Abstract
Metallothioneins (MTs) are a family of low- molecular-weight, cysteine-rich proteins involved in zinc and redox metabolism, that are epigenetically downregulated during colorectal cancer (CRC) progression, but may be re-induced with a variety of agents. Since loss of MT expression is associated with a worse prognosis, in the present study we investigated the effects of overexpression of the most significantly downregulated isoform in CRC, namely MT1G, on the HT-29 cell line. Overexpression of MT1G resulted in xenograft tumors with an aberrant morphology, characterized by an evident increase in mucin-containing cells that were identified as goblet cells under electron microscopy. Immunohistochemical detection of CDX2 and cytokeratin 20 was also increased, as were goblet-cell and enterocyte-specific genes by qRT-PCR. Microarray analysis of gene expression confirmed the alteration of several differentiation signaling pathways, including the Notch pathway. Using sodium butyrate and post-confluent growth as inducers of differentiation, we demonstrated that MT1G does indeed play a functional role in promoting goblet over enterocyte differentiation in vitro. Labile zinc is also induced upon differentiation of CRC cells, functionally contributing to enterocyte over goblet differentiation, as revealed using zinc-specific chelating agents. Overall, our results uncover a new tumor-suppressor activity of MT1G in promoting the differentiation of at least some CRC tumors, and implicate MTs and zinc signaling as new players in colorectal differentiation. This further contributes to the hypothesis that re-induction of MTs may have therapeutic value by diminishing the aggressiveness of CRC tumors.
Keywords: metallothioneins, labile zinc, colorectal cancer, goblet cells, differentiation
Introduction
Colorectal cancer (CRC) is the third most commonly diagnosed cancer worldwide, having a mortality rate near 50% (1). Recent studies have shown that these tumors retain multilineage differentiation processes similar to those of the normal intestinal epithelium, mainly the goblet cell and enterocyte lineages (2). Furthermore, molecular classifications representing these cellular phenotypes can have prognostic value and be predictive of response to different therapeutic agents (3).
Metallothioneins (MTs) are a family of low-molecular-weight, cysteine-rich proteins involved in zinc and redox metabolism. By chelating zinc ions through redox-active thiol groups, they have the capacity to regulate the exchangeable, loosely-bound pool of intracellular zinc, termed the ‘labile’ pool, which participates in zinc transfer reactions and intracellular signaling. Thus MTs have been implicated in many aspects of tumor biology, such as proliferation, differentiation, apoptosis, angiogenesis, redox and zinc homeostasis, anti-inflammatory reactions and immunomodulation (4–7). The human genome encodes at least 11 functional MT isoforms that share structural and functional similarities. Due to their structural similarity, commercially available antibodies do not distinguish between individual MT isoforms, and therefore their individual mRNA expression levels can be measured by qRT-PCR. However, due to the fact that they are variably expressed in tissues and induced by several stimuli, it is possible that different tumors express distinct MT genes, which could help explain the conflicting data on MT function in different tumor types (6,7). We and others have previously shown that multiple MT1 isoforms and MT2A are downregulated during CRC progression (especially isoform MT1G) mainly through epigenetic mechanisms, and that this is associated with shorter patient survival (8–11). Several agents such as DNA methyltransferase inhibitors, histone deacetylase inhibitors or zinc are capable of re-inducing MT expression in colorectal tumors, which can slow down in vivo tumor growth and sensitize these tumors to chemotherapeutic agents (12).
In order to help understand the phenotypic consequences of MT induction, in the present study we investigated the effects of stable overexpression of the most downregulated isoform in CRC, namely MT1G, on the HT-29 CRC cell line. We uncovered a new role for this isoform in modulating tumor differentiation and thus expand the mechanisms by which this gene may act as a tumor suppressor in CRC.
Materials and methods
Reagents and cell lines
The MT1G cDNA was cloned into the pcDNA3.1/myc-His(−)A expression vector, resulting in an MT1G-myc fusion protein as previously described (12). Sodium butyrate and N,N,N',N'-tetrakis(2-pyridylmethyl) ethylenediamine (TPEN) were purchased from Sigma-Aldrich Inc. (St. Louis, MO, USA), and FluoZin-3-AM (FZ) from Invitrogen (San Diego, CA, USA). The human CRC cell lines HT-29 and HCT116 were obtained from the American Type Culture Collection (ATCC; Manassas, VA, USA), maintained as previously described (8), and subjected to STR profiling for authentication after all experiments were finalized. For post-confluent growth, day 0 was considered the day when cells reached 100% confluence, and fresh medium was replaced every 1–2 days thereafter.
Animal studies and histological procedures
Eight- to 10-week-old male nude mice were subcutaneously injected (2×106 cells each) with two independent clones of MOCK or MT1G+ cells (5 mice/group) and tumor size was measured with a caliper to calculate tumor volume using the formula: Tumor volume (mm3) = [length (mm)]×[width (mm)]2×π/6. All animal procedures were approved by the Institutional Animal Care Board of the Leloir Institute. After 50 days, tumors were excised, formalin-fixed and paraffin-embedded for histological examination. A fraction of each tumor was preserved in RNAlater medium (Ambion Inc., Austin TX, USA) at 4̊C for 24 h, and then stored at −80̊C. RNA was extracted from RNAlater-preserved tissues using the TRIzol method (Invitrogen), and quantification and quality control were performed with the Agilent 2100 Bioanalyzer (Agilent Technologies, Santa Clara, CA, USA). Paraffin sections (4 µm thick) were re-hydrated and stained with Alcian Blue stain (1% in 3% acetic acid, pH 2.5) or processed for immunohistochemistry using the Vectastain Universal Elite ABC kit (Vector Laboratories, Inc., Burlingame, CA, USA) with citrate buffer antigen retrieval and the following antibodies: anti-cytokeratin 20 (KS 20.8; Dako Corporation, Carpinteria, CA, USA) and anti-CDX2 (clone EPR2764Y; Cell Marque, Rocklin, CA, USA).
