Abstract
We systematically reviewed and compared the clinical outcomes of thoracoscopic sympathectomy (TS) at different denervation levels for palmar hyperhidrosis. We searched PubMed, Ovid MEDLINE, EMBASE, Web of Science, ScienceDirect, the Cochrane Library, Scopus and Google Scholar for relevant studies published during 1990–2016. Symptom resolution, patient satisfaction, compensatory sweating (CS), recurrence, dry hands and gustatory sweating were assessed. We selected 13 studies from 2228 for the final analysis. A comparison of T2 vs. T3 TS revealed that T3 TS reduced the risk of CS (95% confidence interval [CI]: 1.36–3.19, p = 0.0007) and moderate-to-severe CS (95% CI: 2.14–7.87, p < 0.0001). No significant differences were found in patient satisfaction, symptom resolution, and incidence of dry hands and gustatory sweating. A comparison of T3 vs. T4 TS revealed that T4 TS reduced the risk of CS (95% CI: 2.87–9.53, p < 0.00001), moderate-to-severe CS (95% CI: 2.54–5.83, p < 0.00001), dry hands (95% CI: 4.07–18.13, p < 0.00001) and gustatory sweating (95% CI: 1.53–7.32, p < 0.003), and improved patient satisfaction. No significant differences were found in symptom resolution and recurrence. T4 TS appears to be more useful than T3 or T2 TS for PH.
Introduction
Palmar hyperhidrosis (PH) is a condition marked by excessive perspiration of hands beyond physiologic need, and is aggravated during periods of stress and anxiety. Thoracoscopic sympathectomy (TS) has become the standard surgical treatment for palmar hyperhidrosis (PH) owing to its association with minimal trauma and low morbidity rates1, 2. Conventional surgery to transect the sympathetic chain at the T2–T3 or T2–T4 levels can improve the symptom of PH perfectly well. However, this type of surgery is associated with high incidence rates of complications such as compensatory sweating (CS) and dry hands3–5. Various methods have been tried to decrease the incidence of complications after TS, and limitation of the extent of surgical dissection has been found to be the key to achieving this goal. Several authors have performed TS at a single level and achieved a better curative effect (similar resolution of symptoms and lower incidence of CS) than that achieved with TS at multiple levels6–8. With the deepening of our understanding of TS, single-level surgeries, especially at the T3 or T4 level, became increasingly common. Although TS at the T4 level has been recommended for the treatment of PH under the Lin-Telaranta classification, the optimal level for TS has been the subject of intense debate among thoracic surgeons, possibly due to a lack of large-scale clinical research in this area9. In an attempt to resolve this issue and optimize surgical procedures, we performed a systematic review and meta-analysis of clinical trials investigating TS at the T2, T3 or T4 level for the treatment of PH.
Materials and Methods
Search strategy
On July 10, 2016, we conducted an extensive literature search to identify all relevant studies published from January 1990 to July 2016 according to The Preferred Reporting Items for Systematic Reviews and Meta-Analyses. The following databases were scanned: PubMed, Ovid MEDLINE, EMBASE, Web of Science, ScienceDirect, the Cochrane Library, Scopus and Google Scholar. The MeSH terms used included “hyperhidrosis” and “sympathectomy or sympathicotomy”. We also searched the reference lists of the included articles to identify additional studies.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (1) studies published in English, (2) studies involving patients with either isolated PH or PH combined with hyperhidrosis of other regions, (3) studies comparing the clinical outcomes of TS at different single levels (T2 vs. T3 or T3 vs. T4), (4) studies including ≥10 patients in each group and (5) the most recent study in the case of duplication of data in more than one article.
Reviews without original data, case reports, meta-analyses, letters, expert opinions and animal studies were excluded.
Data extraction
Data extraction was accomplished by two observers independently, using a standardized Excel form. Any disagreement was resolved the help of a third investigator. The recorded data included the following: first author, year of publication, study design, denervation level, number of patients per group, resolution of symptoms, number of satisfied patients, rate of postoperative complications (recurrence, dry hands and gustatory sweating) and CS (incidence and severity).
Quality assessment of included studies
Methodological quality was assessed using the Newcastle-Ottawa Scale (NOS) for non-randomized studies and the Jadad scale for randomized controlled trials (RCTs). The NOS (9 points) contained questions for three main items: selection, comparability and exposure. Studies that scored 8–9 points were considered to be of high quality, while those that scored 6–7 points were considered to be of medium quality10. The Jadad scale (5 points) evaluates the quality of studies by analysing three items: randomization, masking and accountability of all patients (withdrawals and dropouts). Studies that scored ≥3 points were considered to be of high quality11.
