Abstract
Objective
Little smoking research in the past 20 years includes persons 50 and older; herein we describe patterns of clinician cessation advice to US seniors, including variation by Medicare beneficiary characteristics.
Method
In 2012–4, we analyzed 2010 Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey data from Medicare beneficiaries over age 64 (n = 346,674). We estimated smoking rates and the proportion of smokers whose clinicians encouraged cessation.
Results
12% of male and 8% of female respondents aged 65 and older smoke. The rate decreases with age (14% of 65–69, 3% of 85+) and education (12–15% with no high school degree, 5–6% with BA+). Rates are highest among American Indian/Alaskan Native (16%), multiracial (14%), and African–American (13%) seniors, and in the Southeast (14%). Only 51% of smokers say they receive cessation advice “always” or “usually” at doctor visits, with advice more often given to the young, those in low-smoking regions, Asians, and women. For all results cited p < 0.05.
Conclusions
Smoking cessation advice to seniors is variable. Providers may focus on groups or areas in which smoking is less common or when they are most comfortable giving advice. More consistent interventions are needed, including cessation advice from clinicians.
Keywords: Physician/patient communication, Medicare, Patient education, Smoking cessation
Introduction
Quitting smoking at any age reduces morbidity and mortality associated with smoking (Allen, 2009; National Cancer Institute, 1997; Taylor et al., 2002). Seniors’ smoking contributes substantially to mortality and morbidity (e.g., dementia and macular degeneration) and aggravates existing chronic conditions (Burns, 2000; Cong et al., 2008; Ni Dhubhghaill et al., 2010; Reitz et al., 2007; Rusanen et al., 2011). Cessation for older smokers is associated with greatly reduced risk of myocardial infarction and cerebrovascular accidents, and has other short-term benefits (e.g., improved lung function, decreased incidence of pneumonia) as well as longer-term benefits (e.g., lower risk of oral and respiratory system cancers). An important public health goal, then, is to assist older smokers with quitting.
While some have found that smokers over 50 are as motivated to quit as younger smokers (Hall et al., 2008), others have found that smokers over 65 are slightly less motivated to quit (Centers for Disease Control and Prevention, 2011). In addition, some older smokers may be less able to proactively seek smoking cessation treatment or may resist quitting because they think that it is “too late” for them to quit (Glasgow et al., 2001), so outreach to older smokers to improve their access to effective smoking cessation treatments is important. Given seniors’ high healthcare utilization (Schiller et al., 2012), physician office visits present a significant opportunity to provide cessation advice to older smokers. Brief cessation interventions by physicians or other health care providers can effectively help older smokers quit (Morgan et al., 1996; Vetter and Ford, 1990). However, most providers do not offer smoking cessation treatments (Centers for Disease Control and Prevention, 2007), especially for older smokers (Allen, 2009) and those suffering from a smoking-related disease like lung cancer (Wassenaar et al., 2007). Barriers to physician adherence to clinical practice guidelines include lack of awareness and familiarity with guidelines, poor self-efficacy, belief that recommendation will not lead to desired outcome, little office support, limited counseling skills, and inability to overcome the inertia of previous practice; patient barriers include lack of motivation or interest in quitting (Cabana et al., 1999; McIlvain et al., 2002; Weaver et al., 2012). Research with providers serving low-income and minority patients identified five barriers: insufficient time, patient unreadiness to change, inadequate patient resources, inadequate provider resources and inadequate cessation physician training/clinical skills (Balls et al., 2010; Blumenthal, 2007).
More research on the national prevalence of provider cessation advice is needed. Past research has used convenience samples of smokers already enrolled in smoking cessation trials (Ossip-Klein et al., 2000), or has focused on older smokers with concurrent medical conditions or hospitalizations (Brown et al., 2004; Houston et al., 2005) or clinical trials testing smoking cessation interventions outside of physician offices (Hall et al., 2009).
In this study we examine the prevalence of smoking and predictors of clinician smoking cessation advice in a nationally representative sample of US adults age 65 and older. Because individual differences in demographic variables such as gender, age, and race/ethnicity can predict differences in treatment availability, accessibility, and efficacy, (Jarvis et al., 2013; Trinidad et al., 2011) we examine these variables as moderators.
Methods
These analyses focus on a nationally representative sample of Medicare beneficiaries age 65 and older living in the 50 states and Washington, DC. We describe patterns of current smoking and assess whether smokers were advised to quit during medical visits. We used data from the 2010 Medicare Consumer Assessments of Healthcare Providers and Systems (MCAHPS) survey (overall response rate 60%), sponsored by the Centers for Medicare & Medicaid Services (CMS). The smoking question was, ‘Do you now smoke cigarettes or use tobacco every day, some days, or not at all?’ Those replying ‘Every day’ or ‘Some days’ were classified as “current smokers,” then asked, ‘In the last 6 months, how often were you advised to quit smoking or using tobacco by a doctor or other health provider?’, with response options ‘Never’ (1), ‘Sometimes’ (2), ‘Usually (3)’, ‘Always’ (4), and ‘I had no visits in the last 6 months’.
We use “smoker” in this paper to indicate tobacco user more broadly (including those smoking cigarettes or using smokeless tobacco, cigars, etc.). Among smokers, responses regarding cessation advice were linearly rescaled to a 0–100 possible range. Smokers with no medical visits in the past 6 months were excluded from the cessation advice analyses.
