Abstract
To investigate the relationship between corneal biomechanics and anterior segment parameters in the early stage of overnight orthokeratology.
Twenty-three eyes from 23 subjects were involved in the study. Corneal biomechanics, including corneal hysteresis (CH) and corneal resistance factor (CRF), and parameters of the anterior segment, including corneal curvature, central corneal thickness (CCT), and corneal sublayers’ thickness, were measured at baseline and day 1 and 7 after wearing orthokeratology lens. One-way analysis of variance with repeated measures was used to compare the longitudinal changes and partial least squares linear regression was used to explore the relationship between corneal biomechanics and anterior segment parameters.
At baseline, CH and CRF were positively correlated with CCT (r = 0.244, P = .008 for CH; r = 0.249, P < .001 for CRF), central stroma thickness (CST) (r = 0.241, P = .008 for CH; r = 0.244, P = .002 for CRF) and central Bowman layer thickness (CBT) (r = 0.138, P = .039 for CH; r = 0.171, P = .006 for CRF). Both CH and CRF significantly decreased from day 1 after orthokeratology. The corneal curvature and the epithelium thickness also significantly decreased, while the stromal layer thickened significantly from day 1 after orthokeratology. There was no correlation between the changes of corneal biomechanics and anterior segment parameters at day 1 and 7 after orthokeratology.
While corneal biomechanics were positively correlated with CCT, CST, and CBT, the changes of CH and CRF were not correlated with the changes of corneal curvature, CCT, and corneal sublayers’ thickness in the early stage of orthokeratology in our study.
Keywords: corneal biomechanics, corneal curvature, corneal thickness, overnight orthokeratology
1. Introduction
Overnight orthokeratology lens is a specially designed rigid contact lens that is worn at night and removed during the daytime. By flattening the central portion, overnight orthokeratology can reduce refractive error in the short term.[1] As an external object placed against the front surface of the cornea, orthokeratology lens is expected to cause certain changes in the anterior segment parameters, such as corneal curvature and thickness. Previous studies have reported flattened corneal curvature,[2,3] reduced central corneal thickness (CCT), and increased thickness in the mid-peripheral cornea after orthokeratology.[4,5] There are also studies showing a thinned central epithelial layer[6,7] and thickened corneal stromal layer[8,9] after wearing orthokeratology lens.
As an external force placed against the front surface, orthokeratology lens also leads to changes in biomechanical properties of the cornea. Chen et al[10] found that corneal resistance factor (CRF) decreased after wearing lenses for 1 night. Nieto-Bona et al[11] observed the reduction of corneal hysteresis (CH) over 1 month of treatment. Mao et al[12] found both CH and CRF decreased after 1 night of wearing the lens but started to reverse at 1 month and returned to their original levels after 3 months of follow up.
One issue that is still debatable is the correlation between the changes in corenal biomechanics and anterior segment parameters after wearing orthokeratology lens. Gonzalez-Meijome's study showed that the reduction of CH was correlated with the change of CCT[13] and Chen found that the change of CRF was correlated to the changes of curvature.[10] However, Nieto-Bona's study showed no correlation between structural and biomechanical changes of cornea at all.[11] Previous studies have reported CH and CRF were significantly reduced in keratoconus[14,15] and found a thinning of Bowman layer and epithelium which could alter the mechanical stability of the keratoconus cornea.[16,17] Other studies reported the reduced CH and CRF of cornea significantly correlated with corneal structural changes after refractive surgery.[18,19] It is unknown if these causes underlying reducing corneal biomechanics increase clinic risk during orthokeratology. So it is relevant to find out what attributes the reduction of corneal biomechanics after orthokeratology.
Therefore, the aim of this study was to test the relationship between corneal biomechanics and anterior segment parameters at baseline and in the early stage after wearing orthokeratology lens. With the ultra-high resolution optical coherence tomography (UHR-OCT), it is possible to observe the cornea sublayers’ changes and this is the first study taking account of these variables that may attribute the reduction of corneal biomechanics.