For transmission electron microscopy, freshly xenografted tumors were cut into small (~1-mm thick) pieces and promptly fixed in 2.5% glutaraldehyde in phosphate-buffered saline (PBS) for 2 h, washed and fixed for 90 min in 1% osmium tetroxide in phosphate-buffered saline (PBS), de-hydrated in acetone gradients and included in resin. Semi-(0.5 µm) and ultra-thin (70 nm) sections were cut and contrasted in 2.5% uranyl-acetate, and visualized using a Zeiss EM 109T microscope coupled to a digital CCD Gatan ES1000W camera.
Gene expression profile analysis and qRT-PCR
Total RNA was extracted, and mRNA expression was analyzed using an Agilent Custom microarray 8×15K (Agilent Technologies, Palo Alto, CA, USA), which contained 15,744 oligonucleotide probes representing >8,200 different human transcripts. Two samples from each group were used to detect mRNA expression; each biological replicate was run in duplicate, and the fluorochromes were swapped to reduce dye-bias; in total eight 15K microarrays were scanned using the Axon Confocal Scanner 4000B (Molecular Devices, Sunnyvale, CA, USA) with optimized settings: dye channel, 635 nm, PMT=720, laser power, 30%, scan resolution, 10 nm; dye channel, 532 nm, PMT=540, laser power, 30%, scan resolution, 10 nm; line average, 4 lines. The data were analyzed using GenePix® Pro 6 Microarray Acquisition and Analysis Software (Molecular Devices) and normalized with the MIDAS v2.2: Microarray Data Analysis System (TIGR's Microarray Data Analysis System). Normalization was necessary to compensate for variability between slides and fluorescent dyes. To this end we employed a locally weighted linear regression [Lowess (13,14)]; data were filtered using low-intensity cutoff and replicate consistency trimming.
The differentially expressed genes among the MT1G+, and control (MOCK) sets were identified using the significant analysis of microarray (SAM) statistical software from MultiExperiment Viewer (MeV) (TIGR's Microarray Data Analysis System). In the comparisons of MT1G+ vs. MOCK, the genes that were all upregulated in the comparisons were identified as the persistently upregulated genes, and the genes that were all downregulated in the comparisons were defined as the persistently downregulated genes.
The gene annotation enrichment analysis using Gene Ontology (GO) (http://www.geneontology.org/) and Kyoto Encyclopedia of Genes and Genomes (KEGG) (http://www.genome.jp/kegg/) data for gene sets was performed using Database for Annotation, Visualization, and Integrated Discovery (DAVID) software (15,16). A Benjamini p-value of 0.05 was used in the analysis.
Quantitative reverse-transcription PCR (qRT-PCR) was used to quantify mRNA levels as previously described (8). Briefly, PCR runs were carried out using SYBR Universal Master Mix (Applied Biosystems, Carlsbad, CA, USA), and relative expression levels were determined by the ΔΔCt method using ACTB gene expression to normalize all samples. The primers used are listed in Table I.
Table I.
Primer sequences.
| Gene | Forward primer | Reverse primer |
|---|---|---|
| MT1G | CTTCTCGCTTGGGAACTCTA | AGGGGTCAAGATTGTAGCAAA |
| MT2A | GCAACCTGTCCCGACTCTAG | TTGCAGGAGGTGCATTTG |
| ACTB | GCCATCTCTTGCTCGAAGTCCAG | ATGTTTGAGACCTTCAACACCCC |
| CDKN1A | AAGACCATGTGGACCTGT | GGTAGAAATCTGTCATGCTG |
| HSI | GAGGACACTGGCTTGGAGAC | ATCCAGCGGGTACAGAGATG |
| HALPI | GACCACTCCCATGTCTTCTCCTT | TCGCACGCCTGAGTTGAA |
| CA2 | CCGCGGACACACAGTGCAGG | CCAGTGCTCAGGTCCGTTGTGT |
| CA1 | CAGAACATACAGTGGATGGAGTCAA | GGCCTCACCAACCTTCATCA |
| K20 | AAATGCTCGGTGTGTCCTG | ACTTCCTCCTGATGCTCCTT |
| ATOH1 | CCCCGGGAGCATCTTG | GGGACCGAGGCGAAGTT |
| TFF3 | CTCCAGCTCTGCTGAGGAGT | GCTTGAAACACCAAGGCACT |
| HMUC2 | CAGCACCGATTGCTGAGTTG | GCTGGTCATCTCAATGGCAG |
| CDX2 | GATGGTGATGTAGCGACTGTAGTGA | CTCGGCAGCCAAGTGAAAAC |
Alkaline phosphatase activity measurement
The activity of this enzyme was used as a marker of differentiation of HT-29 cells (17). For this purpose, confluent cell lines were lysed in 10 mM Tris (pH 7.4), 1 mM MgCl2, 20 µM ZnCl2, 0.2% Triton X-100 + protease inhibitors, and incubated with NBT-BCIP as the chromogenic substrate for 16 h at 37̊C. The resulting brown precipitate was solubilized in 10% SDS, 10% HCl and absorbance was measured at 595 nm.
siRNA transfection
Two siRNAs targeting the MT1G isoform (si1G.1 and si1G.2) and one targeting all functional MT-1 and MT-2 isoforms were previously validated (12), and transfected at 125 nM using LF2000 (Invitrogen) as described by the manufacturer. After 24 h of siRNA treatment, medium was replaced with or without 2 mM sodium butyrate for 48 h, and cells were collected for RNA extraction or ALP activity measurement.
