Abstract
Introduction:
In younger patients, ceramic-on-ceramic (CoC) bearing surfaces are usually recommended for total hip replacement (THR) because of their low wear rate and longer expected functional life. Although technical advancements have reduced the risk of ceramic bearings fracture, this complication remains a major concern.
Case description:
We present the case of a 56-year-old patient undergoing 3 revision hip arthroplasties of the right hip due to ceramic liner fractures. Initial THR (2008) was performed with a CoC bearing, followed by liner fracture due to trauma a year later. The acetabular component and liner were replaced, with a minor incongruence between the old head and new insert. The 2nd ceramic insert fractured 3.5 years later, following minor trauma. Upon revision, the bearing surface was changed to metal-on-polyethylene (MoP). The performed retrieval analysis demonstrated stripe and rim wear, and evidence of adhesive wear. The patient was referred to us a month later, with a fistula on the lateral side of the hip, discharging black, petroleum-like liquid. Radiology showed well-fixed implants, no dislocation and no apparent polyethylene wear. Microbiological assessment of the discharge showed no infection. Intraoperatively massive metallosis was noticed, with stable acetabular and femoral components. The metal femoral head was heavily abraded, with almost 1% volumetric wear. Hematoxylin and eosin stained frozen tissue samples showed muscular and adipose tissue necrosis, while polarized light microscopy highlighted metal, polyethylene, and ceramic particles.
Conclusion:
The present case is yet another report showing the adverse outcomes of using MoP bearings for revision after ceramic liner fracture in THR.
Keywords: ceramic bearing fracture, histology, metallosis, revision hip arthroplasty
1. Introduction
Total hip replacement (THR) is one of the most successful interventions in orthopedic surgery. After the concept of low friction arthroplasty was introduced in 1958 by Sir John Charnley, the combination of metal-on-polyethylene (MoP) became one of the most popular option for bearing surfaces, with the most consistent results obtained when using a cobalt-chrome alloy femoral head on an ultrahigh molecular weight polyethylene acetabular component. However, as more and more hip replacements are performed at a relatively young age, the longevity of the implants became a major concern. Unfortunately, polyethylene wear can lead to periprosthetic osteolysis and a risk of endoprosthesis loosening. Thus, bearing surfaces have undergone a remarkable evolution in an effort to improve their tribology, aiming for a combination as close as possible to the articular cartilage, with a low coefficient of friction, adequate strength, and no wear in the absence of pathology.[1]
There are 2 major classes of bearing surfaces: hard-on-soft bearings – with the soft bearing always toward the acetabular side, articulating with a metal alloy or ceramic head; and hard-on-hard bearings – metal-on-metal (MoM) or ceramic-on-ceramic (CoC). Although the hard-on-hard bearings generate lesser and smaller wear particles, they come with their own associated risks, such as possibly high levels of cobalt (Co) and chromium (Cr) ions with subsequent cancer risks for the MoM options,[1,2] while stripe wear, squeaking noises, malposition of the acetabular component, and chipping during insertion might complicate the use of CoC bearings.[1]
