Abstract
Performing everyday actions requires fine postural control, which is a major focus of functional rehabilitation programs. Among the various range of training methods likely to improve balance and postural stability, motor imagery practice (MIP) yielded promising results. Transcranial direct current stimulation (tDCS) applied over the primary motor cortex was also found to potentiate the benefits of MIP on upper-limb motor tasks. Yet, combining both techniques has not been tested for tasks requiring fine postural control. To determine the impact of MIP and the additional effects of tDCS, 14 participants performed a postural control task before and after two experimental (MIP + anodal or sham tDCS over the primary motor cortex) and one control (control task + sham tDCS) conditions, in a double blind randomized study. Data revealed a significant decrease of the time required to perform the postural task. Greater performance gains were recorded when MIP was paired with anodal tDCS and when the task involved the most complex postural adjustments. Altogether, findings highlight short-term effects of MIP on postural control and suggest that combining MIP with tDCS might also be effective in rehabilitation programs for regaining postural skills in easily fatigable persons and neurologic populations.
Introduction
Posture is the ability to maintain an adequate body alignment relative to the gravitational vector1. From a functional viewpoint, postural control includes balance, which refers to the dynamics of the body preventing falls1. The possibility of completing every-day tasks is inherent to this basic function of human motor control. A lack of postural control leads to a loss of autonomy and a reduction of daily activities affecting the quality of life2. Therefore, in the case of severe motor impairments, recovering postural functionalities is one of the main focuses of rehabilitation programs3.
Among the various range of training methods used to improve balance and postural stability, motor imagery as well as action observation provided promising results4. Motor imagery is the internal representation of a movement without engaging its actual execution. The benefits of motor imagery practice (the repeated use of motor imagery, MIP) on performance have been widely reported in sport and rehabilitation domains5,6. In the specific context of postural control, Choi et al.7 provided evidence that MIP enhanced motor performance during a weight-shifting task. They revealed that MIP significantly decreased the time required to perform the postural task, although to a lesser extent than physical training. In a recent study, Taube et al.4 showed that MIP might contribute to both promote learning of postural tasks and improve dynamic balance in unstable and non-predictable environments. MIP has further been found to activate the neural regions involved in gait planing8, and might therefore contribute to enhance postural control in easily fatigable and physically impaired populations such as elderly persons9,10 and stroke patients11–14. Specifically, decreased anteroposterior and mediolateral sway, as well as increased holding balance durations on one leg, were measured after MIP during static postural tasks (maintaining a stable stance). Benefits from this method were also recorded for dynamic components of postural control (i.e., remaining stable while performing movements, such as during locomotor tasks). MIP effects on motor performance are frequently interpreted as an account of the neurofunctional equivalence with the physical practice of the same movement15. A handful of neuroimaging studies demonstrated that these types of practice shared overlapping brain activations, including the primary motor cortex [M1]16–20. MIP may thus affect activity-dependent plasticity (i.e., the capacity of neurons to adjust their connectivity to the cognitive/behavioral demand), the neural correlate of the motor learning process21. Motor imagery has also been shown to increase the motor evoked potentials and decrease the depolarization threshold of cortical motor regions22–24, thus matching the neural excitability changes elicited by physical practice, and certainly promoting motor learning.
Facilitation of motor learning through modulations of the cortical excitability can also result from transcranial direct current stimulation (tDCS), which is a noninvasive brain stimulation method25. Neural excitability increases induced by anodal tDCS potentiates inter-neurons communication during physical practice (i.e., increased synaptic gain), thus facilitating motor learning26. This might explain the positive impact of anodal tDCS applied during physical practice on sequential/visuomotor tasks, reaction times and functional performances27. Interestingly, applying anodal tDCS over M1 during motor imagery of a hand movement was found to increase Mu desynchronization, a neural signature of movement execution, imagination and observation28. Anodal tDCS might thus facilitate activity-dependent neuroplasticity within the neural networks recruited during motor imagery, thereby accounting for MIP effects on performance. Foerster et al.29 confirmed the enhancement of motor performance through MIP paired with anodal tDCS applied over M1. While MIP alone tended to improve handwriting, additional gains were recorded when MIP was combined with anodal tDCS. Saimpont et al.30 finally reported greater performance increase after MIP combined with anodal tDCS compared to both MIP and tDCS alone in a sequential task.
Spurred by the results mentioned above, the present study was designed to investigate whether anodal tDCS applied over M1 might contribute to potentiate the benefits of MIP on a postural task. As the effects of tDCS alone on postural skills have been the focus of previous studies31,32, we hypothesized that MIP alone and MIP paired with anodal tDCS might contribute to improve performance on a weight-shifting task.
Results
Motor imagery ability data
Participants’ KVIQ mean visual score (±SD) was 3.46 (±0.70), while their KVIQ mean kinesthetic score was 3.42 (±0.72). Mean total KVIQ score was 3.44 (±0.61).
The comparison of vividness scores on the 5-points Likert scale (Wilcoxon's paired tests) after MI training under MItDCS (3.28 ± 0.72) and MIsham (2.92 ± 0.82) was not statistically significant (V = 18, p = 0.11).
Motor performance data
The analysis of validation times revealed a CONDITION × TEST × PLAN interaction (F(2,1235) = 7.51, p < 0.001, partial η2 = 0.03). As shown in Fig. 1A, a decrease from the Pretest to the Posttest of validation times of Ahead targets was recorded under both MItDCS (Pretest: 4.17 s ± 1.19, Posttest: 3.98 s ± 1.39; p(ART) = 0.02) and MIsham (Pretest: 4.18 s ± 1.27, Posttest: 3.97 s ± 1.36; p(ART) = 0.03), but not for the Control condition (Pretest: 4.16 s ± 1.58, Posttest: 4.13 s ± 1.47; p(ART) > 0.05). Furthermore, we observed a decrease in validation times from the Pretest (4.37 s ± 1.99) to the Posttest (3.93 s ± 1.34) for Behind targets under MItDCS only (p(ART) = 0.01, Fig. 1B).
Figure 1.