We estimated the prevalence of smoking by beneficiary characteristics (gender, age, education, race/ethnicity, census division, dually eligible for Medicare/Medicaid, survey proxy status, and having a personal physician). Among current smokers with a recent medical visit, we estimated the mean of the cessation advice item by the beneficiary characteristics listed above, as well as by confidence in the ability to identify need for medical care, health characteristics (self-reported general and mental health, history of six specific chronic conditions) and smoking intensity (daily versus less often than daily). We estimated the association between the cessation advice scale and each predictor using simple linear regression and used multivariate regression to assess all simultaneously, including interactions of gender with age and race/ethnicity in a second multivariate model. To illustrate the relationship between smoking status and cessation advice, we plotted the mean of the advised-to-quit index against the percentage of current smokers (a) by census division, and (b) for men and women of different racial/ethnic groups. A sensitivity analysis included interactions of beneficiary characteristics with the daily smoking indicator to test whether predictors of cessation advice differed for those who smoked daily versus less frequently.
All analyses were weighted to represent the Medicare population age 65 and older within each county and plan using loglinear poststratification weights estimated by iterative proportional fitting (Deming and Stephan, 1940; Purcell and Kish, 1980) to match weighted plan-level distributions of gender, age, race/ethnicity, Medicaid, low income supplement status, Special Needs Plan status, Part D enrollment, and zip-code level distributions of income, education, and race/ethnicity. Analyses were completed in 2014.
Results
Data from 346,674 senior Medicare beneficiaries are used for the analyses, of whom 9.6% are current smokers (and 6.3% daily smokers). The plan-level intraclass correlation (ICC) coefficient for the cessation advice item is 0.12, which is considered evidence of high reliability (Lyratzopoulos et al., 2011).
Patterns of smoking prevalence
Table 1 presents smoking rates by beneficiary and coverage characteristics. Men are more likely to smoke (12.3%) than women (7.7%). Smoking decreases with age (from 14.4% among 65–69 year olds to 3.4% in those 85+) and educational attainment (12.0%–14.6% of those not completing high school; 5.1%–6.3% of those with a four-year college degree). Rates are highest among American Indians (15.9%), multiracial (14.3%) and African–American (13.3%) seniors, intermediate for non-Hispanic White (9.5%) seniors, and lowest for Asian/Pacific Islander (API, 5.1%) and Hispanic (7.8%) seniors. Rates are highest in the East South Central census division (13.5%) and lowest in New England and the Pacific (7.6–7.7%). Low-income seniors eligible for Medicaid smoke more often (15.1% versus 8.9%). The small proportion of seniors without a personal physician had a higher smoking rate (17.4%) than those with a personal physician (9.2%). Tests of association between current smoking status and each characteristic mentioned in this paragraph were statistically significant (p < 0.001).
Table 1.
Beneficiary and coverage characteristics and differences in smoking prevalence by these characteristicsa.
| Variable | % of total sample in this group | % in this group who smoke at all |
|---|---|---|
| Gender | ||
| Male [Reference] | 42.8 | 12.3 |
| Female | 57.2 | 7.7*** |
| Age category | ||
| 65–69 [Reference] | 28.5 | 14.4 |
| 70–74 | 24.4 | 11.1*** |
| 75–79 | 19.1 | 8.2*** |
| 80–84 | 14.7 | 5.6*** |
| ≥85 | 13.3 | 3.4*** |
| Education | ||
| 8th grade or less | 9.2 | 12.0*** |
| Some high school | 11.0 | 14.6*** |
| High school degree [Reference] | 33.5 | 10.4 |
| Some college/2-yr degree | 23.8 | 9.4*** |
| 4-yr college degree | 9.5 | 6.3*** |
| More than 4-yr college degree | 13.0 | 5.1*** |
| Race/ethnicity | ||
| Non-Hispanic White [Reference] | 80.6 | 9.5 |
| Hispanic | 6.3 | 7.8*** |
| African–American | 7.7 | 13.3*** |
| API | 3.3 | 5.1*** |
| AI/AN | 0.4 | 15.9*** |
| Multiracial | 1.7 | 14.3*** |
| Census divisionb | ||
| New England [Reference] | 5.1 | 7.6 |
| Middle Atlantic | 14.5 | 8.6** |
| East North Central | 15.6 | 9.7*** |
| West North Central | 7.2 | 9.5*** |
| South Atlantic | 19.9 | 10.3*** |
| East South Central | 6.4 | 13.5*** |
| West South Central | 10.3 | 11.3*** |
| Mountain | 6.4 | 9.8*** |
| Pacific | 14.6 | 7.7 |
| Dually eligible for Medicaid | ||
| Yes | 12.5 | 15.1*** |
| No [Reference] | 87.5 | 8.9 |
| Any proxy assistance on survey | ||
| Yes | 12.3 | 9.0** |
| No [Reference] | 87.7 | 9.7 |
| Completion of survey by proxy | ||
| Yes | 4.1 | 7.5*** |
| No [Reference] | 95.9 | 9.7 |
| Has a personal physician | ||
| Yes | 94.4 | 9.2*** |
| No [Reference] | 5.6 | 17.4 |
API: Asian/Pacific Islander.
AI/AN: American Indian/Alaska Native.
p < 0.05;
p < 0.01;
p < 0.001.