One of the most important complications of the CoC bearings is fracture.[3] The current consensus on treatment is immediate revision with complete synovectomy for careful removal of ceramic fragments.[4–6] However, there are 2 controversial issues: what is the optimal new bearing surface, and whether well-fixed implants with damaged tapers should or should not be replaced?[6,7] As the cone of the stem or the inner surface of the cup may be damaged by fractured ceramic particles or direct contact, insertion of a new ceramic bearing on a damaged taper surface might increase the risk of refracture.[8] This would imply that implant change is recommendable even if there is stable fixation.[6,8] Still, one must also consider the technical difficulties of removing well-fixed cementless components, as well as the potential associated bone loss that might affect the revised implant's longevity, and imply a more challenging intervention later on.[9–11] Change to an MoP bearing surface might seem as a possible solution, as it could enable retaining of the stable implants without concerns about ceramic refracture.[9] However, there are controversies regarding this choice.[4,5] In spite of the reported favorable long-term results when combined with complete synovectomy,[5] the change to MoP after ceramic bearing fracture holds a risk of massive metallosis due to 3rd body wear by remnant ceramic particles. Furthermore, there might be fatal systemic complications related to Co or Cr intoxication.[12]
Adverse local tissue reactions (ALTRs) is an umbrella term used for denoting a variety of complications related to the local hypersensitivity response to metal components of implants, and it includes pseudotumors, metal sensitivity in the form of aseptic lymphocyte-dominated vasculitis-associated lesions, osteolysis, metallosis, and chronic inflammatory lesions in the periprosthetic tissues.[13] The specific histologic features are the presence of wear particles, lymphocytes, macrophages, and necrosis. In cases of MoM bearings, the cellular response is dominated by lymphocytes, while for MoP bearings, the majority of reactive cells are macrophages and multinucleated giant cells.[14]
We report a case of ALTR as a complication after 2 revision hip replacements for ceramic liner fractures, with bearing surface change from CoC to MoP. The patient was informed that data from the case would be submitted for publication and gave his consent for this CARE compliant clinical case report.[15]
2. Report of the case
2.1. Patient history
The 56-year-old male patient underwent primary THR of the right hip in a different institution 4.5 years prior to refer to us – the implanted bearing surface was CoC. Approximately 1 year postoperation, he was involved in a road traffic accident and sustained a closed injury that led to the fracture of the ceramic liner (Fig. 1). During revision surgery, both the acetabular cup and liner were replaced. Since the ceramic femoral head could not be replaced, there was a minor incongruence between the old femoral head and the new liner. However, the patient regained normal hip mobility, only complaining of an audible squeaking of the hip. Another 3.5 years later, fracture of the 2nd ceramic liner was diagnosed, following a minor trauma that involved a twisting motion of the hip. During revision the bearing surface was changed to MoP. Upon retrieval analysis, both stripe and rim wear were observed, with evidence of adhesive wear.
Figure 1.
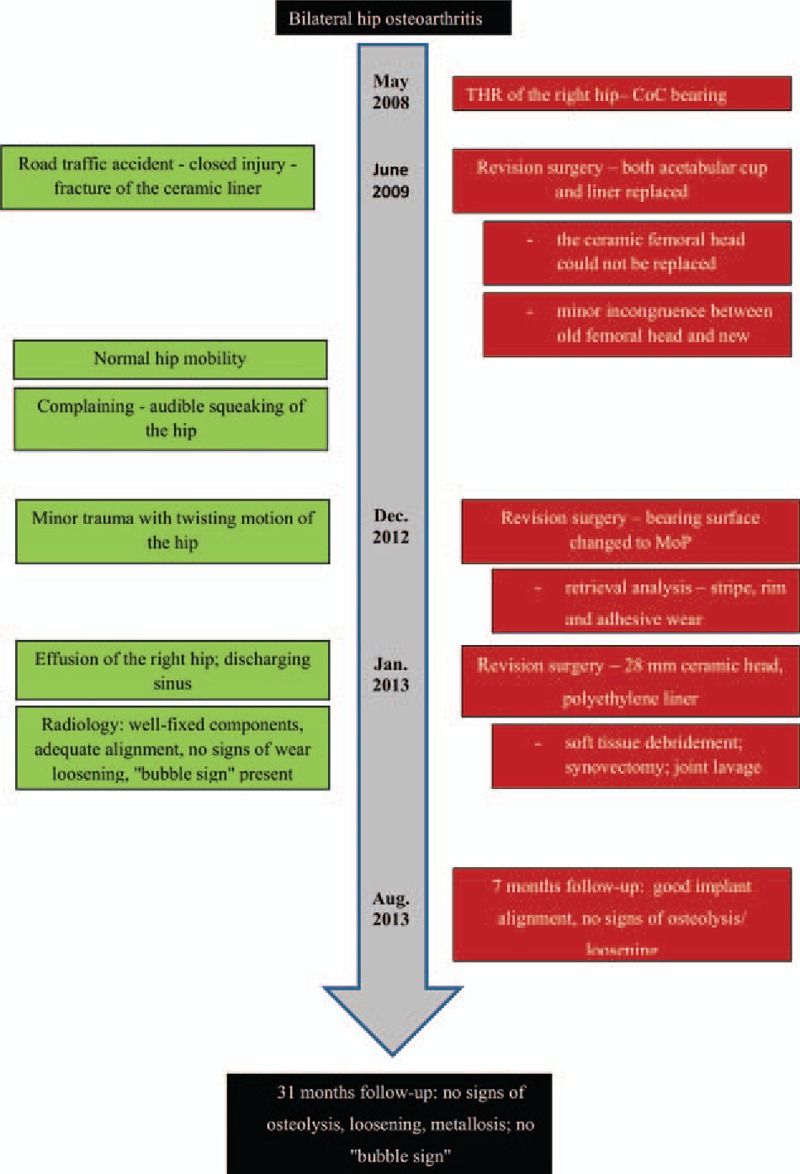
Timeline of interventions and outcomes.
