Abstract
The loss of a close relative is a common event, yet it is associated with increased risk of serious mental health conditions. No large‐scale study has explored up to now the importance of the bereaved person's relation to the deceased while accounting for gender and age. We performed a nationwide Danish cohort study using register information from 1995 through 2013 on four sub‐cohorts including all persons aged ≥18 years exposed to the loss of a child, spouse, sibling or parent. We identified 1,445,378 bereaved persons, and each was matched by gender, age and family composition to five non‐bereaved persons. Cumulative incidence proportions were calculated to estimate absolute differences in suicide, deliberate self‐harm and psychiatric illness. Cox proportional hazard regression was used to calculate hazard ratios while adjusting for potential confounders. Results revealed that the risk of suicide, deliberate self‐harm and psychiatric illness was increased in the bereaved cohorts for at least 10 years after the loss, particularly during the first year. During that year, the risk difference was 18.9 events in 1,000 persons after loss of a child (95% CI: 17.6‐20.1) and 16.0 events in 1,000 persons after loss of the spouse (95% CI: 15.4‐16.6). Hazard ratios were generally highest after loss of a child, in younger persons, and after sudden loss by suicide, homicide or accident. One in three persons with a previous psychiatric diagnosis experienced suicide, deliberate self‐harm or psychiatric illness within the first year of bereavement. In conclusion, this study shows that the risk of suicide, deliberate self‐harm and psychiatric illness is high after the loss of a close relative, especially in susceptible subgroups. This suggests the need for early identification of high‐risk persons displaying adjustment problems after loss of a close family member, in order to reduce the risk of serious mental health outcomes.
Keywords: Bereavement, suicide, deliberate self‐harm, psychiatric hospitalization, loss of a child, sudden loss
Death of a close relative is a common experience in adulthood. In the US, it has been estimated that more than 40,000 parents lose a child every year1, and more than half of the population over 65 years are widowed2. Although bereavement is a natural life event, it is often followed by emotional suffering and adjustment challenges. Studies have shown an association between the loss of a loved one and a range of mental health complications, particularly depression and post‐traumatic stress disorder3, 4, 5, 6, 7, 8, 9.
Prolonged and complicated grief reactions have been frequently studied, and prolonged grief disorder has recently been suggested for inclusion in the ICD‐1110, 11, 12, 13, 14. The relevant Working Group has concluded that prolonged and complicated grief reactions are significantly associated with serious psychosocial and health problems, including suicidality, substance abuse and cardiovascular disease11.
A representative population‐based survey has shown female gender, old age, and loss of a child or the spouse to be risk factors in grief complications15, whereas epidemiological studies show male gender to be associated with an excess risk of suicide and mortality after loss2. Yet, no studies have investigated suicidal behaviour and psychiatric illness across different types of loss, and considered previous history of mental and physical illness in the bereaved when interpreting the data15.
The vast majority of individuals exposed to the loss of a loved person exhibit time‐limited disruptions to daily functioning, and it has been argued that a mix of genetic, personality and environmental determinants act as protective or risk factors16. However, to study this mix of determinants requires large‐scale studies. Up to now, few investigations have had sufficient size to quantify the risk of serious mental health conditions in specific subgroups after the loss of different types of close relatives. Understanding the pattern of grief‐related disorders and serious mental health conditions is important to health care planning13, 16, 17.
In a comprehensive population‐based cohort, we investigated the absolute and relative risk of suicide, deliberate self‐harm and psychiatric illness in people exposed to the loss of a child, spouse, parent or sibling. We evaluated whether the association was modified by gender, age, urbanization, or pre‐existing mental conditions or physical diseases.
METHODS
Study population and design
A population‐based cohort was established by using a unique personal identification number which links individual‐level data between nationwide Danish registers18. The study cohort comprised four sub‐cohorts of persons aged 18 years or older and residing in Denmark during the inclusion period from January 1, 1995 to December 31, 2012 (N=1,445,378). Each sub‐cohort included all persons exposed to the loss of either a child, spouse/registered partner, parent or sibling.
Exposure to loss was assessed by identifying deceased persons and linking them to their family members using information from the Danish Civil Registration System19. Sudden and unnatural loss was defined as suicide, accident or homicide in the Danish Register of Causes of Death20. A person could serve as exposed in more than one sub‐cohort if more than one type of loss was experienced in the study period, but we included only the first loss within each type of loss.