2010 MCAHPS data, age 65 and older, in the 50 states or D.C. (N = 346,674).
Census divisions are created from state of beneficiary residence as follows: New England: CT, MA, ME, NH, RI, VT; Middle Atlantic: NJ, NY, PA; East North Central: IL, IN, MI, OH, WI; West North Central: IA, KS, MN, MO, ND, NE, SD; South Atlantic: DC, DE, FL, GA, MD, NC, SC, VA, WV; East South Central: AL, KY, MS, TN; West South Central: AR, LA, OK, TX; Mountain: AZ, CO, ID, MT, NM, NV, UT, WY; Pacific: AK, CA, HI, OR, WA.
Cessation advice among smokers
Of current smokers, 33% were given cessation advice “always” at medical visits, 18% usually, 23% sometimes, and 26% never, resulting in an overall mean of 52.3 on the 0–100 cessation advice scale. Eight percent of smokers had no medical visits in the past 6 months.
Table 2 presents unadjusted means of the 0–100 advised-to-quit scale by socio-demographic, coverage and health characteristics. Women (+4.3 vs. men, p < 0.001), younger seniors (+15.5 age 65–69 vs. age 85 and older, p < 0.001), API (+9.2 vs. non-Hispanic White, p < 0.01), those living in New England and the Middle Atlantic (+15.1 and +11.4 vs. the East South Central division, respectively, both p < 0.001), and individuals with a personal physician (+21.0 vs. those without a personal physician, p < 0.001) received more cessation advice. Smokers in worse health were advised to quit more often across several measures of health (p < 0.001 for each), including self-rated general health (+21.4 for poor vs. excellent health) and history of chronic conditions: COPD (+19.9), angina (+10.6), heart attack (+10.1), stroke (+6.9), diabetes (+6.8), and cancer (+3.4). Daily smokers received more cessation advice than less frequent smokers (+8.2, p < 0.001).
Table 2.
Means and regression coefficients for advised-to-quit smoking scale (0–100)a by demographic, coverage, and health characteristicsb,c.
| % of all smokers in this group (N = 32,772) | Mean of 0–100 advised-to-quit item (N = 28,783) | Model 1: Multivariate linear regression of advised-to-quit scale | Model 2: Model 1 plus interactions of gender by age and gender by race/ethnicity | |
|---|---|---|---|---|
| Gender | ||||
| Male [Reference] | 54.6 | 50.9 | [Reference] | [Reference] |
| Female | 45.4 | 55.2*** | 3.9 (2.5, 5.3)*** | 3.0 (1.1, 5.0)** |
| Age category | ||||
| 65–69 [Reference] | 42.6 | 55.1 | [Reference] | [Reference] |
| 70–74 | 28.1 | 53.6 | −1.9 (−3.5, −0.4)* | −2.5 (−4.2, −0.8)** |
| 75–79 | 16.2 | 52.2** | −2.8 (−4.7, −0.9)** | −4.0 (−6.2, −1.8)*** |
| 80–84 | 8.5 | 48.6*** | −7.1 (−9.6, −4.7)*** | −9.1 (−12.1, −6.1)*** |
| ≥85 | 4.6 | 39.6*** | −15.9 (−19.2, −12.6)*** | −18.8(−22.9,−14.6)*** |
| Education | ||||
| 8th grade or less | 11.2 | 50.9 | −3.0 (−5.5, −0.5)* | −3.0 (−5.5, −0.5)* |
| Some high school | 16.4 | 54.1 | −0.6 (−2.6, 1.4) | −0.6 (−2.6, 1.4) |
| High school degree [Reference] | 35.9 | 53.2 | [Reference] | [Reference] |
| Some college/2-yr degree | 23.3 | 54.0 | 1.7 (−0.1, 3.4) | 1.7 (−0.1, 3.5) |
| 4-yr college degree | 6.2 | 50.5 | 0.1 (−2.8, 3.0) | 0.2 (−2.7, 3.1) |
| More than 4-yr college degree | 6.9 | 50.5 | 0.7 (−2.1, 3.6) | 0.8 (−2.0, 3.7) |
| Race/ethnicity | ||||
| Non-Hispanic White [Reference] | 79.5 | 52.2 | [Reference] | [Reference] |
| Hispanic | 5.1 | 54.7 | 6.7 (3.4, 10.0)*** | 8.6 (4.3, 12.9)*** |
| African–American | 10.4 | 55.5* | 7.5 (5.0, 10.1)*** | 8.1 (4.4, 11.8)*** |
| API | 1.7 | 61.4** | 14.3 (8.2, 20.4)*** | 13.0 (5.4, 20.7)*** |
| AI/AN | 0.7 | 54.6 | 7.4 (−0.3, 15.1) | 6.6 (−4.3, 17.5) |
| Multiracial | 2.6 | 55.4 | 1.3 (−3.0, 5.6) | 4.2 (−1.6, 10.1) |
| Census divisiond | ||||
| New England [Reference] | 4.0 | 61.9 | [Reference] | [Reference] |
