Abstract
Long-term magnesium supplementation improves arterial stiffness, a cardiovascular disease risk marker. Effects on endothelial function may be another mechanism whereby increased magnesium intakes affect cardiovascular risk. Therefore, a 24-week, randomized, double-blind, placebo-controlled trial was performed to examine effects of magnesium supplementation on endothelial function and cardiometabolic risk markers. Fifty-two overweight and obese subjects (30 men and 22 women, age 62 ± 6 years) were randomized to receive either three times daily magnesium (total dose: 350 mg) or placebo capsules. Endothelial function was assessed at the start and at the end of the study. Cardiometabolic risk markers were measured at baseline, after 12 weeks, and at week 24. Brachial artery flow-mediated vasodilation did not change following long-term magnesium supplementation (0.49 pp; 95% CI: −0.38 to 1.36 pp; P = 0.26). Changes in reactive hyperemia index, retinal microvascular caliber and plasma markers for microvascular endothelial function (sVCAM-1, sICAM-1 and sE-selectin) were also not different. In addition, no effects on serum lipids, plasma glucose, insulin sensitivity, and low-grade systemic inflammation were observed. In conclusion, a daily magnesium supplement of 350 mg for 24 weeks does not improve endothelial function and cardiometabolic risk markers in overweight and obese middle-aged and elderly adults.
Introduction
Prospective cohort studies have not only found an inverse association between dietary magnesium intake and diabetes1, but also with cardiovascular disease (CVD) risk2, 3. However, the number of well-designed intervention trials to examine a potential causal role of magnesium intake in the prevention of CVD is very limited. Recently, we have reported that in overweight and obese adults magnesium supplementation for 24 weeks resulted in a clinically relevant reduction in arterial stiffness, suggesting a potential mechanism by which dietary magnesium affects cardiovascular health4. Effects on endothelial function and cardiometabolic risk markers, which were secondary outcomes of the study, were however not reported. Conventional cardiometabolic risk markers are known determinants of arterial stiffness5 and the vascular endothelium has also been suggested to play an important role in arterial stiffening6. Reported effects of magnesium intake on serum lipids, plasma glucose, insulin sensitivity and low-grade systemic inflammation are inconsistent7–11, while only a few well-controlled intervention studies have examined effects on endothelial function. These trials involved patients taking anti-hypertensive drugs or medication known to affect lipid or glucose metabolism12, 13, which may have masked effects of oral magnesium supplementation, and only used markers reflecting large artery (i.e. the brachial artery) endothelial function11–13.
Endothelial function can be assessed in different ways. Brachial artery flow-mediated vasodilation (FMD), an ultrasound measurement of a large peripheral muscular artery, is considered the current non-invasive gold standard technique14. The change in pulse wave amplitude in response to blood flow-induced increases in shear stress is another functional marker of endothelial function, defined as the reactive hyperemia index (RHI). RHI reflects small artery reactivity15, while microvascular endothelial function can be assessed by measuring plasma markers that are synthesized by activation of the endothelium16. As these markers also relate to CVD risk17, effects on endothelial function of an increased magnesium intake were also assessed in our 24-week, randomized, double-blind, placebo-controlled intervention trial. The study involved overweight and obese middle-aged and elderly adults, because they are expected to have an impaired endothelial function18 and cardiometabolic disturbances at the start of the trial19, allowing for improvement by the intervention.
Results
Study subjects and compliance
The flow of participants through the study is shown in Supplemental Figure 1. A total of 51 subjects (29 men and 22 women) completed the trial. Baseline characteristics of these participants have been described before4. In brief, subjects were on average 62 ± 6 years old and their average BMI was 29.6 ± 2.8 kg/m2. Serum magnesium concentrations tended to increase in the magnesium compared with the placebo group by 0.02 mmol/L (95% CI: 0.00 to 0.04 mmol/L; P = 0.09) after 24 weeks, while twenty-four hour urinary magnesium excretion increased significantly by 2.01 mmol (95% CI: 1.22 to 2.93 mmol; P < 0.001) (Table 1). All subjects from the magnesium group had increased 24-hour urinary magnesium excretion concentrations at the end of the trial. This indicates that compliance of the subjects was excellent, as also evidenced from capsule counts. In fact, based on returned capsules, compliance ranged between 86% and 102%, and was on average >98% for the two treatment groups. No serious adverse events were reported in study diaries. Also, none of the participants has recorded in their study diaries any use of laxatives, which may contain magnesium oxide.
Table 1.