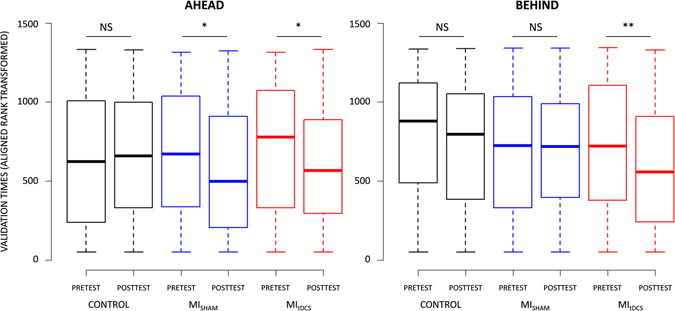
Effect of Control, MISHAM and MItDCS conditions on Ahead and Behind targets validation.
A CONDITION × TEST × DIFFICULTY interaction was also present (F(2,1235) = 4.09, p(ART) = 0.01, partial η2 = 0.07). Validation times of Hard targets decreased from the Pretest to the Posttest under both MItDCS (Pretest: 4.97 s ± 2.25, Posttest: 4.31 s ± 1.31; p(ART) = 0.03) and MIsham (Pretest: 4.91 s ± 1.66, Posttest: 4.38 s ± 1.38; p(ART) = 0.002), but not under Control (Pretest: 5.06 s ± 1.98, Posttest: 4.99 s ± 1.84; p(ART) > 0.05). Posttest validation times of Hard targets were lower during MItDCS than during Control (p(ART) = 0.03) while the comparison between MIsham and Control approached the statistical threshold (p(ART) = 0.07) (Fig. 2A). Noteworthy, validation times of Easy targets decreased from the Pretest to the Posttest only after the MItDCS training (Pretest: 4.04 s ± .79, Posttest: 3.82 s ± .76; p(ART) = 0.02, Fig. 2B). The CONDITION × TEST × DIRECTION interaction approached the statistical threshold (F(2,1235) = 2.50, p = 0.08). Lastly, no CONDITION × TEST × LATERALITY interaction emerged (F(4,1235) = 0.90, p > 0.05).
Figure 2.
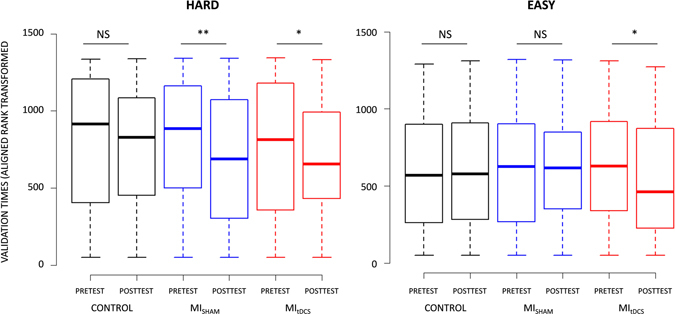
Effect of Control, MISHAM and MItDCS conditions on Easy and Hard targets validation.
In contrast to PLAN, DIFFICULTY and LATERALITY (F(1,1235) = 77.92, p < 0.001, partial η2 = 0.01; F(1,1235) = 228.41, p < 0.001, partial η2 = 0.06; F(2,1235) = 19.34, p < 0.001, partial η2 = 0.01, respectively), there was no main effect of DIRECTION on validation times (F(1,1235) = 0.03, p > 0.05). Participants overall exhibited longer validation times for Behind (4.22 s ± 1.88) compared to Ahead (4.04 s ± 1.13) targets (p(ART) = 0.002), and comparison between Behind targets compared to Neutral approached the statistical threshold (Neutral: 4.08 ± 1.14; p(ART) = 0.09). Hard targets also involved longer validation times than Easy targets (Hard: 4.91 s ± 2.30; Easy: 4.05 ± 1.00; p(ART) < 0.001), while both Dominant (4.16 s ± 1.47) and Non-dominant (4.20 s ± 1.63) targets involved longer validation times than Neutral (3.94 s ± 1.03) targets (p(ART) = 0.02 and p(ART) = 0.01, respectively).
The factorial analysis yielded a CONDITION × TEST interaction (F(2,1235) = 11.80, p < 0.001). Validation times were reduced during the Posttest compared to the Pretest under both MItDCS (Pretest: 4.23 s ± 1.47, Posttest: 3.86 s ± .91; p(ART) = 0.002) and MIsham (Pretest: 4.16 s ± 1.26, Posttest: 3.93 s ± 1.08; p(ART) = 0.02), but remained similar during Control (Pretest: 4.15 s ± 1.25, Posttest: 4.06 s ± 1.16; p(ART) > 0.05). Validation times under MItDCS were lower compared to Control during the Posttest (p(ART) = 0.01), but there was no difference in Posttest validation times between MItDCS and MIsham, nor between MItDCS and Control (p > 0.05, Fig. 3 ).
Figure 3.
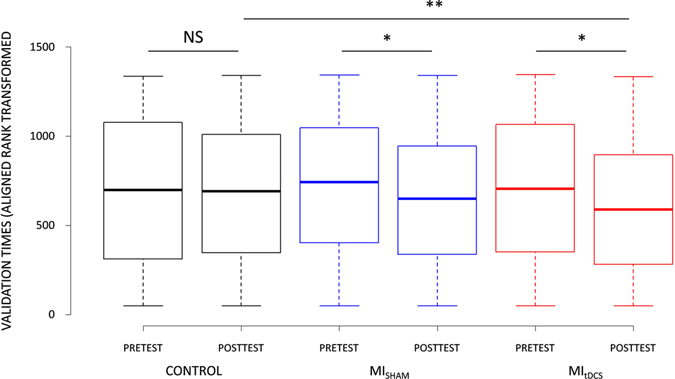
Effect of Control, MISHAM and MItDCS conditions on postural task validation.
Discussion
This study was designed to investigate the effects of MIP on postural control and determine the additional benefits when paired with anodal tDCS over M1. Data revealed i) a significant decrease of the time required to perform the postural task after MIP, and ii) greater performance gains when MIP was coupled with anodal tDCS when the task involved high demands in terms of postural adjustments.