2. Materials and methods
2.1. Subjects
A total of 23 myopes (males/females = 12/11, 14.82 ± 3.58 years, age range: 10–18 years) were recruited from the Eye Clinic at Wenzhou Medical University. The subjects were included into the study if they had no previous history of wearing rigid gas-permeable contact lens, no corneal surgery, and no current ocular or general disease. The refractive error of each subject was ≤−6.00 D and astigmatism was ≤−1.50 D. The protocol of the study followed the tenets of the Declaration of Helsinki, and was approved by the Institutional Review Board of the Wenzhou Medical University. The purpose and details of the study were explained to the subjects and their legal guardians. The subjects and their legal guardians signed the written consent forms prior to the start of the study.
2.2. Orthokeratology lenses and lens fitting
The orthokeratology lenses (E&E Optics Ltd, Hong Kong, China) had a reverse geometry design. The overall diameter of the lenses was 10.6 mm, and the central optic zone was of 6.0 mm in diameter with a 0.22-mm central thickness. The building material of the lens, Boston XO, has high gas permeability (DK, 100 × 10−11(cm2mLO2)/(s mL mm Hg)). A diagnostic lens was used to evaluate lens fitting. A corneal topography was first obtained with the Medmont E300 Corneal Topographer (Medmont Pty Ltd, Victoria, Australia). Two values, taken from the flattest meridian, the simulated keratometry (simK) and asphericity, were used to determine the radius of the alignment curve. The lens fitting was evaluated after 30 min after a subject put on the diagnostic lens. A well-fitted lens should be located centrally, move smoothly on blink, and show a bull's eye fluorescein pattern with a central bearing zone as about 4 to 5 mm in diameter. The parameters of an ordered orthokeratology lenses were determined based on the diagnostic lenses that gave the best fit. At each session after wearing, an experience optometrist evaluated the lens fitting again before took it off. The subjects with optimal lens fitting stayed in the study and those without were excluded.
2.3. Experimental protocol
The subjects were instructed to wear the lens while sleeping for 7 or more hours. At 1 and 7 days after lens wear, they were scheduled to visit the Eye Hospital of the Wenzhou Medical University within 2 h after awakening without removing the lenses. At each session after wearing, the lens fitting was evaluated and only the subjects had an optimal lens fitting were enrolled in the study. Then all of the measurements including refractive error, corneal tomography, thickness, and biomechanics were performed after the lens removal by the same examiner.
2.4. Corneal topography
Corneal topography was performed at baseline and at each follow-up visit. Each eye was measured multiple times and the 3 images with scores higher than 95 were taken into consideration. Changes of corneal curvature were determined based on the values from the steep and flat keratometry at the corneal apex.
2.5. Thickness measurement of different corneal layers
As reported in previous studies,[6,20] a custom-built UHR-OCT instrument was used to measure the changes of different corneal layers’ thickness, including central epithelium thickness (CET), central Bowman layer thickness (CBT), central stroma thickness (CST), and CCT. The specially designed spectrometer in the system can achieve an axial resolution as high as 3 μm and an imaging depth about 2 mm, which enables clear distinguishing of the corneal sublayers. The system can complete 24 K scans per second, and the scan width was 8.425 and 8.418 m in the horizontal and vertical meridians, respectively. To complete the scan, the subjects sat in front the slit lamp, where the scanning tip was mounted, and maintained their fixation on an external target proved. The central UHR-OCT beam was set on the corneal apex that could be normally identified by a specular reflection, and the central cornea was imaged. The same optometrist performed all of the UHR-OCT scanning in this study to minimize the variation that could be caused by different performers.
A custom software[6] was used to measure the thickness of different corneal layers. To segment boundaries of epithelium, Bowman layer, and stroma, 4 to 5 points along the line separating the 2 adjacent layers were manually identified first (Fig. 1). A polynomial line was fit through those identified dots with the least-square algorithm to outline the each boundary between the layers. Finally, the real values were derived with a refraction correction algorithm and to calculate the thickness of different corneal layers. With consideration of the possible lens decentralization and shifting of the measurement locations after orthokeratology lens treatment, a 1-mm diameter zone (222 pixels) around the corneal apex was selected for data analysis as the central area of cornea.
Figure 1.