| Middle Atlantic | 12.9 | 58.2 | −3.9 (−7.4, −0.3)* | −3.8 (−7.3, −0.2 |
| East North Central | 15.6 | 53.5*** | −9.6 (−13.1, −6.1)*** | −9.6 (−13.1, −6.0)*** |
| West North Central | 7.1 | 49.8*** | −13.1 (−16.9, −9.2)*** | −13.0(−16.9, −9.2)*** |
| South Atlantic | 21.3 | 52.6*** | −10.5 (−14, −7.1)*** | −10.5 (−13.9, −7.1)*** |
| East South Central | 8.9 | 46.8*** | −17.7 (−21.5, −14.0)*** | −17.7(−21.5,−13.9)*** |
| West South Central | 12.0 | 49.5*** | −14.2 (−17.9, −10.5)*** | −14.1(−17.8,−10.4)*** |
| Mountain | 6.6 | 51.3*** | −11.4 (−15.3, −7.6)*** | −11.4 (−15.3,−7.6)*** |
| Pacific | 11.6 | 54.8*** | −8.2 (−11.9, −4.5)*** | −8.2 (−11.9,−4.5)*** |
| Dually eligible for Medicaid | ||||
| Yes | 18.8 | 55.9*** | 0.1 (−1.8, 2.0) | 0.1 (−1.8, 2.0) |
| No [Reference] | 81.2 | 52.2 | [Reference] | [Reference] |
| Any proxy assistance on survey | ||||
| Yes | 11.5 | 54.1 | 1.3 (−1.3, 3.9) | 1.3 (−1.4, 3.9) |
| No [Reference] | 88.5 | 52.8 | [Reference] | [Reference] |
| Completion of survey by proxy | ||||
| Yes | 3.2 | 49.3 | −5.7 (−9.9, −1.4)** | −5.8 (−10.0, −1.6)** |
| No [Reference] | 96.8 | 53.0 | [Reference] | [Reference] |
| Has a personal physician | ||||
| Yes | 90.0 | 54.6*** | 18.1 (15.5, 20.8)*** | 18.2 (15.5, 20.9)*** |
| No [Reference] | 10.0 | 33.6 | [Reference] | [Reference] |
| How confident are you that you can identify your need for medical care?e | ||||
| Not at all confident | 1.5 | 47.2 | 0.7 (−0.3, 1.7) | 0.7 (−0.3, 1.7) |
| Somewhat confident | 8.3 | 54.3 | ||
| Confident | 36.4 | 52.8 | ||
| Very confident | 53.7 | 53.1 | ||
| Self-reported general health | ||||
| Excellent | 6.5 | 39.7*** | −9.8 (−13.0, −6.6)*** | −9.8 (−13.0, −6.5)*** |
| Very good | 23.2 | 46.8*** | −4.0 (−5.9, −2.2)*** | −4.1 (−5.9, −2.2)*** |
| Good [Reference] | 37.0 | 52.6 | [Reference] | [Reference] |
| Fair | 25.6 | 58.9*** | 3.2 (1.4, 4.9)*** | 3.2 (1.4, 4.9)*** |
| Poor | 7.6 | 61.1*** | 3.1 (0.4, 5.9)* | 3.2 (0.5, 6.0)* |
| Self-reported mental health | ||||
| Excellent | 28.9 | 51.1* | 2.1 (0.1, 4.0)* | 2.0 (0.1, 4.0)* |
| Very good | 31.8 | 52.6 | 1.0 (−0.8, 2.7) | 0.9 (−0.8, 2.6) |
| Good [Reference] | 27.1 | 53.3 | [Reference] | [Reference] |
| Fair | 10.3 | 57.0** | 1.0 (−1.5, 3.4) | 1.0 (−1.5, 3.4) |
| Poor | 1.9 | 56.5 | −1.2 (−6.6, 4.2 | −1.2 (−6.6, 4.2) |
| History of heart attack | ||||
| Yes | 17.3 | 61.4*** | 5.3 (3.4, 7.3)*** | 5.4 (3.4, 7.3)*** |
| No [Reference] | 82.7 | 51.3 | [Reference] | [Reference] |
| History of angina | ||||
| Yes | 18.7 | 61.7*** | 5.0 (3.1, 6.8)*** | 5.0 (3.1, 6.8)*** |
| No [Reference] | 81.3 | 51.1 | [Reference] | [Reference] |
| History of stroke | ||||
| Yes | 11.4 | 59.1*** | 2.8 (0.7, 5.0)** | 2.8 (0.7, 5.0)** |
| No [Reference] | 88.6 | 52.2 | [Reference] | [Reference] |
| History of cancer | ||||
| Yes | 17.0 | 55.8*** | 2.3 (0.5, 4.1)* | 2.3 (0.6, 4.1)* |
| No [Reference] | 83.0 | 52.4 | [Reference] | [Reference] |
| History of COPD | ||||
| Yes | 28.2 | 67.6*** | 16.3 (14.8, 17.7)*** | 16.3 (14.8, 17.7)*** |
| No [Reference] | 71.8 | 47.7 | [Reference] | [Reference] |
| History of diabetes | ||||
| Yes | 28.3 | 57.8*** | 3.7 (2.2, 5.1)*** | 3.7 (2.2, 5.2)*** |
| No [Reference] | 71.7 | 51.1 | [Reference] | [Reference] |
| Smoking intensity | ||||
| Every day [Reference] | 65.5 | 55.8 | [Reference] | [Reference] |
| Some days | 34.5 | 47.5*** | −8.7 (−10.1, −7.3)*** | −8.7 (−10.0, −7.3)*** |
| Gender × linear agef | ||||
| Female × age | 1.3 (0.1, 2.5)* | |||
| Gender × race/ethnicityg | ||||
| Hispanic × female | −4.7 (−11, 1.7) | |||
| African–American × female | −1.3 (−6.2, 3.6) | |||
| API × female | 4.5 (−7.7, 16.7) | |||
| AI/AN × female | 2.3 (−12.3, 16.8) | |||
| Multiracial × female | −6.6 (−15.2, 2.0) | |||
p < 0.05
p < 0.01
p < 0.001.