While there is ample evidence that MIP contributes to improve motor performance and promote motor learning, its potential benefits on the postural control have been far less examined. Our data confirmed that MIP might significantly enhance motor performance of a complex postural task. Previous behavioral studies focusing on the impact of MIP on postural control (usually incorporated in a locomotor task) used longitudinal assessments and involved several training sessions per week, within a span of at least 2 weeks11,33–37. Interestingly, the present study extends these findings and provides evidence that a small amount of MIP without any physical practice might be sufficient to impact the postural control. The short-term performance gains (time decrease of 8%) observed after only one single MIP session of 12 min were slightly lower than those reported by Choi et al.7 after 15 imagery sessions of 30 min (time decrease of 14%) for a postural task requiring to reach and validate targets located forward. Malouin et al.38 underlined the potential of one single session of MIP to elicit significant enhancement of a functional movement including postural skills in stroke patients, i.e., a greater loading on the affected limb while standing up and sitting down. In this study, the improvement on limb loading was recorded consecutively to 30 min of MIP. As patients also benefited from some physical execution trials in addition to MIP (physical practice/mental practice ratio of 1 to 5), the present results pioneer that a single session of 12 min of MIP without any physical practice may be effective to improve postural control.
It is commonly agreed that the neurofunctional equivalence between motor imagery and actual execution of the same movement is the most plausible explanation for MIP effects on motor performance19,21. In a recent study investigating the neural networks involved during motor imagery of a postural task, Taube et al.39 reported activations in the putamen, the cerebellum, and the supplementary motor area, which play a crucial role during postural control40,41. These regions were also found to be strongly involved during the kinesthetic modality of imagery42,43. Although this remains a working hypothesis, we assume that 12 min of MIP using kinesthetic imagery would predominantly engage these task-specific networks, and therefore prompt performance gains.
A second finding of this study is that applying anodal tDCS over M1 during MIP resulted in slightly greater performance compared to both MIP with sham tDCS and Control conditions. The additional effect of anodal tDCS on MIP-induced performance improvements confirms the results by Foerster et al.29 where a single session of MIP yielded to significant performance gains only when imagery was coupled with tDCS. Using a finger sequential task, Saimpont et al.30 further showed that MIP contributed to improve performance, however with results when tDCS was simultaneously applied over M1. Yet, only these two experimental studies focusing on upper-limb motor performance investigated the combined effect of both tDCS and MIP. The present study tends to support the effectiveness of applying tDCS over M1 during MIP to improve postural control. How anodal tDCS could increase the impact of MIP may be explained by greater stimulation of M1. As enhanced cortical excitability is known to facilitate motor learning25, combining both techniques is likely to improve the strengthening of synaptic transmission. Specifically, Nitsche et al.44 showed that applying tDCS over M1 might modulate the motor cortical transmitter system by reducing the activity of the gamma-aminobutyric acid (GABA)-ergic system. Whether a similar mechanism is effective when combining MIP with anodal tDCS yet remains a working hypothesis awaiting experimental investigation. Given the diffuse nature of tDCS45, however, some areas adjacent to M1 may also have been stimulated concomitantly. In particular, we cannot totally rule out that the SMA, which plays an important role in postural control40,41, and is activated during motor imagery of postural tasks39, was also stimulated. Although Antal et al.46 reported a decreased activation in this region after anodal tDCS over M1, divergent findings have been found when directly applying tDCS over the SMA. While Kaminski et al.47 showed that stimulating the SMA impaired motor learning of a dynamic balance task, some recent data provided evidence of substantial performance gains in different motor tasks48–51. Taken together, the contribution of the SMA, although being debated, can thus not be completely ruled out in the present study.
The beneficial effects of applying tDCS over M1 during MIP were mainly observed when looking at the fine postural adjustments required by the task. The present paradigm involved targets located at different directions with two levels of difficulty (Easy and Hard targets), both forward and backward (Ahead and Behind targets). Performance improvements during both MItDCS and MIsham conditions were recorded for Hard targets, whereas the time needed to complete Easy targets was reduced only under the MItDCS condition. Different strategies might be used to maintain balance. Validating Hard targets may imply a shift of the CoP soliciting the hip joint, whereas minor deviations, such as those required to validate the Easy targets, might primarily manage through ankle involvement52. Furthermore, one can postulate that the margin for performance improvements was higher for Hard than for Easy. Data therefore demonstrate that only MItDCS resulted in performance gains for both types of targets. Likewise, both conditions yielded to significant performance enhancement for Ahead targets, but only MItDCS improved the postural control for trials involving Behind targets. Considering the importance of rehearsal in motor learning, backward CoP displacement are more complicated than those in the forward direction where daily activities are more frequently oriented (e.g., locomotion, prehension). Furthermore, while movements in the forward direction might benefit from a broad support area (i.e., the 5 toes and the midfoot), backward movements rely on a narrow base (i.e., the heel), hence increasing the difficulty of validating Behind targets53. Taken together, these results suggest that the cortical activity in M1 induced by tDCS during MIP might contribute to reinforce the positive effect of MIP and result in greater performance for particularly demanding postural adjustments. As suggested by Foerster et al.29 and Saimpont et al.30, tDCS may therefore appear a promising stimulation method to potentiate the effects of MIP.
