Pharmacoepidemiologic analysis found that OEF/OIF/OND veterans have high rates of opioid use, characterized by moderate dose intensity and long treatment duration.
Keywords: Opioid, Veteran, Pharmacoepidemiology, Drug utilization, OEF/OIF/OND
Abstract
There is a great deal of concern about opioid use in veterans, particularly those who served in Afghanistan (OEF) and Iraq (OIF and OND). The current study provides a detailed pharmacoepidemiologic analysis of opioid use among OEF/OIF/OND veterans from FY09 to FY12. Data from 3 data repositories from the Veterans Health Administration (VHA) were used to describe demographic, clinical, and medication characteristics associated with opioid use among OEF/OIF/OND veterans and among those with TBI. Logistic regression models were used to identify risks associated with chronic opioid use in FY12. Approximately 23% of all OEF/OIF/OND veterans and 35% of those with TBI received any opioid medications. Most received moderate doses ranging from 26 to 30 mg morphine equivalent dose daily. Median days of opioid use for all OEF/OIF/OND veterans were 30 to 40 days. Factors associated with chronic use in both groups included young age, male sex, white race, being married, and living in rural areas. A diagnosis of PTSD (odds ratio [OR] = 1.22, P < 0.0001), major depressive disorder (OR = 1.14, P < 0.0001), and tobacco use disorder (OR = 1.18, P < 0.0001) were strongly associated with chronic opioid use. Back pain was also strongly associated with chronic use (OR = 2.50, P < 0.0001). As pain severity increased the odds of chronic opioid use also increased: mild pain (OR = 3.76, P < 0.0001), moderate pain (OR = 6.80, P < 0.0001), and severe pain (OR = 8.49, P < 0.0001). Opioid use among OEF/OIF/OND veterans is characterized by moderate doses that are used over relatively long periods of time by a minority of veterans.
1. Introduction
Prescribing opioid medications to treat chronic pain has increased dramatically in the last 2 decades, resulting in unprecedented numbers of people receiving opioids chronically.5 This increased opioid use has been accompanied by a well-documented parallel increase in opioid abuse/dependence and accidental overdose, suggesting increases in use and abuse may be linked.6,9–11,17,22,24,26,28 Therefore, understanding risks for chronic opioid use offers the opportunity to identify, and potentially modify, factors associated with chronic use and help prevent development of opioid misuse and abuse.
There is a great deal of concern about opioid use in the veteran population, particularly those that served in Afghanistan (Operation Enduring Freedom–OEF) and Iraq (Operation Iraqi Freedom–OIF and Operation New Dawn–OND). This includes significant lay press coverage and hearings in the U.S. House of Representations and Senate Veterans' Affairs Committees.2,18,21 This issue has also received a great deal of attention in the clinical and scientific communities. The use of pain as the “fifth Vital Sign” is now being questioned, and organizations are taking action to optimize pain care. VHA has implemented a wide range of clinical policies related to opioid use for chronic pain. Updates to these policies in 2009,31,36 2013,30 and 201432 have increased the effort required by providers and patients for opioid prescribing and use, respectively.
A wide range of studies have examined the use of opioids to treat chronic pain in veterans.14–16,27 Several studies described opioid use in VHA using data from a single VHA network in the Pacific Northwest.12,23 These studies likely included OEF/OIF/OND veterans, but did not specifically focus on this cohort. The findings are particularly notable because they suggest pre-existing substance use and mental health disorders are associated with receipt of opioid medications, including receiving opioids chronically. However, it is unclear how well the cohort from those studies represents care for veterans nationwide. Studies utilizing national-level data from VHA do exist,3,4,13,27 but do not focus on opioid utilization in the OEF/OIF/OND cohort. Because this contingent is not the focus, the estimates of opioid use among these veterans vary wildly ranging from 3% to 64%.
None of the work to date provides information about the extent to which OEF/OIF/OND veterans, nationally, receive any opioids, received chronic opioid therapy, receive high opioid doses, or take multiple opioid medications concurrently. Limitations to the current literature include studies with one or more of the following limitations: (1) studies lack national data, (2) studies use data from 2009 or earlier, (3) studies do not require minimal amount of documented VHA care in a given year, and (4) studies require a chronic noncancer pain diagnosis for inclusion. The objective of this study is to fully understand the pharmacoepidemiology of current opioid use in OEF/OIF/OND veterans engaged in VHA care by performing an analysis that uses recent, national data and that includes all OEF/OIF/OND veterans who are regular users of VHA care, regardless of pain diagnosis.
2. Methods
2.1. Data sources
Data for this study were obtained from 3 repositories within the VHA: the Corporate Data Warehouse (CDW), the OEF/OIF/OND Roster, and the VA Pharmacy Benefits Management Service (PBM). The CDW is a relational database derived from the VA electronic health record that records demographics, clinical characteristics, and health care utilization records, including pain scores. The OEF/OIF/OND Roster file35 provides information on all veterans who served in the OEF/OIF/OND conflicts and separated from the military since 2001. The PBM provides records of all opioid prescriptions dispensed by VHA during our study period including medication name, strength, number dispensed, days supplied, and date dispensed. Records from all repositories had a common scrambled social security number (ScrSSN) to allow records to be linked across data sources.
This study was approved by the Institutional Review Boards of the University of Arkansas for Medical Sciences and the Central Arkansas Veterans Healthcare System. A data use agreement was also executed with each data repository.
