Abstract
BACKGROUND
Venous thromboembolism (VTE) is a potentially fatal complication of orthopedic surgery, and until recently, few antithrombotic compounds were available for postoperative thromboprophylaxis. The introduction of the non–vitamin K antagonists oral anticoagulants (NOAC), including apixaban, has extended the therapeutic armamentarium in this field. Therefore, estimation of NOAC net clinical benefit in comparison with the established treatment is needed to inform clinical decision making.
OBJECTIVES
Systematic review to assess the efficacy and safety of apixaban 2.5 mg twice a day versus low-molecular-weight heparins (LMWH) for thromboprophylaxis in patients undergoing knee or hip replacement.
DATA SOURCES
MEDLINE, Embase, and CENTRAL were searched from inception to September 2016, other systematic reviews, reference lists, and experts were consulted.
STUDY ELIGIBILITY CRITERIA, PARTICIPANTS, AND INTERVENTION
All major orthopedic surgery randomized controlled trials comparing apixaban 2.5 mg twice daily with LMWH, reporting thrombotic and bleeding events.
DATA EXTRACTION
Two independent reviewers, using a predetermined form.
STUDY APPRAISAL AND SYNTHESIS METHODS
The Cochrane tool to assess risk bias was used by two independent authors. RevMan software was used to estimate pooled risk ratio (RR) and 95% confidence intervals (95% CI) using random-effects meta-analysis. Trial sequential analysis (TSA) was performed in statistical significant results to evaluate whether cumulative sample size was powered for the obtained effect. Overall confidence in cumulative evidence was assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) Working Group methodology.
RESULTS
Four studies comparing apixaban 2.5 mg twice daily with LMWH were included, with a total of 11.828 patients (55% undergoing knee and 45% hip replacement). The overall risk of bias across studies was low. In comparison with LMWH (all regimens), apixaban showed a significantly lower risk of VTE events and overall mortality combined (RR: 0.63, 95% CI: 0.42–0.95, I2 = 84%, n = 8346), but not of major VTE events (RR: 0.62, 95% CI: 0.32–1.19, I2 = 63%, n = 9493), or of symptomatic VTE events and VTE-related mortality combined (RR: 1.14, 95% CI: 0.68–1.90, I2 = 0%, n = 11 879). Trial sequential analysis showed that the risk reduction obtained for VTE and mortality was based on underpowered cumulative sample size and effect dimension. Subgroup analysis according to LMWH regimens showed that apixaban reduced the risk of VTE events and overall mortality, and major VTE events, when compared with LMWH once daily, without differences between apixaban and LMWH twice daily.
CONCLUSIONS
There is low to moderate evidence that in patients undergoing knee or hip replacement, apixaban seems equally effective and safe to LMWH twice a day. When compared with LMWH once a day, apixaban seems a superior thromboprophylaxis option. However, the results are underpowered which precludes definite answers regarding the true net clinical benefit of apixaban versus LMWH in this clinical context.
Keywords: Venous thromboembolism, non–vitamin K oral anticoagulants, apixaban, heparin, low-molecular-weight, systematic review
Introduction
Venous thromboembolic events (VTEs), such as deep venous thrombolysis and pulmonary embolism (PE), are potentially fatal complications of orthopedic surgery, whose incidence may reach 30% of the patients undergoing knee or hip replacement.1 Furthermore, nonfatal events are frequent and are associated with significant morbidity. The development and clinical launch of new oral anticoagulants also called non–vitamin K antagonist oral anticoagulants (NOACs) has increased the limited arsenal of antithrombotic therapeutic options available for postsurgical thromboprophylaxis for patients undergoing orthopedic surgeries.2
Non–vitamin K antagonist oral anticoagulants selectively inhibit thrombin or factor Xa, and their oral regimen and absence of regular hemostatic parameters evaluation represent a significant advancement of antithrombotic treatment compared with parenteral anticoagulants such as low-molecular-weight heparin (LMWH) and vitamin K antagonists. As occurs with any patient treated with anticoagulants, the main objective is to offer the treatment that provides the best net clinical benefit outcome, that is, which concedes the best balance between thromboembolism prevention and with minimal bleeding risk.3
The aim of this work was to assess the efficacy and safety of apixaban (a Xa inhibitor) at 2.5 mg twice a day (the European Medicines Agency and Food and Drug Administration–approved dosage in VTE prevention in orthopedic patients) in comparison with LMWH for thromboprophylaxis in patients undergoing knee or hip replacement to help informing the process of clinical decision making.
Methods
Protocol and registration
This systematic review was reported in line with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.4 Reporting of statistical data followed Statistical Analyses and Methods in the Published Literature (SAMPL) guidelines.5
Eligibility criteria
We adopted a methodology similar to previously published articles.6–8 All phase 3 randomized controlled trials (RCTs) comparing apixaban against LMWH in patients submitted to major orthopedic surgery were included. All published RCTs were considered for inclusion irrespective of background therapy, treatment duration, or follow-up. Only trials reporting thrombotic events and/or fatal and nonfatal bleeding events were included. Our outcomes of interest were as follows: risk of VTE and all-cause mortality (primary efficacy outcome), major VTE, symptomatic VTE and VTE-related mortality, major bleeding (primary safety outcome), and surgery site bleeding. We used the International Society of Thrombosis and Haemostasis definition for major bleeding.9
Information sources and search method
Records of potentially eligible studies were identified through an electronic search of bibliographic databases from inception to September 2016 (MEDLINE, Embase, and CENTRAL at Cochrane Library). Search strategy details are provided in Supplementary Data 1. No language restrictions were applied. We screened, cross-checked, and identified systematic reviews and meta-analyses evaluating NOACs, as well as reference lists of reports of potential eligible studies.