Scratch assays and gelatin zymography
We used the scratch assay to estimate the migration capacities of MOCK and MT1G+ cell lines, which were plated in triplicate in 24-well plates until they reached confluence. Two perpendicular scratches were made with a pipette tip, after which the cells were washed thrice in PBS and replaced with 1% fetal bovine serum (FBS) medium. Areas with the same wound length were selected and photographed until complete wound closure. Wound closure at a given time t was calculated as: (initial wound length - wound length at time t)/initial wound length×100.
To determine gelatinase activity of matrix metalloproteinases (MMPs), upon reaching confluence medium was replaced with serum-free Dulbeccos modified Eagles medium (DMEM) for 24 h, and the conditioned medium was centrifuged at 1,200 × g for 5 min, and immediately loaded into 10% polyacrylamide electrophoretic gels with or without 2.5 mg/ml gelatin (Sigma-Aldrich) as described in (18). Coomasie Blue staining of the non-gelatin gels were used as a loading control.
Measurement of intracellular labile zinc
For this purpose we employed the cell-permeable zinc-specific fluorophore FZ as described in (12). Briefly, cells were plated in triplicate in sterile plastic coverslips (for fluorescence microscopy) or in 96-well plates (for fluorimetric analysis), and incubated for 30 min at room temperature with 2 µM FZ in PBS, washed in PBS and incubated a further 30 min in PBS at room temperature. Propidium iodide staining was used to control for plating differences and data are expressed as normalized fluorescence FZ = (F - FTPEN)/(FZn - FTPEN), so as to get values relative to a ‘maximum’ intensity given by pretreatment with zinc 400 µM for 8 h (FZn, resulting in FZ=1) and a ‘minimum’ intensity given by 20 µM TPEN treatment during the final 30 min incubation of fluozin (FTPEN, resulting in FZ=0). This score allowed us to better compare results of the different experiments.
Statistical analysis
Data are expressed as mean ± SEM and p-values <0.05 were considered significant. Comparison of means was carried out using Student's t-test, with one-way ANOVA followed by Dunnett's post hoc t-test for three or more groups, or with two-way ANOVA followed by Bonferroni's post hoc t-test for two variables. GraphPad Prism 5.0 (GraphPad Software, Inc., La Jolla, CA, USA) software was used for analysis.
Results
MT1G overexpression in the HT-29 CRC cell line
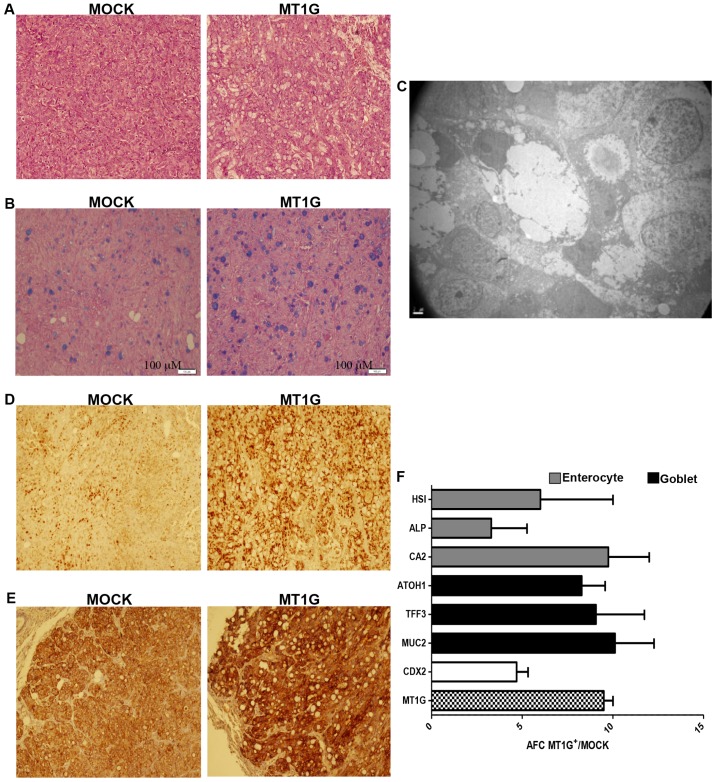
We stably expressed MT1G as a myc-epitope fusion protein in HT-29 cells. When grown in vivo as subcutaneous xenografts on nude mice, these MT1G+ cells grew at similar rates compared to the empty-vector (‘MOCK’)-transfected cells (data not shown), in stark contrast to the antiproliferative effects we had previously observed using the HCT116 cell line (12). However, hematoxylin and eosin (H&E) staining (Fig. 1A) showed that MT1G+ tumors contained a higher number of mucin-containing, Alcian Blue-positive cells (Fig. 1B) that were confirmed to be goblet cells by transmission electron microscopy (Fig. 1C). Nuclear expression of the intestine-specific homeobox transcription factor CDX2 was markedly enhanced in the MT1G+ tumors, as shown by immunohistochemical staining on Fig. 1D, as was also the intensity of cytokeratin 20 (Fig. 1E). The latter also suggests that commitment to the enterocyte lineage may be enhanced as well. Indeed, both goblet-associated (TFF3, ATOH1 and MUC2) and enterocyte-associated genes (HSI, CA2 and ALPI) were overexpressed in the MT1G+ tumors by qRT-PCR analysis (Fig. 1F), suggesting that MT1G+ tumors are more differentiated than MOCK controls.
