondents. Themes, categories and subcategories derived from qualitative study about factors determining utilization services under JSSK are described in Table 2.
Table 2.
Factors determining institutional delivery under JSSK
Discussion
We used both quantitative and qualitative data to document the impact of services under JSSK on institutional delivery at the primary care level. More than double the increase in number of deliveries at primary care level after implementation of JSSK scheme was observed in spite of no significant development either in human resources or in infrastructure up-gradation at the study facility. Hence, the observed increase in institutional deliveries could be attributed to additional services provided under JSSK. Increase in institutional deliveries was contributed proportionately more by women coming from villages away from the study facility. Amudhan S et al documented that service related interventions were more effective in the population primed by demand side intervention.[10] JSY scheme helped to generate demand in the community for institutional delivery since its launch in the year 2006.[11] Under JSSK, services were provided that contributed to further increase in institutional delivery in population already primed by JSY scheme in the study area.
Qualitative data suggested that the utilization of cash less ambulance service was dependent on felt need of the community. Several studies[12,13,14,15,16,17,18,19,20,21] have documented that lack of transport facilities is a barrier to institutional delivery as well as a reason for maternal and neonatal mortality.
Studies evaluating the demand side intervention of “JSY” revealed that it offered only partial financial risk protection and induced new OOP expenditure due to hospital delivery.[14,22,23] Present study demonstrated the increase in utilization of cash less delivery services under JSSK which might have led to a decrease in OOP expenditure.
Previous studies[24,25] documented family traditions, financial constraints, elder's decisions, cost of hospital services, lack of transport facilities, rude behaviour of the healthcare personnel as barriers to availing healthcare facilities similar to the findings of present study. Incorporation of work ethics and stress management in situations of overburden at the work place should be incorporated in the training module of health care providers.
Impact of increased population awareness, improved literacy and socio-economic status on institutional delivery cannot be ruled out. However, factors like age, education, birth order were comparable across both groups in this study. Hence, it seems unlikely that all these factors were responsible for impact of JSSK. The study facility, which was a PHC, functioned as a 24 x 7 delivery facility with adequate health staff. Assured availability of trained health care providers might have influenced patients to opt for institutional delivery. Training of manpower such as staff nurses and medical officers at the study facility was done as a part of routine human resource development strategy under National Rural Health Mission (NRHM). Results of this study could be generalized to those primary care facilities that have adequate health infrastructure and manpower. Impact of other ongoing schemes under NRHM such as JSY, introduction of ASHA could also have contributed to increase in institutional deliveries. It needs to be studied further in order to quantify the impact of JSY and JSSK separately with robust study design.
We observed that services through JSSK in adequate health infrastructure situation could bring pregnant women to the public health facility for child-birth. Out of all services, Ambulance service was identified as most important facilitator for reducing access barriers. Increase in institutional deliveries at primary care level through JSSK will not only decrease the OOP of the population, but also help build faith in the government health facilities. Nonetheless, there is need to increase awareness in all sections of the community through strong media campaigns covering all aspects of JSSK to get maximum output of the scheme.
Financial support and sponsorship
Nil
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Ethical approval for the study was obtained from the Ethics Committee of All India Institute of Medical Sciences, New Delhi.
References
- 1.Rai SK, Dasgupta R, Das MK, Singh S, Devi R, Arora NK. Determinants of utilization of services under MMJSSA scheme in Jharkhand ‘Client Perspective’: A qualitative study in a low performing state of India. Indian J Public Health. 2011;55:252–9. doi: 10.4103/0019-557X.92400. [DOI] [PubMed] [Google Scholar]
- 2.Registrar General of India Special Bulletin on Maternal Mortality in India 2007-09. [Last accessed on 2013 May 13]. http://www.censusindia.gov.in/vital_statistics/SRS_Bulletins/Final-MMR%20Bulletin-2007-09_070711.pdf .
- 3.Unicef Coverage Evaluation Survey. 2009. [Last accessed on 2013 May 13]. http://www.unicef.org/india/National_Fact_Sheet_CES_2009.pdf .
- 4.International Institute for Population Sciences (IIPS) and Macro International National Family Health Survey (NFHS-3) India, 2005-06.
- 5.Ministry of Health Family Welfare Janani Suraksha Yojana Guidelines for implementation. [Last accessed on 2013 May 13]. http://www.mohfw.nic.in/NRHM/RCH/guidelines/JSY_guidelines_09_06.pdf .
- 6.Gopalan SS, Durairaj V. Addressing maternal healthcare through demand side financial incentives: experience of Janani Suraksha Yojana program in India. BMC Health Serv Res. 2012;12:319-. doi: 10.1186/1472-6963-12-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Press Information Bureau, GOI. Health Ministry Launches Janani-Shishu Suraksha Karyakram JSSK to benefit more than one Crore Pregnant Women and Newborns. [Last accessed on 2013 May 13]. http://pib.nic.in/newsite/erelease.aspx?relid=72433 .