API: Asian/Pacific Islander.
AI/AN: American Indian/Alaska Native.
COPD: Chronic obstructive pulmonary disease.
Linear rescaled from 4 answer options to the item ‘In the last 6 months, how often were you advised to quit smoking or using tobacco by a doctor or other health provider? (0 = Never; 33 = Sometimes; 67 = Usually; 100 = Always).
In 2010 MCAHPS data, age 65 and older, in the 50 states or D.C., current smokers with at least one visit in the past 6 months.
Models 1 and 2 also adjust for type of Medicare coverage (Fee-For-Service, in a Medicare Advantage Special Needs Plan, or in any other type of Medicare Advantage plan), results not shown.
Census divisions are created from state of beneficiary residence as follows: New England: CT, MA, ME, NH, RI, VT; Middle Atlantic: NJ, NY, PA; East North Central: IL, IN, MI, OH, WI; West North Central: IA, KS, MN, MO, ND, NE, SD; South Atlantic: DC, DE, FL, GA, MD, NC, SC, VA, WV; East South Central: AL, KY, MS, TN; West South Central: AR, LA, OK, TX; Mountain: AZ, CO, ID, MT, NM, NV, UT, WY; Pacific: AK, CA, HI, OR, WA.
Linear version used in modeling. Coded 1 to 4; higher indicates more confident. P-value = 0.68.
Linear age used in interactions, coded as: 0 = 65–69 years; 1 = 70–74; 2 = 75–79; 3 = 80–84; 4 = 85+.
Joint test of gender × race/ethnicity interaction has p-value = 0.41 (df = 5).
Table 2 also presents results from simple and multivariate linear regressions of the advised-to-quit item. After adjusting for all other beneficiary and coverage characteristics, differences associated with gender, age, region, having a personal physician, and smoking frequency remain significant and are similar in size to the differences in the unadjusted means. Adjusted differences by race/ethnicity remain statistically significant: +14.3 API, +7.5 African American, and +6.7 Hispanic compared to non-Hispanic Whites. Self-reported general health also remained statistically significant (+12.9 for poor vs. excellent health). The associations with history of chronic conditions were attenuated but remained statistically significant: COPD (+16.3), heart attack (+5.3), angina (+5.0), diabetes (+3.7), stroke (+2.8), and cancer (+2.3). All noted differences were significant at p < .05.
The female by age interaction (Table 2, column 5) is positive and statistically significant (p = 0.027), indicating that the decrease in cessation advice with age is greater for men than women. The gender by race/ethnicity interaction is not statistically significant.
Fig. 1 illustrates the relationship between the mean advice-to-quit index and smoking rate (a) in each census division and (b) for men and women of four racial/ethnic groups. The figure also includes the two associated regression lines. Generally, in census divisions with higher smoking rates, smokers are advised to quit less often (r = −0.83). A similar pattern emerges for gender by racial/ethnic groups (r = −0.62). For example, API women and New England residents have among the lowest smoking prevalence but those who do smoke in those groups receive especially frequent cessation advice.
Fig. 1.
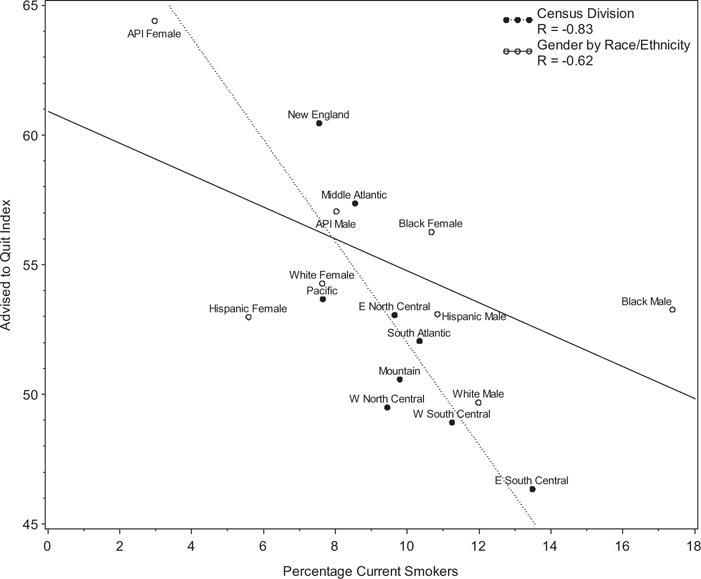
Scatterplot of mean advised-to-quit index (0–100) and percentage who smoke for each census division and gender by race/ethnicity combination.
Additional models included interactions between daily smoking and the other predictors (p < 0.001 overall, results not shown). In particular, there were significant positive interactions (p < 0.001) between daily smoking and (a) male gender, (b) better health status, and (c) having a personal physician. While women are more likely to receive cessation advice, models stratified by smoking frequency suggest that pattern is limited to occasional smokers. Similarly, the tendency for more cessation advice for those in worse health is strongest among less frequent smokers. Beneficiaries without a regular physician are much less likely to receive cessation advice; the gap is especially large for daily smokers.
Discussion
In this study, 9.6% of Medicare beneficiaries age 65 and older reported smoking currently, including 6.3% who reported smoking daily. These rates are lower than other studies have reported for older adults (Schiller et al., 2012), possibly because of differences in smoking questions. Rates were higher among men, younger and low-income Medicaid-eligible seniors, those without a personal physician, and those with less than a high school degree. While these patterns generally mirror those in younger adults, the gender difference is more pronounced than for younger adults (Schiller et al., 2012).