2.2. Presenting symptoms and clinical examination
The patient was referred to our clinic 1 month later, presenting with considerable effusion of the right hip and a discharging sinus in the middle of the postoperative scar. He had a body mass index of 29.5 and a past medical history of hypertension.
On local examination of the right hip, the postoperative scar was well healed, aside from the fistula in its middle part, which was discharging a black, petroleum-like fluid (Fig. 2A). There was also a considerable palpable effusion of the soft tissues on the lateral aspect of the hip, but no erythema or any sign of infection. The hip range of motion was slightly limited, with no evidence of motor or sensory abnormalities of the lower limb.
Figure 2.
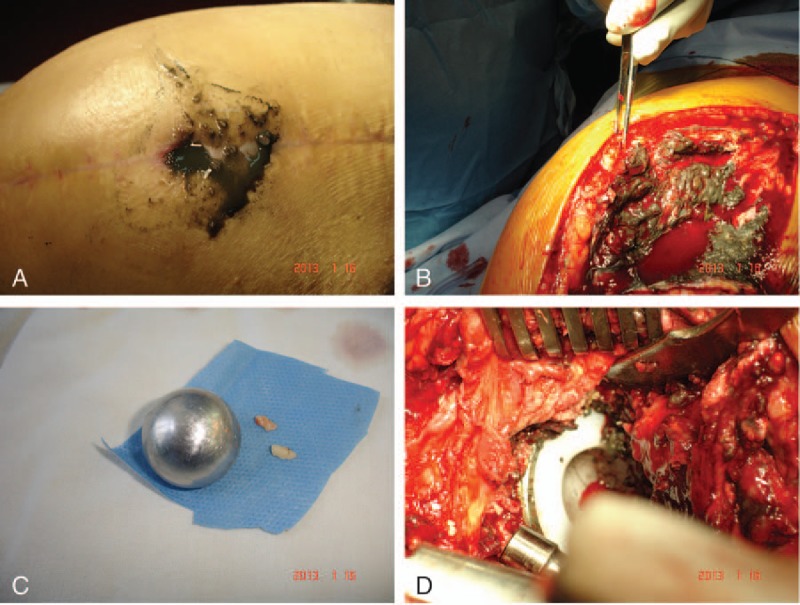
(A) Lateral aspect of the right hip, showing a healed postoperative scar with a fistula in its middle part, discharging a black, petroleum-like liquid. (B) Intraoperative aspect of the right hip after incision of the deep fascia – metallosis was confirmed by the presence of a black colored fluid and darkly pigmented soft tissues around the hip. (C) The retrieved femoral head and some of the ceramic fragments. The metal femoral head shows multiple scratches and is severely abraded. (D) Intraoperative aspect of the right hip showing a stable acetabular component.
2.3. Paraclinical examinations and diagnosis
Radiologic evaluation showed well-fixed components with adequate alignment, with no signs of wear or loosening, but the “bubble sign” was present (Fig. 3A).[16] The sign is created by metallic debris which outline the joint cavity, forming hyperdensities similar to bubbles. Ultrasonography of the right hip showed a significant fluid collection extending from the hip joint to the surrounding tissues, raising the suspicion of ALTR.
Figure 3.