As with all experimental research, the present pilot study has some limitations which should be overcome in future experiments. As mentioned previously, applying tDCS over M1 might have activated other cortical adjacent regions, such as the SMA. One alternative to resolve this issue might be to stimulate M1 and the SMA in two separate sessions, as shown by Foerster et al.29. From a pure methodological viewpoint, however, Lang et al.54 argued that tDCS stimulation is likely to induce widespread bi-directional changes in regional neuronal activity, hence resulting in profound effects on the overall level of regional activity in many other brain regions. Future studies should certainly combine electroencephalographic measurements to tDCS stimulation in order to better understand and improve the neurophysiological correlates of the brain activity during each experimental condition. Within a behavioral perspective, additional postural variables (e.g., sway length) could have been informative regarding the qualitative aspects of the experimentally-induced changes in postural control. Here, the data revealed that both MItDCS and MIsham led to performance gains, as shown by decreased time to validate targets. Interestingly, Choi et al.7 reported that similar effects were not paralleled by reduced sway length, hence suggesting that participants took less time to perform the task, but were not necessarily more accurate. Replicating the study while recording postural sway might thus be relevant to clarify this issue. Third, future studies might include retention tests in order to see whether the effects observed after one single session of MIP are strictly maintained over time. Fourth, the experimental design did not involve a tDCS “only” condition. Based on recent findings by Saimpont et al.30, however, coupling MIP with tDCS applied over M1 resulted in significant greater performance compared to tDCS alone. Finally, other experimental conditions should ideally be included in future experimental designs to adequately frame and conclude about the relevance of combining MIP and tDCS. A pure physical practice condition might be necessary to compare the effects of physical and mental practice. Investigating the effects of tDCS during different ratios of physical and MIP (see Reiser et al.55) might also be very informative to improve the reasoning about the functional relevance of combining MIP with tDCS.
Overall, our results provide evidence of short-term beneficial effects of both MIP combined with tDCS and MIP alone on postural control. Combining MIP with tDCS applied over M1 might further appear a promising approach to enhance fine postural skills. Determining whether combining tDCS during MIP leads to greater performance than performing MIP before/after a tDCS session may be an exciting focus of research for future studies. More generally, these results have theoretical and practical applications in both motor learning and (neuro)rehabilitation. Clinical studies should notably address the relevance of combining both methods as an adjunctive rehabilitation practice to classical physical therapy for regaining postural skills in easily fatigable persons (e.g., elderly people) and neurologic populations (e.g., stroke patients).
Methods
Participants
Fourteen right-handed healthy participants (8 males, 6 women, mean age 25.78 ± 3.76 years) voluntarily participated in this double-blind study, which was approved by the Research Ethics Committee of the Center of Research and Innovation in Sport (University Claude Bernard Lyon 1). Handedness was surveyed by a brief self-report patient-based questionnaire adapted from Olfield56. Only persons reporting a strong dominance of the right hand to perform everyday activities were recruited in the experimental design. Contra-indication to tDCS and musculoskeletal disorders were considered exclusion criteria. Shoe size above 10.5 (US size) was also an exclusion criterion to avoid feet extending beyond the postural tool assessment area. The experiment was performed in accordance with relevant guidelines and regulations. Informed consent in agreement with the terms of the Declaration of Helsinki (2013) was obtained from all participants. The procedure of the experiment and the tasks were individually explained, but no information was provided about the objectives of the study or the variables of interest before experimentation began. Participants were debriefed at the end of the study. Due to the novelty of the postural task investigated in this pilot study, and the lack of corresponding information in the literature, we were not able to run a power analysis to determine sample size a priori.
Design
The experiment took place in a quiet room, lit by homogeneous white light, i.e., in stable and reproducible environmental conditions. Two experimental (MItDCS, MIsham) and one control (Control) conditions were scheduled, within a test-retest procedure. All sessions were randomized and separated by one week. Participants were thus randomly assigned to one of the 6 possible session orders, to avoid both practice and order effects. Before engaging in the experimental design, participants were subjected to a pre-visit to assess their MI vividness (i.e., the clarity of the mental images and the intensity of the sensations perceived during MI) through the Kinesthetic and Visual Imagery Questionnaire (KVIQ-10)57. The questionnaire includes 10 items corresponding to 5 basic movements that participants must perform and then mentally imagine using both visual and kinesthetic imagery. For each movement, participants were requested to rate the clarity of the images (visual imagery) or the intensity of the sensations they perceived (kinesthetic imagery) during the imagined movement using, a 5-point analog scale. A score of 5 corresponded to the highest level of MI (images as clear as seeing and sensations as intense as perceived when performing the action). Conversely, a score of 1 corresponded to the poorest imagery (no images/no sensations).
For both experimental and Control conditions, participants were subjected to identical pre- and post-tests, and consisted on a complex postural task (Fig. 4A). Participants had to shift their center of pressure (CoP), without lifting their feet nor losing balance, to validate 16 targets that appeared in 8 different directions. CoP was measured using a Wii Balance Board (Nintendo, USA), which has shown consistent concurrent validity when tested with healthy and young people58. When compared to a laboratory force plate, Clark et al.58 found good test-retest and between-device intra-class correlation coefficient (>0.66). Moreover, the use of the Wii Balance Board as a posture measure tool was validated in young people31,32, elderly59, persons with Parkinson's disease60, visual impairment61, and reconstructed anterior cruciate ligament62. A software (Polyenco, France) was specifically developed to connect the Wii Balance Board to the computer in order to display the CoP position in a form of a cross on the screen, and randomly picture the targets to validate (Fig. 4A). Targets were located in 8 directions (Front, Back, Left, Right, Front-Left, Front-Right, Back-Left and Back-Right), at two levels of difficulty (easy and hard) directly based on the individual sustentation polygon (Fig. 5A). Coordinates of feet position were measured at six different points (thumbs, pinky fingers and heels) to delimitate the individual theoretical stability limitations in both axes, and to fix the places where targets randomly appeared for each participant. To respect the individual characteristics of the natural stance position, participants were asked to stand comfortably and motionless during measurement. Coordinates were recorded once, and then reused for each condition. Back-Left and Back-Right axes were the lines connecting the center to the heels. Front-Left and Front-Right axes connected the center to the point of equilibrium between toes (i.e., half distance between the big toe and the pinky toe, Fig. 5B). Easy targets corresponded to 20% of the theoretical maximum stability limitation, regardless of the forward/backward direction, while hard targets were placed at 50% of this limit. All Ahead targets located in the forward direction, as well as all Behind targets, located in the backward direction, were therefore either considered easy or hard. The 16 targets (one per location and difficulty) had to be validated by placing the CoP into each target during 3 s (time was cumulated if participants moved outside the target area). Participants should systematically move back to the center before validating the next target, and were never allowed to lift their feet throughout the testing session.
Figure 4.