Statistical analysis
We designed two comparisons (T2 vs. T3 and T3 vs. T4) to identify the optimal level of TS. Meta-analysis was conducted using Review Manager 5.3 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark) and STATA 12.0 (StataCorp. LP, College Station, Texas, USA). A p-value < 0.05 suggested statistical significance. Between-group differences were compared using analysis of variance in the case of continuous variables or pooled relative risk with 95% confidence interval (CI) in the case of categorical variables. We used the I 2 and Cochran Q statistics to evaluate the between-study heterogeneity. A random-effects model was adopted when the heterogeneity was significant (p ≤ 0.10 and I 2 > 50%); otherwise, a fixed-effects model was used. The Egger test based on CS data was used to assess potential publication bias.
Results
Search results and quality assessment
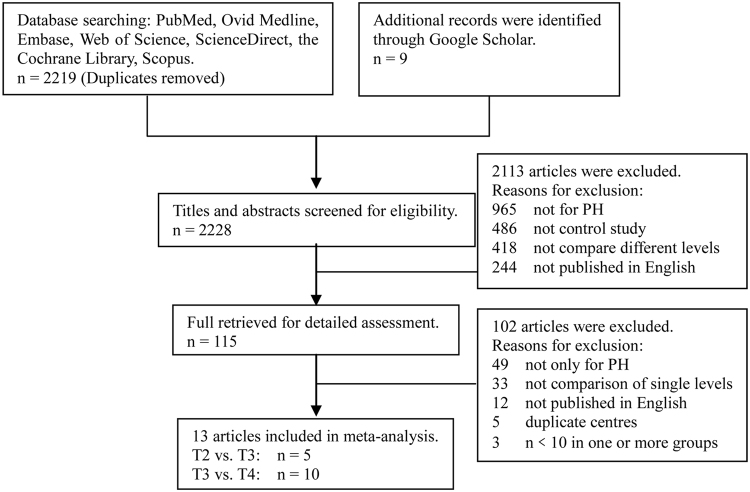
We initially identified 2228 publications from the database and reference-list searches. From these, 13 studies with 1577 patients (261 in the T2 group, 723 in the T3 group and 593 in the T4 group) were selected for final analysis (Fig. 1). Among the 13 studies, 8 were retrospective studies and 5 were RCTs. Quality assessments using the NOS and Jadad scales showed that 10 studies were of good quality, and the other 3 were of medium quality. The baseline characteristics of the included studies and the main evaluation indexes are shown in Table 1.
Figure 1.
Flow diagram of screened and included papers.
Table 1.
Summary of the 13 studies included in the present meta-analysis.
| Study | Levels | NO. of Patients (n) | Resolution (n) | Satisfied cases (n) | CH (n) | Moderate-severe CH (n) | Over dry hands (n) | Gustatory sweating (n) | Recurrence (n) | Design | Quality (score) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2004 | Lee13 | T2 | 64 | 60 | 50 | 43 | 26 | Retrospective | 8 | |||
| T3 | 83 | 68 | 57 | 36 | 9 | |||||||
| 2007 | Yang14 | T3 | 78 | 78 | 55 | 18 | 0 | RCT | 3 | |||
| T4 | 85 | 85 | 38 | 6 | 0 | |||||||
| 2007 | Chang15 | T2 | 86 | 78 | 80 | 31 | 5 | 22 | Retrospective | 7 | ||
| T3 | 78 | 75 | 72 | 31 | 18 | 6 | ||||||
| T4 | 70 | 70 | 56 | 6 | 8 | 16 | ||||||
| 2008 | Wolosker16 | T3 | 35 | 34 | 35 | 24 | Retrospective | 8 | ||||
| T4 | 35 | 33 | 25 | 3 | ||||||||
| 2008 | Mahdy17 | T2 | 20 | 12 | 12 | 7 | 6 | 2 | Retrospective | 9 | ||
| T3 | 20 | 15 | 9 | 4 | 5 | 1 | ||||||
| T4 | 20 | 20 | 2 | 0 | 1 | 0 | ||||||
| 2009 | Liu18 | T3 | 68 | 68 | 68 | 48 | 9 | 8 | RCT | 3 | ||
| T4 | 73 | 73 | 73 | 39 | 2 | 1 | ||||||
| 2009 | Yazbek19 | T2 | 30 | 30 | 30 | 10 | RCT | 4 | ||||
| T3 | 30 | 29 | 29 | 3 | ||||||||
| 2010 | Kim20 | T3 | 56 | 56 | 55 | 46 | 6 | 3 | 5 | 1 | Retrospective | 7 |
| T4 | 63 | 63 | 61 | 11 | 2 | 0 | 0 | 2 | ||||
| 2011 | Ishy21 | T3 | 20 | 20 | 20 | 1 | RCT | 4 | ||||
| T4 | 20 | 20 | 15 | 1 | ||||||||
| 2011 | Baumgartner22 | T2 | 61 | 58 | 61 | 40 | 4 | 3 | RCT | 4 | ||
| T3 | 60 | 57 | 59 | 29 | 3 | 3 | ||||||
| 2012 | Kavakli23 | T3 | 43 | 8 | 1 | Retrospective | 6 | |||||
| T4 | 46 | 0 | 2 | |||||||||
| 2014 | Ellatif24 | T3 | 129 | 129 | 128 | 96 | 28 | 11 | 1 | Retrospective | 8 | |
| T4 | 145 | 145 | 143 | 41 | 17 | 1 | 2 | |||||
| 2016 | Joo25 | T3 | 23 | 17 | 17 | 11 | 8 | Retrospective | 8 | |||
| T4 | 36 | 35 | 22 | 5 | 9 |
Main analysis
We comprehensively evaluated the curative effects of TS in two aspects: (1) resolution of symptoms and patient satisfaction and (2) occurrence of postoperative complications (CS, moderate-to-severe CS, recurrence, dry hands and gustatory sweating).