Only 50% of smokers reported that they “usually” or “always” received smoking cessation advice from their clinicians. Cessation advice is more frequent for daily smokers (perhaps because of greater perceived risk, or because they are more likely to identify themselves as smokers to providers (Berg et al., 2009) and for younger seniors (perhaps because of greater potential for long-term harm). These findings replicate other studies (Doolan and Froelicher, 2008; Wassenaar et al., 2007). Other findings suggest that cessation advice may be more often given to “atypical” smokers—smokers in regions or sociodemographic groups with low smoking rates. This pattern might indicate that providers are less comfortable challenging smoking they perceive as normative (He et al., 2010). Alternatively, these negative correlations may simply reflect the greater incidence and effectiveness of cessation advice in certain regions.
Given evidence of the efficacy of smoking cessation advice to seniors (Rimer and Orleans, 1994) and their access to providers through Medicare, these results suggest the need for more targeted smoking interventions including provider cessation advice (Richmond and Anderson, 1994), which is not always emphasized in current physician training (Zwar and Richmond, 2006). Smokers with lower levels of education (8th grade or less) reported receiving less advice from physicians to quit, consistent with other studies finding less access to cessation treatment for such seniors (Shiffman et al., 2008). In addition, smoking rates are highest (Centers for Disease Control and Prevention, 2009) and cessation rates are lowest (Barbeau et al., 2004; Centers for Disease Control and Prevention, 2009; Kanjilal et al., 2006; Shiffman et al., 2008; Wetter et al., 2005) among those with less education, who are at greater risk of developing smoking-related disease (Kanjilal et al., 2006).
Existing brief treatments and pharmacotherapies can be effective in low-education populations (Fiore et al., 2008). Clinicians should be trained and encouraged to deliver combined brief counseling and pharmacological interventions to all of their patients, particularly those with less education. In addition, clinicians should be informed about the best ways to elicit smoking information, especially from light smokers (Berg et al., 2009). Clinicians should be reminded that the population-level effects of brief, consistent cessation advice can be substantial (Abrams et al., 1996), even if effects are not immediately visible for many patients. Incorporating non-physician members of the primary-care team to deliver cessation advice might help overcome the barrier of limited physician time with patients (Fiore et al., 2008).
Limitations
This study has several limitations. First, measures were self-reported and could be subject to recall biases (Hammersley, 1994). Recordings of encounters revealed high specificity but lower sensitivity in patient reports of receiving cessation advice (Ward and Sanson-Fisher, 1996), suggesting that only advice clear enough to be perceived by patients was reported. Advice both given and perceived, however, may be the relevant construct, since there is evidence that only physician communication that patients perceive and recall has effects (Beckett et al., 2009). Second, cessation advice may vary by chronic conditions known to the physician, including terminal illnesses, not measured on the MCAHPS survey. Third, the optimal frequency of cessation advice is unknown, so the 0–100 scale used as the primary outcome might not be optimal. Nevertheless, sensitivity tests using a binary never-advised-to-quit indicator resulted in similar findings (data not shown). Fourth, the cessation advice item only asks about the consistency of advice in the preceding six months, but does not indicate the frequency of patient counseling for patients with different visit frequencies. Finally, some have speculated that smokers might be less likely to respond to a survey specifically about smoking than non-smokers (Davis, 1998), but such concerns are unlikely to apply to Medicare CAHPS, a survey of general healthcare experiences. In addition, we adjusted for the modest differences between responders and non-responders on observed characteristics using nonresponse weighting.
Conclusions
This research provides important information about smoking prevalence and cessation advice among adults age 65 and older. Inconsistent cessation advice from clinicians indicates a need to emphasize smoking cessation for seniors in clinician training and more intervention with older smokers.
Acknowledgments
We thank Fergal McCarthy, MPhil for assistance with the preparation of the manuscript.
No financial disclosures were reported by the authors of this paper. Authors are employed by their designated institutions and have received no further financial support from any organization that might have an interest in the submitted work.
Footnotes
This study was funded by CMS contract HHSM-500-2005-00028I to RAND.
Conflict of interest statement
The authors declare that there are no conflicts of interest.