2.2. Inclusion or exclusion criteria
The analytic data set was created by using the CDW to identify all veterans who used inpatient or outpatient care in the VHA nationwide from FY08 to FY13. To avoid truncation of data, we used data from FY09 to FY12 for analysis. It was difficult to tell which year a veteran entered the OEF/OIF/OND registry, so we identified all veterans who used VHA care at least once during the study period and matched them to the registry to identify OEF/OIF/OND veterans. Because VHA has implemented a range of policies with respect to management of chronic pain and opioid use, we wanted to identify a cohort that used VHA care regularly, since they would be most affected by these policies. In addition, because veterans can receive care in non-VA settings, it was important to identify a cohort that was likely to be using VHA regularly, including using VHA for pain management and therefore, may be less likely to receive opioids from non-VHA providers. Therefore, only those OEF/OIF/OND veterans who used VHA inpatient or outpatient care at least twice during a given fiscal year were included in the analyses. A veteran could also be counted in more than 1 fiscal year. Using the ScrSSN, we extracted outpatient opioid prescription records from the PBM and each veteran's corresponding demographic and clinical information, including pain scores, from the CDW. Veterans with a cancer diagnosis, those enrolled in VHA hospice care, and those residing in a VHA nursing home or domiciliary were excluded because pain management or use of medication in these groups may be different than those with other painful conditions or in other environments. In addition, patients who were receiving opioids in injectable or suppository form or whose opioid prescription records were incomplete were excluded because calculating a daily opioid dose was not possible from those records.
Opioid dependence is sometimes treated with methadone or buprenorphine, known as opioid agonist therapy. To ensure that these individuals were not included in the analyses, veterans with clinic visits for opioid agonist therapy and those with prescriptions for buprenorphine were also excluded. To protect against data entry errors in the prescription records, individuals with an average daily dose greater than 1000 mg morphine equivalent dose (MED) per day were treated as having a potentially invalid value and were excluded from the analyses. These criteria resulted in 3.2% to 3.4% of OEF/OIF/OND veterans being excluded per year.
2.3. Demographic characteristics