Study selection, data collection process, and data items
Titles and abstract of records obtained from the search process were screened by 2 investigators (D.C. and F.B.R.). Doubts and disagreements were solved by consensus. Whenever needed a third element was consulted (J.C.). Selected studies were assessed in full text to determine its appropriateness for inclusion. Data from included studies were independently extracted by 2 authors (D.C. and F.B.R.) to a prepiloted electronic form. Retrieved data items were as follows: study design, year of publication, patients’ characteristics, interventions tested, studies’ outcomes, and data of required outcomes. Data were double-checked for software entry before analyses by an additional author (J.C.).
Risk of bias in individual studies
We used the Cochrane tool for assessing risk of bias of included studies.10 The 6 predefined specific domains of analysis were as follows: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, and selective reporting. For-profit bias domain was added. Two independent review authors (D.C. and F.B.R.) performed critical assessments for each domain of the risk of bias tool. Any disagreement was solved by discussion between the 2 reviewers and, if necessary, reached consensus with the participation of a third reviewer (J.C.). The risk of bias was qualitatively evaluated as high, unclear, or low risk. Risk of bias graphs were derived from these tools.
Summary measures
All outcomes data were summarized as dichotomous data. The effect measurement estimate chosen was risk ratio (RR) because relative estimates are more similar across studies with different designs, populations, and lengths of follow-up than absolute effects.11
Synthesis results
We used RevMan 5.3.3 software (The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) for statistical analysis and to derive forest plot showing the results of individual studies and pooled analysis. We compared apixaban 2.5 mg twice a day with LMWH, through random-effects meta-analysis weighted by the Mantel-Haenszel method to estimate pooled RR and 95% confidence intervals (95% CI). Heterogeneity measured as the percentage of total variation between studies due to heterogeneity was assessed through the I2 test.12 We used random-effects model independently of the existence (I2 ⩾ 50%) or not of substantial heterogeneity between studies’ results because we pooled results of studies with different designs and patients’ characteristics. When significant differences were found, we also determined the number needed to treat (NNT) and 95% CI taking into account the baseline risk (proportion of event rate in control group).10 Prespecified sensitivity (by excluding studies at a higher risk of bias) and/or subgroup (by considering different regimens of LMWH) analyses were performed to explain and explore the outcome estimates potentially associated with statistical and/or clinical heterogeneity.
Trial sequential analyses (TSAs) were performed for primary outcomes using TSA version 0.9 beta (Copenhagen Trial Unit, Centre for Clinical Intervention Research, Copenhagen, Denmark, 2011) to explore whether cumulative data were adequately powered to evaluate outcomes.13,14 The required information size and the O’Brien-Fleming adjacent trial sequential alpha spending monitoring boundaries were calculated based on a 2-sided 5% risk of a type I error, 20% risk of a type II error (power of 80%), risk reduction based on pooled analysis, the weighted incidence of events in the control group, and heterogeneity. Power of the primary outcomes findings was interpreted if significance was reached with either a minimum sample size or crossing trial sequential alpha spending monitoring boundary.
Assessment of confidence in cumulative evidence
As recommended by the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) Working Group methodology,15,16 2 reviewers independently assessed all the critical outcomes in the following domains: risk of bias, inconsistency, indirectness, imprecision, and publication bias. In case of disagreement, the authors reached consensus, consulting an independent third review, if necessary. For this purpose, we used the GRADEprofiler (GRADEpro) software tool, which was then extracted into the form of a summary of findings table for inclusion into the review manuscript. We applied the standard definitions of the quality of evidence17 and explicit criteria to ensure the consistency and reproducibility of GRADE judgments for each domain and for all key comparisons of the critical outcomes (Supplementary Data 2).