Magnesium concentrations and vascular function measurements at baseline, and after a 12-week and 24-week magnesium or placebo treatment in a randomized controlled trial (RCT) with overweight and obese middle-aged and elderly adults1.
| Magnesium Group | Placebo Group | Treatment Effect | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline2 | 12 weeks2 | 24 weeks2 | Baseline2 | 12 weeks2 | 24 weeks2 | Δ 12 weeks3 | Δ 24 weeks3 | |
| Magnesium concentrations | ||||||||
| Serum Mg, mmol/L | 0.84 ± 0.05 | 0.87 ± 0.05 | 0.86 ± 0.04 | 0.85 ± 0.05 | 0.86 ± 0.04 | 0.85 ± 0.05 | 0.01 (−0.01; 0.04) | 0.02 (0.00; 0.04)# |
| Urinary Mg, mmol/24 h | 4.67 ± 1.15 | N/A | 6.55 ± 1.15 | 4.32 ± 1.44 | N/A | 4.28 ± 2.17 | N/A | 2.01 (1.22; 2.93)## |
| Vascular function | ||||||||
| Brachial artery diameter, cm | 0.38 ± 0.05 | N/A | 0.38 ± 0.05 | 0.38 ± 0.06 | N/A | 0.39 ± 0.07 | N/A | −1.39 (−3.19, 0.41) |
| Brachial artery FMD, % | 3.11 ± 2.68 | N/A | 3.23 ± 2.57 | 3.75 ± 2.90 | N/A | 3.17 ± 2.15 | N/A | 0.49 (−0.38, 1.36) |
| Reactive hyperemia index | 2.41 ± 0.61 | N/A | 2.57 ± 0.63 | 2.64 ± 0.48 | N/A | 2.57 ± 0.49 | N/A | 0.05 (−0.27, 0.37) |
| CRAE, μm | 126 ± 17 | 124 ± 14 | 124 ± 15 | 128 ± 19 | 127 ± 20 | 125 ± 21 | −1 (−4, 2) | 1 (−1, 4) |
| CRVE, μm | 223 ± 17 | 223 ± 15 | 222 ± 16 | 226 ± 19 | 225 ± 19 | 223 ± 21 | 1 (−2, 4) | 1 (−1, 4) |
| Retinal AVR | 0.56 ± 0.06 | 0.56 ± 0.05 | 0.56 ± 0.06 | 0.56 ± 0.06 | 0.56 ± 0.06 | 0.56 ± 0.06 | −0.01 (−0.02, 0.01) | 0.00 (−0.01, 0.01) |
| Endothelial dysfunction | ||||||||
| sVCAM-1, ng/mL | 746 ± 122 | N/A | 742 ± 127 | 725 ± 155 | N/A | 708 ± 99 | N/A | 21 (−23, 65) |
| sICAM-1, ng/mL | 467 ± 75 | N/A | 479 ± 79 | 449 ± 72 | N/A | 425 ± 71 | N/A | 14 (−17, 45) |
| sE-selectin, ng/mL | 9.6 ± 4.5 | N/A | 11.8 ± 4.4 | 9.3 ± 5.0 | N/A | 11.3 ± 5.7 | N/A | 0.3 (−1.7, 2.3) |
1Magnesium group: n = 26; placebo group: n = 25. Mg: magnesium; FMD: flow-mediated vasodilation; CRAE: central retinal arteriolar equivalent; CRVE: central retinal venular equivalent; AVR: arteriolar-to-venular diameter ratio; sVCAM: soluble vascular cell adhesion molecule; sICAM: soluble intercellular adhesion molecule; sE-selectin: soluble endothelial selectin; N/A: not available. 2Values are means ± SDs. 3Values are mean changes (95% CI) obtained from a one-way ANCOVA with baseline value as covariate. Treatment effect: # P < 0.10, ## P < 0.001.
Vascular function markers
After 24 weeks of supplementation, changes in baseline brachial artery diameters were not statistically different between the two treatment groups (Table 1). Also, FMD did not change (Fig. 1). In addition, no effects of long-term magnesium supplementation on the RHI were found. Finally, the central retinal arteriolar equivalent (CRAE), central retinal venular equivalent (CRVE) and the retinal arteriolar-to-venular diameter ratio (AVR) did not change following long-term magnesium supplementation. Table 1 shows effects on plasma markers for microvascular endothelial function. No differences in soluble vascular cell adhesion molecule (sVCAM)-1, soluble intercellular adhesion molecule (sICAM)-1 and soluble endothelial selectin (sE-selectin) concentrations were observed.
Figure 1.
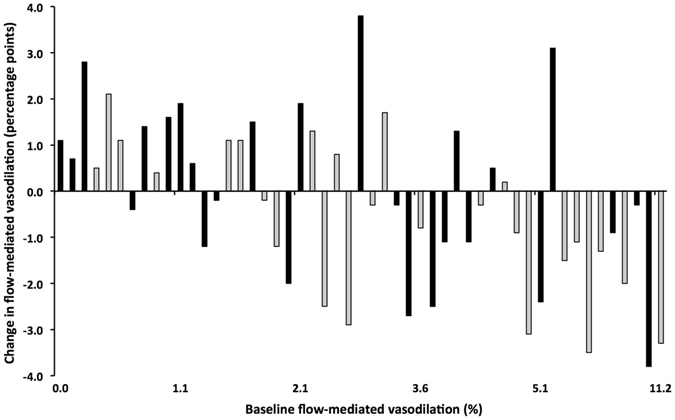
Individual changes in flow-mediated vasodilation. Effects of 24-week magnesium (black) and placebo supplementation (grey) on brachial artery flow-mediated vasodilation in overweight and obese middle-aged and elderly adults.