Figure 1.
HT-29 MOCK and MT1G+ subcutaneous xenografts in nude mice. (A) H&E and (B) Alcian Blue stainings showing an increase in the number of mucin-like cells in the MT1G+ tumors. (C) Microphotograph of a goblet-like cell in MT1G+ tumors. (D) CDX2 and (E) keratin 20 immunohistochemistry. (F) Expression of enterocyte and goblet-associated differentiation markers, as assessed by qRT-PCR. AFC, average fold-change.
Gene expression analysis of HT-29 MT1G+ tumors using cDNA microarrays
We then used cDNA microarrays to profile the mRNA expression of MOCK and MT1G+ HT-29 xenografts, derived from two different MT1G+ or MOCK clonal cell lines (MT1G-1 and MT1G-2, or MOCK-1 and MOCK-2, respectively). Gene expression profiles of the biological replicates were reproducible and highly correlated (Pearson's correlation coefficient 0.81). Analysis of data with Rank product analysis revealed significant gene expression differences among the groups, with a total of 305 known genes found to be consistently upregulated or downregulated in the MT1G+ tumors (Table II). GO analysis indicated that several functional categories were enriched by DAVID, and included upregulated genes associated with cell differentiation, cell fate commitment and Notch signaling pathway, as well as downregulated genes in the categories of regulation of apoptosis, cell migration and cell proliferation (Table III). Differentially expressed genes were also analyzed for KEGG pathway enrichment and two significantly enriched pathways were identified between upegulated or downregulated genes: the Notch signaling pathway and pathways in cancer, respectively.
Table II.
List of all significantly differentially expressed genes in MT1G+ vs. MOCK HT-29 xenografts.
| A, Upregulated genes | |||||
|---|---|---|---|---|---|
| Gene reference | Gene symbol | Name | Mean | P-values (Up) | RP-values (Up) |
| NM_138444 | KCTD12 | Potassium channel tetramerisation domain containing 12 | 2.65 | 2.81E-06 | 80.00 |
| NM_000051 | ATM | Ataxia telangiectasia mutated | 2.52 | 4.68E-06 | 91.77 |
| NM_175698 | SSX2 | Synovial sarcoma, X breakpoint 2 | 3.06 | 6.56E-06 | 99.19 |
| NM_031964 | KRTAP17-1 | Keratin-associated protein 17-1 | 2.35 | 2.25E-05 | 141.15 |
| NM_003357 | SCGB1A1 | Secretoglobin, family 1A, member 1 (uteroglobin) | 2.19 | 2.72E-05 | 155.94 |
| NM_005430 | WNT1 | Wingless-type MMTV integration site family, member 1 | 2.40 | 2.81E-05 | 156.29 |
| NM_001031672 | CYB5RL | Cytochrome b5 reductase-like | 2.37 | 3.18E-05 | 164.29 |
| NM_000546 | TP53 | Tumor protein p53 | 2.12 | 3.75E-05 | 168.99 |
| NM_001123065 | Chromosome 7 open reading frame 65 | 2.04 | 4.59E-05 | 181.40 | |
| NM_001443 | FABP1 | Fatty acid binding protein 1, liver | 2.27 | 5.99E-05 | 197.89 |
| NM_000364 | TNNT2 | Troponin T type 2 (cardiac) | 2.01 | 8.24E-05 | 216.07 |
| NM_001201 | BMP3 | Bone morphogenetic protein 3 | 2.17 | 1.01E-04 | 224.84 |
| NM_031310 | PLVAP | Plasmalemma vesicle-associated protein | 2.02 | 1.22E-04 | 239.78 |
| NM_182981 | OSGIN1 | Oxidative stress induced growth inhibitor 1 | 1.89 | 1.44E-04 | 249.22 |
| NM_139211 | HOPX | HOP homeobox | 1.88 | 1.65E-04 | 256.18 |
| NM_017774 | CDKAL1 | CDK5 regulatory subunit-associated protein 1-like 1 | 1.86 | 2.00E-04 | 271.00 |
| NM_001077195 | ZNF436 | Zinc finger protein 436 | 1.96 | 2.62E-04 | 289.52 |
| NM_000067 | CA2 | Carbonic anhydrase II | 1.76 | 2.82E-04 | 295.37 |
| NM_015894 | STMN3 | Stathmin-like 3 | 1.17 | 2.86E-04 | 296.25 |
| NM_014237 | ADAM18 | ADAM metallopeptidase domain 18 | 2.19 | 2.95E-04 | 298.48 |
| NM_182705 | FAM101B | Family with sequence similarity 101, member B | 1.81 | 4.28E-04 | 330.71 |