Each person experiencing loss was matched based on gender and birthday (±70 days) with five unexposed reference persons. We ensured that each of the reference persons had a relative of the same type as the one lost by the bereaved person. The matching algorithm was applied with replacements between strata. Each person was followed until one of the studied outcomes, death, emigration, or end of study period, whichever came first.
Outcome variables and data sources
The main outcome was a serious mental health condition defined as suicide, deliberate self‐harm, or psychiatric illness. The three events were studied individually and as a composite outcome for all four types of loss. Suicide was identified via the ICD‐10 coding system (codes X60‐X84) obtained from the Danish Register of Causes of Death20. Psychiatric illness was defined as any inpatient or outpatient hospitalization, or psychiatric emergency room contact registered in the Danish Psychiatric Central Research Register21. Deliberate self‐harm was defined in accordance with the criteria of the Danish National Patient Register22 or the Psychiatric Central Research Register, which has previously been used in Danish register studies23.
Potential confounders or effect modifiers included in the analyses were: gender, age, calendar period, degree of urbanization, history of psychiatric diagnosis, past inpatient psychiatric hospitalization, past deliberate self‐harm, current use of psychotropic medication, and history of selected somatic diseases. Urbanization was classified according to the DEGURBA variable24 used by the European Union and Statistics Denmark (densely, intermediately ≥40000, intermediately <40000, thinly ≥15000, or thinly <15000 populated). Past psychiatric diagnoses were categorized based on a five‐year history in the Psychiatric Central Research Register. Considered diagnoses were: mood and anxiety disorders (ICD‐10 codes F30‐F48), schizophrenia and related disorders (F20‐F29), and alcohol or drug abuse (F10‐F19). History of psychiatric hospitalization was coded by identifying any inpatient hospitalization in the Psychiatric Central Research Register during the five years prior to entry date. Past deliberate self‐harm was also considered during the five years prior to the entry date based on the earlier defined criteria. The National Prescription Registry25 was used to assess a one‐year history of redeemed psychotropic medication by the Anatomical Therapeutic Chemical codes for antipsychotics (N05A), anxiolytics (N05B), sedatives (N05C), or antidepressants (N06A). Data on somatic diseases were obtained from the National Patient Register on the basis of diagnoses (ICD‐8/ICD‐10 codes) of chronic obstructive pulmonary disease (491‐492/J41‐J44), cancer (140‐209/C00‐C97), spine disorder (728/M40‐M54), asthma (493/I60‐I66), diabetes (249‐250/E10‐E14), and ischemic heart disease (410‐414/I20‐I25).
The study was approved by the Danish Data Protection Agency (2013‐41‐1719).
Statistical analysis
To assess the absolute risk of a serious mental health condition, we calculated the cumulative incidence proportion for the bereaved and non‐bereaved cohorts while taking into account competing death. The hazard ratios for suicide, deliberate self‐harm and psychiatric illness comparing bereaved to non‐bereaved persons were calculated by stratified Cox proportional hazard regression with time since bereavement as the underlying time scale to allow for separate baseline hazards in each matching group (one exposed and five matches). The hazard ratios were adjusted for degree of urbanization, past psychiatric diagnoses, past psychiatric hospitalization, past deliberate self‐harm, current use of psychotropic medication, and history of somatic diseases. In sub‐analyses, hazard ratios were calculated on the basis of both sudden and unnatural losses and disease‐related losses.
All data handling and statistical analyses were performed with SAS9 (SAS Institute Inc., Cary, NC, USA) and Stata 14 (StataCorp LP, College Station, TX, USA).
RESULTS
Within the study period, 83,659 persons experienced loss of a child, 373,744 loss of the spouse, 885,379 loss of a parent, and 102,596 loss of a sibling. The matched cohorts were five times larger (N=418,295, 1,868,720, 4,426,895, and 512,980, respectively). During 72,621,128 person‐years of follow‐up (range = 0‐19 years), we identified 128,120 (8.9%) bereaved persons and 530,026 (7.3%) non‐bereaved persons (p<0.0001) who suffered from one of the three outcomes: suicide (0.1% vs. 0.06%, p<0.0001), deliberate self‐harm (3.5% vs. 2.8%, p<0.0001) or psychiatric illness (5.3% vs. 4.5%, p<0.0001).