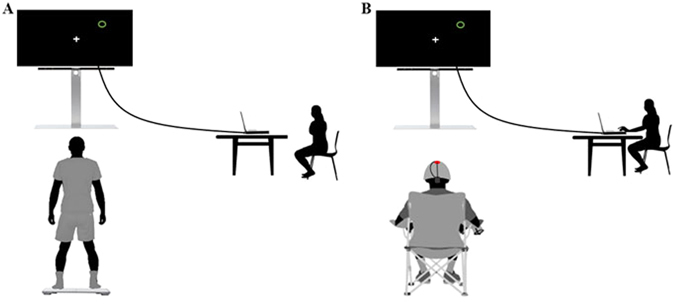
Actual performance and MI of the postural task. (A) Actual performance assessed during Pre and Post-Test. (B) MI of the task during MItDCS, MIsham and Control conditions.
Figure 5.
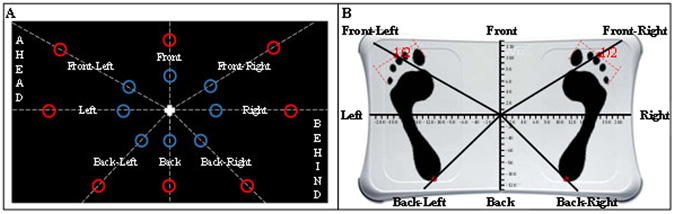
Axes and targets. (A) Location of the 16 targets on each of the 8 locations, for easy (blue targets) and hard (red targets) difficulty levels. Note that targets appeared only in green during the experimentation. (B) Measurement of individual support polygon for personalized theoretical stability limitations and directions definition.
Immediately after the Pretest, participants were subjected either to a 12 min experimental (MItDCS or MIsham) or Control condition. During each experimental condition, participants were requested to mentally imagine the postural task while receiving anodal tDCS (MItDCS condition) or sham tDCS (MIsham condition) over M1. To avoid muscular contractions and fatigue due while remaining motionless in a standing position for a long time, the MI session was performed while participants seated on a chair, at the exact place where they actually performed the postural task on the Wii Balance Board. They were asked to imagine that they validated each target by mentally shifting their body weight, through kinesthetic imagery, as well as to focus on tactile sensation of their feet on the Wii board. Using a custom made program, individual targets, similar to those presented during both pre- and post-test, randomly appeared on the screen. Participants verbally indicated when the target was validated and the investigator clicked to make the next target appear (Fig. 4B). As during both the pre- and post-test, they were asked to imagine moving back to the center before mentally validating the next appearing target. After both experimental conditions, participants rated on a 5-point Likert scale (graduated from 1: no sensation, to 5: as intense as during actual performance) the intensity of the sensations perceived during the 12 min of MIP. In the Control condition, participants played a manual precision interactive game while receiving sham tDCS.
Apparatus
tDCS was delivered with a constant current stimulator (STARSTIM, Neuroelectrics) using two sponge electrodes impregnated with a saline-soaked solution. To increase cortical excitability of lower-limbs, the anode electrode was placed medially over the leg areas of both M1 63, which are located laterally to the vertex64,65. To cover both left and right hemispheres, the anode (25 cm², current density 0.04 mA/cm²) was placed at Cz66, with reference to the International 10/20 system. The cathode electrode (35 cm², current density 0.028 mA/cm²) was placed on the middle of the forehead. To avoid discomfort, current ramped up during 40 s until it reached 1 mA, and then ramped-down during 40 s after 12 min of stimulation. For blinding effect, the current was ramped up to 1 mA and down to 0 during the first and last 40 s of the sham conditions, but was nil during the remaining time. At the end of each session, participants were asked whether they received a real stimulation and could answer “Yes”, “No”, or “I don’t know”. We performed conformity Chi-squared test on the proportions of participants’ “Yes” and “No” answers for each session against proportions corresponding to the chance level (50%). Participants who responded “I don’t know” were not included in this analysis since they acknowledged not being able to discriminate sham from real stimulations. The conformity Chi-squared test were not statistically significant (all p > 0.05).
Data analysis
The time elapsed from target display to target validation (i.e., validation time) was the dependent variable quantifying motor performance. In addition to CONDITION (MItDCS, MIsham, and Control) and TEST (Pretest; Posttest), we included DIFFICULTY (Easy: easy targets; Hard: hard targets), LATERALITY (Dominant: front-right, right and back-right targets, Non-Dominant: front-left, left and back-left targets; Neutral: front and back targets), PLAN (Ahead: front-left, front and front-right targets; Behind: back-left, back and back-right targets; Neutral: left and right targets), and DIRECTION (Antero-posterior: front and back targets; Medio-lateral: left and right targets; Mixed: front-left, front-right, back-left and back-right targets) as independent variables (see Fig. 2A).
We used R67 and the packages lme4 68 and ARTool 69 to perform a nonparametric factorial analysis of motor performance data. Due to deviations from normality (Q-Q plots), we implemented a validated aligned rank transform (ART) procedure70. The ART procedure consists in a preliminary step of data alignment based on the mean estimates of main and interaction effects of a given factorial model, followed by rank assignment (for further details, see Wobbrock et al.70). We applied the ART to a mixed linear model with validation times as response variable. As fixed effects, we entered the independent variables (with interaction term). As random effect, we entered the by-subject random intercept. As post-hoc investigations, we used contrast tests with ART (least square means difference) and ran a systematic investigation of the three-way interactions involving CONDITION, TEST and one of the target location factor (i.e., DIFFICULTY, DIRECTION, LATERALITY and PLAN). The main effect of DIFFICULTY, DIRECTION, LATERALITY and PLAN was also investigated. The statistical significance threshold was set for a type 1 error rate of 5%. Holm's corrections for multiple comparisons were applied to control the false discovery rate71. Effect sizes were reported for each significant result. Small effect sizes were, however, expected due to the small sample size, the short duration of the experimental design (investigating immediate effects on performance at the session level), as well as the variable of interest (i.e., validation of the targets with limited magnitude of performance gains) and the three-way interactions.