Cardiometabolic risk markers
Fasting total cholesterol, HDL-cholesterol, LDL-cholesterol, triacylglycerol, non-esterified fatty acid (NEFA), glucose, insulin and HOMAIR did not differ after oral magnesium supplementation compared with the placebo treatment. The effects on plasma markers for low-grade systemic inflammation were also investigated. No effects were found on interleukin (IL)-6, IL-8, tumor necrosis factor (TNF)-α, C-reactive protein (CRP) and serum amyloid A (SAA) (Table 2). One man from the magnesium and four participants from the placebo group had CRP concentrations above 10 μg/mL on one (i.e. three CRP values at the start of the study and one at the end of the placebo treatment) or both occasions. Conclusions did not change when these participants were excluded form the statistical analyses (data not shown).
Table 2.
Cardiometabolic risk measurements at baseline, and after a 12-week and 24-week magnesium or placebo treatment in a randomized controlled trial (RCT) with overweight and obese middle-aged and elderly adults1.
| Magnesium Group | Placebo Group | Treatment Effect | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline2 | 12 weeks2 | 24 weeks2 | Baseline2 | 12 weeks2 | 24 weeks2 | Δ 12 weeks3 | Δ 24 weeks3 | |
| Cardiometabolic risk | ||||||||
| Total cholesterol, mmol/L | 6.26 ± 0.96 | 6.34 ± 0.93 | 6.30 ± 0.97 | 5.70 ± 0.90 | 5.75 ± 0.87 | 5.66 ± 0.73 | 0.13 (−0.16, 0.41) | 0.20 (−0.07, 0.48) |
| HDL-cholesterol, mmol/L | 1.59 ± 0.49 | 1.60 ± 0.46 | 1.58 ± 0.48 | 1.39 ± 0.38 | 1.38 ± 0.32 | 1.36 ± 0.31 | 0.06 (−0.03, 0.14) | 0.06 (−0.04, 0.16) |
| LDL-cholesterol, mmol/L | 4.08 ± 0.79 | 4.10 ± 0.82 | 4.07 ± 0.89 | 3.59 ± 0.76 | 3.67 ± 0.71 | 3.61 ± 0.64 | 0.02 (−0.21, 0.25) | 0.06 (−0.20, 0.32) |
| Triacylglycerol, mmol/L | 1.30 ± 0.51 | 1.40 ± 0.56 | 1.41 ± 0.65 | 1.55 ± 0.65 | 1.55 ± 0.55 | 1.49 ± 0.58 | 0.04 (−0.16, 0.24) | 0.11 (−0.12, 0.34) |
| NEFA, mmol/L5 | 430 ± 145 | 440 ± 144 | 436 ± 146 | 417 ± 126 | 382 ± 160 | 414 ± 145 | 50 (−19, 119) | 15 (−55, 85) |
| Glucose, mmol/L5 | 5.91 ± 0.74 | 5.90 ± 0.80 | 5.97 ± 0.94 | 5.95 ± 0.63 | 5.88 ± 0.62 | 5.89 ± 0.66 | 0.05 (−0.15, 0.25) | 0.12 (−0.09, 0.32) |
| Insulin, uU/mL5 | 12.1 ± 4.7 | 12.2 ± 4.7 | 12.7 ± 6.1 | 15.0 ± 5.3 | 14.1 ± 5.5 | 14.1 ± 6.1 | 0.6 (−1.0, 2.2) | 1.5 (−0.6, 3.6) |
| HOMAIR 5 | 3.19 ± 1.35 | 3.22 ± 1.37 | 3.41 ± 1.77 | 4.03 ± 1.69 | 3.74 ± 1.71 | 3.77 ± 1.86 | 0.23 (−0.22, 0.67) | 0.48 (−0.12, 1.08) |
| Low-grade inflammation | ||||||||
| IL-6, pg/mL4 | 0.76 (0.62–0.97) | N/A | 0.73 (0.65–0.97) | 0.81 (0.64–1.02) | N/A | 0.81 (0.65–1.12) | N/A | −0.07 vs. 0.00 |
| IL-8, pg/mL4 | 3.75 (3.30–4.83) | N/A | 4.55 (3.89–5.88) | 4.28 (3.56–4.72) | N/A | 4.60 (3.88–5.25) | N/A | 0.56 vs. 0.36 |
| TNF-α, pg/mL4 | 2.65 (2.25–2.97) | N/A | 2.72 (2.40–3.16) | 2.71 (2.18–2.96) | N/A | 2.75 (2.29–2.95) | N/A | 0.18 vs. −0.02 |
| CRP, μg/mL4,6 | 1.59 (1.34–3.20) | N/A | 1.77 (1.39–2.30) | 1.72 (1.00–3.14) | N/A | 1.65 (1.06–2.90) | N/A | −0.12 vs. −0.17 |
| SAA, μg/mL4,7 | 3.84 (3.06–5.11) | N/A | 4.45 (3.16–5.46) | 3.79 (2.58–5.30) | N/A | 2.94 (2.42–4.69) | N/A | 0.40 vs. −0.15 |
1Magnesium group: n = 26; placebo group: n = 25. NEFA: non-esterified fatty acid; IL: interleukin; TNF: tumor necrosis factor; CRP: C-reactive protein; SAA: serum amyloid A; N/A: not available. 2Values are means ± SDs or medians (25–75th percentile). 3For normally distributed variables, values are mean changes (95% CI) obtained from a one-way ANCOVA with baseline value as covariate. For non-normally distributed variables, variables are the median of the changes in respectively the magnesium and the placebo group. 4Markers for low-grade systemic inflammation were tested by a Wilcoxon rank-sum test for non-normal distributed data. 5Magnesium group: n = 25; placebo group: n = 25. 6Magnesium group: n = 25; placebo group: n = 21. 7Magnesium group: n = 24; placebo group: n = 22.