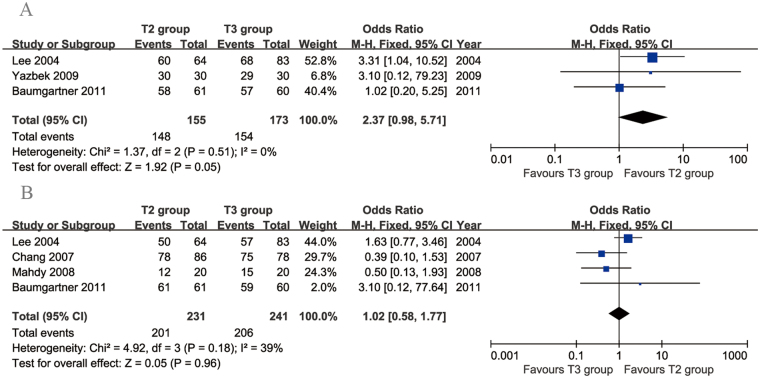
T2 versus T3
We identified 5 articles that compared T2 vs. T3 TS. They included 261 patients in the T2 group and 271 patients in the T3 group. Data on the resolution of symptoms were available in 3 articles. There was no evidence of heterogeneity among these studies (p = 0.51, I 2 = 0%). No significant difference was found in the resolution of symptoms between the two groups (95% CI: 0.98 to 5.71, p = 0.05; Fig. 2A). Four articles compared patient satisfaction between the two groups. The heterogeneity among these studies was acceptable (p = 0.18, I 2 = 39%). No significant difference in the patient satisfaction rate was found between the two groups (95% CI: 0.58 to 1.77, p = 0.96; Fig. 2B).
Figure 2.
Forest plots for resolution of symptoms (A) and patient satisfaction (B) in the T2 and T3 groups.
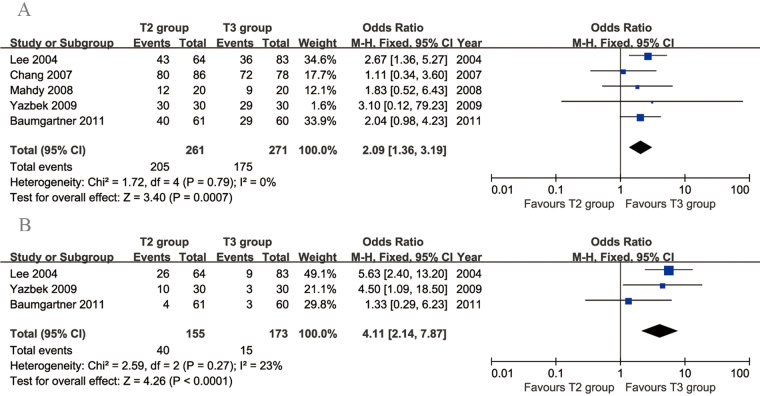
Five articles compared the rate of CS. There was no evidence of heterogeneity among these studies (p = 0.79, I 2 = 0%). The incidence of CS was significantly lower in the T3 group than in the T2 group (95% CI: 1.36 to 3.19, p = 0.0007; Fig. 3A). Three articles compared the rate of moderate-to-severe CS. The heterogeneity among these studies was acceptable (p = 0.27, I 2 = 23%). The incidence of moderate-to-severe CS was significantly lower in the T3 group than in the T2 group (95% CI: 2.14 to 7.87, p < 0.0001; Fig. 3B).
Figure 3.
Forest plots for compensatory sweating (A) and moderate-to-severe compensatory sweating (B) in the T2 and T3 groups.