- 8.JSSK Government Order Dated 19_11_2011.pdf. [Last accessed on May 13, 2013]. http://www.nrhmharyana.org/Writereaddata/userfiles/file/PDFs/JSSK%20instructions/JSSK%20Govt_%20Order%20Dated%2019_11_2011.pdf .
- 9.Kant S, Misra P, Gupta S, Goswami K, Krishnan A, Nongkynrih B, et al. Cohort Profile: The Ballabgarh Health and Demographic Surveillance System (CRHSP-AIIMS) Int J Epidemiol. 2013;42:758–68. doi: 10.1093/ije/dyt055. [DOI] [PubMed] [Google Scholar]
- 10.Amudhan S, Mani K, Rai SK, Pandav CS, Krishnan A. Effectiveness of demand and supply side interventions in promoting institutional deliveries- a quasi-experimental trial from rural north India. Int J Epidemiol. 2013;42:769–80. doi: 10.1093/ije/dyt071. [DOI] [PubMed] [Google Scholar]
- 11.Lim SS, Dandona L, Hoisington JA, James SL, Hogan MC, Gakidou E. India's Janani Suraksha Yojana, a conditional cash transfer programme to increase births in health facilities: An impact evaluation. Lancet. 2010;375:2009–23. doi: 10.1016/S0140-6736(10)60744-1. [DOI] [PubMed] [Google Scholar]
- 12.Das S, Bapat U, More NS, Chordhekar L, Joshi W, Osrin D. Prospective study of determinants and costs of home births in Mumbai slums. BMC Pregnancy Childbirth. 2010;10:38. doi: 10.1186/1471-2393-10-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ved R, Sundararaman T, Gupta G, Rana G. Program evaluation of the Janani Suraksha Yojna. BMC Proc. 2012;6:(Suppl 5):O15. [Google Scholar]
- 14.Costa AD, Patil R, Kushwah SS, Diwan VK. Financial incentives to influence maternal mortality in a low-income setting: making available ‘money to transport’- experiences from Amarpatan, India. Glob Health Action. 2009;18:2. doi: 10.3402/gha.v2i0.1866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hussein J, Kanguru L, Astin M, Munjanja S. The effectiveness of emergency obstetric referral interventions in developing country settings: A systematic review. PLoS Med. 2012:9. doi: 10.1371/journal.pmed.1001264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iyengar K, Iyengar SD, Suhalka V, Dashora K. Pregnancy-related deaths in Rural Rajasthan, India: Exploring causes, context, and care-seeking through verbal autopsy. J Health Popul Nutr. 2009;27:293–302. doi: 10.3329/jhpn.v27i2.3370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Upadhyay RP, Rai SK, Krishnan A. Using three delays model to understand the social factors responsible for neonatal deaths in rural Haryana, India. J Trop Pediatr. 2013;59:100–5. doi: 10.1093/tropej/fms060. [DOI] [PubMed] [Google Scholar]
- 18.Tiwari B. Role of National Rural Health Mission in promoting Institutional Delivery Services in Rural Uttar Pradesh, India: An assessment of ‘Janani Suraksha Yojana’. [Last accessed on 2013 May 13]. http://paa2013.princeton.edu/papers/132285 .
- 19.Kumar S, Dansereau E, Murray C. Geographic constraint to Institutional Delivery in Rural India: An instrumental variable approach. [Last accessed on 2013 May 13]. Available from: http://paa2013.princeton.edu/papers/132477 .
- 20.Titaley C, Hunter CL, Dibley MJ, Heywood P. Why do some women still prefer traditional birth attendants and home delivery? A qualitative study on delivery care services in West Java Province, Indonesia. BMC Pregnancy Childbirth. 2010;10:43. doi: 10.1186/1471-2393-10-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ekirapa-Kiracho E, Waiswa P, Rahman MH, Makumpi F, Kiwanuka N, Okui O. Increasing access to institutional deliveries using demand and supply side incentives: Early results from a quasi-experimental study. BMC. Int Health Hum Rights. 2011;11:S11. doi: 10.1186/1472-698X-11-S1-S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Modugu HR, Kumar M, Kumar A, Millett C. State and socio-demographic group variation in out-of-pocket expenditure, borrowings and Janani Suraksha Yojana (JSY) programme use for birth deliveries in India. BMC Public Health. 2012;12:1048. doi: 10.1186/1471-2458-12-1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ved R, Sundararaman T, Gupta G, Rana G. Program evaluation of the Janani Suraksha Yojna. BMC Proc. 2012;6:O15. [Google Scholar]
- 24.Khan Z, Mehnaz S, Ansari MA, Khalique N, Siddiqui AR. Existing practices and barriers to avail of maternal healthcare services in two slums of Aligarh. HealthPopul Perspect Issues. 2009;32:113–23. [Google Scholar]
- 25.The Population council Increasing institutional delivery and access to emergency obstetric care services in rural Uttar Pradesh: Implications for behavior change communication. [Last accessed on 2013 May 13]. http://www.popcouncil.org/pdfs/2010India_PolicyBrief01.pdf .