Discussion
In this randomized controlled trial (RCT) involving overweight and obese middle-aged and elderly adults, we found no significant effect on FMD, RHI, retinal microvascular caliber and plasma markers for microvascular endothelial function after 24 weeks of daily supplementation with 350 mg magnesium. Also, cardiometabolic risk markers did not change following magnesium supplementation.
The lack of effect on FMD is in agreement with several11, 12, but not all13, earlier randomized, double-blind, placebo-controlled intervention trials examining effects of magnesium supplementation. In a 6-month study in 50 patients with stable coronary artery disease (CAD), a daily magnesium supplement of 365 mg increased FMD by 11.1 pp 13. The observed improvement by Shechter et al.13 is very pronounced and related with an estimated decrease of approximately 90% in the long-term risk to develop CVD20. In retrospect, we had a statistical power of 80% (P < 0.05) to detect a true change in FMD of at least 1.30 pp. Thus, our study was certainly adequately powered to detect such a huge effect. Differences in subject characteristics may have contributed to these inconsistent results. CAD may be associated with magnesium depletion21 and a magnesium-deficient state was indeed found in 36 of the 50 CAD patients13. Also, study participants had low intracellular magnesium concentrations, as assessed in sublingual epithelial cells. In our intervention trial and others involving also apparently healthy individuals11 or patients on hemodialysis12, participants had baseline serum magnesium concentrations within normal ranges. This suggests that a very specific population was studied by Shechter13.
Baseline diameters of the brachial artery did not change in our study. Consequently, changes in brachial diameters cannot explain our lack of effect on FMD. Also, no effects were found on the RHI. The RHI reflects small artery reactivity15, while FMD targets a large peripheral muscular artery14. To date, no other RCT has addressed the effect of magnesium supplementation on the RHI. Taken together, our study does not provide evidence that improvements in endothelial function have contributed to the beneficial effects on arterial stiffness associated with an increased magnesium intake for a 24-week experimental period, as reported previously4. As discussed4, long-term magnesium supplementation may primarily have an impact on the aorta and not on peripheral muscular arteries, possibly as a result of improvements in the structural characteristics of large elastic arterial walls. In fact, longer-term use of magnesium in patients receiving hemodialysis significantly decreased common carotid artery intima-media thickness12, 22, which reflects structural changes of the arterial wall23, without any apparent effects on FMD12.
Magnesium supplementation did also not affect retinal microvascular caliber. To the best of our knowledge, no other RCTs have assessed the effects of magnesium on microvascular diameters. Finally, markers for microvascular endothelial function were investigated in plasma, but no significant effects were observed for sVCAM-1, sICAM-1 and sE-selectin that are involved in the recruitment of leukocytes to the vascular wall24. In agreement, Chacko et al. observed that a daily magnesium supplement of 500 mg for four weeks did not change plasma concentrations of these markers in 14 otherwise healthy overweight individuals10.
Alternate possible mechanisms to explain the beneficial effects of oral magnesium supplementation on arterial stiffness in overweight and obese adults4 may relate to the postulated actions of magnesium on blood pressure and other cardiometabolic risk markers25. However, we have already reported that blood pressure did not change4, while serum lipids and lipoproteins, plasma glucose, insulin sensitivity and plasma markers for low-grade systemic inflammation were also comparable between the two treatment groups. A meta-analysis of nine RCTs involving patients with type II diabetes reported that magnesium supplementation (median daily dose: 360 mg) for 4 to 16 weeks increased HDL-cholesterol, but found no effects on total cholesterol, LDL-cholesterol and triacylglycerol concentrations26. In healthy subjects, however, there is no evidence that an increased dietary magnesium intake improves the serum lipid profile9–11. A recent meta-analysis and systematic review of 21 randomized trials summarized the effects of magnesium supplements (range: 300 to 600 mg/day) on glucose, insulin and HOMAIR in both diabetic and non-diabetic individuals27. Study duration ranged from one to six months. In agreement, no effects were observed on fasting glucose and insulin. However, the HOMAIR significantly decreased suggesting that insulin sensitivity improved following oral magnesium supplementation. These effects were more pronounced in individuals with hypomagnesemia as compared with normomagnesemic subjects, but did not depend on the presence of diabetes. Adults who completed the present trial had serum magnesium concentrations within normal range28, which may explain the lack of effect on the HOMAIR. Finally, no beneficial effects on pro-inflammatory cytokines were found. Similar conclusions were drawn in the very few RCTs that examined effects of magnesium supplementation on systemic inflammation in apparently healthy overweight adults10, 29.