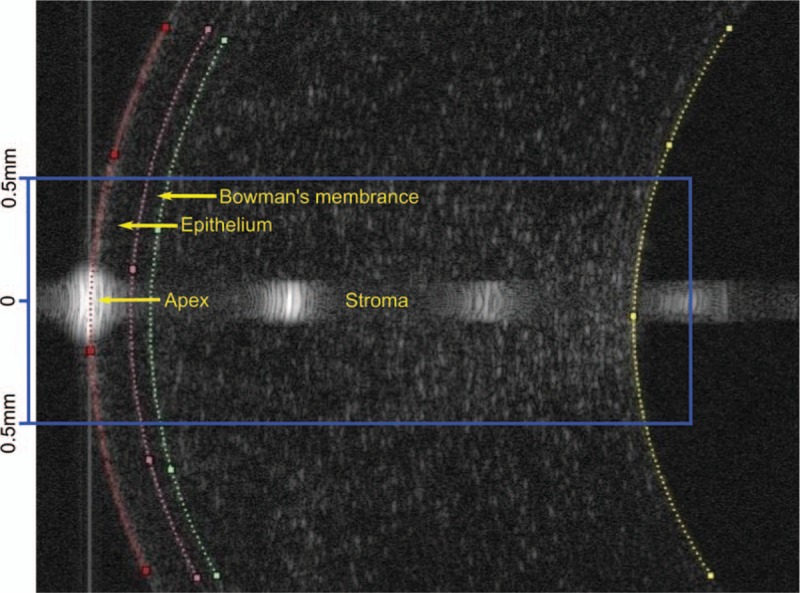
An ultra-high resolution optical coherence tomography corneal image showing the segmentation of the corneal epithelium, Bowman, and stromal layers.
2.6. Corneal biomechanics
CH and CRF were measured by the ocular response analyzer (Reichert Ophthalmic Instruments, Depew, NY). Two measurements on intraocular pressure were also obtained, including Goldmann intraocular pressure (IOPg) and corneal-compensated intraocular pressure (IOPcc). For each eye of every subject, a maximum of 10 consecutive readings were made to obtain 3 outputs with waveform score ≥ 3.6 to ensure that the quality of the waveform signals was maintained. The best 3 outputs with the highest waveform scores were averaged as the representative value for the eye.
2.7. Statistical analysis
For each subject, only right eye's data were included for analysis. R version 3.3.1 (http://www.r-project.org/) was used to conduct statistical analysis. Kolmogorov–Smirnov test was applied to test if the data were normally distributed. The level of statistical significance was set at P = .05. One-way analysis of variance with repeated measure was applied to see if there was significant difference between the baseline and the wearing sessions. Paired t tests with P values adjusted by Bonferroni corrections were used for post hoc tests. Because there were strong correlations between predictor variables, partial least square linear regression (PLSLR) was performed first, followed by multiple regression, to reveal the relationship between corneal biomechanics and anterior segment parameters at baseline and after lens wear.