| NM_025191 | EDEM3 | ER degradation enhancer, α-mannosidase-like 3 | 1.78 | 4.56E-04 | 337.06 |
| NM_020639 | RIPK4 | Receptor-interacting serine-threonine kinase 4 | 1.70 | 4.56E-04 | 337.43 |
| NM_004557 | NOTCH4 | Notch 4 | 1.70 | 4.77E-04 | 340.80 |
| NM_005618 | DLL1 | δ-like 1 (Drosophila) | 1.70 | 5.05E-04 | 346.21 |
| NM_004001 | FCGR2B | Fc fragment of IgG, low affinity IIb, receptor (CD32) | 1.71 | 5.22E-04 | 349.94 |
| NM_001008225 | CNOT4 | CCR4-NOT transcription complex, subunit 4 | 1.66 | 6.17E-04 | 367.80 |
| NM_170664 | OTOA | Οtoancorin | 1.64 | 6.23E-04 | 368.88 |
| NM_019845 | RPRM | Reprimo, TP53-dependent G2 arrest mediator candidate | 1.39 | 6.24E-04 | 369.37 |
| NM_033409 | SLC52A3 | Chromosome 20 open reading frame 54 | 1.65 | 6.26E-04 | 369.79 |
| NM_001010879 | ZIK1 | Zinc finger protein interacting with K protein 1 homolog (mouse) | 1.59 | 6.68E-04 | 376.61 |
| NM_007365 | PADI2 | Peptidyl arginine deiminase, type II | 1.98 | 6.99E-04 | 381.36 |
| NM_007314 | ABL2 | v-abl Abelson murine leukemia viral oncogene homolog 2 | 0.99 | 7.21E-04 | 385.01 |
| NM_001080519 | BAHCC1 | BAH domain and coiled-coil containing 1 | 1.58 | 7.93E-04 | 397.25 |
| NM_000584 | CXCL8 | Interleukin 8 | 1.68 | 9.46E-04 | 419.56 |
| NM_002649 | PIK3CG | Phosphoinositide-3-kinase, catalytic, γ-polypeptide | 1.74 | 1.07E-03 | 437.34 |
| NM_178311 | GGTLC1 | γ-glutamyltransferase light chain 1 | 1.28 | 1.09E-03 | 440.27 |
| NM_001124756 | PABPC1L | Poly(A) binding protein, cytoplasmic 1-like | 1.51 | 1.11E-03 | 442.81 |
| NM_001010926 | HES5 | Hairy and enhancer of split 5 (Drosophila) | 1.09 | 1.15E-03 | 446.74 |
| NM_152643 | KNDC1 | Kinase non-catalytic C-lobe domain (KIND) containing 1 | 1.85 | 1.18E-03 | 449.71 |
| NM_152279 | ZNF585B | Zinc finger protein 585B | 1.30 | 1.18E-03 | 450.06 |
| NM_003018 | SFTPC | Surfactant protein C | 1.51 | 1.20E-03 | 452.03 |
| NM_003460 | ZP2 | Zona pellucida glycoprotein 2 (sperm receptor) | 1.79 | 1.23E-03 | 456.86 |
| NM_022101 | Chromosome X open reading frame 56 | 0.84 | 1.30E-03 | 464.79 | |
| NM_001136566 | RAD21L1 | RAD21-like 1 (S. pombe) | 0.61 | 1.31E-03 | 465.53 |
| NM_019886 | CHST7 | Carbohydrate (N-acetylglucosamine 6-O) sulfotransferase 7 | 1.49 | 1.43E-03 | 477.78 |
| NM_002410 | MGAT5 | Mannosyl (α-1,6-)-glycoprotein β-1,6-N-acetyl-glucosaminyltransferase | 1.37 | 1.49E-03 | 484.02 |
| NM_001130715 | PLAC8 | Placenta-specific 8 | 1.47 | 1.51E-03 | 485.05 |
| NM_012368 | OR2C1 | Olfactory receptor, family 2, subfamily C, member 1 | 1.42 | 1.60E-03 | 493.64 |
| NM_198463 | C3ORF67 | Chromosome 3 open reading frame 67 | 1.55 | 1.72E-03 | 503.50 |
| NM_080647 | TBX1 | T-box 1 | 1.01 | 1.74E-03 | 504.66 |
| NM_001136003 | C2CD4D | C2 calcium-dependent domain containing 4D | 1.38 | 1.83E-03 | 512.27 |
| NM_014909 | VASH1 | Vasohibin 1 | 1.38 | 1.84E-03 | 512.54 |
| NM_002318 | LOXL2 | Lysyl oxidase-like 2 | 1.44 | 1.91E-03 | 518.96 |
| NM_031457 | MS4A8 | Membrane-spanning 4-domains, subfamily A, member 8B | 1.36 | 2.17E-03 | 538.29 |
| NM_001146190 | ZNF407 | Zinc finger protein 407 | 1.35 | 2.20E-03 | 541.10 |
| NM_004375 | COX11 | COX11 cytochrome c oxidase assembly homolog (yeast) | 1.37 | 2.36E-03 | 552.91 |
| NM_001040462 | BTNL8 | Butyrophilin-like 8 | 0.84 | 2.39E-03 | 554.54 |
| NM_001265 | CDX2 | Caudal type homeobox 2 | 1.33 | 2.44E-03 | 558.57 |
| NM_001013661 | VSIG8 | V-set and immunoglobulin domain containing 8 | 1.33 | 2.50E-03 | 563.31 |
| NM_019119 | PCDHB9 | Protocadherin-β9 | 1.32 | 2.51E-03 | 564.49 |
| NM_001144875 | DOK3 | Docking protein 3 | 1.29 | 2.54E-03 | 566.33 |
| NM_003722 | TP63 | Tumor protein p63 | 1.38 | 2.56E-03 | 569.10 |