Results
Study selection
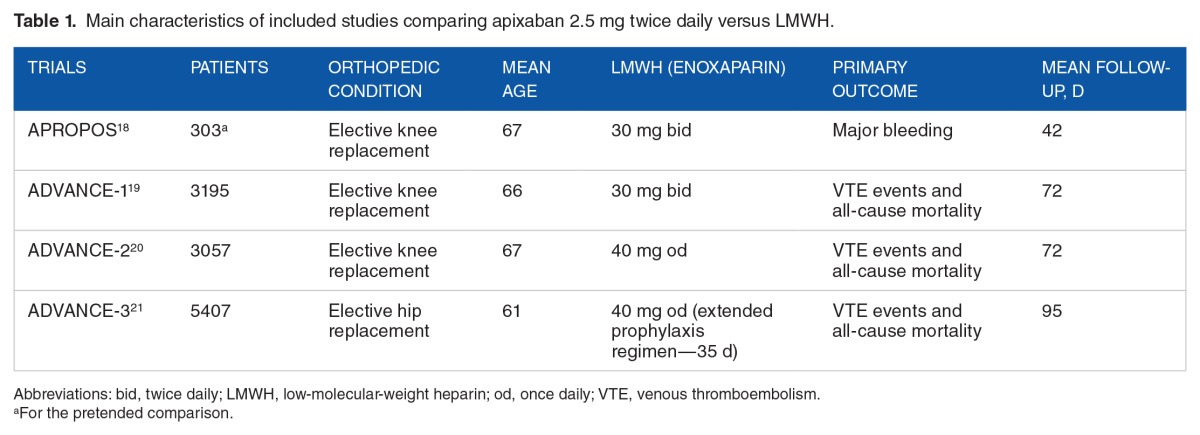
Overall, 1161 references were retrieved from the electronic search (425 MEDLINE, 492 Embase, and 244 CENTRAL). After manual and automatic deduplication, 743 titles and abstracts were screened for full-text review (Figure 1). Four studies with overall 11 828 patients undergoing knee (55%; 6496 patients) or hip replacement (45%; 5332 patients), treated with apixaban 2.5 mg twice daily or LMWH (2 studies with enoxaparin 40 mg once daily, and 2 studies with enoxaparin 30 mg twice daily), were selected to be included.18–21 Their main features are briefly characterized in Table 1.
Figure 1.
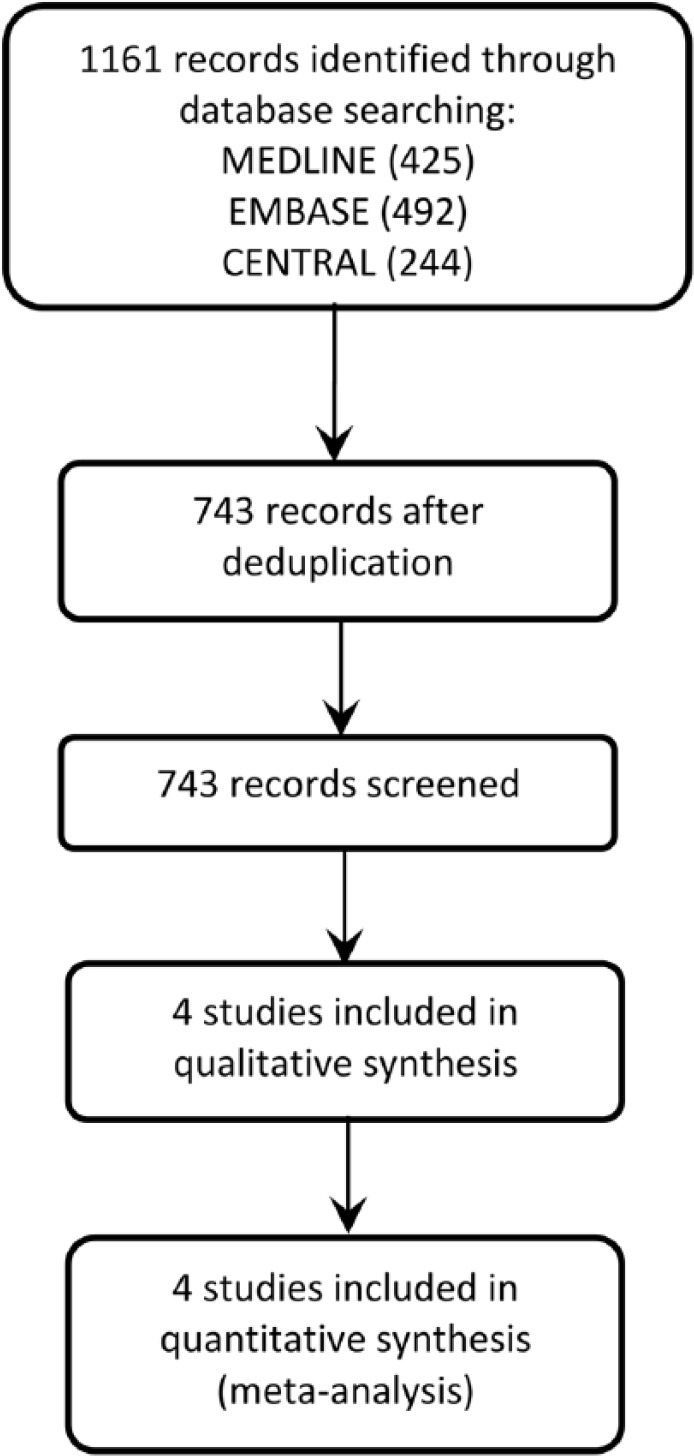
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart of studies selection.
Table 1.
Main characteristics of included studies comparing apixaban 2.5 mg twice daily versus LMWH.
Risk of bias within studies
The overall risk of bias across studies was low (Figure 2). No study had high or low risk of bias for every evaluated domain. One study (APROPOS18) did not report the methods of randomization. All studies used a centralized method for patient allocation. The blinding of participants, study personnel, and outcome assessors was of low risk of bias across RCTs. In a single study (APROPOS), it was not possible to evaluate the influence of the imbalances present on some of treatment arm in the study results. All studies were of high risk of for-profit bias because the studies were funded and sponsored by the companies who owned apixaban’s patent, but one (APROPOS), where study funding was not declared.