Demographic characteristics include age, race, sex, marital status, and rural–urban status. Table 1 provides the mean age for each study year. Categorical variables for age were also created and used in the model examining risk factors for chronic opioid use in FY12 (Table 4). The categories for race were collapsed into white, nonwhite, and missing because of small sample sizes in nonwhite categories. The “missingness” of race data is a well-known and well-studied problem in VHA databases and can be as high as 30%.33,34 To populate this field as much as possible, we searched inpatient records and outpatient encounter records because race is a field in each record. Race was missing for less than 10% of veterans included in our analyses. Marital status was collapsed into 2 categories: married and unmarried. Lastly, veterans were categorized into 1 of 4 categories based on the 5-digit zip code from the most recent home address on file with VHA: urban, large rural, small rural, and isolated rural.25
Table 1.
Demographic characteristics all OEF/OIF/OND.
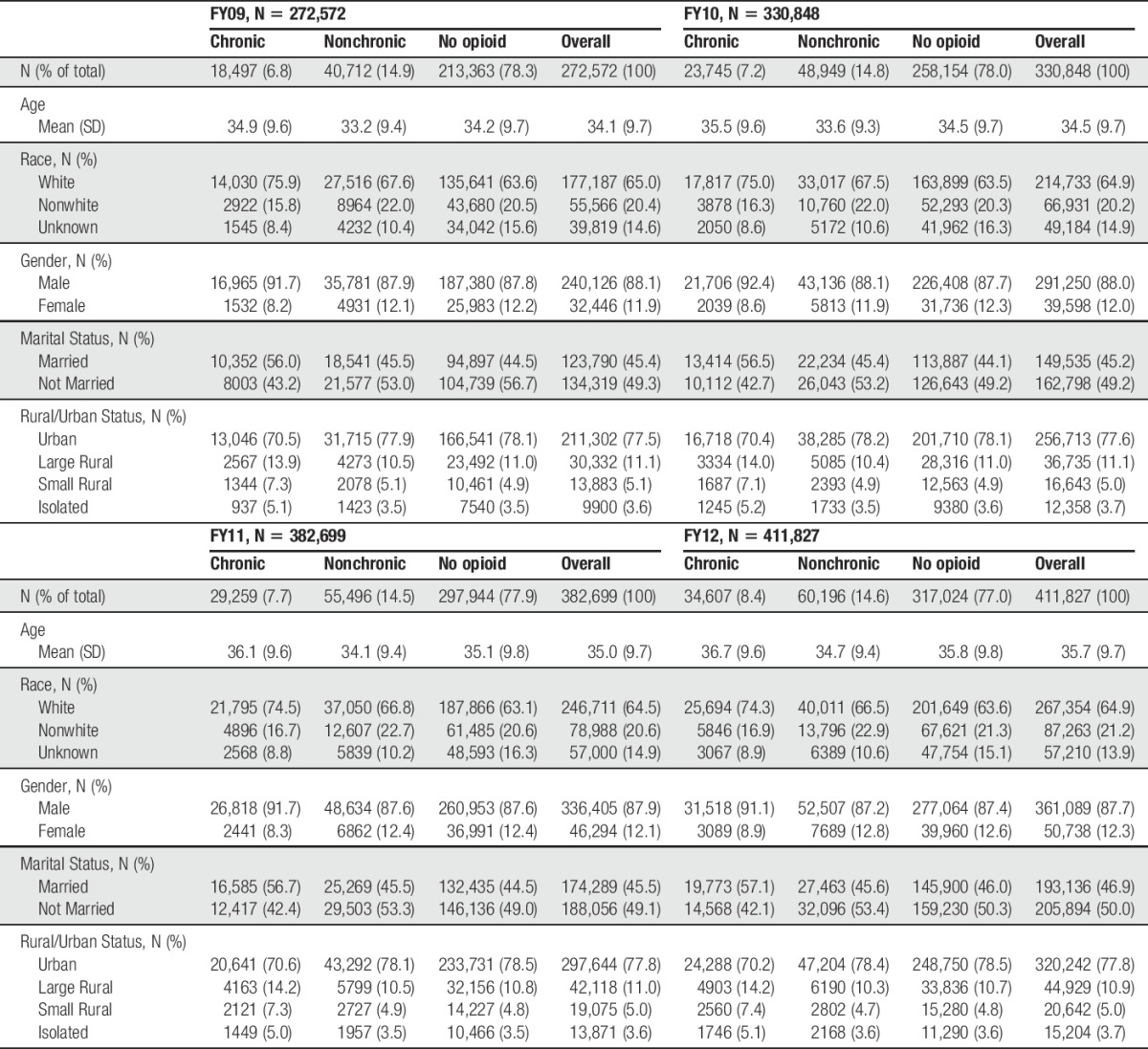
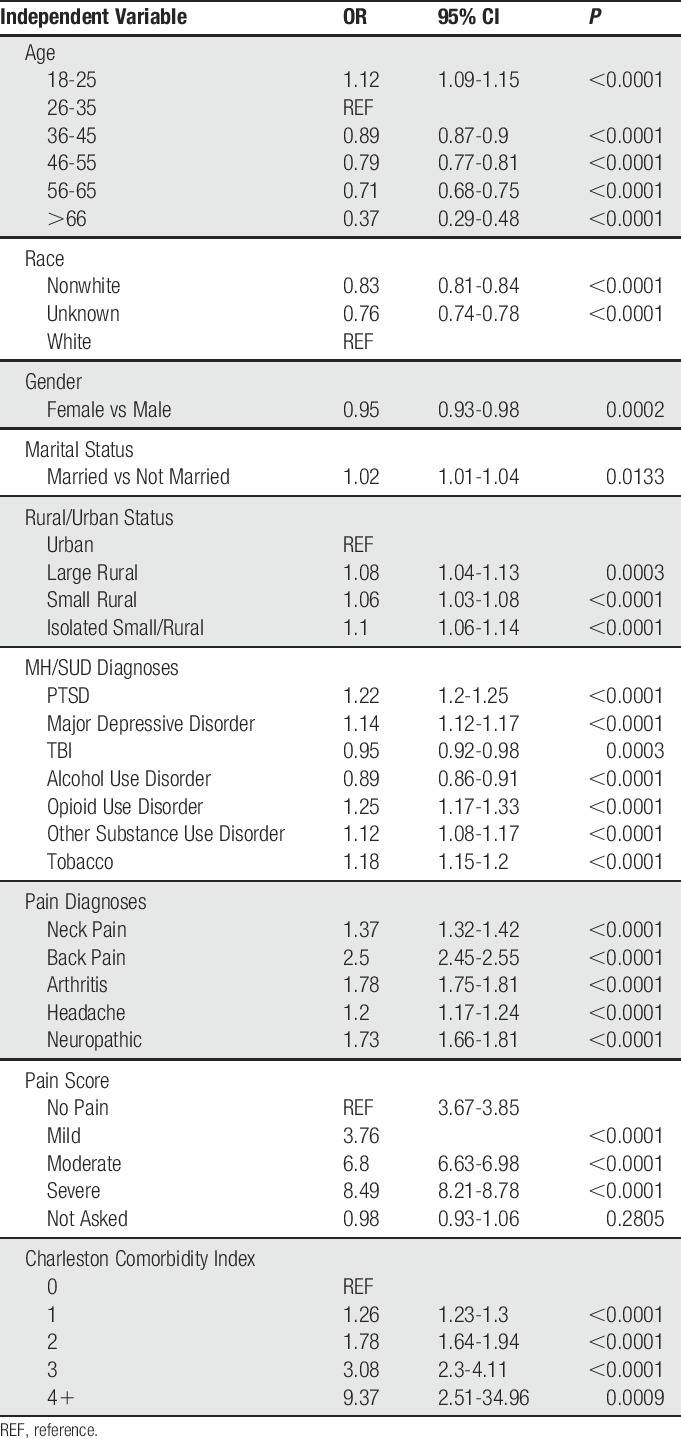
Table 4.
Likelihood of chronic opioid use in FY12 all OEF/OIF/OND.
2.4. Clinical characteristics
To identify the clinical indications for veterans receiving opioids, we extracted ICD-9 codes from the CDW and specified 5 categories of pain that are common among veterans: neck, back, arthritis or joint, headache or migraine, and neuropathic. Veterans were categorized as having 1 of the 5 pain conditions if they had at least 1 outpatient visit coded with a condition within a fiscal year and had a second code for that same condition at least 30 days but less than or equal to 365 days later. Each person included in the study could have more than one of the 5 painful conditions.
Mental health and substance use diagnoses were based on definitions used by the VA Northeast Program Evaluation Center (NEPEC).19 We identified veterans with diagnoses who, in other analyses, have been associated with opioid use, including depression, post-traumatic stress disorder (PTSD), non-opioid substance use disorder, opioid use disorder, alcohol use disorder, and tobacco use. Based on the NEPEC definition, a mental health diagnosis was defined as having at least 2 outpatient encounters for any of the mental health or substance use diagnoses described above, and at least one of the outpatient encounters must have been an in‐person encounter (ie, both encounters cannot be telephone contacts). Each unique veteran could receive more than one mental health or substance use diagnosis.