| NM_006138 | MS4A3 | Membrane-spanning 4-domains, subfamily A, member 3 (hematopoietic cell-specific) | 1.58 | 2.73E-03 | 580.41 |
| NM_005427 | TP73 | Tumor protein p73 | 1.37 | 2.88E-03 | 589.30 |
| NM_003106 | SOX2 | SRY (sex determining region Y)-box 2 | 1.07 | 3.12E-03 | 604.10 |
| NM_033318 | SMDT1 | Chromosome 22 open reading frame 32 | 0.80 | 3.14E-03 | 605.59 |
| NM_012426 | SF3B3 | Splicing factor 3b, subunit 3, 130 kDa | 1.31 | 3.31E-03 | 615.60 |
| NM_002458 | MUC5B | Mucin 5B, oligomeric mucus/gel-forming | 1.53 | 3.45E-03 | 623.75 |
| NM_001001411 | ZNF676 | Zinc finger protein 676 | 1.45 | 3.48E-03 | 625.90 |
| NM_000362 | TIMP3 | TIMP metallopeptidase inhibitor 3 | 1.33 | 3.55E-03 | 629.94 |
| NM_014751 | MTSS1 | Metastasis suppressor 1 | 1.23 | 3.62E-03 | 633.32 |
| NM_201442 | C1S | Complement component 1, s subcomponent | 0.91 | 3.63E-03 | 633.68 |
| NM_005961 | MUC6 | Mucin 6, oligomeric mucus/gel-forming | 1.21 | 3.92E-03 | 647.05 |
| NM_001002758 | PRY2 | PTPN13-like, Y-linked 2 | 1.47 | 3.99E-03 | 650.48 |
| NM_001135654 | PABPC4 | Poly(A) binding protein, cytoplasmic 4 (inducible form) | 1.31 | 4.01E-03 | 651.26 |
| NM_014030 | GIT1 | G protein-coupled receptor kinase interacting ArfGAP 1 | 1.17 | 4.13E-03 | 657.53 |
| NM_001083537 | FAM86B1 | Family with sequence similarity 86, member B1 | 1.29 | 4.16E-03 | 658.91 |
| NM_001645 | APOC1 | Apolipoprotein C-I | 1.20 | 4.27E-03 | 664.10 |
| NM_003226 | TFF3 | Trefoil factor 3 (intestinal) | 1.19 | 4.29E-03 | 664.92 |
| NM_005172 | ATOH1 | Atonal homolog 1 (Drosophila) | 1.26 | 4.31E-03 | 665.93 |
| NM_003708 | RDH16 | Retinol dehydrogenase 16 (all-trans) | 0.92 | 4.41E-03 | 670.22 |
| NM_002917 | RFNG | RFNG O-fucosylpeptide 3-β-N-acetylglucosaminyltransferase | 1.28 | 4.56E-03 | 677.43 |
| NM_016585 | THEG | Theg homolog (mouse) | 1.19 | 4.63E-03 | 681.11 |
| NM_007058 | CAPN11 | Calpain 11 | 1.51 | 4.73E-03 | 684.84 |
| NM_003759 | SLC4A4 | Solute carrier family 4, sodium bicarbonate co-transporter, member 4 | 1.19 | 4.74E-03 | 685.17 |
| NM_020299 | AKR1B10 | Aldo-keto reductase family 1, member B10 (aldose reductase) | 1.17 | 4.77E-03 | 686.57 |
| NM_032133 | MYCBPAP | MYCBP-associated protein | 0.92 | 4.95E-03 | 693.39 |
| NM_001631 | ALPI | Alkaline phosphatase, intestinal | 1.25 | 4.98E-03 | 695.09 |
| NM_002486 | NCBP1 | Nuclear cap binding protein subunit 1, 80 kDa | 1.23 | 5.09E-03 | 699.73 |
| NM_001105659 | LRRIQ3 | Leucine-rich repeats and IQ motif containing 3 | 1.18 | 5.13E-03 | 702.05 |
| NM_014276 | RBPJL | Recombination signal binding protein for immunoglobulin-κJ region-like | 1.15 | 5.29E-03 | 708.75 |
| NM_015461 | ZNF521 | Zinc finger protein 521 | 0.91 | 5.35E-03 | 711.10 |
| NM_001105662 | Ubiquitin specific peptidase 17 | 1.21 | 5.63E-03 | 722.91 | |
| NM_005068 | SIM1 | Single-minded homolog 1 (Drosophila) | 1.19 | 5.73E-03 | 726.21 |
| NM_018646 | TRPV6 | Transient receptor potential cation channel, subfamily V, member 6 | 0.64 | 6.05E-03 | 739.17 |
| NM_139026 | ADAMTS13 | ADAM metallopeptidase with thrombospondin type 1 motif, 13 | 0.84 | 6.31E-03 | 749.50 |
| NM_152749 | ATXN7L1 | Ataxin 7-like 1 | 0.75 | 6.31E-03 | 749.64 |
| NM_019034 | RHOF | Ras homolog gene family, member F (in filopodia) | 1.21 | 6.35E-03 | 751.22 |
| NM_017592 | MED29 | Mediator complex subunit 29 | 0.92 | 6.38E-03 | 752.10 |
| NM_206965 | FTCD | Formiminotransferase cyclodeaminase | 1.16 | 6.40E-03 | 752.88 |
| NM_020063 | BARHL2 | BarH-like homeobox 2 | 1.10 | 6.41E-03 | 753.43 |
| NM_016338 | IPO11 | Importin 11 | 0.74 | 6.51E-03 | 756.92 |