The hazard ratio of a serious mental health condition was increased in the bereaved cohorts for at least 10 years after the loss, particularly during the first year (Figure 1). In this first year, the risk difference was 18.9 events in 1,000 persons (95% CI: 17.6‐20.1) after loss of a child, 16.0 events in 1,000 persons (95% CI: 15.4‐16.6) after loss of the spouse, 4.3 events in 1,000 persons (95% CI: 4.0‐4.6) after loss of a parent, and 12.8 events in 1,000 persons (95% CI: 11.8‐13.9) after loss of a sibling, compared to non‐bereaved persons (Table 1). Psychiatric illness was the most frequent outcome.
Figure 1.
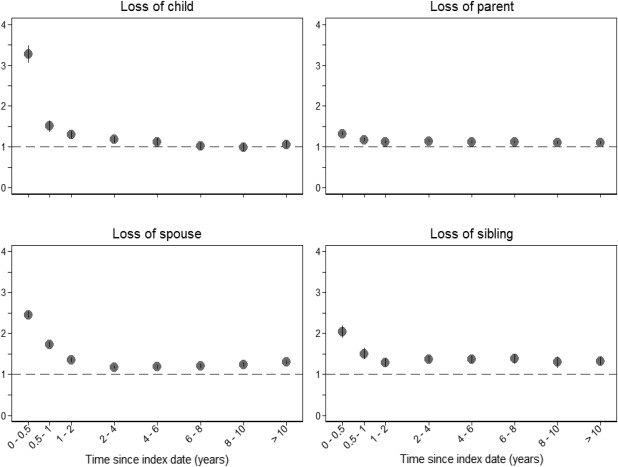
Hazard ratios (Y‐axis) for serious mental health outcomes based on time since bereavement (0‐10 years)
Table 1.
Risk differences of suicide, deliberate self‐harm and psychiatric illness in the first year after loss per 1,000 persons
| Bereaved | Non‐bereaved | ||||
|---|---|---|---|---|---|
| Events |
CIP (95% CI) |
Events |
CIP (95% CI) |
Difference (95% CI) |
|
| Loss of child (N=501,954) | |||||
| Composite | 2,762 | 33.0 (31.8‐34.2) | 5,920 | 14.2 (13.8‐14.5) | 18.9 (17.6‐20.1) |
| Suicide | 30 | 0.36 (0.25‐0.51) | 66 | 0.16 (0.12‐0.20) | 0.20 (0.07‐0.34) |
| Deliberate self‐harm | 1,007 | 12.0 (11.3‐12.8) | 2,641 | 6.3 (6.1‐6.6) | 5.7 (4.9‐6.5) |
| Psychiatric illness | 2,447 | 29.3 (28.1‐30.4) | 4,912 | 11.7 (11.4‐12.1) | 17.5 (16.3‐18.7) |
| Loss of spouse (N=2,242,464) | |||||
| Composite | 11,002 | 29.5 (28.9‐30.0) | 25,110 | 13.4 (13.3‐13.6) | 16.0 (15.4‐16.6) |
| Suicide | 279 | 0.74 (0.66‐0.84) | 204 | 0.11 (0.10‐0.13) | 0.64 (0.55‐0.73) |
| Deliberate self‐harm | 3,612 | 12.3 (12.0‐12.7) | 10,324 | 5.5 (5.4‐5.6) | 6.8 (6.5‐7.2) |
| Psychiatric illness | 9,124 | 24.4 (23.9‐24.9) | 20,355 | 10.9 (10.7‐11.0) | 13.5 (13.0‐14.0) |
| Loss of parent (N=5,312,274) | |||||
| Composite | 16,858 | 19.1 (18.8‐19.3) | 65,426 | 14.8 (14.7‐14.9) | 4.3 (4.0‐4.6) |