Figure 2.
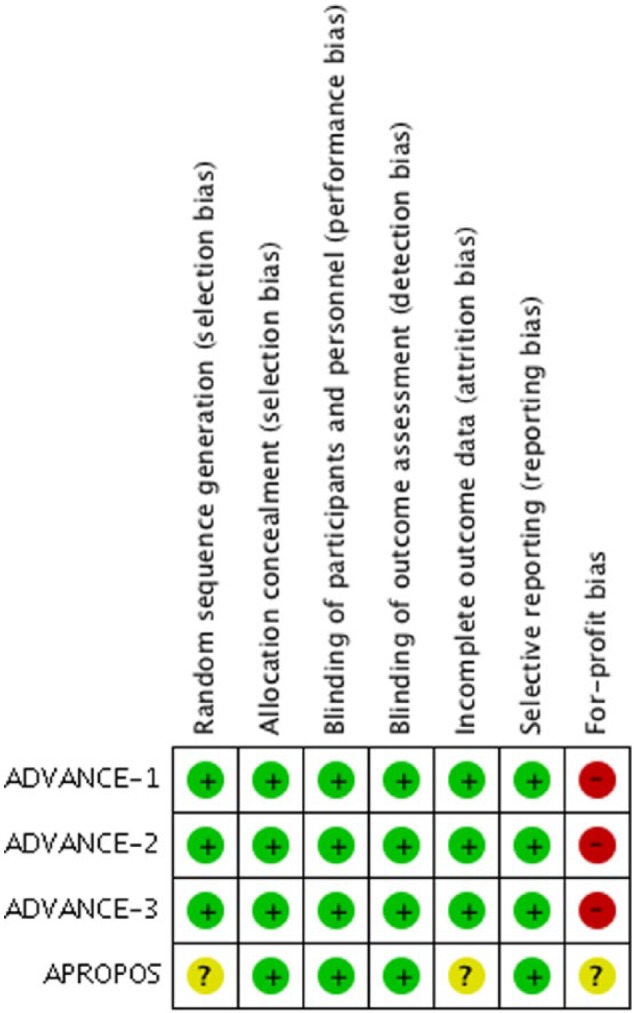
Risk of bias graph.
Synthesis of results
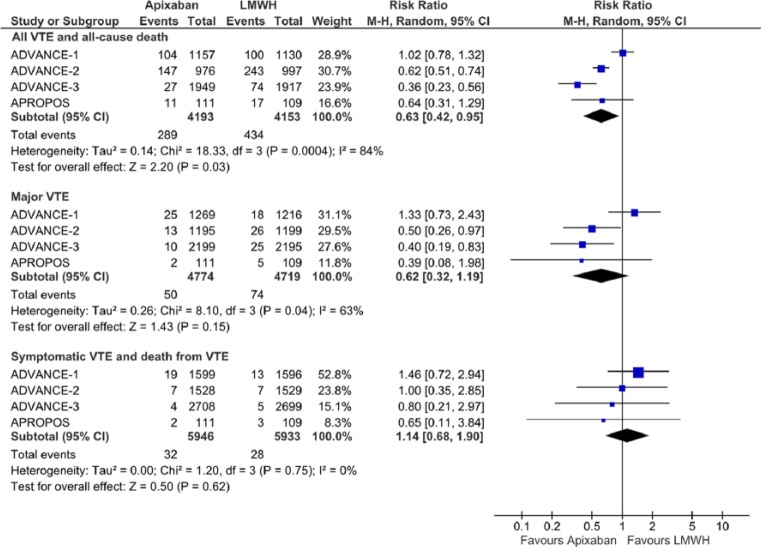
Apixaban 2.5 mg showed a 37% significant risk reduction (RR: 0.63, 95% CI: 0.42–0.95) of the composite outcome of all VTE events or mortality (Figure 3) in comparison with LMWH. According to this estimate, the NNT with apixaban would be 26 patients (95% CI: 16–190) for a weighted mean period of 73 days.
Figure 3.
Forest plot for efficacy outcomes.