Some limitations of the present trial warrant consideration. Our study was sufficiently powered to detect a change of 1.30 pp in FMD, while we estimated an effect of 0.49 pp (95% CI: −0.38 to 1.36 pp). Although the variability in our study was in line with findings of earlier studies30, we cannot exclude the possibility of false-negative finding. However, other markers of endothelial function did also not change and we therefore do no consider it very likely that oral magnesium supplementation improves endothelial function. Studies on underlying mechanisms are also needed, as the observed beneficial effects on large elastic arterial walls4 may relate to the postulated actions of magnesium on endothelial cells31. In fact, in vitro studies have shown that low extracellular magnesium induces the development of a pro-atherosclerotic phenotype of cultured endothelial cells32. Recent studies also suggest an important role of microRNAs on vascular function33 and the ability of endothelial cells to produce atherogenic catecholamines34. Broadening our knowledge in these novel fields will contribute to our understanding of mechanisms by which an increased oral magnesium intake beneficially affects cardiovascular health outcomes.
In conclusion, the present results indicate that a magnesium intervention for 24 weeks does not improve endothelial function and cardiometabolic risk markers in overweight and obese men and postmenopausal women. It is therefore unlikely that effects on endothelial function have contributed to the beneficial effects on arterial stiffness.
Subjects and Methods
Subjects and study design
Overweight and slightly obese men and postmenopausal women with a mean age of 62 ± 6 years participated in a randomized, double-bind, placebo-controlled, parallel study with a 24-week experimental period, as described previously4. In brief, study subjects were allocated to receive either three times daily magnesium (total dose: 350 mg; Magnesium Citrate Complex [Mg 16%]) or placebo capsules containing starch (Amylum Solani). A total daily dose of 350 mg is considered the tolerable upper intake level (UL) of supplemental magnesium for adults35. All capsules were kindly provided by Laboratorium Medisan B.V. (Heerenveen, The Netherlands). The capsules were prepared in one batch. Participants maintained their habitual diet, physical activity levels and consumption of alcohol throughout the total study period. Inclusion and exclusion criteria have been described before4. Briefly, all volunteers were apparently healthy and did not receive proton pump inhibitors, anti-hypertensive medication or drugs known to affect lipid or glucose metabolism. Fifty-two overweight and obese study subjects were included. They had a BMI between 25 and 35 kg/m2; serum creatinine concentrations <116 μmol/L for men and <101 μmol/L for women; and no indications for treatment with cholesterol-lowering medications36. All study participants gave written informed consent before the start of the trial. The study was approved by the Ethics Committee of Maastricht University Medical Center, and registered on 8 September 2014 at ClinicalTrials.gov as NCT02235805. The methods were performed in accordance with the described procedures in the approved study protocol.
Blood sampling and analyses
Fasting blood samples were taken at the start of the study (days −3 and 0), at week 12 (day 84), and at the end of the study (days 165 and 168) from a forearm vein by venipuncture. On the days preceding blood sampling, participants were requested not to consume alcohol or to perform any strenuous physical exercise. On the morning of blood sampling, subjects arrived after an overnight fast (no food or drink after 08.00 PM, except for water) at the Metabolic Research Unit Maastricht (MRUM) research facilities by public transport or by car to the standardize measurements as much as possible. After blood sampling, NaF-containing vacutainer tubes (Becton, Dickinson and Company, Franklin Lanes, NY, USA) and EDTA-coated vacutainer tubes (Becton, Dickinson and Company) were immediately kept on ice and centrifuged within 30 minutes. To obtain plasma, plasma separator tubes were centrifuged at 1300× g for 15 minutes at 4 °C. Blood drawn in vacutainer serum tubes (Becton, Dickinson and Company) was first allowed to clot for at least 30 minutes at 21 °C. To obtain serum, serum separator tubes were centrifuged at 1300× g for 15 minutes at 21 °C. Following centrifugation, plasma and serum samples were immediately portioned into aliquots and stored at −80 °C until analysis at the end of the trial.
Fasting glucose (Horiba ABX SAS, Montpellier, France) and NEFA concentrations (NEFA kit; WAKO Chemicals GmbH, Neuss, Germany) were measured in NaF-plasma. Fasting serum samples were analyzed for total cholesterol (Cobas 8000; Roche Diagnostics Systems, Hoffmann-La Roche Ltd., Mannheim, Germany), HDL-cholesterol (Cobas 8000; Roche Diagnostics Systems), triacylglycerol (Cobas 8000; Roche Diagnostics Systems), and insulin concentrations (RIA; Millipore, Billerica, MA, USA). LDL-cholesterol was calculated using the Friedewald formula37. The degree of insulin resistance was estimated by calculating the HOMAIR 38. Fasting EDTA-plasma samples were analyzed for markers for low-grade systemic inflammation (IL-6, IL-8, TNF-α, CRP, SAA) and markers for microvascular endothelial function (sVCAM-1, sICAM-1, sE-selectin) by using a multi-array detection system based on electro-chemiluminescence technology (SECTOR Imager 2400; Meso Scale Discovery, Rockville, MD, USA)39.