3. Results
3.1. Changes in spherical equivalent refraction, biomechanics, corneal curvature, IOP, and layer thickness
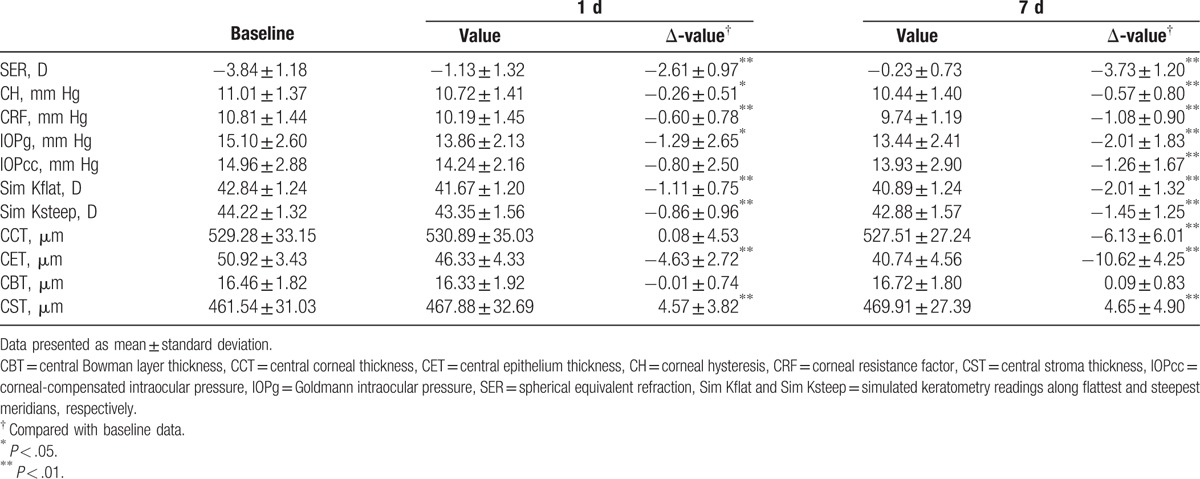
Twenty-three eyes from 23 subjects were involved in the study. During the early stage of orthokeratology, the refractive errors immediately decreased significantly from day 1 and showed further reduction by day 7. Biomechanical measurements, including CH and CRF, quickly decreased significantly from day 1 to 7. IOP showed a similar trend. Corneal curvature became significantly flatter on both meridians from day 1 and remained so at day 7. Among the corneal layers, Bowman layer showed little change in thickness. The epithelial layer became significantly thinner from day 1 and showed further thinning at day 7. By contrast, the stromal layer became significantly thicker from day 1 and remained so at day 7. Because of the combination of the changes of epithelial and stromal layer, the CCT showed no significant change at day 1 and became significantly thinner at day 7 (Table 1).
Table 1.
Changes in refraction error, biomechanics, corneal curvature, intraocular pressure, and layer thickness.
3.2. Correlations between corneal biomechanics and anterior segment parameters
Due to the high correlation between the measurements, such as the thickness of different layers, PLSLR analysis was used to find the correlation between biomechanics and other parameters.
Analysis was first performed on baseline data. The computation of regression coefficients was performed with the number of components set to 5 because the root mean squared error of prediction significantly reduced at this number for both CH and CRF (Fig. 2). It was evident that CH and CRF were only highly correlated with IOPg and IOPcc (Table 2), not other parameters.
Figure 2.
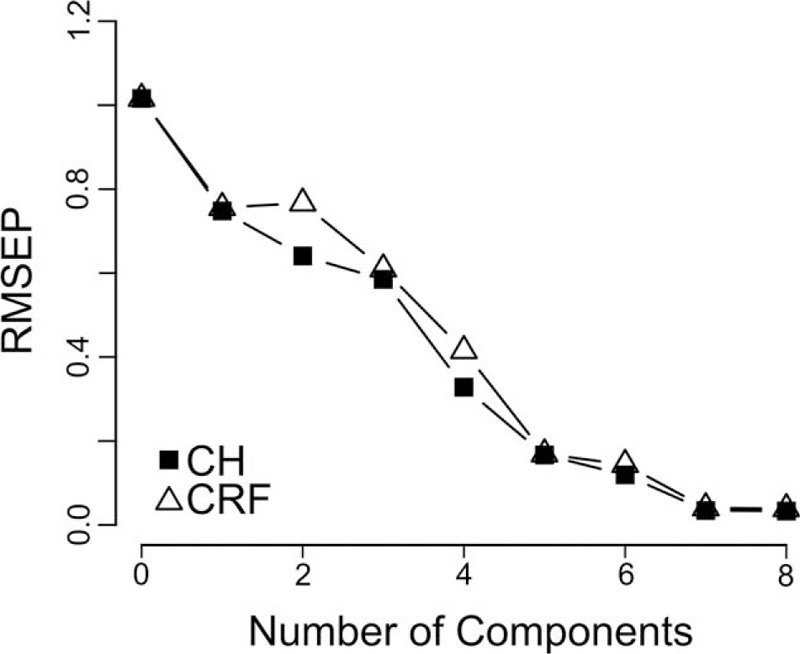
RMSEP curves for partial least squares linear regression models. This figure showed the effect of the number of components on the precision of CH and CRF regression models at baseline. CH = corneal hysteresis, CRF = corneal resistance factor, RMSEP = root mean squared error of prediction.