We also identified outpatient pain scores for each veteran. The VHA uses a 0 to 10 numeric rating scale with 0 indicating no pain and 10 indicating the worse possible pain.20 Pain scores for each veteran were averaged across each year so that they had a single score for each fiscal year. Veterans were grouped into those with a pain score of 0, those with mild pain (1-3), moderate (4-6), and severe (7-10)38 and included in regression models as a categorical variable (Table 4), those with no reported pain score were included as a separate group.
2.5. Medication characteristics
Opioid days were defined as the number of days in a given year that the veteran could have taken at least 1 dose of an opioid medication. To calculate the number of opioid days, the prescriptions for each year were sorted into chronological order based on the date dispensed. If any 2 prescriptions overlapped by more than 10 days or 20%, the overlapping portions of the prescription were assumed to be taken concurrently and the overlapping days were only included once in the opioid days calculation. If the overlap was ≤10 days or 20%, the second prescription was shifted and the overlapping days from both the first and second prescription were included in the opioid day calculation. Opioid use in each fiscal year was categorized as chronic use (≥90 d/yr) or nonchronic use (<90 d/yr). Each opioid prescription was converted to an MED by multiplying the medication strength and the quantity dispensed by a published conversion factor.1,29,37 All MEDs were summed across a given year to create the total MED/patient/year. The average daily MED was calculated by dividing the total MED by the number of opioid days that a patient could have taken opioids in that year.
In addition to opioid use being categorized as chronic or nonchronic, it was further characterized by calculating the proportion of chronic users who received a daily dose of >100 mg MED daily and those who received >120 mg MED daily because opioid doses at these levels have been identified as high dose and as being associated with opioid overdose, respectively.5 The proportion of veterans who were identified as chronic opioid users and who were receiving long-acting opioid medications was calculated for each year. Long-acting opioids were defined as any opioid formulated to have sustained release properties (such as oxycodone sustained release or fentanyl patch) or those that are intrinsically long-acting, such as methadone. We did not differentiate between opioids classified as schedule II (the most restrictive in terms of prescribing regulations) vs schedules III to V. We also created a “multiple opioid” measure to identify veterans taking more than 1 opioid medication concurrently. This was defined as 2 or more types of opioids that overlapped by more than 30 days in any 40-day period.
We have provided descriptive tables of opioid use in OEF/OIF/OND veterans as well as those with traumatic brain injury. Logistic regression models were used to model the likelihood of receiving opioids chronically in FY12 for all OEF/OIF/OND veterans. Each model included demographic characteristics, mental health and substance use diagnoses, pain conditions, pain score, and opioid characteristics. The Charlson Comorbidity Index was used to control for other physical health diagnoses.7,8
3. Results
Tables 1–3 describe the demographic, clinical, and medication characteristics, respectively, for all OEF/OIF/OND veterans who met our inclusion criteria from FY09 to FY12 and are divided into the following categories: chronic users, nonchronic users, no opioid use, and the cohort overall. The number of veterans meeting our inclusion criteria increased during the study period, which is consistent with the increase in the number of OEF/OIF/OND veterans in general and the number using VHA care (Table 1). Across the study period, approximately 22% to 23% of the cohort received opioids, with 7% to 8% receiving them chronically. Overall, most veterans were white and male. This was consistent across the categories of chronic opioid use, nonchronic use, and no opioid use, and across fiscal years. Interestingly, the majority of chronic opioid users were married. Regardless of study year, most veterans lived in urban settings; this was true among chronic and nonchronic users as well as those with no opioid use.
Table 3.
Medication characteristics all OEF/OIF/OND.