(A) Preoperative antero-posterior radiograph of the pelvis, showing adequately aligned, well-fixed components, no signs of wear or loosening, but evident “bubble sign” (deposited metallic debris outlining the joint space, creating bubble-like hyperdensities). (B) Follow-up antero-posterior radiograph of the pelvis at 7 months postoperatively showing good implant alignment and no sign of loosening or metallosis. (C) Antero-posterior radiograph of the pelvis at 31 months postoperatively showing stable components and no signs of osteolysis, loosening, or metallosis.
Serum inflammatory markers were negative for infection, and swab cultures from the fistula showed no bacterial growth after 48 hours. Serum Cr level was 1.9 μg/L. Although blood samples had been collected to determine preoperative serum metal ion levels, due to an unfortunate technical issue of the laboratory, the samples could not be processed, so results were not available prior to surgery.
Given the clinical context and paraclinical findings, correlated with the history of revisions due to ceramic liner fracture and the presence of the new MoP bearing surface, the suspected diagnosis was that of ALTR, likely caused by debris due to 3rd body wear by remnant ceramic particles. The treatment plan was discussed with the patient, who consented to surgical exploration of the hip and revision THR.
2.4. Surgical intervention
The hip was explored through the previous incision, using a standard antero-lateral approach. Following the incision of the deep fascia, metallosis was confirmed by the presence of a black colored fluid and darkly pigmented soft tissues around the hip (Fig. 2B). Swab and tissue samples were collected for microbiological and histological assessment. Once the hip was dislocated, ceramic fragments of different sizes were observed and removed from the surrounding soft tissues. The retrieved femoral head was severely abraded (Fig. 2C), with almost 1% volumetric wear, but the femoral stem and acetabular component appeared stable (Fig. 2D).
The metal head was replaced with a new 28 mm ceramic head, and a new polyethylene liner was inserted into the cup. Extended soft tissue debridement and synovectomy were performed, as well as joint lavage with dilute Betadine solution before wound closure.
2.5. Microbiology and histology
Swab samples collected intraoperatively were processed in 2 different laboratories. All samples were negative for both Gram stain and culture.
Intraoperatively harvested tissue samples were frozen processed and stained with hematoxylin and eosin for examination in both optical microscopy and polarized light microscopy. Histopathological examination identified multiple foreign body granulomas. The inflammatory foci mostly showed macrophages and multinucleated giant cells, with several intracytoplasmic polyethylene and ceramic particles (Fig. 4A). The blackish ceramic particles showed no birefringence when examined in polarized light, as opposed to the polyethylene and metal particles (Fig. 4B). Ischemic necrosis lesions were present in the adipose, synovial, and muscular tissue (intensely eosinophilic, with absence of the nuclei), surrounded by granulation tissue with blackish deposits of ceramic particles. The latter contained rare phagocytic mononuclear cells in which intracytoplasmic blackish ceramic particles could be identified (Fig. 4C).
Figure 4.
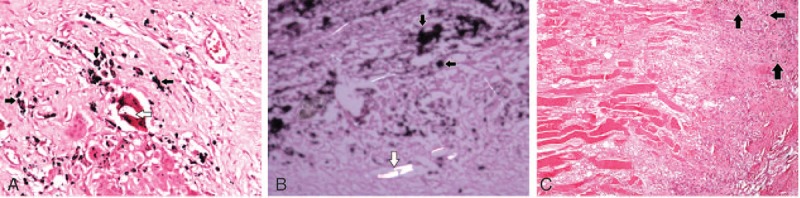
(A) Foreign body granuloma: inflammatory focus with a central multinucleated giant cell with intracytoplasmic polyethylene (white arrow) and ceramic particles (colored in black, black arrow). The same particles are also found in the surrounding macrophages (hematoxylin and eosin [HE], ×200). (B) Blackish interstitial deposits of ceramic particles (black arrows) without birefringence in polarized light microscopy compared to the neighboring birefringent polyethylene particles (white arrow) (HE, ×200, polarized light). (C) Ischemic necrosis lesions of striated muscle surrounded by granulation tissue containing rare macrophages. Intracytoplasmic blackish ceramic particles (black arrows) can be identified in the macrophages (HE, ×40).
2.6. Postoperative care, rehabilitation, and follow-up
Postoperatively the patient followed the clinic's standard antibiotic prophylaxis and rehabilitation protocol, with no immediate complications. Hip mobility was restored close to normal, and the patient resumed his normal activities.