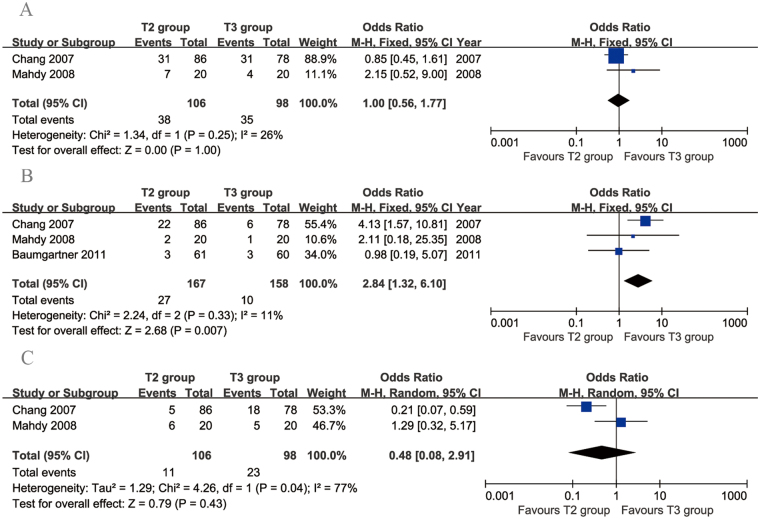
Two articles compared the rate of dry hands. The heterogeneity between these studies was acceptable (p = 0.25, I 2 = 26%). No significant difference was found in the rate of dry hands between the two groups (95% CI: 0.56 to 1.77, p = 1.00; Fig. 4A). Three articles compared recurrence rates between T2 and T3 TS. The heterogeneity among these studies was acceptable (p = 0.33, I 2 = 11%). Significantly more recurrences were found in the T2 group than in the T3 group (95% CI: 1.32 to 6.10, p = 0.007; Fig. 4B). Two articles compared the rate of gustatory sweating. No significant difference in gustatory sweating was found between the two groups (95% CI: 0.08 to 2.91, p = 0.43), but there was significant heterogeneity across the studies (p = 0.04, I 2 = 77%; Fig. 4C).
Figure 4.
Forest plots for other postoperative complications in the T2 and T3 groups. (A) Recurrence, (B) dry hands and (C) gustatory sweating.
T3 versus T4
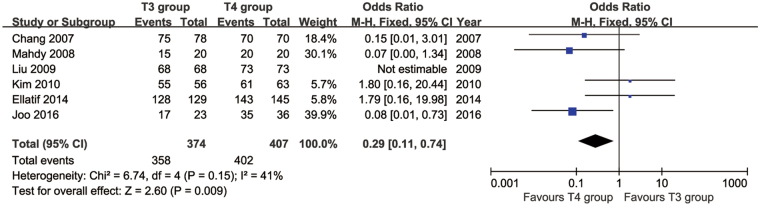
We identified 10 articles that compared T3 vs. T4 TS. These studies involved a total of 550 patients in the T3 group and 593 patients in the T4 group. The resolution of symptoms was investigated in 6 studies. Of these, five studies reported that the symptom of PH was resolved in all patients in both groups. Only one study reported that there was no significant difference between the two groups (34/35 vs. 33/35, p = 0.56). Satisfaction rates were compared in six papers. The heterogeneity between these studies was acceptable (p = 0.15, I 2 = 41%). Significantly higher satisfaction rates were found in the T4 group than in the T3 group (95% CI: 0.11 to 0.74, p = 0.009; Fig. 5).
Figure 5.
Forest plot for patient satisfaction in the T3 and T4 groups.
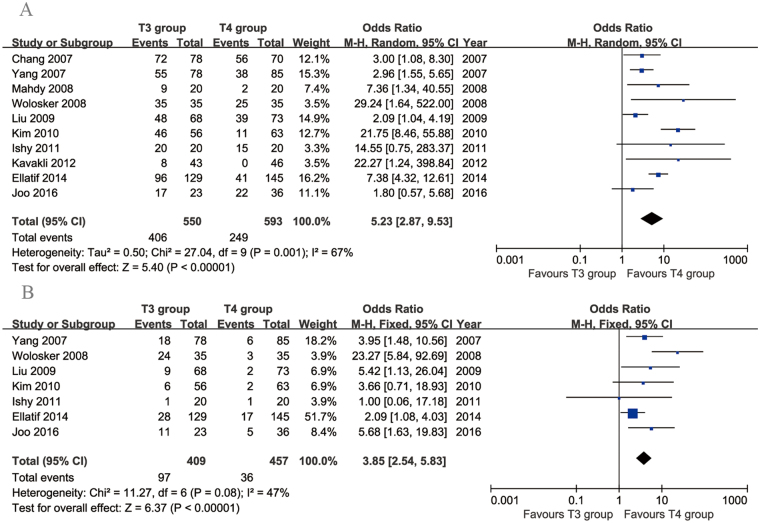
Ten articles compared CS rates. The incidence of CS was significantly lower in the T4 group than in the T3 group (95% CI: 2.87 to 9.53, p < 0.00001), with significant heterogeneity across the studies (p = 0.001, I 2 = 67%; Fig. 6A). Seven articles compared the rates of moderate-to-severe CS. This rate was significantly lower in the T4 group than in the T3 group (95% CI: 2.54 to 5.83, p < 0.00001), with acceptable heterogeneity across the studies (p = 0.08, I 2 = 47%; Fig. 6B).