Vascular function measurements
Measurements were performed at the start of the trial (day 0), at week 12 (day 84), and at the end of the study (day 168) in a quiet and darkened room. The room was temperature controlled at 22 °C. After blood sampling and an acclimatization period of 30 minutes in the supine position, measurements were performed.
FMD was assessed using ultrasound echography (SONOS 5500; Hewlett-Packard [Philips], Andover, MA, USA) and recording of echo images on DVD40. After a 5-minute reference period, the pneumatic cuff placed around the participant's forearm was inflated to 250 mmHg for 5 minutes, causing distal hypoxia. Upon cuff-release reactive hyperemia ensued. The echo images were analyzed offline using a custom-written Matlab program (MyFMD V14.07; Prof. A.P. Hoeks, Department of Biomedical Engineering, Maastricht University Medical Center, Maastricht, The Netherlands). The FMD response was quantified as the maximal percentage change in post occlusion arterial diameter relative to baseline diameter. During FMD measurements, the Endo-PAT 2000 (Itamar Medical Ltd, Caesarea, Israel) was used to measure changes in pulse wave amplitude in response to reactive hyperemia. In brief, a pneumatic probe was placed on the index finger of both hands to record the peripheral arterial tone, according to instructions of the manufacturer. The RHI was quantified as the post-to-pre occlusion peripheral arterial tone signal ratio in the occluded hand, normalized to values in the control hand and then further corrected for baseline vascular tone41. Finally, retinal vascular images were obtained to assess microvascular diameters in the eye. During this test, study participants were seated with their head resting on a chinrest, looking directly into the non-mydriatic retinal camera (Topcon TRC-NW-300; Topcon Co., Tokyo, Japan). The camera focused on the optic disc and photographed the retina. Images were digitized and analyzed to calculate the CRAE, CRVE, and retinal AVR with appropriate software (Generalized Dual-Bootstrap Iterative Closest Point [GDBP-ICP])42. In brief, the software automatically aligns the retinal images based on detected vascular centerlines by iteratively transforming the algorithm. At least two arteriolar and two venular retinal segments were measured and summarized by using the Parr-Hubbard formulas43. These segments had to be the same segments at each time point for an individual.
Statistical analyses
Study results are presented as means ± SDs, unless otherwise indicated. A per protocol analysis was performed. Differences in baseline values between the magnesium and placebo group were tested using an unpaired Student's t test. A one-way ANCOVA, using the baseline measurements of the outcome variables as covariates, was conducted to investigate differences in responses between magnesium and placebo treatments. When residuals were not normally distributed as assessed with the Kolmogorov-Smirnov test, a Wilcoxon rank-sum was used. Changes were then calculated for each individual as the difference between the values at the end of the trial and at the start of the trial. A P < 0.05 was considered statistically significant. The study was powered on carotid-to-femoral pulse wave velocity, which was the primary outcome, but a retrospective power analysis showed that with 51 participants we had 80% power to detect a true change in FMD of at least 1.30 pp. For this power calculation, an alpha of 0.05 and observed within-subject variability in FMD of 1.64 pp were used. Analyses were performed using SPSS 23.0 (SPSS Incorporated, Chicago, IL, USA).
Electronic supplementary material
Acknowledgements
The present study is funded by research grant CH001 from Top Institute of Food and Nutrition (TIFN), a public-private partnership on precompetitive research in food and nutrition. The public partners are responsible for the study design, data collection and analysis, decision to publish, and preparation of the manuscript. The private partners have contributed to the project through regular discussion. We thank D. Luiten and C. Op’t Eyndt for dietary assistance, and M. Hulsbosch for technical support. Finally, we thank our volunteers for their enthusiasm and cooperation. Supported by research grant CH001 from Top Institute of Food and Nutrition (TIFN), a public-private partnership on precompetitive research in food and nutrition. Capsules were provided by Laboratorium Medisan B.V. (Heerenveen, The Netherlands).