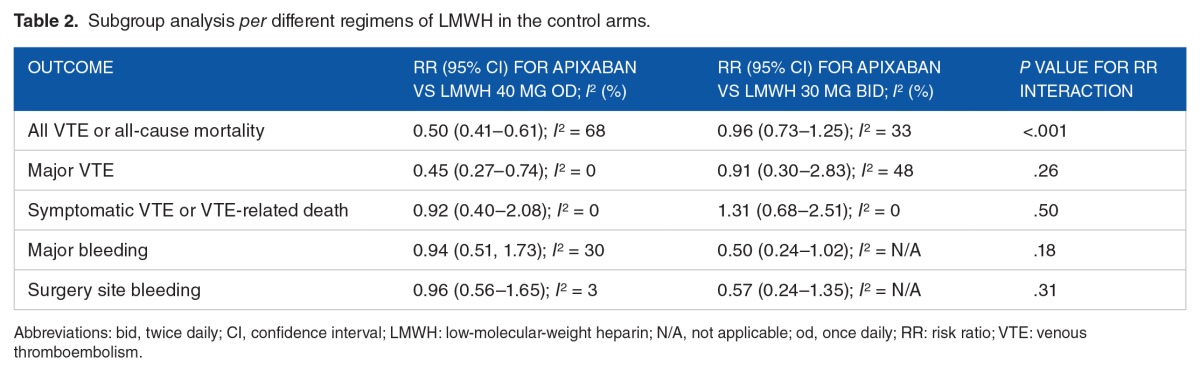
However, the statistical heterogeneity was very high (I2 = 84%) which can be partially attributed to the different regimens of LMWH (enoxaparin) in the control arms. In subgroup analysis, apixaban significantly reduced VTE events or mortality compared with once-daily LMWH regimens (RR: 0.50, 95% CI: 0.41–0.61; I2 = 68%), but no significant difference was found when comparing with twice-daily LMWH regimens (RR: 0.96, 95% CI: 0.73–1.25, I2 = 33%) (Table 2).
Table 2.
Subgroup analysis per different regimens of LMWH in the control arms.
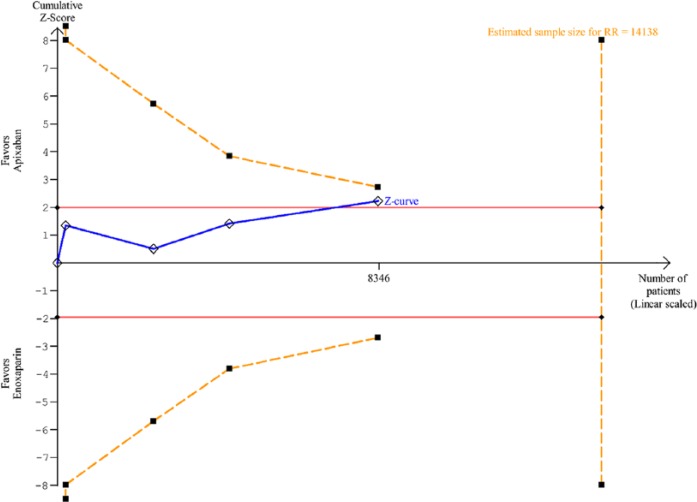
Regarding TSA analysis, RR reduction (RRR) of 37% was assumed based on the RR of 0.63 found in the meta-analysis for VTE and all-cause mortality. The cumulative evidence reached 59% of minimum information size required (14 138 patients) adjusted for the obtained RRR and heterogeneity (Figure 4). As statistical significance was obtained before the information size has been reached, it was important to evaluate whether an adjustment of significance boundaries (O’Brien-Fleming boundaries) to the sample size still results in statistical significant estimates. The TSA graph shows that cumulative estimates were not robust enough to determine the premature statistically significant results (ie, the blue line did not cross the dotted orange line in Figure 4).
Figure 4.
Trial sequential analysis for all venous thromboembolism events and all-cause mortality. RR indicates risk ratio.
Considering the risk of major VTE, there were no differences between apixaban and LMWH (RR: 0.62, 95% CI: 0.32–1.19) (Figure 3). Similar to the results found for the primary efficacy outcome, substantial statistical heterogeneity was also noticed (I2 = 63%). Subgroup analysis according to LMWH regimens showed a significant risk reduction in major VTE of apixaban compared with once-daily LMWH (RR: 0.45, 95% CI: 0.27–0.74; I2 = 0%), but no significant differences when compared with twice-daily LMWH (RR: 0.91, 95% CI: 0.30–2.83; I2 = 48%).
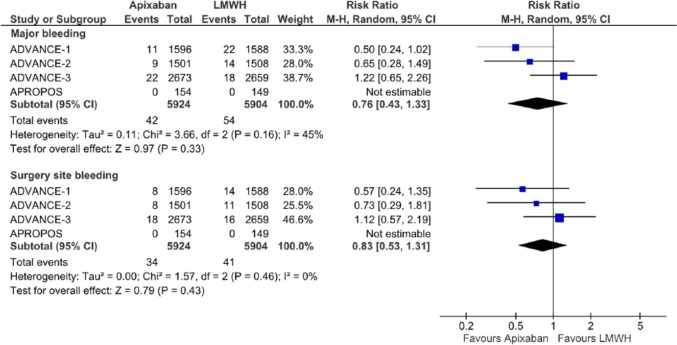
The overall risk of symptomatic VTE and VTE-related death, major bleeding, and surgery site bleeding was not different between apixaban and LMWH (considering all regimens) (Figures 3 and 5).
Figure 5.
Forest plot for safety/bleeding outcomes. CI indicates confidence interval; LMWH, low-molecular-weight heparin.