| NM_001109997 | KLHL33 | Kelch-like 33 (Drosophila) | 1.15 | 6.61E-03 | 761.02 |
| NM_004235 | KLF4 | Kruppel-like factor 4 (gut) | 0.96 | 6.64E-03 | 762.27 |
| NM_172365 | PPP1R36 | Protein phosphatase 1, regulatory subunit 36 | 0.93 | 6.74E-03 | 765.82 |
| NM_003665 | FCN3 | Ficolin (collagen/fibrinogen domain containing) 3 (Hakata antigen) | 1.23 | 6.86E-03 | 770.05 |
| NM_017910 | TRMT61B | tRNA methyltransferase 61 homolog B (S. cerevisiae) | 0.97 | 7.11E-03 | 778.71 |
| NM_031459 | SESN2 | Sestrin 2 | 0.27 | 7.16E-03 | 780.18 |
| NM_203458 | NOTCH2NL | Notch 2 N-terminal like | 0.59 | 7.16E-03 | 780.21 |
| NM_002203 | ITGA2 | Integrin, α2 (CD49B, α2 subunit of VLA-2 receptor) | 1.20 | 7.16E-03 | 780.44 |
| NM_138337 | CLEC12A | C-type lectin domain family 12, member A | 1.32 | 7.22E-03 | 782.42 |
| NM_020533 | MCOLN1 | Mucolipin 1 | 0.51 | 7.33E-03 | 786.12 |
| NM_022481 | ARAP3 | ArfGAP with RhoGAP domain, ankyrin repeat and PH domain 3 | 1.11 | 7.42E-03 | 789.36 |
| NM_001105578 | SYCE2 | Synaptonemal complex central element protein 2 | 1.13 | 7.66E-03 | 797.43 |
| NM_021969 | NR0B2 | Nuclear receptor subfamily 0, group B, member 2 | 1.16 | 7.68E-03 | 798.17 |
| NM_015852 | ZNF117 | Zinc finger protein 117 | 1.18 | 7.69E-03 | 798.86 |
| NM_023946 | LYNX1 | Ly6/neurotoxin 1 | 1.10 | 7.89E-03 | 805.77 |
| NM_001039887 | PROSER3 | Chromosome 19 open reading frame 55 | 1.17 | 7.94E-03 | 807.24 |
| NM_015184 | PLCL2 | Phospholipase C-like 2 | 1.06 | 8.02E-03 | 809.76 |
| NM_004938 | DAPK1 | Death-associated protein kinase 1 | 0.54 | 8.06E-03 | 811.54 |
| NM_004755 | RPS6KA5 | Ribosomal protein S6 kinase, 90 kDa, polypeptide 5 | 1.04 | 8.21E-03 | 816.35 |
| NM_001007532 | STH | Saitohin | 1.17 | 8.24E-03 | 817.51 |
| NM_002613 | PDPK1 | 3-Phosphoinositide-dependent protein kinase-1 | 1.10 | 8.34E-03 | 820.46 |
| NM_006620 | HBS1L | HBS1-like (S. cerevisiae) | 1.04 | 8.46E-03 | 824.24 |
| NM_003382 | VIPR2 | Vasoactive intestinal peptide receptor 2 | 0.77 | 8.55E-03 | 826.94 |
| NM_203486 | DLL3 | δ-like 3 (Drosophila) | 1.07 | 8.56E-03 | 827.15 |
| NM_018010 | IFT57 | Intraflagellar transport 57 homolog (Chlamydomonas) | 0.92 | 8.74E-03 | 833.66 |
| NM_001135816 | CXORF56 | C1QTNF9B antisense RNA 1 (non-protein coding) | 0.87 | 8.76E-03 | 834.30 |
| NM_033133 | CNP | 2′,3′-Cyclic nucleotide 3 phosphodiesterase | 1.02 | 8.84E-03 | 836.32 |
| NM_005199 | CHRNG | Cholinergic receptor, nicotinic, γ | 0.98 | 9.01E-03 | 841.20 |
| NM_182765 | HECTD2 | HECT domain containing 2 | 0.79 | 9.12E-03 | 844.85 |
| NM_001145290 | SLC37A2 | Solute carrier family 37 (glycerol-3- phosphate transporter), member 2 | 0.90 | 9.15E-03 | 845.70 |
| NM_001195252 | APTX | Aprataxin | 1.05 | 9.31E-03 | 850.77 |
| NM_001251964 | TP53AIP1 | Tumor protein p53-regulated apoptosis inducing protein 1 | 1.26 | 9.35E-03 | 851.82 |
| NM_198270 | NHS | Nance-Horan syndrome (congenital cataracts and dental anomalies) | 1.13 | 9.53E-03 | 857.71 |
| NM_000578 | SLC11A1 | Solute carrier family 11 (proton-coupled divalent metal ion transporters), member 1 | 1.06 | 9.63E-03 | 859.97 |
| NM_002139 | RBMX | RNA binding motif protein, X-linked | 1.06 | 9.65E-03 | 860.47 |
| NM_000435 | NOTCH3 | Notch 3 | 1.10 | 9.71E-03 | 862.14 |
| NM_033066 | MPP4 | Membrane protein, palmitoylated 4 (MAGUK p55 subfamily member 4) | 1.12 | 9.87E-03 | 867.43 |
| B, Downregulated genes | |||||
| Gene reference | Gene symbol | Name | Mean | P-values (Down) | RP-values (Down) |
| AJ298317 | MUC5AC | Mucin 5AC, oligomeric mucus/gel-forming | −2.54 | 8.43E-06 | 112.88 |
| AF547222 | LOC280665 | Anti-CNG α1 cation channel translation product-like | −2.76 | 1.31E-05 | 123.92 |