During follow-up, serial X-rays taken at 7 and 31 months postoperatively showed good implant alignment, and no signs of osteolysis or loosening (Fig. 3B, C). Also no metallosis or “bubble sign” was noted.
3. Discussion
The ideal bearing for THR should offer low friction and virtually no wear, use chemically stable, tough, hard, nonductile materials to reduce the risks of fracture, scratching and 3rd-body wear,[14,17–19] and produce debris particles which do not induce a host immune response.[14] With one of the lowest rates of volumetric wear, CoC bearings are excellent choices, characterized by high chemical stability, excellent lubrication, high biocompatibility, and outstanding resistance to mechanical damage,[14,20,21] with good/excellent mid- and long-term clinical results.[14,22,23] However, their more widespread use in THR was prevented by some disadvantages related to reliability (fracture risk), squeaking, and the limited choices of materials.[21]
Fractures of the ceramic bearing surfaces are among the most important complications, usually occurring early, within the 1st 4 years post-THR in up to 2/3 of the cases.[21] Fortunately fracture rates are decreasing due to improvements in materials, designs, manufacturing processes, and surgical technique. Although ceramic head fractures are catastrophic events, ceramic liner fractures might present more subtly and not always related to trauma, with an estimated occurrence in 0.013% to 1.1% of cases.[7,20] Although ceramic component fractures might be caused by trauma, interposition of debris between the neck taper/acetabular cup and the ceramic component, or improper handling during implantation, ceramic liners are at higher risk of fracture when malpositioned or malseated in the acetabular component.[24] Therefore, component positioning is essential for the longevity of CoC bearing THR. In our case, the 1st fracture was caused by trauma, while the 2nd liner's fracture might have been due to incongruence between the femoral head and new liner. This supposition was verified by the stripe and rim wear found on retrieval analysis, as well as the minor trauma sustained before this 2nd fracture.
Revision of fractured ceramic components requires careful removal of all ceramic fragments and complete synoviectomy, with the recommendation to only replace CoC bearings with ceramics. Either CoC or ceramic-on-polyethylene (CoP) are good choices, while a softer bearing surface might be at a higher risk of 3rd body wear.[1,7,25] Unfortunately in the presented case, the CoC bearing was replaced by an MoP bearing during revision for the 2nd ceramic liner fracture, leading to the ALTR observed in as little as a month later.
A possible complication of THR, ALTRs are multifactorial adverse events, which can be caused by metal hypersensitivity, implant corrosion, edge loading of malpositioned components, and abrasive wear from 3rd body particles. In addition, the development of ALTRs is also influenced by the patient's individual susceptibility to wear debris.[26,27] Given the aspect of the retrieved head, in our patient the cause of ALTR seems to have been abrasive wear of the metal femoral head.
According to a consensus statement by the Hip Society, American Academy of Hip and Knee Surgeons, and American Academy of Orthopaedic Surgeons, assessment of a possible case of ALTR must include several factors: symptomatology, the implant's track record, component positioning, metal ion levels, cross-sectional imaging, histopathological analysis, as well as other possible diagnoses, such as infection.[28] In the presented case, infection was excluded based on multiple microbiological assessments of both preoperatively and intraoperatively collected samples, as well as normal serum levels of inflammatory markers. Although malalignment or loosening was not evident radiologically, the specific “bubble sign” was present – this is created by metallic debris that outline the joint cavity and forms a dense “bubble.” In terms of metal ion levels, reports usually show higher Co and Cr levels in patients with MoM bearings as compared to MoP bearings.[29] Unfortunately, the specific ion concentration level at which toxicity is induced is still unknown, but currently proposed acceptable upper limits are 2.56 μg/L for Cr and 2.02 μg/L for Co in whole blood.[29] With a serum Cr level of 1.9 μg/L our patient was in the acceptable range.