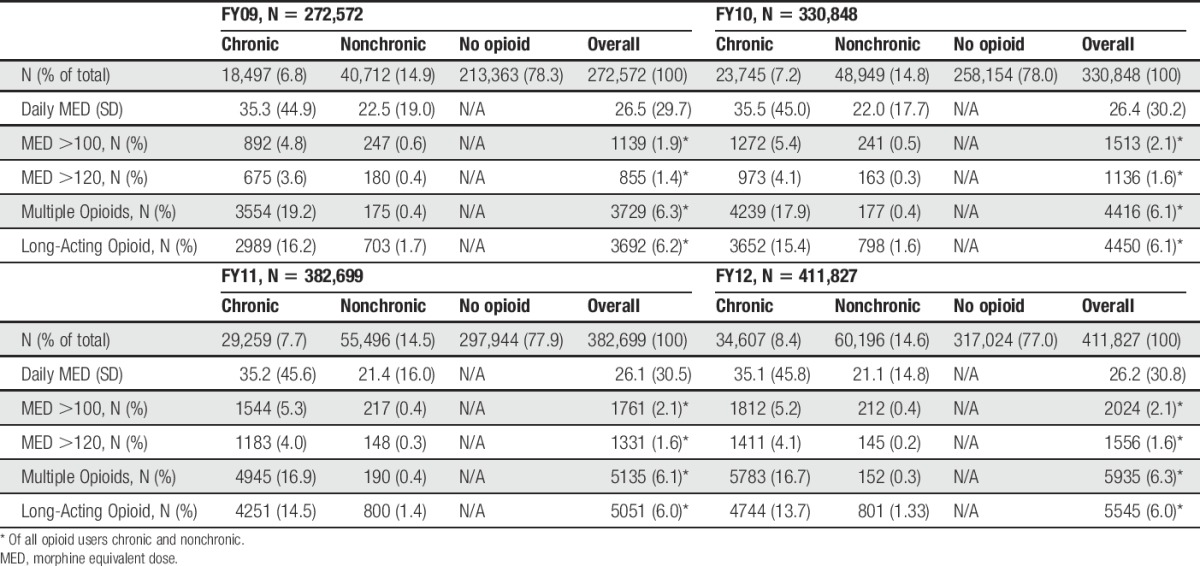
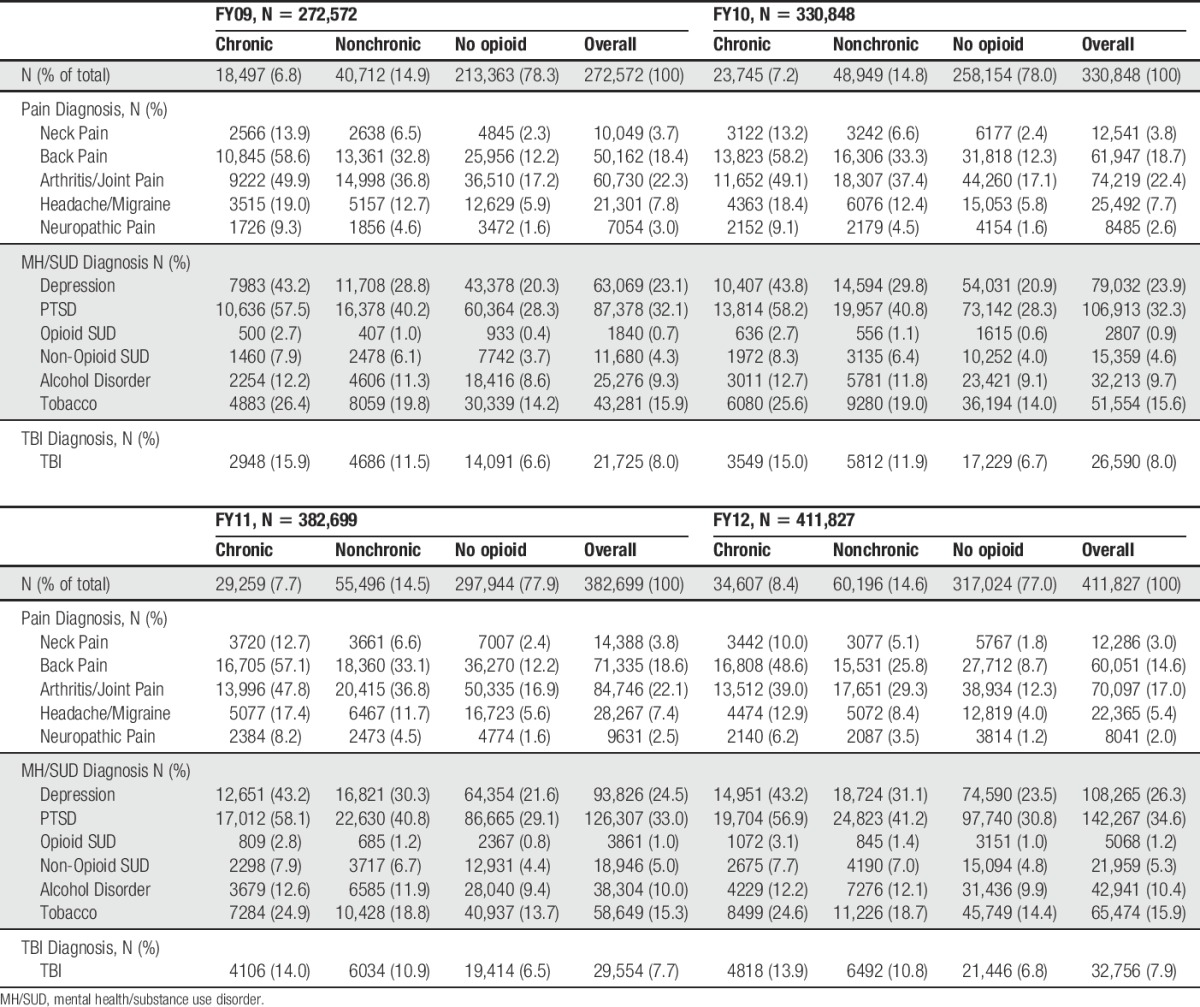
Table 2 provides clinical characteristics for each fiscal year. Arthritis and joint pain were the most prevalent painful conditions overall, but back pain was the most common painful condition among chronic opioid users. The proportion of chronic users with depression and PTSD was higher than nonchronic users or those with no opioid use. Tobacco use was also the most common substance-related condition and was more common among chronic opioid users.
Table 2.
Clinical characteristics all OEF/OIF/OND.