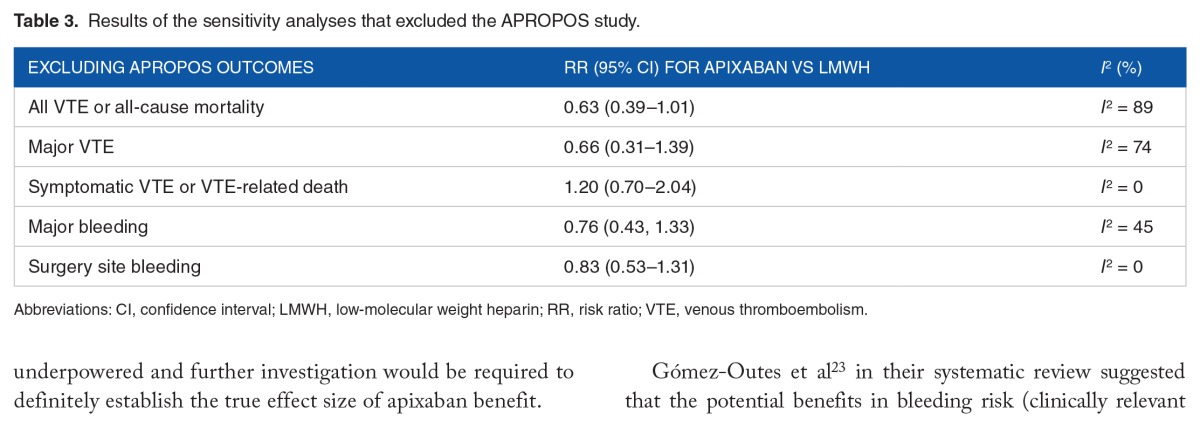
The sensitivity analyses excluded the APROPOS study which was the only phase 2 trial and the only study with an unclear risk of bias in 3 of the 7 items analyzed. Such sensitivity analyses did not result in any statistically significant results, and statistical heterogeneity did not change substantially for all outcomes’ estimates (Table 3).
Table 3.
Results of the sensitivity analyses that excluded the APROPOS study.
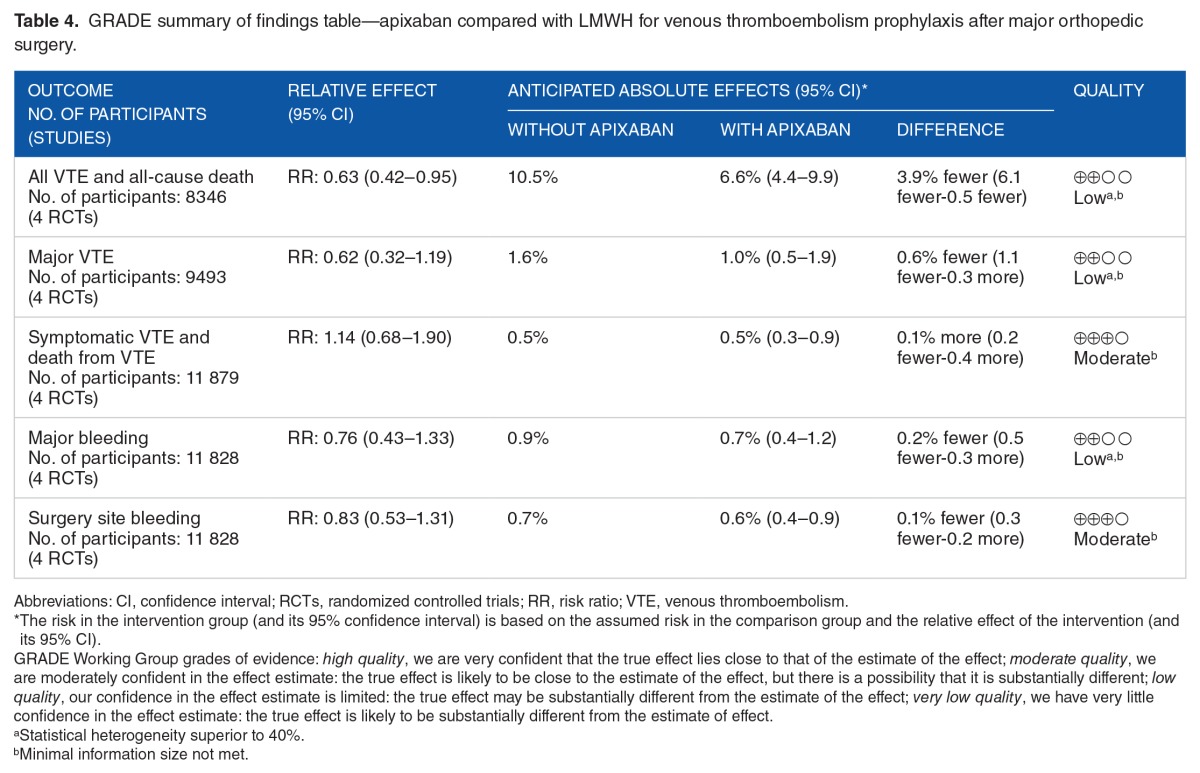
Table 4 details the GRADE approach for the quality of the available evidence which was considered to be low to moderate.
Table 4.
GRADE summary of findings table—apixaban compared with LMWH for venous thromboembolism prophylaxis after major orthopedic surgery.