Author Contributions
The authors’ responsibilities were as follows; P.J.J.: designed and conducted the trial, performed the statistical analyses, interpreted the data, and wrote the manuscript; J.P.: interpreted the data and wrote the manuscript; S.J.L.B.: interpreted the data and wrote the manuscript; and R.P.M.: designed the trial, interpreted the data, had overall responsibility for the study, and wrote the manuscript. All authors read and approved the final manuscript.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at doi:10.1038/s41598-017-00205-9
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fang X, et al. Dietary magnesium intake and the risk of cardiovascular disease, type 2 diabetes, and all-cause mortality: a dose-response meta-analysis of prospective cohort studies. BMC Med. 2016;14:210. doi: 10.1186/s12916-016-0742-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Del Gobbo LC, et al. Circulating and dietary magnesium and risk of cardiovascular disease: a systematic review and meta-analysis of prospective studies. Am. J. Clin. Nutr. 2013;98:160–173. doi: 10.3945/ajcn.112.053132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Joosten MM, et al. Urinary and plasma magnesium and risk of ischemic heart disease. Am. J. Clin. Nutr. 2013;97:1299–1306. doi: 10.3945/ajcn.112.054114. [DOI] [PubMed] [Google Scholar]
- 4.Joris PJ, Plat J, Bakker SJ, Mensink RP. Long-term magnesium supplementation improves arterial stiffness in overweight and obese adults: results of a randomized, double-blind, placebo-controlled intervention trial. Am. J. Clin. Nutr. 2016;103:1260–1266. doi: 10.3945/ajcn.116.131466. [DOI] [PubMed] [Google Scholar]
- 5.Laurent S, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur. Heart J. 2006;27:2588–2605. doi: 10.1093/eurheartj/ehl254. [DOI] [PubMed] [Google Scholar]
- 6.Wilkinson IB, et al. Nitric oxide regulates local arterial distensibility in vivo. Circulation. 2002;105:213–217. doi: 10.1161/hc0202.101970. [DOI] [PubMed] [Google Scholar]
- 7.Guerrero-Romero F, et al. Oral magnesium supplementation improves insulin sensitivity in non-diabetic subjects with insulin resistance. A double-blind placebo-controlled randomized trial. Diabetes Metab. 2004;30:253–258. doi: 10.1016/S1262-3636(07)70116-7. [DOI] [PubMed] [Google Scholar]
- 8.Paolisso G, et al. Daily magnesium supplements improve glucose handling in elderly subjects. Am. J. Clin. Nutr. 1992;55:1161–1167. doi: 10.1093/ajcn/55.6.1161. [DOI] [PubMed] [Google Scholar]
- 9.Marken PA, et al. Effects of magnesium oxide on the lipid profile of healthy volunteers. Atherosclerosis. 1989;77:37–42. doi: 10.1016/0021-9150(89)90007-5. [DOI] [PubMed] [Google Scholar]
- 10.Chacko SA, et al. Magnesium supplementation, metabolic and inflammatory markers, and global genomic and proteomic profiling: a randomized, double-blind, controlled, crossover trial in overweight individuals. Am. J. Clin. Nutr. 2011;93:463–473. doi: 10.3945/ajcn.110.002949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cosaro E, et al. Effects of magnesium supplements on blood pressure, endothelial function and metabolic parameters in healthy young men with a family history of metabolic syndrome. Nutr. Metab. Cardiovasc. Dis. 2014;24:1213–1220. doi: 10.1016/j.numecd.2014.05.010. [DOI] [PubMed] [Google Scholar]
- 12.Mortazavi M, et al. Effect of magnesium supplementation on carotid intima-media thickness and flow-mediated dilatation among hemodialysis patients: a double-blind, randomized, placebo-controlled trial. Eur. Neurol. 2013;69:309–316. doi: 10.1159/000346427. [DOI] [PubMed] [Google Scholar]
- 13.Shechter M, et al. Oral magnesium therapy improves endothelial function in patients with coronary artery disease. Circulation. 2000;102:2353–2358. doi: 10.1161/01.CIR.102.19.2353. [DOI] [PubMed] [Google Scholar]
- 14.Ellins EA, Halcox JP. Where are we heading with noninvasive clinical vascular physiology? Why and how should we assess endothelial function? Cardiol. Res. Pract. 2011;2011:870132. doi: 10.4061/2011/870132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Poredos P, Jezovnik MK. Testing endothelial function and its clinical relevance. J. Atheroscler. Thromb. 2013;20:1–8. doi: 10.5551/jat.14340. [DOI] [PubMed] [Google Scholar]
- 16.Deanfield JE, Halcox JP, Rabelink TJ. Endothelial function and dysfunction: testing and clinical relevance. Circulation. 2007;115:1285–1295. doi: 10.1161/CIRCULATIONAHA.106.652859. [DOI] [PubMed] [Google Scholar]
- 17.Cohn JN, Quyyumi AA, Hollenberg NK, Jamerson KA. Surrogate markers for cardiovascular disease: functional markers. Circulation. 2004;109:IV31–IV46. doi: 10.1161/01.CIR.0000115207.45378.BC. [DOI] [PubMed] [Google Scholar]
- 18.Beijers HJ, et al. Higher central fat mass and lower peripheral lean mass are independent determinants of endothelial dysfunction in the elderly: the Hoorn study. Atherosclerosis. 2014;233:310–318. doi: 10.1016/j.atherosclerosis.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 19.Despres JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444:881–887. doi: 10.1038/nature05488. [DOI] [PubMed] [Google Scholar]