Figure 6.
Forest plots for compensatory sweating (A) and moderate-to-severe compensatory sweating (B) in the T3 and T4 groups.
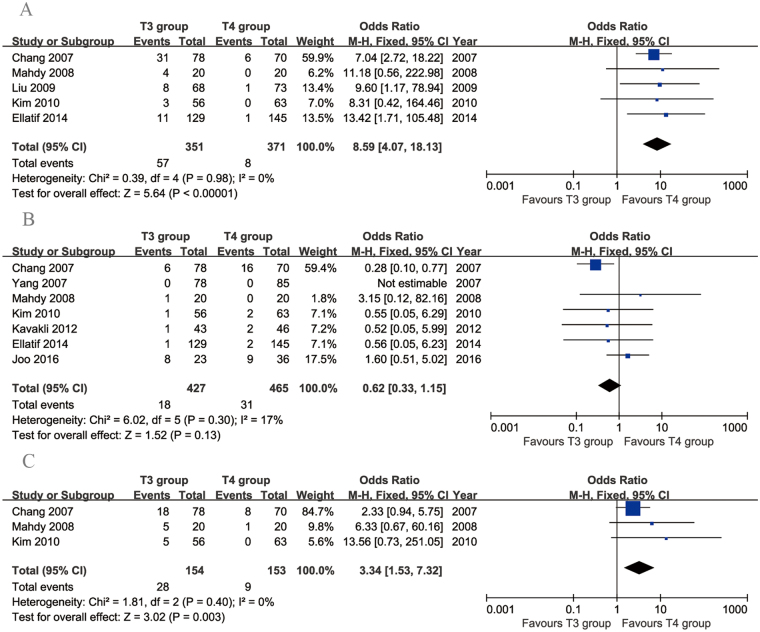
Five articles compared the rates of dry hands. There was no evidence of heterogeneity among these studies (p = 0.98, I 2 = 0%). The incidence of dry hands was significantly higher in the T3 group than in the T4 group (95% CI: 4.07 to 18.13, p < 0.00001; Fig. 7A). Seven articles compared recurrence rates between T3 and T4 TS. The heterogeneity among these studies was acceptable (p = 0.30, I 2 = 17%). No significant difference in recurrence rates was found between the two groups (95% CI: 0.33 to 1.15, p = 0.13; Fig. 7B). Three articles investigated the incidence of gustatory sweating. There was no evidence of heterogeneity among these studies (p = 0.40, I 2 = 0%). The incidence of gustatory sweating was higher in the T3 group than in the T4 group (95% CI: 1.53 to 7.32, p < 0.003; Fig. 7C).
Figure 7.
Forest plots for other postoperative complications in the T3 and T4 groups. (A) Recurrence, (B) dry hands and (C) gustatory sweating.
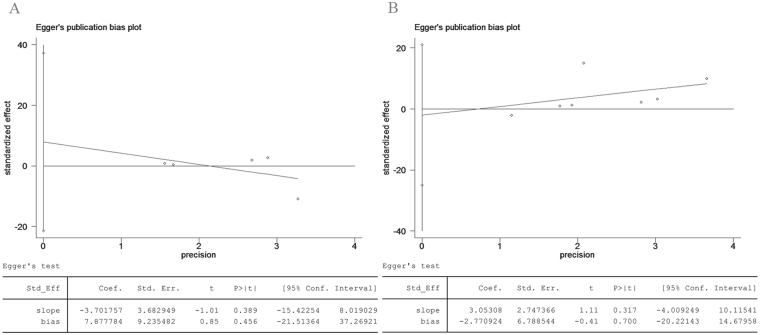
Publication bias
This study involved two comparisons (T2 vs. T3 and T3 vs. T4), whose publication biases were assessed using the Egger test based on the data for CS. The results showed that there was no significant publication bias (T2 vs. T3, p = 0.456; T3 vs. T4, p = 0.700; Fig. 8).
Figure 8.
Egger test for compensatory sweating, suggesting no publication bias in the pooled analysis. (A) T2 vs. T3 group and (B) T3 vs. T4 group.