| Suicide | 187 | 0.21 (0.18‐0.24) | 533 | 0.16 (0.16‐0.17) | 0.09 (0.06‐0.12) |
| Deliberate self‐harm | 7,599 | 8.6 (8.4‐8.8) | 28,814 | 6.5 (6.4‐6.6) | 2.1 (1.9‐2.3) |
| Psychiatric illness | 15,086 | 17.0 (16.8‐17.3) | 58,961 | 13.3 (13.2‐13.4) | 3.7 (3.4‐4.0) |
| Loss of sibling (N=615,576) | |||||
| Composite | 2,904 | 28.3 (27.3‐29.3) | 7,945 | 15.5 (15.2‐15.8) | 12.8 (11.8‐13.9) |
| Suicide | 21 | 0.20 (0.13‐0.31) | 75 | 0.15 (0.12‐0.18) | 0.06 (−0.04 to 0.15) |
| Deliberate self‐harm | 1,381 | 13.5 (12.8‐14.2) | 3,640 | 7.1 (6.9‐7.3) | 6.4 (5.6‐7.1) |
| Psychiatric illness | 2,576 | 25.1 (24.2‐26.1) | 7,102 | 13.9 (13.5‐14.2) | 11.3 (10.3‐12.3) |
CIP − cumulative incidence proportion
When we compared bereaved with non‐bereaved persons, the overall adjusted hazard ratio at one year post‐loss was 2.53 (95% CI: 2.39‐2.67) for persons who lost a child, 2.14 (95% CI: 2.08‐2.19) for persons who lost the spouse, 1.27 (95% CI: 1.23‐1.30) for persons who lost a parent, and 1.85 (95% CI: 1.74‐1.97) for persons who lost a sibling (Figures 2 and 3).
Figure 2.
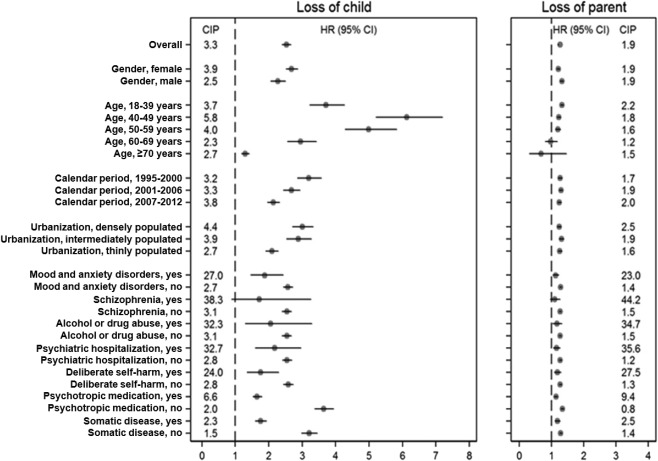
Adjusted hazard ratios (HR) and cumulative incidence proportion (CIP, %) within one year of the loss of a child or parent according to demographic variables and health status at the time of the loss
Figure 3.
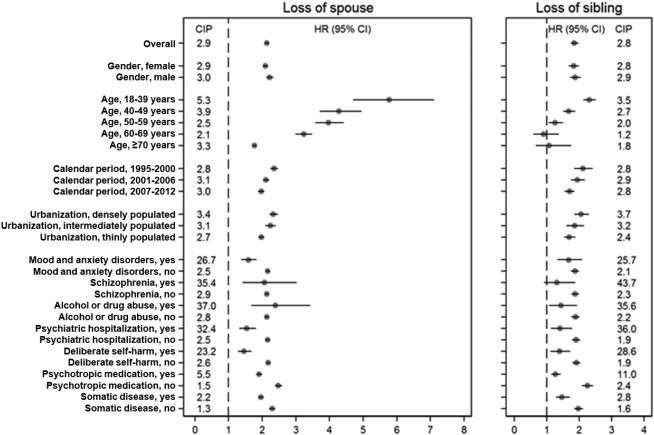
Adjusted hazard ratios (HR) and cumulative incidence proportion (CIP, %) within one year of the loss of the spouse or a sibling according to demographic variables and health status at the time of the loss
The hazard ratio of developing a serious mental health condition was generally highest for 18‐39 year‐olds after loss of spouse (5.78; 95% CI: 4.70‐7.10) and for 40‐49 years‐olds after loss of child (6.13; 95% CI: 5.21‐7.20). The overall risk was similar for males and females, except after loss of child, where females were at higher risk (hazard ratio: 2.68; 95% CI: 2.51‐2.87) than males (hazard ratio: 2.29; 95% CI: 2.06‐2.49).