- 20.Ras RT, Streppel MT, Draijer R, Zock PL. Flow-mediated dilation and cardiovascular risk prediction: a systematic review with meta-analysis. Int. J. Cardiol. 2013;168:344–351. doi: 10.1016/j.ijcard.2012.09.047. [DOI] [PubMed] [Google Scholar]
- 21.Seelig M. Cardiovascular consequences of magnesium deficiency and loss: pathogenesis, prevalence and manifestations-magnesium and chloride loss in refractory potassium repletion. Am. J. Cardiol. 1989;63:4G–21G. doi: 10.1016/0002-9149(89)90213-0. [DOI] [PubMed] [Google Scholar]
- 22.Turgut F, et al. Magnesium supplementation helps to improve carotid intima media thickness in patients on hemodialysis. Int. Urol. Nephrol. 2008;40:1075–1082. doi: 10.1007/s11255-008-9410-3. [DOI] [PubMed] [Google Scholar]
- 23.Lorenz MW, et al. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. 2007;115:459–467. doi: 10.1161/CIRCULATIONAHA.106.628875. [DOI] [PubMed] [Google Scholar]
- 24.Calder PC, et al. A consideration of biomarkers to be used for evaluation of inflammation in human nutritional studies. Br. J. Nutr. 2013;109:S1–S34. doi: 10.1017/S0007114512005119. [DOI] [PubMed] [Google Scholar]
- 25.Cunha AR, Umbelino B, Correia ML, Neves MF. Magnesium and vascular changes in hypertension. Int. J. Hypertens. 2012;2012:754250. doi: 10.1155/2012/754250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Song Y, He K, Levitan EB, Manson JE, Liu S. Effects of oral magnesium supplementation on glycaemic control in Type 2 diabetes: a meta-analysis of randomized double-blind controlled trials. Diabet. Med. 2006;23:1050–1056. doi: 10.1111/j.1464-5491.2006.01852.x. [DOI] [PubMed] [Google Scholar]
- 27.Simental-Mendia LE, Sahebkar A, Rodriguez-Moran M, Guerrero-Romero F. A systematic review and meta-analysis of randomized controlled trials on the effects of magnesium supplementation on insulin sensitivity and glucose control. Pharmacol. Res. 2016;111:272–282. doi: 10.1016/j.phrs.2016.06.019. [DOI] [PubMed] [Google Scholar]
- 28.Heil, W. & Ehrhardt, V. Reference ranges for adults and children. Pre-analytical considerations in Roche Diagnostics 9th Edition (2008).
- 29.Moslehi N, Vafa M, Rahimi-Foroushani A, Golestan B. Effects of oral magnesium supplementation on inflammatory markers in middle-aged overweight women. J. Res. Med. Sci. 2012;17:607–614. [PMC free article] [PubMed] [Google Scholar]
- 30.van Mil AC, et al. Impact of volunteer-related and methodology-related factors on the reproducibility of brachial artery flow-mediated vasodilation: analysis of 672 individual repeated measurements. J. Hypertens. 2016;34:1738–1745. doi: 10.1097/HJH.0000000000001012. [DOI] [PubMed] [Google Scholar]
- 31.Maier JA, Malpuech-Brugère C, Zimowska W, Rayssiguier Y, Mazur A. Low magnesium promotes endothelial cell dysfunction: implications for atherosclerosis, inflammation and trombosis. Biochim. Biophys. Acta. 2004;1689:13–21. doi: 10.1016/j.bbadis.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 32.Maier JA. Endothelial cells and magnesium: implications in atherosclerosis. Clin. Sci. (Lond.) 2012;122:397–407. doi: 10.1042/CS20110506. [DOI] [PubMed] [Google Scholar]
- 33.Santulli G. MicroRNAs and Endothelial (Dys) Function. J. Cell Physiol. 2016;231:1638–1644. doi: 10.1002/jcp.25276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sorriento D, et al. Endothelial cells are able to synthesize and release catecholamines both in vitro and in vivo. Hypertension. 2012;60:129–136. doi: 10.1161/HYPERTENSIONAHA.111.189605. [DOI] [PubMed] [Google Scholar]
- 35.Institute of Medicine (US). Dietary reference intakes: calcium, phosphorus, magnesium, vitamin D, and fluoride In The National Academies, 190–249 (1997). [PubMed]
- 36.van Dis L, Geleijnse JM, Verschuren WM, Kromhout D. Cardiovascular risk management of hypertension and hypercholesterolaemia in the Netherlands: from unifactorial to multifactorial approach. Neth. Heart J. 2012;20:320–325. doi: 10.1007/s12471-012-0268-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 1972;8:499–502. [PubMed] [Google Scholar]
- 38.Matthews DR, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 39.Stam F, et al. Impaired renal function is associated with markers of endothelial dysfunction and increased inflammatory activity. Nephrol. Dial. Transplant. 2003;18:892–898. doi: 10.1093/ndt/gfg080. [DOI] [PubMed] [Google Scholar]
- 40.Corretti MC, et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J. Am. Coll. Cardiol. 2002;39:257–265. doi: 10.1016/S0735-1097(01)01746-6. [DOI] [PubMed] [Google Scholar]
- 41.Axtell AL, Gomari FA, Cooke JP. Assessing endothelial vasodilator function with the Endo-PAT 2000. J. Vis. Exp. 2010;44:e2167. doi: 10.3791/2167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stewart CV, Tsai CL, Roysam B. The dual-bootstrap iterative closest point algorithm with application to retinal image registration. IEEE Trans. Med. Imaging. 2003;22:1379–1394. doi: 10.1109/TMI.2003.819276. [DOI] [PubMed] [Google Scholar]
- 43.Hubbard LD, et al. Methods for evaluation of retinal microvascular abnormalities associated with hypertension/sclerosis in the Atherosclerosis Risk in Communities Study. Ophthalmology. 1999;106:2269–2280. doi: 10.1016/S0161-6420(99)90525-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