Table 2.
Coefficients of PLSLR predictive models for corneal hysteresis and corneal resistance factor at baseline.
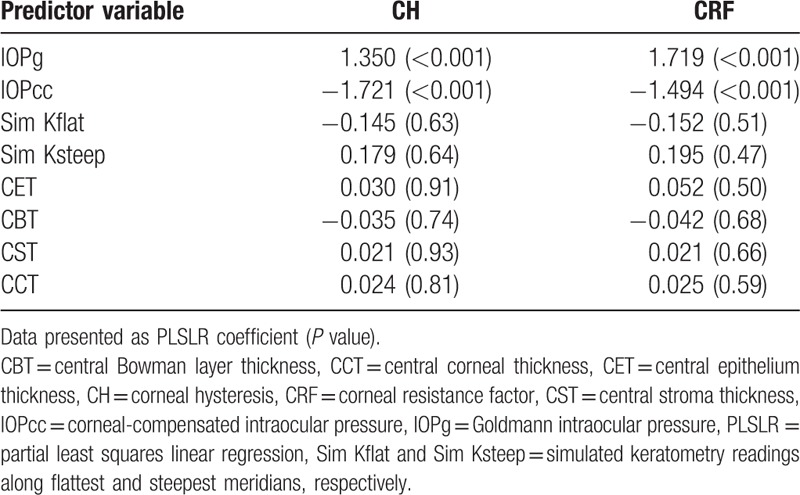
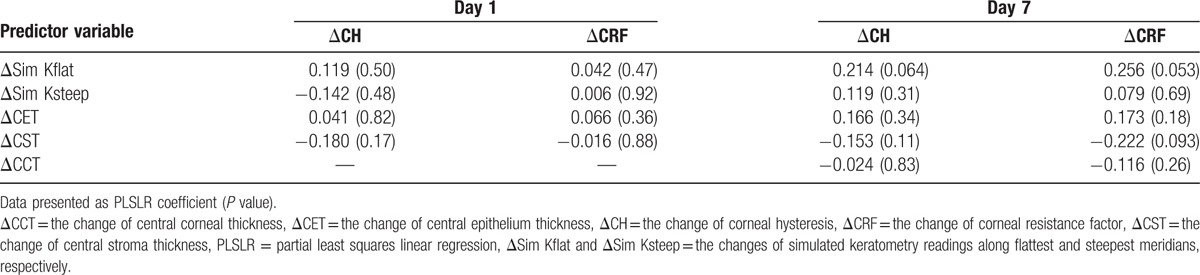
The extremely high correlation between corneal biomechanics and IOP might have masked the true relationship between the biomechanical and morphological changes during early orthokeratology. In the following analysis, we removed IOP from the regression models and our results are shown in Table 3. At baseline, both CH and CRF were significantly correlated with CCT, CBT, and CST. At day 1 and 7 after orthokeratology, both CH and CRF were significantly correlated with CST and CCT. However, CH and CRF were only correlated with CBT at day 1. PLSLR was also performed on the changes in biomechanical measurements over morphological changes. No significant correlation was found at either day 1 or 7 (Table 4).
Table 3.
Coefficients of PLSLR predictive models for corneal hysteresis and corneal resistance factor at baseline and after orthokeratology.
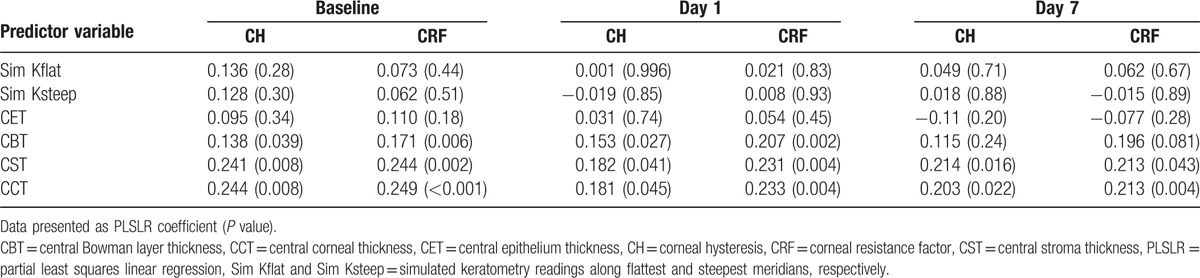
Table 4.