The cumulative incidence proportion was considerably higher in persons with a previous psychiatric diagnosis. In general, about one third of these persons experienced serious mental health conditions during bereavement (i.e., 37% of persons previously diagnosed with alcohol or drug abuse who lost a spouse; 44% of persons with a previous diagnosis of schizophrenia who lost a parent). Sub‐analyses revealed that sudden unnatural loss resulted in a markedly higher risk of a serious mental health condition in the first year after bereavement (for all types of loss) compared to other losses (Figure 4).
Figure 4.
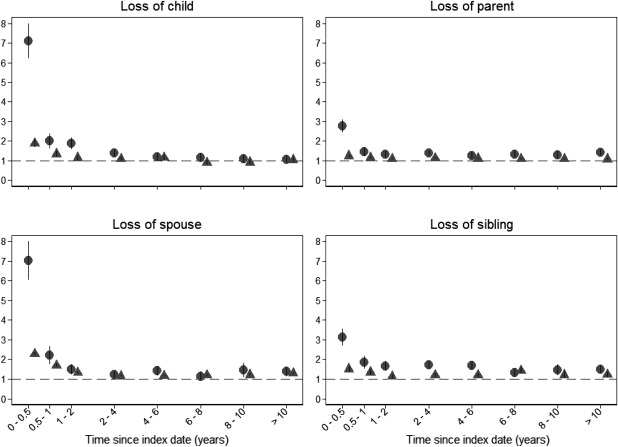
Hazard ratios of serious mental health outcomes for persons who lost a relative due to a disease (triangles) or to an unnatural cause of death (diamonds) according to time since bereavement (0‐10 years)
DISCUSSION
In this comprehensive nationwide cohort study, loss of a close relative was associated with higher risk of suicide, deliberate self‐harm or psychiatric illness for up to ten years after the loss, but particularly within the first year. Risk profiles varied according to the bereaved person's relation to the deceased, age, gender, history of mental illness, and cause of death. We generally found higher risks for persons who lost a child or the spouse, with a risk difference of 18.9 in 1,000 persons after loss of a child and 16.0 in 1,000 persons after loss of the spouse. Hazard ratios were generally highest in younger persons and after sudden and unnatural loss. One in three persons with a history of psychiatric disorders experienced at least one of the three investigated outcomes within the first year of bereavement.
Our finding of increased risk of suicide and psychiatric illness after the loss of a close relative is consistent with earlier studies, which have shown that risk is particularly high within the first year after the loss3, 4, 5, 6, 26, 27, 28, 29. To the best of our knowledge, this is the first large‐scale study to explore the importance of the bereaved person's relation to the deceased while accounting for gender and age. Death of the spouse has, for many years, ranked as the life event demanding the most intense readjustment when measured by the Social Readjustment Rating Scale30, but recent studies with data on younger populations have suggested that loss of a child is also associated with intense and persistent grief2, 31, mental illness, and suicide6. In our study, the largest risk difference for developing a serious mental health condition was actually seen in persons who lost a child.
The absolute and relative risk of a serious mental health condition increased with young age at the time of bereavement, except for persons who lost of child, for whom the risk peaked at the age of 40‐49 years. Earlier findings have been inconsistent. Some studies have reported that younger spouses are at highest risk of negative health consequences27, 28, whereas others have found persons aged >60 years to be at highest risk, especially of prolonged or complicated grief and suicide3, 13, 26, 32. The proportion of sudden and unnatural losses was higher in younger age groups, whereas losses in older age were more often due to disease and expected deaths, which may contribute to explain the more severe acute grief responses of the former. Age‐specific vulnerabilities could also offer an explanation: younger persons might lack experience with loss adjustment and emotional suffering, which may result in susceptibility to mental illness.