The mean MED was low to moderate, approximately 26 mg daily, across all study years. (See Table 3 for mean dose in each year and SD.) Among chronic users, the dose was higher, but still moderate at approximately 35 mg MED daily in each year. The prevalence of high-dose opioids, concurrent use of multiple opioids, and use of long-acting opioids was fairly low. Prevalence of high-dose opioid therapy was much higher in chronic users than in nonchronic users. From FY09 to FY12, approximately 5% of chronic users (2% of all opioid users) received MED >100 mg daily and approximately 4% of chronic users (approximately 1.5% of all opioid users) received MED >120 mg daily. Interestingly, the use of multiple opioids decreased over time. In FY09, 19.2% of chronic users received multiple opioid medications concurrently compared to 16.7% in FY12. Likewise, use of long-acting opioids has decreased over time from 16.2% of chronic users in FY09 to 13.7% in FY12. Although it is not included in the table, we also examined the days of opioid use for each year. In the OEF/OIF/OND cohort, median days of opioid use (50th percentile) were 31, 35, 38, and 42 for FY09, FY10, FY11, and FY12, respectively.
Table 4 provides the logistic regression model examining factors associated with chronic opioid use in FY12 for all OEF/OIF/OND veterans. From a demographic perspective, the findings in this model are similar to other groups, with the risk of opioid use decreasing in the older age groups.4,27,39 Veterans living in any type of rural area are less likely to receive opioids chronically compared to veterans living in urban areas. Similar to other studies, veterans with a diagnosis of PTSD, major depressive disorder, and tobacco use disorder are more likely to receive opioids chronically.4,27,39 However, those with diagnosed TBI were less likely to receive chronic opioid therapy. In addition, veterans with a diagnosed alcohol use disorder had approximately 10% lower odds of receiving chronic opioid therapy, whereas those with a diagnosed opioid use disorder had approximately 25% higher odds of receiving this treatment; diagnosis of other substance use disorders did not significantly affect the likelihood of receiving chronic opioids. Among pain diagnoses, veterans with a diagnosis of back pain had more than triple the odds of receiving chronic opioid therapy compared to veterans without back pain. As pain scores increased, the odds of receiving opioid medication also increased relative to individuals with no pain. Opioid characteristics were most strongly associated with chronic opioid therapy.
4. Discussion
To our knowledge, this is the first detailed national report of opioid prescribing among OEF/OIF/OND veterans. These findings suggest that the prevalence of opioid use in OEF/OIF/OND veterans is relatively modest. In these analyses, 23% of all OEF/OIF/OND veterans received any outpatient opioid in FY12. Among opioid users, chronic use was also modest, with 8.4% of OEF/OIF/OND veterans using opioids chronically in FY12. These findings are well within the large range (3%-64%) reported in other studies of OEF/OIF/OND veterans, and much smaller than the findings from Macey et al.23 (64%), which examined data from 2008. Similar to previous work, we also found that most veterans received moderate doses of opioids and few had high-risk opioid use such as high MED, use of multiple opioids concurrently, and use of long-acting opioids.12,13,23 This suggests that high-risk opioid use is less of a problem in OEF/OIF/OND veterans than suggested in previous studies, and certainly less than suggested by the lay press. Several previous studies found that history of substance use disorders was associated with the likelihood of receiving opioids, especially receiving them chronically.12,13,23 On the contrary, OEF/OIF/OND veterans with a diagnosed alcohol use disorder had about 20% lower odds of receiving chronic opioids, and a diagnosis of substance abuse other than opioids, tobacco, or alcohol was not associated with chronic opioid use at all. Unfortunately, a diagnosis of opioid use disorder, increased opioid dose, and use of long-acting opioids were each significantly associated with an increased likelihood of chronic opioid use, although it is not possible to determine the direction of these associations.
Our findings are also interesting when examined in comparison to a recent analysis of opioid use among veterans nationwide with a diagnosis of chronic noncancer pain.13 This analysis found that, although the prevalence of any outpatient opioid use in 2011 was approximately 50%, with about 57% of opioid users receiving opioids chronically, use among OEF/OIF/OND veterans was lower than veterans as a whole (47%). These results suggest that the OEF/OIF/OND cohort may be at a lower risk of opioid use, including chronic use, than veterans as a whole.
This study is subject to several limitations. The work is based on outpatient opioid prescriptions prescribed within the VHA, therefore the analyses do not account for opioids that veterans may have received outside the VHA system. These analyses included data from veterans who use the VHA at least twice in a given fiscal year. This was an effort to ensure a cohort of veterans who were seen in VHA regularly, may be less likely to receive care outside the VHA system, and were most likely to be affected by opioid-related policies implemented by VHA. These analyses are also subject to the limitations of any secondary data analyses. First, it is possible that some diagnoses may be miscoded or that some veterans may have a particular diagnosis that was not annotated in the record. Furthermore, the opioid use disorder may be coded simply as substance abuse disorder in the health record. However, we accounted for both opioid use disorder and other substance use disorders in each model. Therefore, regardless of how a provider coded opioid use disorder, it would have been included in the analysis, but we can only specifically attribute opioid use disorder to records specifically coded for it. Theoretically, the risk of a patient misusing the opioid and it not being recognized clinically and/or not coded would be similar across all studies using VHA electronic health record data; therefore, it seems reasonable to compare findings related to both opioid use disorder and substance use disorder to previous work. While this analysis helps to explain the prescribing and utilization of opioids in veterans, the administrative claims used to answer these questions are insufficient to make inferences as to the effect opioids may have on functional status or quality of life.
Taken as a whole, these analyses suggest that opioid use among OEF/OIF/OND veterans is characterized by moderate doses that are used over relatively long periods of time by a minority of veterans. Practices such as prescribing high-dose opioids, use of multiple concurrent opioids, and use of long-acting opioids occur in a fairly small percentage of these veterans. These findings also suggest that the use of opioids is less common among OEF/OIF/OND veterans compared with veterans as a whole. This analysis provides a strong baseline for evaluating the impact of recently implemented additional opioid-related policies.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supported by the National Institute on Drug Abuse grant no. R01 DA030300. T. J. Hudson also receives support from the VA HSR&D Center for Mental Healthcare and Outcomes Research.