Coefficients of PLSLR predictive models for the change of corneal hysteresis and corneal resistance factor at day 1 and 7.
4. Discussion
The first important finding in our study was that corneal biomechanics were related to the thickness of stroma and Bowman layer, not the thickness of epithelium or corneal curvature. After orthokeratology, corneal biomechanics correlated with CST and CBT at day 1, but only with CST at day 7. It is natural to think that stroma is responsible for the mechanical properties of cornea because it constitutes 90% of corneal thickness.[21] However, the role of Bowman layer remains controversial. Seiler reported removal of Bowman layer did not alter the mechanical properties of cornea.[22] Conversely, Dupps reported that both stroma and Bowman layer support the major biomechanical tension of the cornea because of the existence of collagen fibrils exist in these 2 layers.[23] Our finding suggests that both stroma and Bowman play significant roles in cornea biomechanics but it needs further studies to confirm since we found neither CH nor CRF was correlated with CBT at day 7 after orthokeratology, which may due to the limit of the subject number in this study.
The other finding was that the changes in corneal biomechanics were not associated with the changes of the anterior segment parameters in the early stage after orthokeratology. Our results were in agreement with Nieto-Bona's results except they did not measure corneal sublayers’ thickness and the lens wearing durations were 15 and 30 days.[11] Although 2 other studies reported the existence of the correlation, their results should be treated with caution. Gonzalez-Meijome's study showed the reduction of CH were correlated with changes of CCT, but they used ultrasound pachymetry to measure CCT, which required topical anesthesia and the duration of lens wearing was only 3 h.[13] Chen found that the change of CRF was correlated to the changes of corneal curvature but the reduction of CRF did not follow the degree of flattening of the corneal curvature.[10] In the following section, we will discuss what accounts for the lack of association between those 2 aspects.
One potential reason for a negative finding could be measurement errors in some of the measurements. But this possibility could be eliminated based on the following several considerations. First, similar to previous studies, our results reported a strong correlation between biomechanics and CCT at baseline. Aachal Kotecha's and Shen's studies showed that CH and CRF were strongly positively associated with CCT.[24,25] Second, the changes in anterior segment parameters were similar to previous reports. In our study, we reported thinner CET, unchanged CBT, and thicker CST at day 1 and 7. Thinner CET has been reported as much as 5% in Wang's study after 1 night of orthokeratology,[7] 10% in Haque's study,[8] and 13% to 32% in Nieto-Bona's studies.[26,27] Unchanged CBT was reported in Lian's study.[6] Thicker stroma, by 5.7%, was also found in Haque's study after 1 day of lens wearing[8] and in Alharbi's study.[28] We also observed thinning of CCT at day 7, similar to Nieto-Bona's findings 1 month after orthokeratology.[27] Third, our observed changes in corneal biomechanics after orthokeratology were similar to previous reports. We found that both CH and CRF decreased at day 1 and 7, which were similar to Mao's and Yeh's results.[12,29]
Since our results on baseline measurements and on biomechanical and anterior segment parameters changes after wearing orthokeratology agree well with previous studies, this points to a second potential explanation, that the causes leading to reduced biomechanics might be at a cellular level, which is beyond the detection of our measurements. Zhong et al found the density of keratocytes decreased in the stroma and the shape of keratocytes also changed after 8 h of lens wearing.[26] Nieto-Bona found a reduction of basal cells and an increase of activated keratocytes after 15 days of lens wearing.[27] Many researchers have reported central epithelium thinning and peripheral thickening and thought that epithelium changes contribute to the refractive change. Matsubara found histological changes in epithelial distribution in rabbit corneas as a result of compressive force produced by orthokeratology lens after 7 days of wear.[28] Ding et al[29] found a decrease in intercellular junctions after orthokeratology. These previous studies suggested that there were many other corneal microstructures changed during orthokeratology that may contribute to the changes in corneal biomechanics. Further studies are needed to investigate more details of corneal behavior and their correlation with biomechanics while undergoing orthokeratology.