The histopathological characteristics of ALTR include both the presence of wear particles and specific reactive cells: lymphocytes, macrophages, and multinucleated giant cells. The former are preponderant in the reaction to MoM bearings wear, while the latter are dominant in cases of MoP bearings. Histological examination of the tissue samples collected during revision THR in our patient showed metal, polyethylene, and ceramic particles distinguishable under polarized light. The identified cells (mostly macrophages and multinucleated giant cells) were consistent with the features of ALTR caused by MoP bearings wear and supported the diagnosis.
The choice to replace the bearing surfaces to CoP yielded good short-term results in this case, as the patient had a quick and eventless recovery and no signs of osteolysis, loosening, or metallosis on radiologic examination at 31 months postoperatively. Other authors have also reported good outcomes for CoP bearings, albeit the results are for primary THR.[22,23] However, in a small series of 23 cases, Kwak et al[30] found higher re-revision rates for replacing fractured ceramic bearings with CoP bearings compared to MoP bearings. Still, in lack of sufficient data to highlight the best coupling, both CoC and CoP seem to be advisable choices for replacing fractured ceramic bearings during revision THR.
As of the moment, there is no definitive consensus for what is the best bearing choice for primary or revision THR. For each option, a multitude of factors must be weighed to determine if the bearing is suitable for each particular patient. Our case is yet another example that warns against replacing a CoC bearing with an MoP one, because of the rapid development of metallosis and significant local tissue reaction.
Footnotes
Abbreviations: ALTR = adverse local tissue reaction, CoC = ceramic-on-ceramic, CoP = ceramic-on-polyethylene, MoM = metal-on-metal, MoP = metal-on-polyethylene, THR = total hip replacement.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Kumar N, Arora NC, Datta B. Bearing surfaces in hip replacement – evolution and likely future. Med J Armed Forces India 2014;70:371–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Niculescu M, Laptoiu D, Miculescu F, et al. Biomaterials view on the complications associated with hip resurfacing arthroplasty. Adv Mater Res 2015;1114:247–52. [Google Scholar]
- [3].Barrack RL, Burak C, Skinner HB. Concerns about ceramics in THA. Clin Orthop Relat Res 2004;429:73–9. [DOI] [PubMed] [Google Scholar]
- [4].Allain J, Roudot-Thoraval F, Delecrin J, et al. Revision total hip arthroplasty performed after fracture of a ceramic femoral head. A multicenter survivorship study. J Bone Joint Surg Am 2003;85:825–30. [DOI] [PubMed] [Google Scholar]
- [5].Sharma V, Ranawat AS, Rasquinha VJ, et al. Revision total hip arthroplasty for ceramic head fracture: a long-term follow-up. J Arthroplasty 2010;25:342–7. [DOI] [PubMed] [Google Scholar]
- [6].Koo KH, Ha YC, Kim SY, et al. Revision of ceramic head fracture after third generation ceramic-on-ceramic total hip arthroplasty. J Arthroplasty 2014;29:214–8. [DOI] [PubMed] [Google Scholar]
- [7].Traina F, De Fine M, Di Martino A, et al. Fracture of ceramic bearing surfaces following total hip replacement: a systematic review. Biomed Res Int 2013;2013:157247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Bierbaum BE, Nairus J, Kuesis D, et al. Ceramic-on-ceramic bearings in total hip arthroplasty. Clin Orthop Relat Res 2002;405:158–63. [DOI] [PubMed] [Google Scholar]
- [9].Yoo JJ, Kim YM, Yoon KS, et al. Alumina-on-alumina total hip arthroplasty. A five-year minimum follow-up study. J Bone Joint Surg Am 2005;87:530–5. [DOI] [PubMed] [Google Scholar]
- [10].Zazgyva A, Zuh SG, Roman CO, et al. Acetabular reconstruction with a reinforcement device and bone grafting in revision arthroplasty – a mean five years of follow-up. Int Orthop 2016;40:1631–8. [DOI] [PubMed] [Google Scholar]
- [11].Zuh SG, Zazgyva A, Gergely I, et al. Acetabuloplasty with bone grafting in uncemented hip replacement for protrusion. Int Orthop 2015;39:1757–63. [DOI] [PubMed] [Google Scholar]