Author Contributions
E.S., F.D.R., S.N.N., M.A.R.G., and A.G. participated to the development of the experimental design. E.S. conducted the experiment and collected the data. F.D.R. Performed statistical analyses. E.S., F.D.R., and A.G. wrote the manuscript. P.L.J., C.C., A.S. and A.G. reviewed the manuscript.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Winter DA. Human balance and posture control during standing and walking. Gait Posture. 1995;3:193–214. doi: 10.1016/0966-6362(96)82849-9. [DOI] [Google Scholar]
- 2.Weiss GN, Gorton T, Read RC, Neal LA. Outcomes of lower extremity amputations. J. Am. Geriatr. Soc. 1990;38:877–883. doi: 10.1111/j.1532-5415.1990.tb05703.x. [DOI] [PubMed] [Google Scholar]
- 3.Löfgren B, Nyberg L, Österlind PO, Gustafson Y. In-patient rehabilitation after stroke: outcome and factors associated with improvement. Disabil. Rehabil. 1998;20:55–61. doi: 10.3109/09638289809166054. [DOI] [PubMed] [Google Scholar]
- 4.Taube W, Lorch M, Zeiter S, Keller M. Non-physical practice improves task performance in an unstable, perturbed environment: motor imagery and observational balance training. Front. Hum. Neurosci. 2014;8:972. doi: 10.3389/fnhum.2014.00972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schuster C, et al. Best practice for motor imagery: a systematic literature review on motor imagery training elements in five different disciplines. BMC Med. 2011;9:1. doi: 10.1186/1741-7015-9-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dickstein R, Deutsch JE. Motor imagery in physical therapist practice. Phys. Ther. 2007;87:942–953. doi: 10.2522/ptj.20060331. [DOI] [PubMed] [Google Scholar]
- 7.Choi JH, et al. Effect of mental training on the balance control ability of healthy subjects. J. Phys. Ther. Sci. 2010;22:51–55. doi: 10.1589/jpts.22.51. [DOI] [Google Scholar]
- 8.Snijders AH, Leunissen I, et al. “Gait-related cerebral alterations in patients with Parkinson's disease with freezing of gait”. Brain. 2011;134:59–72. doi: 10.1093/brain/awq324. [DOI] [PubMed] [Google Scholar]
- 9.Fansler CL, Poff CL, Shepard KF. Effects of mental practice on balance in elderly women. Phys. Ther. 1985;65:1332–1338. doi: 10.1093/ptj/65.9.1332. [DOI] [PubMed] [Google Scholar]
- 10.Hamel MF, Lajoie Y. Mental imagery. Effects on static balance and attentional demands of the elderly. Aging Clin. Exp. Res. 2005;17:223–228. doi: 10.1007/BF03324601. [DOI] [PubMed] [Google Scholar]
- 11.Dickstein R, Dunsky A, Marcovitz E. Motor imagery for gait rehabilitation in post-stroke hemiparesis. Phys. Ther. 2004;84:1167–1177. [PubMed] [Google Scholar]
- 12.Hwang S, et al. Locomotor imagery training improves gait performance in people with chronic hemiparetic stroke: a controlled clinical trial. Clin. Rehabil. 2010;24:514–522. doi: 10.1177/0269215509360640. [DOI] [PubMed] [Google Scholar]
- 13.Kim J-S, Oh D-W, Kim S-Y, Choi J-D. Visual and kinesthetic locomotor imagery training integrated with auditory step rhythm for walking performance of patients with chronic stroke. Clin. Rehabil. 2011;25:134–145. doi: 10.1177/0269215510380822. [DOI] [PubMed] [Google Scholar]
- 14.Kim SS, Lee HJ, You YY. Effects of ankle strengthening exercises combined with motor imagery training on the timed up and go test score and weight bearing ratio in stroke patients. J. Phys. Ther. Sci. 2015;27:2303. doi: 10.1589/jpts.27.2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Di Rienzo F, Collet C, Hoyek N, Guillot A. Impact of neurologic deficits on motor imagery: A systematic review of clinical evaluations. Neuropsychol. Rev. 2014;24:116–147. doi: 10.1007/s11065-014-9257-6. [DOI] [PubMed] [Google Scholar]
- 16.Decety J, et al. Mapping motor representations with positron emission. Nature. 1994;371:13. doi: 10.1038/371600a0. [DOI] [PubMed] [Google Scholar]
- 17.Porro CA, et al. Primary motor and sensory cortex activation during motor performance and motor imagery: a functional magnetic resonance imaging study. J. Neurosci. 1996;16:7688–7698. doi: 10.1523/JNEUROSCI.16-23-07688.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lafleur MF, et al. Motor learning produces parallel dynamic functional changes during the execution and imagination of sequential foot movements. Neuroimage. 2002;16:142–157. doi: 10.1006/nimg.2001.1048. [DOI] [PubMed] [Google Scholar]
- 19.Munzert J, Lorey B, Zentgraf K. Cognitive motor processes: the role of motor imagery in the study of motor representations. Brain Res. Rev. 2009;60:306–326. doi: 10.1016/j.brainresrev.2008.12.024. [DOI] [PubMed] [Google Scholar]
- 20.Guillot A, et al. Functional neuroanatomical networks associated with expertise in motor imagery. Neuroimage. 2008;41:1471–1483. doi: 10.1016/j.neuroimage.2008.03.042. [DOI] [PubMed] [Google Scholar]
- 21.Di Rienzo F, et al. Online and offline performance gains following motor imagery: A comprehensive review of behavioral and neuroimaging studies. Front. Hum. Neurosc. 2016;10:1–15. doi: 10.3389/fnhum.2016.00315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kasai T, Kawai S, Kawanishi M, Yahagi S. Evidence for facilitation of motor evoked potentials (MEPs) induced by motor imagery. Brain Res. 1997;744:147–150. doi: 10.1016/S0006-8993(96)01101-8. [DOI] [PubMed] [Google Scholar]
- 23.Rossini PM, Rossi S, Pasqualetti P, Tecchio F. Corticospinal excitability modulation to hand muscles during movement imagery. Cereb. Cortex. 1999;9:161–167. doi: 10.1093/cercor/9.2.161. [DOI] [PubMed] [Google Scholar]