One limitation of this study is relatively small sample size. The negative finding of the relationship between changes of corneal biomechanics and anterior segment parameters may come from the small number of eyes in 1 and 7 days after orthokeratology. Nonetheless, we observed statistically significant reduction of corneal biomechanics, changes of corneal thickness and positive correlation between corneal biomechanics with CCT, CBT, and CST in the early stage of orthokeratology. Results of this study warrant further investigations on this field in order to fully understand the course of changes in corneal biomechanics during orthokeratology. Further studies considering large samples are needed to confirm the relationship and other corneal histology or morphology parameters should be taken into account.
Footnotes
Abbreviations: CBT = central Bowman layer thickness, CCT = central corneal thickness, CET = central epithelium thickness, CH = corneal hysteresis, CRF = corneal resistance factor, CST = central stroma thickness, IOPcc = corneal-compensated intraocular pressure, IOPg = Goldmann intraocular pressure, PLSLR = partial least square linear regression, UHR-OCT = ultra-high resolution optical coherence tomography.
This study was supported by research grants from the National Major Equipment Program of China (2012YQ12008004 to FL) and the National Nature Science Foundation of China Grant (No. 81570880 to FL).
The authors have no funding and conflicts of interest to disclose.
References
- [1].Swarbrick HA. Orthokeratology review and update. Clin Exp Optom 2006;89:124–43. [DOI] [PubMed] [Google Scholar]
- [2].Swarbrick HA, Wong G, O’Leary DJ. Corneal response to orthokeratology. Optom Vis Sci 1998;75:791–9. [DOI] [PubMed] [Google Scholar]
- [3].Maseedupally V, Gifford P, Lum E, et al. Central and paracentral corneal curvature changes during orthokeratology. Optom Vis Sci 2013;90:1249–58. [DOI] [PubMed] [Google Scholar]
- [4].Lian Y, Shen M, Huang S, et al. Corneal reshaping and wavefront aberrations during overnight orthokeratology. Eye Contact Lens 2014;40:161–8. [DOI] [PubMed] [Google Scholar]
- [5].Alharbi A, Swarbrick HA. The effects of overnight orthokeratology lens wear on corneal thickness. Invest Ophthalmol Vis Sci 2003;44:2518–23. [DOI] [PubMed] [Google Scholar]
- [6].Lian Y, Shen M, Jiang J, et al. Vertical and horizontal thickness profiles of the corneal epithelium and Bowman's layer after orthokeratology. Invest Ophthalmol Vis Sci 2013;54:691–6. [DOI] [PubMed] [Google Scholar]
- [7].Wang J, Fonn D, Simpson TL, et al. Topographical thickness of the epithelium and total cornea after overnight wear of reverse-geometry rigid contact lenses for myopia reduction. Invest Ophthalmol Vis Sci 2003;44:4742–6. [DOI] [PubMed] [Google Scholar]
- [8].Haque S, Fonn D, Simpson T, et al. Corneal refractive therapy with different lens materials, part 1: corneal, stromal, and epithelial thickness changes. Optom Vis Sci 2007;84:343–8. [DOI] [PubMed] [Google Scholar]
- [9].Reinstein DZ, Gobbe M, Archer TJ, et al. Epithelial, stromal, and corneal pachymetry changes during orthokeratology. Optom Vis Sci 2009;86:E1006–14. [DOI] [PubMed] [Google Scholar]
- [10].Chen D, Lam AKC, Cho P. A pilot study on the corneal biomechanical changes in short-term orthokeratology. Ophthalmic Physiol Optics 2009;29:464–71. [DOI] [PubMed] [Google Scholar]
- [11].Nieto-Bona A, Gonzalez-Mesa A, Villa-Collar C, et al. Biomechanical properties in corneal refractive therapy during adaptation period and after treatment interruption. J Optom 2012;5:164–70. [Google Scholar]
- [12].Mao XJ, Huang CC, Chen L, et al. A study on the effect of the corneal biomechanical properties undergoing overnight orthokeratology. Zhonghua Yan Ke Za Zhi 2010;46:209–13. [PubMed] [Google Scholar]