Discussion
TS has been used for the treatment of PH for over 20 years12. With our deepening understanding of the disease itself and of the complications associated with TS, the aim of treatment has changed from simply resolving the symptoms to maximizing the quality of life after surgery. Traditional TS at the T2–T3 or T2–T4 levels can improve the symptoms of PH well but also increases the risk of postoperative complications (such as CS and dry hands)3–5. Limitation of the denervation level is the most commonly used method to decrease the incidence of complications and achieve satisfactory results6–8. In recent years, TS at a single level rather than at multiple levels is increasingly preferred. T2, T3 and T4 are all frequently used denervation levels for PH, and result in fairly good results and a varying incidence of postoperative complications11, 13–24. At present, there is still some debate about the optimal transection level for PH. The present meta-analysis therefore assessed 13 studies (5 comparing T2 vs. T3 and 10 comparing T3 vs. T4) in order to provide the most comprehensive evidence for level selection for TS.
Resolution of symptoms and recurrence are the two most important outcomes determining patient satisfaction. Our meta-analysis showed that there was no significant difference in the resolution of symptoms in both comparisons. All three TS levels could achieve a high rate of symptom remission (T2, 95.48%; T3, 96.42%; T4, 99.52%). In the case of recurrence rates, we surprisingly found that T3 was better than T2 and similar to T4. However, only one of the included studies supported this result, and explained that the short duration of follow-up in the T3 group may account for the low recurrence rates in this group15. We therefore repeated our analysis after excluding this article, and found no significant differences in both comparisons. Patient satisfaction is the most important criterion to evaluate the success of an operation. Our results suggested that there was no significant difference in patient satisfaction between T2 and T3 TS, and that the satisfaction rate was significantly higher after T4 TS than after T3 TS. The main reasons for dissatisfaction were severe CS and dry hands in the T2 and T3 groups and recurrence in the T4 group17, 18, 23, 25.
CS is the most common complication of TS and severely diminishes the postoperative quality of life of the patient2, 26. The incidence and severity of CS were regarded as the most important indicators of operative success in most correlational studies. In our study, both the incidence and severity of CS decreased with the descent of the denervation level. The overall incidence of CS was 78.54% in the T2 group, 69.15% in the T3 group and 41.99% in the T4 group, while the incidence of moderate-to-severe CS was 25.81%, 19.24% and 7.88% in the T2, T3 and T4 groups, respectively. The occurrence of CS was believed to be the result of a disturbance in the sympathetic system after the surgery, and greater denervation of the sympathetic nerve might be associated with a higher risk of CS. The preganglionic fibres that innervate the sweat glands of the hands originate mostly from the 2nd−6th spinal segments, of which, those from the 3rd and 4th segments are considered to be mainly responsible for PH27. TS at the T2 level inevitably cuts off the nerve conduction from the T3 and T4 segments. By the same token, TS at the T3 level cuts off the nerve conduction from the T4 segment. From our results, we consider that the aim of TS should be to transect a certain percentage of sympathetic nerve fibres, but not all. TS at the T4 level might be closer to achieving this aim than TS at the T2 or T3 levels.
Dry hands is a common complication of TS, and if severe, this complication can make patients feel even worse than they did before the operation15. In severe cases, the skin on the hands develops cracks, and regular application of hand cream is required to keep the hands moist. In the present meta-analysis, we found that the incidence of dry hands did not differ between the T2 (35.85%) and T3 (16.24%) groups, but was significantly lower in the T4 group (2.16%) than in the T3 group. These results suggest that the incidence of dry hands might be associated with the excessive denervation of sweat glands.
Gustatory sweating has been rarely reported in previous papers. Our results showed that with incidence rates of 10.38% (T2 group), 18.18% (T3 group) and 5.88% (T4 group), gustatory sweating was not a rare side effect. In the study by Herbst, the incidence of gustatory sweating was as high as 50.7%, and was particularly related to spicy or acidic foods28, 29. The pathogenesis of gustatory sweating is still unknown. Hashmonai et al. have reported that it could result from the sprouting of vagal nerve fibres into the severed sympathetic chain30. Our meta-analysis showed that the incidence of gustatory sweating did not significantly differ between the T2 and T3 groups, and was lower in the T4 group than in the T3 group.
Collectively, the above results show that the incidence of postoperative complications (CS, dry hands and gustatory sweating) decreased with the descent of the denervation level. TS at the T4 level could achieve the best curative effect with the lowest incidence of postoperative complications and equally high cure and satisfaction rates. Most of the included studies supported this result and reached a similar conclusion: the lower, the better.
The limitations of our study are as follows: (1) only English articles were included, which might have resulted in a language bias; (2) the sample size of 1577 participants from 13 studies with only 5 RCTs might have weakened the quality of the results; and (3) the operative technique, CS assessment and CS investigation time were similar but not the same across the included studies. These differences might have affected the comparability of the data.