- 24.Facchini S, Muellbacher W, Battaglia F, Boroojerdi B, Hallett M. Focal enhancement of motor cortex excitability during motor imagery: a transcranial magnetic stimulation study. Acta Neurol. Scand. 2002;105:146–151. doi: 10.1034/j.1600-0404.2002.1o004.x. [DOI] [PubMed] [Google Scholar]
- 25.Nitsche MA, et al. Facilitation of implicit motor learning by weak transcranial direct current stimulation of the primary motor cortex in the human. J. Cogn. Neurosci. 2003;15:619–626. doi: 10.1162/089892903321662994. [DOI] [PubMed] [Google Scholar]
- 26.Reis J, Fritsch B. Modulation of motor performance and motor learning by transcranial direct current stimulation. Curr. Opin. Neurol. 2011;24:590–596. doi: 10.1097/WCO.0b013e32834c3db0. [DOI] [PubMed] [Google Scholar]
- 27.Reis J, et al. Consensus: can transcranial direct current stimulation and transcranial magnetic stimulation enhance motor learning and memory formation? Brain Stimulat. 2008;1:363–369. doi: 10.1016/j.brs.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 28.Matsumoto J, et al. Modulation of mu rhythm desynchronization during motor imagery by transcranial direct current stimulation. J. Neuroeng. Rehabil. 2010;7:1. doi: 10.1186/1743-0003-7-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Foerster A, et al. Site-specific effects of mental practice combined with transcranial direct current stimulation on motor learning. Eur. J. Neurosci. 2013;37:786–794. doi: 10.1111/ejn.12079. [DOI] [PubMed] [Google Scholar]
- 30.Saimpont A, et al. Anodal transcranial direct current stimulation enhances the effects of motor imagery training in a finger tapping task. Eur. J. Neurosci. 2016;43:113–119. doi: 10.1111/ejn.13122. [DOI] [PubMed] [Google Scholar]
- 31.Chugh S, Banerjee A, Dutta A. Effects of transcranial direct current stimulation on functional reach tasks. NeuroRehabilitation. 2013;34(4):789–798. doi: 10.3233/NRE-141077. [DOI] [PubMed] [Google Scholar]
- 32.Dutta, A. & Chugh, S. Effect of transcranial direct current stimulation on cortico-muscular coherence and standing postural steadiness. In the 2nd IASTED International Conference on Assistive Technologies (2012).
- 33.Yoo E, Chung B. The effect of visual feedback plus mental practice on symmetrical weight-bearing training in people with hemiparesis. Clin. Rehabil. 2006;20:388–397. doi: 10.1191/0269215506cr962oa. [DOI] [PubMed] [Google Scholar]
- 34.Hosseini SA, Fallahpour M, Sayadi M, Gharib M, Haghgoo H. The impact of mental practice on stroke patients’ postural balance. J. Neurol. Sci. 2012;322:263–267. doi: 10.1016/j.jns.2012.07.030. [DOI] [PubMed] [Google Scholar]
- 35.Lee H, Kim H, Ahn M, You Y. Effects of proprioception training with exercise imagery on balance ability of stroke patients. J. Phys. Ther. Sci. 2015;27:1–4. doi: 10.1589/jpts.27.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dunsky A, Dickstein R, Ariav C, Deutsch J, Marcovitz E. Motor imagery practice in gait rehabilitation of chronic post-stroke hemiparesis: four case studies. Int. J. Rehabil. Res. 2006;29:351–356. doi: 10.1097/MRR.0b013e328010f559. [DOI] [PubMed] [Google Scholar]
- 37.Bae YH, et al. An efficacy study on improving balance and gait in subacute stroke patients by balance training with additional motor imagery: a pilot study. J. Phys. Ther. Sci. 2015;27:3245. doi: 10.1589/jpts.27.3245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Malouin F, Richards CL, Doyon J, Desrosiers J, Belleville S. Training mobility tasks after stroke with combined mental and physical practice: a feasibility study. Neurorehabil. Neural Repair. 2004;18:66–75. doi: 10.1177/0888439004266304. [DOI] [PubMed] [Google Scholar]
- 39.Taube W, et al. Brain activity during observation and motor imagery of different balance tasks: An fMRI study. Cortex. 2015;64:102–114. doi: 10.1016/j.cortex.2014.09.022. [DOI] [PubMed] [Google Scholar]
- 40.Taubert M, et al. Dynamic properties of human brain structure: learning-related changes in cortical areas and associated fiber connections. J. Neurosci. 2010;30:11670–11677. doi: 10.1523/JNEUROSCI.2567-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Taubert M, Lohmann G, Margulies DS, Villringer A, Ragert P. Long-term effects of motor training on resting-state networks and underlying brain structure. Neuroimage. 2011;57:1492–1498. doi: 10.1016/j.neuroimage.2011.05.078. [DOI] [PubMed] [Google Scholar]
- 42.Solodkin A, Hlustik P, Chen EE, Small SL. Fine modulation in network activation during motor execution and motor imagery. Cereb. Cortex. 2004;14:1246–1255. doi: 10.1093/cercor/bhh086. [DOI] [PubMed] [Google Scholar]
- 43.Guillot A, et al. Brain activity during visual versus kinesthetic imagery: an fMRI study. Hum. Brain Map. 2009;30:2157–2172. doi: 10.1002/hbm.20658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nitsche MA, et al. Modulating parameters of excitability during and after transcranial direct current stimulation of the human motor cortex. J. Physiol. 2005;568:291–303. doi: 10.1113/jphysiol.2005.092429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nitsche MA, et al. Transcranial direct current stimulation: State of the art 2008. Brain Stimul. 2008;1:206–223. doi: 10.1016/j.brs.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 46.Antal A, Polania R, Schmidt-Samoa C, Dechent P, Paulus W. Transcranial direct current stimulation over the primary motor cortex during fMRI. Neuroimage. 2011;55:590–596. doi: 10.1016/j.neuroimage.2010.11.085. [DOI] [PubMed] [Google Scholar]
- 47.Kaminski E, et al. Effect of transcranial direct current stimulation (tDCS) during complex whole body motor skill learning. Neurosci. Lett. 2013;552:76–80. doi: 10.1016/j.neulet.2013.07.034. [DOI] [PubMed] [Google Scholar]