- [13].Gonzalez-Meijome JM, Villa-Collar C, Queiros A, et al. Pilot study on the influence of corneal biomechanical properties over the short term in response to corneal refractive therapy for myopia. Cornea 2008;27:421–6. [DOI] [PubMed] [Google Scholar]
- [14].Shah S, Laiquzzaman M, Bhojwani R, et al. Assessment of the biomechanical properties of the cornea with the ocular response analyzer in normal and keratoconic eyes. Invest Ophthalmol Vis Sci 2007;48:3026–31. [DOI] [PubMed] [Google Scholar]
- [15].Fontes BM, Ambrosio R, Jr, Jardim D, et al. Corneal biomechanical metrics and anterior segment parameters in mild keratoconus. Ophthalmology 2010;117:673–9. [DOI] [PubMed] [Google Scholar]
- [16].Xu Z, Jiang J, Yang C, et al. Value of corneal epithelial and Bowman's layer vertical thickness profiles generated by UHR-OCT for sub-clinical keratoconus diagnosis. Sci Rep 2016;6:31550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Li Y, Tan O, Brass R, et al. Corneal epithelial thickness mapping by Fourier-domain optical coherence tomography in normal and keratoconic eyes. Ophthalmology 2012;119:2425–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Kirwan C, O’Keefe M. Corneal hysteresis using the Reichert ocular response analyser: findings pre- and post-LASIK and LASEK. Acta Ophthalmol 2008;86:215–8. [DOI] [PubMed] [Google Scholar]
- [19].Pepose JS, Feigenbaum SK, Qazi MA, et al. Changes in corneal biomechanics and intraocular pressure following LASIK using static, dynamic, and noncontact tonometry. Am J Ophthalmol 2007;143:39–47. [DOI] [PubMed] [Google Scholar]
- [20].Du C, Wang J, Cui L, et al. Vertical and horizontal corneal epithelial thickness profiles determined by ultrahigh resolution optical coherence tomography. Cornea 2012;31:1036–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Shah S, Laiquzzaman M, Yeung I, et al. The use of the Ocular Response Analyser to determine corneal hysteresis in eyes before and after excimer laser refractive surgery. Cont Lens Anterior Eye 2009;32:123–8. [DOI] [PubMed] [Google Scholar]
- [22].Seiler T, Matallana M, Sendler S, et al. Does Bowman's layer determine the biomechanical properties of the cornea? J Refract Surg 1992;8:139–42. [PubMed] [Google Scholar]
- [23].Dupps WJ, Jr, Wilson SE. Biomechanics and wound healing in the cornea. Exp Eye Res 2006;83:709–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Kotecha A, Russell RA, Sinapis A, et al. Biomechanical parameters of the cornea measured with the Ocular Response Analyzer in normal eyes. BMC Ophthalmol 2014;14:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Shen M, Fan F, Xue A, et al. Biomechanical properties of the cornea in high myopia. Vision Res 2008;48:2167–71. [DOI] [PubMed] [Google Scholar]
- [26].Zhong XW, Chen XL, Xie RZ, et al. Differences between overnight and long-term wear of orthokeratology contact lenses in corneal contour, thickness, and cell density. Cornea 2009;28:271–9. [DOI] [PubMed] [Google Scholar]
- [27].Nieto-Bona A, Gonzalez-Mesa A, Nieto-Bona MP, et al. Short-term effects of overnight orthokeratology on corneal cell morphology and corneal thickness. Cornea 2011;30:646–54. [DOI] [PubMed] [Google Scholar]
- [28].Matsubara M, Kamei Y, Takeda S, et al. Histologic and histochemical changes in rabbit cornea produced by an orthokeratology lens. Eye Contact Lens 2004;30:198–204. [DOI] [PubMed] [Google Scholar]
- [29].Ding H, Pu A, He H, et al. Changes in corneal biometry and the associated histology in rhesus monkeys wearing orthokeratology contact lenses. Cornea 2012;31:926–33. [DOI] [PubMed] [Google Scholar]