Conclusion
In conclusion, our analysis suggests that the T2, T3 and T4 sympathectomies were all safe and effective for PH. TS at the T4 level achieved the best curative effect with the lowest incidence of postoperative complications (CS, dry hands and gustatory sweating). However, due to inter-study heterogeneity and the inherent limitations of our meta-analysis, this conclusion requires further validation through more high-quality and large-scale RCTs.
Acknowledgements
The authors would like to thank Professor Han Jiang for his advice. We also thank all the patients who participated in this study.
Author Contributions
W.Z. and X.Z. designed the study and wrote the manuscript. W.Z., D.Y. and Y.W. performed the literature searches and collected the data. W.Z. and J.X. conducted the statistical analysis. X.Z. revised the manuscript.
Competing Interests
The authors declare no competing financial interests.
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ravari H, Rajabnejad A. Unilateral Sympathectomy for Primary Palmar Hyperhidrosis. Thorac Cardiovasc Surg. 2015;63(8):723–726. doi: 10.1055/s-0034-1397041. [DOI] [PubMed] [Google Scholar]
- 2.Vanderhelst E, De Keukeleire T, Verbanck S, Vincken W, Noppen M. Quality of life and patient satisfaction after video-assisted thoracic sympathicolysis for essential hyperhidrosis: a follow-up of 138 patients. J Laparoendosc Adv Surg Tech A. 2011;21(10):905–909. doi: 10.1089/lap.2011.0258. [DOI] [PubMed] [Google Scholar]
- 3.Ambrogi V, et al. Bilateral thoracoscopic T2 to T3 sympathectomy versus botulinum injection in palmar hyperhidrosis. Ann Thorac Surg. 2009;88(1):238–45. doi: 10.1016/j.athoracsur.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 4.Ramos R, et al. Quantification of eccrine sweat glands with acetylcholine sweat-spot test and anatomical redistribution of sweating after T2-T3 thoracoscopic sympathicolysis. Surg Endosc. 2009;23(2):321–6. doi: 10.1007/s00464-008-9922-z. [DOI] [PubMed] [Google Scholar]
- 5.Chen HJ, Liang CL, Lu K. Associated change in plantar temperature and sweating after transthoracic endoscopic T2–3 sympathectomy for palmar hyperhidrosis. J Neurosurg. 2001;95:58–63. doi: 10.3171/spi.2001.95.1.0058. [DOI] [PubMed] [Google Scholar]
- 6.Ong W, Lee A, Tan WB, Lomanto D. Long-term results of a randomized controlled trial of T2 versus T2–T3 ablation in endoscopic thoracic sympathectomy for palmar hyperhidrosis. Surg Endosc. 2016;30(3):1219–1225. doi: 10.1007/s00464-015-4335-2. [DOI] [PubMed] [Google Scholar]
- 7.Li X, et al. Endoscopic thoracic sympathectomy for palmar hyperhidrosis: a randomized control trial comparing T3 and T2–4 ablation. Ann Thorac Surg. 2008;85(5):1747–51. doi: 10.1016/j.athoracsur.2008.01.060. [DOI] [PubMed] [Google Scholar]
- 8.Katara AN, Domino JP, Cheah WK, So JB, Ning C, Lomanto D. Comparing T2 and T2–T3 ablation in thoracoscopic sympathectomy for palmar hyperhidrosis: a randomized control trial. Surg Endosc. 2007;21(10):1768–71. doi: 10.1007/s00464-007-9241-9. [DOI] [PubMed] [Google Scholar]
- 9.Lin CC, Telaranta T. Lin-Telaranta classification: the importance of different procedures for different indications in sympathetic surgery. Ann Chir Gynaecol. 2001;90(3):161–156. [PubMed] [Google Scholar]
- 10.Wells, G. A. et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of non-randomised studies in meta-analyses. Available at http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm. Accessed 2012.