The views expressed in this article are those of the authors and do not represent the views of the Department of Veterans Affairs or the United States Government.
Acknowledgements
The authors thank Ms. Cynthia Brace for editing and formatting the manuscript.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
References
- [1].Ashburn MA, Lipman AG, Carr D, Rubingh C. Principles of analgesic use in the treatment of acute pain and cancer pain. Glenview: American Pain Society, 2003. [Google Scholar]
- [2].Axelrod J; CBS News. Veterans dying from overmedication. Available at: http://www.cbsnews.com/news/veterans-dying-from-overmedication/. Accessed July 21, 2016.
- [3].Barry DT, Sofuoglu M, Kerns RD, Wiechers IR, Rosenheck RA. Prevalence and correlates of co-prescribing psychotropic medications with long-term opioid use nationally in the Veterans Health Administration. Psychiatry Res 2015;227:324–32. [DOI] [PubMed] [Google Scholar]
- [4].Bohnert AS, Ilgen MA, Trafton JA, Kerns RD, Eisenberg A, Ganoczy D, Blow FC. Trends and regional variation in opioid overdose mortality among Veterans Health Administration patients, Fiscal Year 2001 to 2009. Clin J Pain 2014;30:605–12. [DOI] [PubMed] [Google Scholar]
- [5].Bohnert AS, Valenstein M, Bair MJ, Ganoczy D, McCarthy JF, Ilgen MA, Blow FC. Association between opioid prescribing patterns and opioid overdose-related deaths. J Am Med Assoc 2011;305:1315–21. [DOI] [PubMed] [Google Scholar]
- [6].Chabal C, Erjavec MK, Jacobson L, Mariano A, Chaney E. Prescription opiate abuse in chronic pain patients: clinical criteria, incidence, and predictors. Clin J Pain 1997;13:150–5. [DOI] [PubMed] [Google Scholar]
- [7].Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol 1994;47:1245–51. [DOI] [PubMed] [Google Scholar]
- [8].Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–83. [DOI] [PubMed] [Google Scholar]
- [9].Chelminski PR, Ives TJ, Felix KM, Prakken SD, Miller TM, Perhac JS, Malone RM, Bryant ME, DeWalt DA, Pignone MP. A primary care, multi-disciplinary disease management program for opioid-treated patients with chronic non-cancer pain and a high burden of psychiatric comorbidity. BMC Health Serv Res 2005;5:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Compton WM, Volkow ND. Major increases in opioid analgesic abuse in the United States: concerns and strategies. Drug Alcohol Depend 2006;81:103–7. [DOI] [PubMed] [Google Scholar]
- [11].Cowan DT, Wilson-Barnett J, Griffiths P, Allan LG. A survey of chronic noncancer pain patients prescribed opioid analgesics. Pain Med 2003;4:340–51. [DOI] [PubMed] [Google Scholar]
- [12].Dobscha SK, Morasco BJ, Duckart JP, Macey T, Deyo RA. Correlates of prescription opioid initiation and long-term opioid use in veterans with persistent pain. Clin J Pain 2013;29:102–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Edlund MJ, Austen MA, Sullivan MD, Martin BC, Williams JS, Fortney JC, Hudson TJ. Patterns of opioid use for chronic noncancer pain in the Veterans Health Administration from 2009 to 2011. PAIN 2014;155:2337–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Edlund MJ, Steffick D, Hudson T, Harris KM, Sullivan M. Risk factors for clinically recognized opioid abuse and dependence among veterans using opioids for chronic non-cancer pain. PAIN 2007;129:355–62. [DOI] [PubMed] [Google Scholar]
- [15].Edlund MJ, Sullivan MD, Han X, Booth BM. Days with pain and substance use disorders: is there an association? Clin J Pain 2013;29:689–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Epidemiology Program, Post-Deployment Health Group, Office of Public Health, Veterans Health Administration, Department of Veterans Affairs. Analysis of VA health care utilization among Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) veterans: cumulative from 1st Qtr FY 2002 through 4th Qtr FY 2013 (October 1, 2001-September 30, 2013). Washington, DC: 2014. Available at: http://www.publichealth.va.gov/docs/epidemiology/healthcare-utilization-repor-fy2013-qtr4.pdf. Accessed July 21, 2016. [Google Scholar]
- [17].Gilson AM, Ryan KM, Joranson DE, Dahl JL. A reassessment of trends in the medical use and abuse of opioid analgesics and implications for diversion control: 1997-2002. J Pain Symptom Management 2004;28:176–88. [DOI] [PubMed] [Google Scholar]
- [18].Glantz A. VA's opiate overload feeds veterans' addictions, overdose deaths. Available at: http://cironline.org/reports/vas-opiate-overload-feeds-veterans-addictions-overdose-deaths-5261. Accessed July 21, 2016.
- [19].Greenberg G, Pilver L, Hoff R; Northeast Program Evaluation Center. 2012 National Mental Health Fact Sheet: National, VISN, and VAMC Tables. Available at: http://vaww.nepec.mentalhealth.va.gov/NMHPPMS/nmhFaSAC.pdf. Accessed July 21, 2016.