- 48.Vollman H, et al. Anodal transcranial direct current stimulation (tDCS) over supplementary motor area (SMA) but not pre-SMA promotes short-term visuomotor learning. Brain Stimul. 2013;6:101–107. doi: 10.1016/j.brs.2012.03.018. [DOI] [PubMed] [Google Scholar]
- 49.Carter MJ, Maslovat D, Carlsen AN. Anodal direct current stimulation applied over the supplementary motor area delays spontaneous antiphase-to-in-phase transitions. J. Neurophysiol. 2015;113:780–785. doi: 10.1152/jn.00662.2014. [DOI] [PubMed] [Google Scholar]
- 50.Carlsen AN, Eagles JS, MacKinnon CD. Transcranial direct current stimulation over the supplementary motor area modulates the preparatory activation level in the human motor system. Behav. Brain Res. 2015;279:68–75. doi: 10.1016/j.bbr.2014.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hupfeld, K.E., Ketcham, C. J., Schneider, H. D. Transcranial direct current stimulation (tDCS) to the supplementary motor area (SMA) influences performance on motor tasks. Exp. Brain Res. In press (2017). [DOI] [PubMed]
- 52.Karlsson A, Lanshammar H. Analysis of postural sway strategies using an inverted pendulum model and force plate data. Gait Posture. 1997;5:198–203. doi: 10.1016/S0966-6362(96)01082-X. [DOI] [Google Scholar]
- 53.Baydal-Bertomeu JM, et al. Determinación de los patrones de comportamiento postural en población sana española. [Determination of postural behavior patterns in Spanish healthy people] Acta Otorrinolaringol Esp. 2004;55:260–269. doi: 10.1016/S0001-6519(04)78520-9. [DOI] [PubMed] [Google Scholar]
- 54.Lang N, et al. How does transcranial DC stimulation of the primary motor cortex alter regional neuronal activity in the human brain? Eur. J. Neurosci. 2005;22:495–504. doi: 10.1111/j.1460-9568.2005.04233.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Reiser M, Büsch D, Munzert J. Strenght gains by motor imagery with different ratios of physical to mental practice. Front. Psychol. 2011;2:1–8. doi: 10.3389/fpsyg.2011.00194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Olfield RC. The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia. 1971;9:97–113. doi: 10.1016/0028-3932(71)90067-4. [DOI] [PubMed] [Google Scholar]
- 57.Malouin F, et al. The kinesthetic and visual imagery questionnaire (KVIQ) for assessing motor imagery in persons with physical disabilities: a reliability and construct validity study. JNPT. 2007;31:20–29. doi: 10.1097/01.npt.0000260567.24122.64. [DOI] [PubMed] [Google Scholar]
- 58.Clark RA, et al. Validity and reliability of the Nintendo Wii Balance Board for assessment of standing balance. Gait Posture. 2010;31:307–310. doi: 10.1016/j.gaitpost.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 59.Dutta A, Chugh S, Banerjee A, Dutta A. Point-of-care-testing of standing posture with Wii balance board and microsoft kinect during transcranial direct current stimulation: a feasibility study. NeuroRehabilitation. 2014;34:789–798. doi: 10.3233/NRE-141077. [DOI] [PubMed] [Google Scholar]
- 60.Holmes JD, Jenkins ME, Johnson AM, Hunt MA, Clark RA. Validity of the Nintendo Wii® balance board for the assessment of standing balance in Parkinson's disease. Clin. Rehabil. 2013;27:361–366. doi: 10.1177/0269215512458684. [DOI] [PubMed] [Google Scholar]
- 61.Jeter PE, et al. Intra-session test-retest reliability of magnitude and structure of center of pressure from the Nintendo Wii Balance BoardTM for a visually impaired and normally sighted population. Gait Posture. 2015;41:482–487. doi: 10.1016/j.gaitpost.2014.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Howells BE, et al. The assessment of postural control and the influence of a secondary task in people with anterior cruciate ligament reconstructed knees using a Nintendo Wii Balance Board. Br. J. Sports Med. 2012;47:914–919. doi: 10.1136/bjsports-2012-091525. [DOI] [PubMed] [Google Scholar]
- 63.Kaminski E, et al. Transcranial direct current stimulation (tDCS) over primary motor cortex leg area promotes dynamic balance task performance. Clin. Neurophysiol. 2016;127:2455–2462. doi: 10.1016/j.clinph.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 64.Madhavan S, Stinear JW. Focal and bidirectional modulation of lower limb motor cortex using anodal transcranial direct current stimulation. Brain Stimulat. 2010;3:42–50. doi: 10.1016/j.brs.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Madhavan S, Weber KA, II, Stinear JW. Non-invasive brain stimulation enhances fine motor control of the hemiparetic ankle: implications for rehabilitation. Exp. Brain Res. 2011;209:9–17. doi: 10.1007/s00221-010-2511-0. [DOI] [PubMed] [Google Scholar]
- 66.Lee YS, et al. The effects of transcranial direct current stimulation on functional movement performance and balance of the lower extremities. J. Phys. Ther. Sci. 2012;24:1215–1218. doi: 10.1589/jpts.24.1215. [DOI] [Google Scholar]
- 67.R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org (2015).
- 68.Bates D, Maechler M, Bolker B, Walker S. Fitting Linear Mixed-Effects Models Using lme4. J. Stat. Sotw. 2015;67(1):1–48. [Google Scholar]
- 69.Kay, M. & Wobbrock, J. ARTool: Aligned Rank Transform for Nonparametric Factorial ANOVAs. R package version 0.10.2. https://github.com/mjskay/ARTool (2016).
- 70.Wobbrock, J., Findlater, L., Gergle, D. & Higgins, J. The Aligned Rank Transform for Nonparametric Factorial Analyses Using Only ANOVA Procedures. In Proceedings of the ACM Conference on Human Factors in Computing Systems. http://depts.washington.edu/aimgroup/proj/art/ (2011).
- 71.Holm S. A simple sequentially rejective multiple test procedure. Scand. J. Stat. 1979;6:65–67. [Google Scholar]