- 11.Jadad AR, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 12.Landreneau RJ, et al. Video-assisted thoracic surgery: basic technical concepts and intercostal approach strategies. Ann Thorac Surg. 1992;54(4):800–807. doi: 10.1016/0003-4975(92)91040-G. [DOI] [PubMed] [Google Scholar]
- 13.Lee DY, Kim DH, Paik HC. Selective division of T3 rami communicantes (T3 ramicotomy) in the treatment of palmar hyperhidrosis. Ann Thorac Surg. 2004;78(3):1052–5. doi: 10.1016/j.athoracsur.2004.03.034. [DOI] [PubMed] [Google Scholar]
- 14.Yang J, et al. T3/T4 thoracic sympathictomy and compensatory sweating in treatment of palmar hyperhidrosis. Chin Med J (Engl) 2007;120(18):1574–1577. [PubMed] [Google Scholar]
- 15.Chang YT, et al. Treatment of palmar hyperhidrosis: T(4) level compared with T(3) and T(2) Ann Surg. 2007;246(2):330–336. doi: 10.1097/SLA.0b013e3180caa466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wolosker N, et al. Is sympathectomy at T4 level better than at T3 level for treating palmar hyperhidrosis? J Laparoendosc Adv Surg Tech A. 2008;18(1):102–106. doi: 10.1089/lap.2007.0030. [DOI] [PubMed] [Google Scholar]
- 17.Mahdy T, Youssef T, Elmonem HA, Omar W, Elateef AA. T4 sympathectomy for palmar hyperhidrosis: looking for the right operation. Surgery. 2008;143(6):784–789. doi: 10.1016/j.surg.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 18.Liu Y, et al. Surgical treatment of primary palmar hyperhidrosis: a prospective randomized study comparing T3 and T4 sympathicotomy. Eur J Cardiothorac Surg. 2009;35(3):398–402. doi: 10.1016/j.ejcts.2008.10.048. [DOI] [PubMed] [Google Scholar]
- 19.Yazbek G, et al. Twenty months of evolution following sympathectomy on patients with palmar hyperhidrosis: sympathectomy at the T3 level is better than at the T2 level. Clinics (Sao Paulo) 2009;64(8):743–749. doi: 10.1590/S1807-59322009000800006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim WO, Kil HK, Yoon KB, Yoon DM, Lee JS. Influence of T3 or T4 sympathicotomy for palmar hyperhidrosis. Am J Surg. 2010;199(2):166–169. doi: 10.1016/j.amjsurg.2008.12.024. [DOI] [PubMed] [Google Scholar]
- 21.Ishy A, et al. Objective evaluation of patients with palmar hyperhidrosis submitted to two levels of sympathectomy: T3 and T4. Interact Cardiovasc Thorac Surg. 2011;12(4):545–548. doi: 10.1510/icvts.2010.252015. [DOI] [PubMed] [Google Scholar]
- 22.Baumgartner FJ, Reyes M, Sarkisyan GG, Iglesias A, Reyes E. Thoracoscopic sympathicotomy for disabling palmar hyperhidrosis: a prospective randomized comparison between two levels. Ann Thorac Surg. 2011;92(6):2015–2019. doi: 10.1016/j.athoracsur.2011.07.083. [DOI] [PubMed] [Google Scholar]
- 23.Kavakli K, et al. Comparative outcomes of T3 and T4 sympathicotomy for patients with palmar hyperhidrosis. Interact Cardiovasc Thorac Surg. 2012;12:S28–S29. [Google Scholar]
- 24.Ellatif ME, et al. Optimal level of sympathectomy for primary palmar hyperhidrosis: T3 versus T4 in a retrospective cohort study. Int J Surg. 2014;12(8):778–782. doi: 10.1016/j.ijsu.2014.05.039. [DOI] [PubMed] [Google Scholar]
- 25.Joo S, Lee GD, Haam S, Lee S. Comparisons of the clinical outcomes of thoracoscopic sympathetic surgery for palmar hyperhidrosis: R4 sympathicotomy versus R4 sympathetic clipping versus R3 sympathetic clipping. J Thorac Dis. 2016;8(5):934–941. doi: 10.21037/jtd.2016.03.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Menna C, et al. Long term compensatory sweating results after sympathectomy for palmar and axillary hyperhidrosis. Ann Cardiothorac Surg. 2016;5(1):26–32. doi: 10.3978/j.issn.2225-319X.2015.12.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gray, H. The sympathetic nerves. In: Lewis, W. H., editor. Anatomy of the human body. 20th ed. Philadelphia: Lea & Febiger 1292–1299 (2000).
- 28.Herbst F, Plas EG, Fugger R, Fritsch A. Endoscopic thoracic sympathectomy for primary hyperhidrosis of the upper limbs. A critical analysis and long-term results of 480 operations. Ann Surg. 1994;220:86–90. doi: 10.1097/00000658-199407000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang WX, Xu JJ, Xiong LH. Single-port Video-assisted Thoracoscopic Sympathectomy for the Treatment of Palmar Hyperhidrosis in 48 Patients. Chin J Clin Thorac Cardiovasc Surg. 2015;22(3):220–224. [Google Scholar]
- 30.Hashmonai M, Kopelman D, Kein O, Schein M. Upper thoracic sympathectomy for primary palmar hyperhidrosis: long-term follow-up. Br J Surg. 1992;79:268–71. doi: 10.1002/bjs.1800790329. [DOI] [PubMed] [Google Scholar]