Risk of serious mental health conditions was similar for males and females, yet females were at higher risk after loss of a child. Increased risk of mortality after loss of the spouse has been established in males26, 27, 33, 34, 35, while increased psychiatric morbidity following loss has especially been found in females2, 15, 36. Different risk profiles have been explained on the basis of differences in attachment patterns, social interaction, and coping strategies2, 6, 33, 36: males tend to be less prone to seek help and more likely to suffer from undertreated substance abuse and act on impulse, which increases their risk of deliberate self‐harm and suicide33. Females tend to be more prone to rumination and react with emotional coping strategies, making them more susceptible to anxiety, depression, and post‐traumatic stress, which could complicate their grief response.
Our study also showed that a history of mental illness is associated with substantial increase in risk, as is sudden loss from suicide, accidents or homicide. Previous studies have established comorbidity between mental illness, substance abuse, and prolonged or complicated grief13, 37, 38, 39, between suicide and a family history of suicidal behavior40, 41, and between violent deaths and increased risk of prolonged or complicated grief, mental illness, or suicide during bereavement13, 42, 43. Nevertheless, in our study, one in three bereaved with a history of mental illness experienced a serious mental health condition after loss; this has never previously been established while also adjusting for age and gender. Our finding points to the role of personal vulnerability in adjustment to loss.
The sample size of this study is unparalleled by other studies on risk of health consequences after loss and provides estimates with high statistical precision, while controlling for several confounders, such as history of mental or physical health, that might have been shared with the deceased family member and affected the health of the bereaved person.
In the Danish registration system, the overall validity and completeness of the records of death is close to 100%, which ensured accurate classification of people exposed to bereavement. We followed the entire Danish population for up to 19 years without loss to follow‐up; thus, selection bias cannot explain the results. However, information on reasons for contacts with psychiatric outpatient clinics or psychiatric emergency care units was not included. As severity of mental health issues may vary in these contacts, the adversity could have been overestimated. Yet, only contacts with a psychiatric unit were recorded, whereas information on persons who were treated for mental disorders in primary care was not included.
Although we adjusted for several potential confounding factors, residual confounding by unmeasured factors cannot be ruled out. Unfortunately, data on socio‐economic factors, educational level and lifestyle factors were not available. However, loss‐induced changes in lifestyle, such as alcohol intake, diet or sleeping pattern, are considered as intermediate steps on the causal pathway and should not be adjusted for. Furthermore, our register‐based study had no information on potentially modifying factors, such as genetic variables, family attachment pattern, social network, and distress.
The generalizability of our findings may be limited to similar Western societies, with comparable health behaviors and risk factors. Yet, the estimates in this study provide significant information on the far‐reaching health consequences of familial loss.
Serious mental health conditions and suicide after loss of a close relative are potentially preventable13, 44. Early mitigation of risk may have wide‐ranging beneficial effects, especially for distinct high‐risk groups. Suicide and psychiatric illness after bereavement may be prevented by early identification of symptom severity and adjustment problems. Future public health strategies should consider policy implications of disseminating knowledge about high‐risk groups as well as strengthening the professional competencies in assessing symptom severity. Hence, more studies are needed about assessment methods and early identification of adjustment problems.
In conclusion, this nationwide study provides the first comprehensive assessment of the incidence of serious mental health conditions after the loss of a close relative. A significantly elevated risk of suicide, deliberate self‐harm and psychiatric illness is shown, particularly in the first year after the loss. Loss of child or spouse resulted in higher risk, and young age, a history of mental illness and sudden losses were found to be specific risk factors. This study points to early identification of high‐risk persons displaying adjustment problems in order to mitigate distress and reduce the risk of serious mental health conditions after loss of a close family member.