- [20].Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: visual analog scale for pain (VAS pain), numeric rating scale for pain (NRS pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short Form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP). Arthritis Care Res 2011;63:S240–52. [DOI] [PubMed] [Google Scholar]
- [21].House Committee on Veterans' Affairs, Subcommittee on Health. Between peril and promise: facing the dangers of VA's skyrocketing use of prescription painkillers to treat Veterans. Available at: http://veterans.house.gov/hearing/between-peril-and-promise-facing-the-dangers-of-va%E2%80%99s-skyrocketing-use-of-prescription. Accessed July 21, 2016.
- [22].Jonasson U, Jonasson B, Wickstrom L, Andersson E, Saldeen T. Analgesic use disorders among orthopedic and chronic pain patients at a rehabilitation clinic. Subst Use Misuse 1998;33:1375–85. [DOI] [PubMed] [Google Scholar]
- [23].Macey TA, Morasco BJ, Duckart JP, Dobscha SK. Patterns and correlates of prescription opioid use in OEF/OIF Veterans with chronic noncancer pain. Pain Med 2011;12:1502–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Michna E, Ross EL, Hynes WL, Nedeljkovic SS, Soumekh S, Janfaza D, Palombi D, Jamison RN. Predicting aberrant drug behavior in patients treated for chronic pain: importance of abuse history. J Pain Symptom Manage 2004;28:250–8. [DOI] [PubMed] [Google Scholar]
- [25].Rural Health Research Center. RUCA maps: map classifications. 2014. Available at: http://depts.washington.edu/uwruca/ruca-maps.php. Accessed July 21, 2016.
- [26].Schieffer BM, Pham Q, Labus J, Baria A, Van VW, Davis P, Davis F, Naliboff BD. Pain medication beliefs and medication misuse in chronic pain. J Pain 2005;6:620–9. [DOI] [PubMed] [Google Scholar]
- [27].Seal KH, Shi Y, Cohen G, Cohen BE, Maguen S, Krebs EE, Neylan TC. Association of mental health disorders with prescription opioids and high-risk opioid use in US Veterans of Iraq and Afghanistan. J Am Med Assoc 2012;307:940–7. [DOI] [PubMed] [Google Scholar]
- [28].U.S. Department of Health and Human Services. Prescription opioid use and abuse in the treatment of pain. Request for Applications (RFA) No: RFA-DA-06–005. 2005. Available at: https://grants.nih.gov/grants/guide/rfa-files/RFA-DA-06-005.html. Accessed July 21, 2016. [Google Scholar]
- [29].U.S. Department of Justice, U.S. Drug Enforcement administration, Office of Diversion Control. Drug scheduling. Available at: http://www.usdoj.gov/dea/pubs/scheduling.html. Accessed February 24, 2009.
- [30].U.S. Department of veterans Affairs. VA initiative shows early promise in reducing use of opioids for chronic pain. Available at: http://www.va.gov/opa/pressrel/docs/opioids.docx. Accessed July 21, 2016.
- [31].U.S. Department of Veterans Affairs, Veterans Health Administration. VHA directive 2009-053: pain management. Washington, DC: 2009. Available at: http://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=2781. Accessed July 21, 2016. [Google Scholar]
- [32].U.S. Department of Veterans Affairs, Veterans Health Administration. VHA directive 1005: informed consent for long-term opioid therapy for pain. Washington, DC: 2014. Available at: http://www1.va.gov/vhapublications/ViewPublication.asp?pub_ID=3005. Accessed July 21, 2016. [Google Scholar]
- [33].VA Information Resource Center (VIReC). VIReC research user guide: select variable frequencies from the FY 2002 VHA medical SAS datasets. 2003. Available at: http://www.virec.research.med.va.gov/References/RUG/RUG-SelectVarFreq02.pdf. Accessed July 21, 2016.
- [34].VA Information Resource Center (VIReC). Using VA data for research: cancer as an example. 2005. Presented at the 7th Annual Seattle Epidemiology, Biostatistics and Clinical Research Methods Summer Session, June 20-24, 2005. Seattle, WA. Available at: http://www.virec.research.med.va.gov/References/SelectPresentations/SelectPresentations.htm. Accessed July 21, 2016.
- [35].VA Information Resource Center (VIReC). OEF/OIF/OND Roster. Hines, IL: 2011. Available at: http://vaww.virec.research.va.gov/OEF-OIF-OND-Roster/RG-OEF-OIF-OND-Roster-CY11-RA.pdf. Accessed July 21, 2016. [Google Scholar]
- [36].Veterans Health Administration, Department of Defense. VA/DoD clinical practice guideline for the management of opioid therapy for chronic pain. v2.0. Washington, DC: 2010. Available at: http://www.healthquality.va.gov/guidelines/Pain/cot/COT_312_Full-er.pdf. Accessed July 21, 2016. [Google Scholar]
- [37].Vieweg WVR, Carlyle Lipps WF, Fernandez A. Opioids and methadone equivalents for clinicians. Prim Care Companion J Clin Psychiatry 2005;7:86–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Wetherington S, Delong L, Kini S, Veledar E, Schaufele MK, McKenzie-Brown AM, Chen SC. Pain quality of life as measured by utilities. Pain Med 2014;15:865–70. [DOI] [PubMed] [Google Scholar]
- [39].Zedler B, Xie L, Wang L, Joyce A, Vick C, Kariburyo F, Rajan P, Baser O, Murrelle L. Risk factors for serious prescription opioid-related toxicity or overdose among Veterans Health Administration patients. Pain Med 2014;15:1911–29. [DOI] [PubMed] [Google Scholar]