- [12].Zywiel MG, Brandt JM, Overgaard CB, et al. Fatal cardiomyopathy after revision total hip replacement for fracture of a ceramic liner. Bone Joint J 2013;95-B:31–7. [DOI] [PubMed] [Google Scholar]
- [13].Campbell P, Ebramzadeh E, Nelson S, et al. Histological features of pseudotumor-like tissues from metal-on-metal hips. Clin Orthop Relat Res 2010;468:2321–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Rajpura A, Kendoff D, Board TN. The current state of bearing surfaces in total hip replacement. Bone Joint J 2014;96-B:147–56. [DOI] [PubMed] [Google Scholar]
- [15].Gagnier J, Kienle G, Altman DG, et al. The CARE guidelines: consensus-based clinical case report guideline development. J Clin Epidemiol 2013;67:46–51. [DOI] [PubMed] [Google Scholar]
- [16].Su EP, Callander PW, Salvati EA. The bubble sign: a new radiographic sign in total hip arthroplasty. J Arthroplasty 2003;18:110–2. [DOI] [PubMed] [Google Scholar]
- [17].Niculescu M, Antoniac I, Blajan A. Metallic biomaterials processing technologies in order to obtain a new design for a hip prosthesis femoral component. Solid State Phenom 2014;216:239–42. [Google Scholar]
- [18].Rau JV, Antoniac I, Cama G, et al. Bioactive materials for bone tissue engineering. Biomed Res Int 2016;3741428.DOI:10.1155/2016/3741428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Ionescu R, Mardare M, Dorobantu A, et al. Correlation between materials, design and clinical issues in the case of associated use of different stainless steels as implant materials. Key Eng Mater 2014;583:41–4. [Google Scholar]
- [20].D’Antonio JA, Sutton K. Ceramic materials as bearing surfaces for total hip arthroplasty. J Am Acad Orthop Surg 2009;17:63–8. [PubMed] [Google Scholar]
- [21].Porat M, Parvizi J, Sharkey PF, et al. Causes of failure of ceramic-on-ceramic and metal-on-metal hip arthroplasties. Clin Orthop Relat Res 2012;470:382–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Schmolders J, Amvrazis G, Pennekamp PH, et al. Thirteen year follow-up of a cementless femoral stem and a threaded acetabular cup in patients younger than fifty years of age. Int Orthop 2017;41:39–45. [DOI] [PubMed] [Google Scholar]
- [23].Studers P, Belajevs D, Jurkevics V, et al. Ten to fifteen-year clinical and radiographic follow-up with a third-generation cementless stem in a young patient population. Int Orthop 2016;40:465–71. [DOI] [PubMed] [Google Scholar]
- [24].Varnum C, Pedersen AB, Kjærsgaard-Andersen P, et al. Comparison of the risk of revision in cementless total hip arthroplasty with ceramic-on-ceramic and metal-on-polyethylene bearings data on 11,096 patients from the Danish Hip Arthroplasty Registry. Acta Orthop 2015;86:477–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Lee SJ, Kwak HS, Yoo JJ, et al. Bearing change to metal-on-polyethylene for ceramic bearing fracture in total hip arthroplasty; does it work? J Arthroplasty 2016;31:204–8. [DOI] [PubMed] [Google Scholar]
- [26].Niculescu M, Laptoiu D, Miculescu F, et al. Metal allergy and other adverse reactions in patients with total hip replacement. Adv Mater Res 2015;1114:283–7. [Google Scholar]
- [27].Willert HG, Buchhorn GH, Fayyazi A, et al. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study. J Bone Joint Surg Am 2005;87:28–36. [DOI] [PubMed] [Google Scholar]
- [28].Chalmers BP, Perry KI, Taunton MJ, et al. Diagnosis of adverse local tissue reactions following metal-on-metal hip arthroplasty. Curr Rev Musculoskelet Med 2016;9:67–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Jantzen C, Jørgensen HL, Duus BR, et al. Chromium and cobalt ion concentrations in blood and serum following various types of metal-on-metal hip arthroplasties. A literature overview. Acta Orthop 2013;84:229–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Kwak HS, Yoo JJ, Lee YK, et al. The result of revision total hip arthroplasty in patients with metallosis following a catastrophic failure of a polyethylene liner. Clin Orthop Surg 2015;7:46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]