References
- Abrams DB, Orleans CT, Niaura RS, Goldstein MG, Prochaska JO, Velicer W. Integrating individual and public health perspectives for treatment of tobacco dependence under managed health care: a combined stepped-care and matching model. Ann Behav Med. 1996;18:290–304. doi: 10.1007/BF02895291. [DOI] [PubMed] [Google Scholar]
- Allen S. Tobacco smoking in older people. Rev Clin Gerontol. 2009;19:185–192. [Google Scholar]
- Balls JE, Price JH, Dake JA, Jordan TR, Khuder S. African American primary care physicians’ perceptions and practices regarding smoking cessation therapy. J Natl Med Assoc. 2010;102:579–589. doi: 10.1016/s0027-9684(15)30635-0. [DOI] [PubMed] [Google Scholar]
- Barbeau EM, Krieger N, Soobader MJ. Working class matters: socioeconomic disadvantage, race/ethnicity, gender, and smoking in NHIS 2000. Am J Public Health. 2004;94:269–278. doi: 10.2105/ajph.94.2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckett MK, Elliott MN, Richardson A, Mangione-Smith R. Outpatient satisfaction: the role of nominal versus perceived communication. Health Serv Res. 2009;44:1735–1749. doi: 10.1111/j.1475-6773.2009.01001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg CJ, Lust KA, Sanem JR, Kirch MA, Rudie M, Ehlinger E, Ahluwalia JS, An LC. Smoker self-identification versus recent Smoking among college students. Am J Prev Med. 2009;36(4):333–336. doi: 10.1016/j.amepre.2008.11.010. [DOI] [PubMed] [Google Scholar]
- Blumenthal DS. Barriers to the provision of smoking cessation services reported by clinicians in underserved communities. J Am Board Fam Med. 2007;20:272–279. doi: 10.3122/jabfm.2007.03.060115. [DOI] [PubMed] [Google Scholar]
- Brown DW, Croft JB, Schenck AP, Malarcher AM, Giles WH, Simpson RJ., Jr Inpatient smoking-cessation counseling and all-cause mortality among the elderly. Am J Prev Med. 2004;26:112–118. doi: 10.1016/j.amepre.2003.10.004. [DOI] [PubMed] [Google Scholar]
- Burns DM. Cigarette smoking among the elderly: disease consequences and the benefits of cessation. Am J Health Promot. 2000;14:357–361. doi: 10.4278/0890-1171-14.6.357. [DOI] [PubMed] [Google Scholar]
- Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–1465. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Smoking-Cessation Advice from Health-Care Providers—Canada, 2005, Morbidity and Mortality Weekly Report. Centers for Disease Control and Prevention; Atlanta, GA: 2007. pp. 708–712. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Cigarette smoking among adults and trends in smoking cessation—United States, 2008. MMWR. 2009;58:1227–1232. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Quitting Smoking Among Adults—United States 2001–2010, Morbidity and Mortality Weekly Report (MMWR) Centers for Disease Control and Prevention; 2011. pp. 1513–1519. [Google Scholar]
- Cong R, Zhou B, Sun Q, Gu H, Tang N, Wang B. Smoking and the risk of age-related macular degeneration: a meta-analysis. Ann Epidemiol. 2008;18:647–656. doi: 10.1016/j.annepidem.2008.04.002. [DOI] [PubMed] [Google Scholar]
- Davis RM. An overview of tobacco measures. Tob Control. 1998;7(Suppl):S36–40. doi: 10.1136/tc.7.2008.s36. discussion S47–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deming WE, Stephan FF. On a least squares adjustment of a sampled frequency table when the expected marginal totals are known. Ann Math Stat. 1940:427–444. [Google Scholar]
- Doolan DM, Froelicher ES. Smoking cessation interventions and older adults. Prog Cardiovasc Nurs. 2008;23:119–127. doi: 10.1111/j.1751-7117.2008.00001.x. [DOI] [PubMed] [Google Scholar]
- Fiore MC, Jaen CR, Baker TB, et al. Treating Tobacco Use and Dependence: 2008 Update. U.S. Department of Health and Human Services, U.S. Public Health Service; Rockville, MD: 2008. [Google Scholar]
- Glasgow RE, McKay HG, Piette JD, Reynolds KD. The RE-AIM framework for evaluating interventions: what can it tell us about approaches to chronic illness management? Patient Educ Couns. 2001;44:119–127. doi: 10.1016/s0738-3991(00)00186-5. [DOI] [PubMed] [Google Scholar]
- Hall SM, Humfleet GL, Gorecki JA, Muñoz RF, Reus VI, Reus JJ. Older versus younger treatment-seeking smokers: differences in smoking behavior, drug and alcohol use, and psychosocial and physical functioning. Nicotin Tob Res. 2008;10:463–470. doi: 10.1080/14622200801901922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall SM, Humfleet GL, Muñoz RF, Reus VI, Robbins JA, Prochaska JJ. Extended treatment of older cigarette smokers. Addiction. 2009;104:1043–1052. doi: 10.1111/j.1360-0443.2009.02548.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammersley R. A digest of memory phenomena for addiction research. Addiction. 1994;89:283–293. doi: 10.1111/j.1360-0443.1994.tb00890.x. [DOI] [PubMed] [Google Scholar]
- He Y, Wolf RE, Normand SLT. Assessing geographical variations in hospital processes of care using multilevel item response models. Health Serv Outcome Res Methodol. 2010;10:111–133. doi: 10.1007/s10742-010-0065-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houston TK, Allison JJ, Person S, Kovac S, Williams OD, Kiefe CI. Post-myocardial infarction smoking cessation counseling: associations with immediate and late mortality in older Medicare patients. Am J Med. 2005;118:269–275. doi: 10.1016/j.amjmed.2004.12.007. [DOI] [PubMed] [Google Scholar]