ACKNOWLEDGEMENTS
This study was supported by an unrestricted grant from the Lundbeck Foundation (no. R155‐2012‐11280), TrygFonden, and the Danish Cancer Society. J. Li was supported by the European Research Council (ERC‐2010‐StG 2010‐260242‐ProgEuro), Danish Council for Independent Research (project no. 6110‐00019A) and the Nordic Cancer Union (2015‐176673). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
REFERENCES
- 1. Wilcox HC, Mittendorfer‐Rutz E, Kjeldgard L et al. Functional impairment due to bereavement after the death of adolescent or young adult offspring in a national population study of 1,051,515 parents. Soc Psychiatry Psychiatr Epidemiol 2015;50:1249‐56. [DOI] [PubMed] [Google Scholar]
- 2. Stroebe M, Schut H, Stroebe W. Health outcomes of bereavement. Lancet 2007;370:1960‐73. [DOI] [PubMed] [Google Scholar]
- 3. Christakis NA, Allison PD. Mortality after the hospitalization of a spouse. N Engl J Med 2006;354:719‐30. [DOI] [PubMed] [Google Scholar]
- 4. Elwert F, Christakis NA. The effect of widowhood on mortality by the causes of death of both spouses. Am J Publ Health 2008;98:2092‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Li J, Precht DH, Mortensen PB et al. Mortality in parents after death of a child in Denmark: a nationwide follow‐up study. Lancet 2003;361:363‐7. [DOI] [PubMed] [Google Scholar]
- 6. Li J, Laursen TM, Precht DH et al. Hospitalization for mental illness among parents after the death of a child. N Engl J Med 2005;352:1190‐6. [DOI] [PubMed] [Google Scholar]
- 7. Qin P, Mortensen PB. The impact of parental status on the risk of completed suicide. Arch Gen Psychiatry 2003;60:797‐802. [DOI] [PubMed] [Google Scholar]
- 8. Wilcox HC, Kuramoto SJ, Brent D et al. The interaction of parental history of suicidal behavior and exposure to adoptive parents’ psychiatric disorders on adoptee suicide attempt hospitalizations. Am J Psychiatry 2012;169:309‐15. [DOI] [PubMed] [Google Scholar]
- 9. Bolton JM, Au W, Chateau D et al. Bereavement after sibling death: a population‐based longitudinal case‐control study. World Psychiatry 2016;15:59‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bonanno GA, Neria Y, Mancini A et al. Is there more to complicated grief than depression and posttraumatic stress disorder? A test of incremental validity. J Abnorm Psychol 2007;116:342‐51. [DOI] [PubMed] [Google Scholar]
- 11. Maercker A, Brewin CR, Bryant RA et al. Diagnosis and classification of disorders specifically associated with stress: proposals for ICD‐11. World Psychiatry 2013;12:198‐206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Prigerson HG, Horowitz MJ, Jacobs SC et al. Prolonged grief disorder: psychometric validation of criteria proposed for DSM‐V and ICD‐11. PLoS Med 2009;6:e1000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shear MK. Complicated grief. N Engl J Med 2015;372:153‐60. [DOI] [PubMed] [Google Scholar]
- 14. Maciejewski PK, Maercker A, Boelen PA et al. “Prolonged grief disorder” and “persistent complex bereavement disorder”, but not “complicated grief”, are one and the same diagnostic entity: an analysis of data from the Yale Bereavement Study. World Psychiatry 2016;15:266‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kersting A, Brahler E, Glaesmer H et al. Prevalence of complicated grief in a representative population‐based sample. J Affect Disord 2011;131:339‐43. [DOI] [PubMed] [Google Scholar]
- 16. Bonanno GA. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol 2004;59:20‐8. [DOI] [PubMed] [Google Scholar]
- 17. Stroebe W, Schut H, Stroebe MS. Grief work, disclosure and counseling: do they help the bereaved? Clin Psychol Rev 2005;25:395‐414. [DOI] [PubMed] [Google Scholar]
- 18. Erlangsen A, Fedyszyn I. Danish nationwide registers for public health and health‐related research. Scand J Publ Health 2015;43:333‐9. [DOI] [PubMed] [Google Scholar]
- 19. Pedersen CB. The Danish Civil Registration System. Scand J Public Health 2011;39:22‐5. [DOI] [PubMed] [Google Scholar]
- 20. Helweg‐Larsen K. The Danish Register of causes of death. Scand J Publ Health 2011;39:26‐9. [DOI] [PubMed] [Google Scholar]