Discussion
The main findings of this review were as follows: (1) there is low to moderate quality evidence comparing apixaban with LMWH; (2) apixaban 2.5 twice daily decreases the risk of VTE or all-cause mortality, and major VTE, mostly due to the results of trials comparing apixaban with once-daily 30 mg enoxaparin; (3) this risk reduction is, however, underpowered according to the TSA analysis; (4) the risk of symptomatic VTE and VTE-related death with apixaban was similar to LMWH; (5) there were no significant differences between both interventions concerning major bleeding and surgery site bleeding events.
The interpretation of current data is not as optimistic as reported in a previous systematic review.22 Despite the overall statistical significant reduction in the risk of VTE and all-cause mortality, it seems reasonable to assume that this difference was mainly driven by the risk of major VTE, particularly in comparison with the “European” once-daily regimen of enoxaparin, which may be an important gain in the care of these patients. It is important to state that the significance of such outcome and risk reduction estimates are underpowered and further investigation would be required to definitely establish the true effect size of apixaban benefit.
Gómez-Outes et al23 in their systematic review suggested that the potential benefits in bleeding risk (clinically relevant bleeding) and potential prothrombotic effects (particularly PE) could be the result from delaying the administration of apixaban first postoperative dose for 18 hours. Our data show that major bleeding and surgical site bleeding risks are similar between apixaban and enoxaparin regimens, and that major VTE was not increased with apixaban, despite the trend toward a protective effect. Furthermore, as occurs with all NOACs, there is a significant decrease in intracranial hemorrhage, and the pharmacokinetic and pharmacodynamic profiles of these drugs,7 including apixaban, disclose a predictable anticoagulant effect, thereby dismissing regular evaluations of hemostatic parameters.
Overall, apixaban 2.5 mg twice daily seems to be a valuable option for the thromboprophylaxis of patients undergoing elective knee or hip replacement.
There are still some unanswered questions, such as the existence or not of net clinical benefits of apixaban compared with LMWH twice daily (besides the intracranial hemorrhage risk reduction7), and the optimal timing for apixaban administration after surgery, as well as the optimal treatment duration for each condition (knee or hip replacement). It is still unknown whether using an ultraspecific factor Xa/thrombin tests for LMWH monitoring (4 hours after the administration) could improve the outcomes in the control arm, as suggested for some subgroups of patients with venous thromboembolism.
The results of this review should be interpreted in line with the limitations inherent to systematic reviews and meta-analysis. The heterogeneity in the anticoagulation duration and in controls somehow impairs the robustness of the presented data. The comparators were also different as low-dose enoxaparin (30 mg) was given twice daily in 1 trial, whereas the remaining trials engaged for a once-daily 40 mg of enoxaparin for thromboprophylaxis. The follow-up was different according to the conditions (trials ended earlier in the knee replacement studies) as well as the measurement of outcomes that required examinations such as venography.
These limitations may at least partially explain to some extent the high statistical heterogeneity found in most efficacy outcomes. Even though we consider the results are reassuring for efficacy and safety.
Despite the available data and previous meta-analysis, none of them had analyzed the power of the significant results obtained in their meta-analysis. Therefore, the methods and conclusions derived from TSA are important for elucidating the robustness of the data regarding apixaban efficacy in patients undergoing major elective orthopedic surgeries such as knee or hip replacement.
Conclusions
Apixaban 2.5 mg twice daily is a valuable and practical option for thromboprophylaxis with bleeding risks similar to LMWH and an efficacy likely to be better than current enoxaparin regimens.
Footnotes
PEER REVIEW: Four peer reviewers contributed to the peer review report. Reviewers’ reports totaled 351 words, excluding any confidential comments to the academic editor.
FUNDING: The author(s) received no financial support for the research, authorship, and/or publication of this article.
DECLARATION OF CONFLICTING INTERESTS: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions
DC contributed to the concept and design, data acquisition, data analysis, and interpretation of the data; wrote the first draft of the manuscript; critically revised the manuscript; and gave final approval of the submitted manuscript. FR contributed to the data analysis and interpretation; contributed for the first draft; critically revised the manuscript; and gave final approval of the submitted manuscript. JC contributed to the concept and design, and interpretation of the data; critically revised the manuscript; and gave final approval of the submitted manuscript. FJP and JJF contributed to the interpretation of data, critically revised the manuscript, and gave final approval of the submitted manuscript. DC and JC are the guarantors.