- Jarvis MJ, Cohen JE, Delnevo CD, Giovino GA. Dispelling myths about gender differences in smoking cessation: population data from the USA, Canada and Britain. Tob Control. 2013;22:356–360. doi: 10.1136/tobaccocontrol-2011-050279. [DOI] [PubMed] [Google Scholar]
- Kanjilal S, Gregg EW, Cheng YJ, et al. Socioeconomic status and trends in disparities in 4 major risk factors for cardiovascular disease among US adults, 1971–2002. Arch Intern Med. 2006;166:2348–2355. doi: 10.1001/archinte.166.21.2348. [DOI] [PubMed] [Google Scholar]
- Lyratzopoulos G, Elliott MN, Barbiere JM, et al. How can health care organizations be reliably compared?: Lessons from a national survey of patient experience. Med Care. 2011;49:724–733. doi: 10.1097/MLR.0b013e31821b3482. [DOI] [PubMed] [Google Scholar]
- McIlvain HE, Backer EL, Crabtree BF, Lacy N. Physician attitudes and the use of office-based activities for tobacco control. Fam Med. 2002;34:114–119. [PubMed] [Google Scholar]
- Morgan GD, Noll EL, Orleans CT, Rimer BK, Amfoh K, Bonney G. Reaching midlife and older smokers: tailored interventions for routine medical care. Prev Med. 1996;25:346–354. doi: 10.1006/pmed.1996.0065. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. Changes in Cigarette-Related Disease Risks and Their Implications for Prevention and Control, Smoking and Tobacco Control Monograph No 8. National Cancer Institute; Washington DC: 1997. [Google Scholar]
- Ni Dhubhghaill SS, Cahill MT, Campbell M, Cassidy L, Humphries MM, Humphries P. The pathophysiology of cigarette smoking and age-related macular degeneration. Adv Exp Med Biol. 2010;664:437–446. doi: 10.1007/978-1-4419-1399-9_50. [DOI] [PubMed] [Google Scholar]
- Ossip-Klein DJ, McIntosh S, Utman C, Burton K, Spada J, Guido J. Smokers ages 50+: who gets physician advice to quit? Prev Med. 2000;31:364–369. doi: 10.1006/pmed.2000.0721. [DOI] [PubMed] [Google Scholar]
- Purcell NJ, Kish L. Postcensal estimates for local areas (or domains) Int Stat Rev. 1980:3–18. [Google Scholar]
- Reitz C, den Heijer T, van Duijn C, Hofman A, Breteler MM. Relation between smoking and risk of dementia and Alzheimer disease: the Rotterdam Study. Neurology. 2007;69:998–1005. doi: 10.1212/01.wnl.0000271395.29695.9a. [DOI] [PubMed] [Google Scholar]
- Richmond RL, Anderson P. Research in general practice for smokers and excessive drinkers in Australia and the UK. III. Dissemination of interventions. Addiction. 1994;89:49–62. doi: 10.1111/j.1360-0443.1994.tb00849.x. [DOI] [PubMed] [Google Scholar]
- Rimer BK, Orleans CT. Tailoring smoking cessation for older adults. Cancer. 1994;74:2051–2054. doi: 10.1002/1097-0142(19941001)74:7+<2051::aid-cncr2820741711>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- Rusanen M, Kivipelto M, Quesenberry CP, Jr, Zhou J, Whitmer RA. Heavy smoking in midlife and long-term risk of Alzheimer disease and vascular dementia. Arch Intern Med. 2011;171:333–339. doi: 10.1001/archinternmed.2010.393. [DOI] [PubMed] [Google Scholar]
- Schiller JS, Lucas JW, Ward BW, Peregoy JA. Summary health statistics for U.S. adults: National Health Interview Survey, 2010. Vital Health Stat. 2012;10:1–207. [PubMed] [Google Scholar]
- Shiffman S, Brockwell S, Pillitteri J, Gitchell J. Use of smoking-cessation treatments in the United States. Am J Prev Med. 2008;34:102–111. doi: 10.1016/j.amepre.2007.09.033. [DOI] [PubMed] [Google Scholar]
- Taylor DH, Jr, Hasselblad V, Henley SJ, Thun MJ, Sloan FA. Benefits of smoking cessation for longevity. Am J Public Health. 2002;92:990–996. doi: 10.2105/ajph.92.6.990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinidad DR, Perez-Stable EJ, White MM, Emery SL, Messer K. A nationwide analysis of US racial/ethnic disparities in smoking behaviors, smoking cessation, and cessation-related factors. Am J Public Health. 2011;101:699–706. doi: 10.2105/AJPH.2010.191668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vetter NJ, Ford D. Smoking prevention among people aged 60 and over: a randomized controlled trial. Age Ageing. 1990;19:164–168. doi: 10.1093/ageing/19.3.164. [DOI] [PubMed] [Google Scholar]
- Ward J, Sanson-Fisher R. Accuracy of patient recall of opportunistic smoking cessation advice in general practice. Tob Control. 1996;5:110–113. doi: 10.1136/tc.5.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wassenaar TR, Eickhoff JC, Jarzemsky DR, Smith SS, Larson ML, Schiller JH. Differences in primary care clinicians’ approach to non-small cell lung cancer patients compared with breast cancer. J Thorac Oncol. 2007;2:722–728. doi: 10.1097/JTO.0b013e3180cc2599. [DOI] [PubMed] [Google Scholar]
- Weaver KE, Danhauer SC, Tooze JA, et al. Smoking cessation counseling beliefs and behaviors of outpatient oncology providers. Oncologist. 2012;17:455–462. doi: 10.1634/theoncologist.2011-0350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetter DW, Cofta-Gunn L, Irvin JE, et al. What accounts for the association of education and smoking cessation? Prev Med. 2005;40:452–460. doi: 10.1016/j.ypmed.2004.07.001. [DOI] [PubMed] [Google Scholar]
- Zwar NA, Richmond RL. Role of the general practitioner in smoking cessation. Drug Alcohol Rev. 2006;25:21–26. doi: 10.1080/09595230500459487. [DOI] [PubMed] [Google Scholar]