- 21. Munk‐Jorgensen P, Mortensen PB. The Danish Psychiatric Central Register. Dan Med Bull 1997;44:82‐4. [PubMed] [Google Scholar]
- 22. Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health 2011;39:30‐3. [DOI] [PubMed] [Google Scholar]
- 23. Nordentoft M, Mortensen PB, Pedersen CB. Absolute risk of suicide after first hospital contact in mental disorder. Arch Gen Psychiatry 2011;68:1058‐64. [DOI] [PubMed] [Google Scholar]
- 24. Statistics Denmark. Degree of urbanization. Copenhagen: Statistics Denmark, 2016. [Google Scholar]
- 25. Kildemoes HW, Sorensen HT, Hallas J. The Danish National Prescription Registry. Scand J Publ Health 2011;39:38‐41. [DOI] [PubMed] [Google Scholar]
- 26. Erlangsen A, Jeune B, Bille‐Brahe U et al. Loss of partner and suicide risks among oldest old: a population‐based register study. Age Ageing 2004;33:378‐83. [DOI] [PubMed] [Google Scholar]
- 27. Manor O, Eisenbach Z. Mortality after spousal loss: are there socio‐demographic differences? Soc Sci Med 2003;56:405‐13. [DOI] [PubMed] [Google Scholar]
- 28. Schaefer C, Quesenberry CP Jr, Wi S. Mortality following conjugal bereavement and the effects of a shared environment. Am J Epidemiol 1995;141:1142‐52. [DOI] [PubMed] [Google Scholar]
- 29. Kaltman S, Bonanno GA. Trauma and bereavement: examining the impact of sudden and violent deaths. J Anxiety Disord 2003;17:131‐47. [DOI] [PubMed] [Google Scholar]
- 30. Holmes TH, Rahe RH. The social readjustment rating scale. J Psychosom Res 1967;11:213‐8. [DOI] [PubMed] [Google Scholar]
- 31. Zetumer S, Young I, Shear MK et al. The impact of losing a child on the clinical presentation of complicated grief. J Affect Disord 2015;170:15‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Elwert F, Christakis NA. Widowhood and race. Am Sociol Rev 2006;71:16‐41. [Google Scholar]
- 33. Agerbo E. Midlife suicide risk, partner's psychiatric illness, spouse and child bereavement by suicide or other modes of death: a gender specific study. J Epidemiol Community Health 2005;59:407‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Espinosa J, Evans WN. Heightened mortality after the death of a spouse: marriage protection or marriage selection? J Health Econ 2008;27:1326‐42. [DOI] [PubMed] [Google Scholar]
- 35. Li G. The interaction effect of bereavement and sex on the risk of suicide in the elderly: an historical cohort study. Soc Sci Med 1995;40:825‐8. [DOI] [PubMed] [Google Scholar]
- 36. Stroebe M. Gender differences in adjustment to bereavement: an empirical and theoretical review. Rev Gen Psychol 2001;5:62‐83. [Google Scholar]
- 37. Lobb EA, Kristjanson LJ, Aoun SM et al. Predictors of complicated grief: a systematic review of empirical studies. Death Stud 2010;34:673‐98. [DOI] [PubMed] [Google Scholar]
- 38. Melhem NM, Rosales C, Karageorge J et al. Comorbidity of axis I disorders in patients with traumatic grief. J Clin Psychiatry 2001;62:884‐7. [DOI] [PubMed] [Google Scholar]
- 39. Simon NM, Pollack MH, Fischmann D et al. Complicated grief and its correlates in patients with bipolar disorder. J Clin Psychiatry 2005;66:1105‐10. [DOI] [PubMed] [Google Scholar]
- 40. Guldin MB, Li J, Pedersen HS et al. Incidence of suicide among persons who had a parent who died during their childhood: a population‐based cohort study. JAMA Psychiatry 2015;72:1227‐34. [DOI] [PubMed] [Google Scholar]
- 41. Qin P, Agerbo E, Mortensen PB. Suicide risk in relation to family history of completed suicide and psychiatric disorders: a nested case‐control study based on longitudinal registers. Lancet 2002;360:1126‐30. [DOI] [PubMed] [Google Scholar]
- 42. Tal Young I, Iglewicz A, Glorioso D et al. Suicide bereavement and complicated grief. Dialogues Clin Neurosci 2012;14:177‐86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. van Denderen M, de Keijser J, Kleen M et al. Psychopathology among homicidally bereaved individuals: a systematic review. Trauma Violence Abuse 2015;16:70‐80. [DOI] [PubMed] [Google Scholar]
- 44. Nordentoft M, Madsen T, Fedyszyn I. Suicidal behavior and mortality in first‐episode psychosis. J Nerv Ment Dis 2015;203:387‐92. [DOI] [PubMed] [Google Scholar]