REFERENCES
- 1.Geerts WH, Bergqvist D, Pineo GF, et al. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition) Chest. 2008;133:381S–453S. doi: 10.1378/chest.08-0656. [DOI] [PubMed] [Google Scholar]
- 2.Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e278S–e325S. doi: 10.1378/chest.11-2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Caldeira D, Costa J, Ferreira JJ, Pinto FJ. Net clinical benefit outcome should be standardized in trials evaluating antithrombotic drugs: the example of NOACs in atrial fibrillation. Int J Cardiol. 2014;174:405–406. doi: 10.1016/j.ijcard.2014.04.051. [DOI] [PubMed] [Google Scholar]
- 4.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lang TA, Altman DG. Science Editors’ Handbook. European Association of Science Editors; 2013. Basic statistical reporting for articles published in Biomedical Journals: the “Statistical Analyses and Methods in the Published Literature” or The SAMPL Guidelines. http://www.equator-network.org/wp-content/uploads/2013/07/SAMPL-Guidelines-6-27-13.pdf. [DOI] [PubMed] [Google Scholar]
- 6.Caldeira D, Barra M, Santos AT, et al. Risk of drug-induced liver injury with the new oral anticoagulants: systematic review and meta-analysis. Heart. 2014;100:550–556. doi: 10.1136/heartjnl-2013-305288. [DOI] [PubMed] [Google Scholar]
- 7.Caldeira D, Barra M, Pinto FJ, Ferreira JJ, Costa J. Intracranial hemorrhage risk with the new oral anticoagulants: a systematic review and meta-analysis. J Neurol. 2015;262:516–522. doi: 10.1007/s00415-014-7462-0. [DOI] [PubMed] [Google Scholar]
- 8.Caldeira D, Barra M, David C, Costa J, Ferreira JJ, Pinto FJ. The prevalence of oral anticoagulation in patients with atrial fibrillation in Portugal: systematic review and meta-analysis of observational studies. Rev Port Cardiol. 2014;33:555–560. doi: 10.1016/j.repc.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 9.Schulman S, Kearon C. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005;3:692–694. doi: 10.1111/j.1538-7836.2005.01204.x. [DOI] [PubMed] [Google Scholar]
- 10.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. 510 ed. Hoboken, NJ: John Wiley & Sons; 2011. [Google Scholar]
- 11.Deeks JJ. Issues in the selection of a summary statistic for meta-analysis of clinical trials with binary outcomes. Stat Med. 2002;21:1575–1600. doi: 10.1002/sim.1188. [DOI] [PubMed] [Google Scholar]
- 12.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 13.Brok J, Thorlund K, Gluud C, Wetterslev J. Trial sequential analysis reveals insufficient information size and potentially false positive results in many meta-analyses. J Clin Epidemiol. 2008;61:763–769. doi: 10.1016/j.jclinepi.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 14.Caldeira D, Rodrigues FB, Barra M, et al. Non-vitamin K antagonist oral anticoagulants and major bleeding-related fatality in patients with atrial fibrillation and venous thromboembolism: a systematic review and meta-analysis. Heart. 2015;101:1204–1211. doi: 10.1136/heartjnl-2015-307489. [DOI] [PubMed] [Google Scholar]
- 15.Alonso-Coello P, Oxman AD, Moberg J, et al. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: clinical practice guidelines. BMJ. 2016;353:i2089. doi: 10.1136/bmj.i2089. [DOI] [PubMed] [Google Scholar]
- 16.Alonso-Coello P, Schunemann HJ, Moberg J, et al. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: introduction. BMJ. 2016;353:i2016. doi: 10.1136/bmj.i2016. [DOI] [PubMed] [Google Scholar]
- 17.Balshem H, Helfand M, Schunemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64:401–406. doi: 10.1016/j.jclinepi.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 18.Lassen MR, Davidson BL, Gallus A, Pineo G, Ansell J, Deitchman D. The efficacy and safety of apixaban, an oral, direct factor Xa inhibitor, as thromboprophylaxis in patients following total knee replacement. J Thromb Haemost. 2007;5:2368–2375. doi: 10.1111/j.1538-7836.2007.02764.x. http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/373/CN-00619373/frame.html. [DOI] [PubMed] [Google Scholar]
- 19.Lassen MR, Raskob GE, Gallus A, Pineo G, Chen D, Portman RJ. Apixaban or enoxaparin for thromboprophylaxis after knee replacement. N Engl J Med. 2009;361:594–604. doi: 10.1056/NEJMoa0810773. http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/569/CN-00700569/frame.html. [DOI] [PubMed] [Google Scholar]
- 20.Lassen MR, Raskob GE, Gallus A, Pineo G, Chen D, Hornick P, ADVANCE-2 Investigators Apixaban versus enoxaparin for thromboprophylaxis after knee replacement (ADVANCE-2): a randomised double-blind trial. Lancet. 2010;375:807–815. doi: 10.1016/S0140-6736(09)62125-5. [DOI] [PubMed] [Google Scholar]
- 21.Lassen MR, Gallus A, Raskob GE, Pineo G, Chen D, Ramirez LM, ADVANCE-3 Investigators Apixaban versus enoxaparin for thromboprophylaxis after hip replacement. N Engl J Med. 2010;363:2487–2498. doi: 10.1056/NEJMoa1006885. [DOI] [PubMed] [Google Scholar]
- 22.Li XM, Sun SG, Zhang WD. Apixaban versus enoxaparin for thromboprophylaxis after total hip or knee arthroplasty: a meta-analysis of randomized controlled trials. Chin Med J (Engl) 2012;125:2339–2345. [PubMed] [Google Scholar]
- 23.Gómez-Outes A, Terleira-Fernandez AI, Suarez-Gea ML, Vargas-Castrillon E. Dabigatran, rivaroxaban, or apixaban versus enoxaparin for thromboprophylaxis after total hip or knee replacement: systematic review, meta-analysis, and indirect treatment comparisons. BMJ. 2012;344:e.3675. doi: 10.1136/bmj.e3675. [DOI] [PMC free article] [PubMed] [Google Scholar]