| AK097187 | NQO2 | NAD(P)H dehydrogenase, quinone 2 | −2.48 | 3.75E-05 | 169.61 |
| AK128551 | RNF216 | Ring finger protein 216 | −2.19 | 6.09E-05 | 198.31 |
| BC062748 | EFCAB10 | EF-hand calcium binding domain 10 | −2.10 | 1.14E-04 | 233.55 |
| NM_000639 | FASLG | Fas ligand (TNF superfamily, member 6) | −1.61 | 2.15E-04 | 274.72 |
| NM_001124 | ADM | Adrenomedullin | −1.48 | 3.43E-04 | 311.18 |
| NM_000043 | FAS | Fas (TNF receptor superfamily, member 6) | −1.68 | 4.22E-04 | 329.27 |
| BC065002 | EXD3 | Exonuclease 3′-5′ domain containing 3 | −2.04 | 5.19E-04 | 349.20 |
| NM_004931 | CD8B | CD8b molecule | −1.24 | 6.82E-04 | 378.73 |
| NM_021635 | PBOV1 | Prostate and breast cancer overexpressed 1 | −1.17 | 7.31E-04 | 386.63 |
| NM_000093 | COL5A1 | Collagen, type V, α1 | −1.67 | 8.08E-04 | 398.60 |
| NM_000429 | MAT1A | Methionine adenosyltransferase I, α | −1.67 | 8.43E-04 | 403.54 |
| NM_000033 | ABCD1 | ATP-binding cassette, sub-family D (ALD), member 1 | −1.69 | 8.92E-04 | 411.33 |
| NM_000125 | ESR1 | Estrogen receptor 1 | −1.67 | 8.95E-04 | 411.64 |
| NM_000808 | GABRA3 | γ-Aminobutyric acid (GABA) A receptor, α3 | −1.60 | 9.27E-04 | 415.96 |
| NM_000595 | LTA | Lymphotoxin-α (TNF superfamily, member 1) | −1.63 | 9.95E-04 | 427.69 |
| NM_000197 | HSD17B3 | Hydroxysteroid (17-β) dehydrogenase 3 | −1.67 | 1.04E-03 | 432.79 |
| NM_001037442 | RUFY3 | RUN and FYVE domain containing 3 | −1.54 | 1.05E-03 | 434.60 |
| NM_000545 | HNF1A | HNF1 homeobox A | −1.64 | 1.07E-03 | 437.31 |
| NM_001005490 | OR6C74 | Olfactory receptor, family 6, subfamily C, member 74 | −1.59 | 1.09E-03 | 439.40 |
| NM_001031848 | SERPINB8 | Serpin peptidase inhibitor, clade B (ovalbumin), member 8 | −1.54 | 1.15E-03 | 447.15 |
| NM_000612 | IGF2 | Insulin-like growth factor 2 (somatomedin A) | −1.63 | 1.16E-03 | 448.01 |
| NM_000517 | HBA2 | Hemoglobin, α2 | −1.64 | 1.19E-03 | 451.63 |
| NM_001130861 | CLDN5 | Claudin 5 | −1.44 | 1.24E-03 | 458.33 |
| NM_001004688 | OR2M2 | Olfactory receptor, family 2, subfamily M, member 2 | −1.59 | 1.24E-03 | 458.57 |
| NM_001030004 | HNF4A | Hepatocyte nuclear factor 4, α | −1.56 | 1.26E-03 | 460.62 |
| NM_001033952 | CALCA | Calcitonin-related polypeptide α | −1.54 | 1.26E-03 | 461.21 |
| NM_001010870 | TDRD6 | Tudor domain containing 6 | −1.58 | 1.32E-03 | 466.23 |
| NM_001018025 | MTCP1 | Mature T cell proliferation 1 | −1.57 | 1.41E-03 | 475.20 |
| NM_001012967 | DDX60L | DEAD (Asp-Glu-Ala-Asp) box polypeptide 60-like | −1.57 | 1.41E-03 | 475.20 |
| NM_001085 | SERPINA3 | Serpin peptidase inhibitor, clade A (α-1 antiproteinase, antitrypsin), member 3 | −1.49 | 1.42E-03 | 476.63 |
| NM_000633 | BCL2 | B-cell CLL/lymphoma 2 | −1.63 | 1.45E-03 | 479.53 |
| NM_001037666 | GATSL3 | GATS protein-like 3 | −1.52 | 1.52E-03 | 486.52 |
| NM_001165 | BIRC3 | Baculoviral IAP repeat containing 3 | −1.42 | 1.58E-03 | 491.86 |
| NM_002247 | KCNMA1 | Potassium large conductance calcium-activated channel, subfamily M, α member 1 | −1.33 | 1.94E-03 | 521.16 |
| NM_173625 | C17ORF78 | Chromosome 17 open reading frame 78 | −1.01 | 1.95E-03 | 521.61 |
| NM_001124759 | FRG2C | FSHD region gene 2 family, member C | −1.44 | 2.00E-03 | 524.95 |
| NM_001080453 | INTS1 | Integrator complex subunit 1 | −1.51 | 2.00E-03 | 524.88 |
| NM_004613 | TGM2 | Transglutaminase 2 (C polypeptide, protein-glutamine-γ-glutamyltransferase) | −1.24 | 2.14E-03 | 536.10 |
| NM_001044392 | MUC1 | Mucin 1, cell surface-associated | −1.51 | 2.31E-03 | 548.26 |
| NM_001195127 | WI2-2373I1.2 | Forkhead box L1-like | −1.39 | 2.41E-03 | 556.59 |
| NM_001243042 | HLA-C | Major histocompatibility complex, class I, C | −1.38 | 2.43E-03 | 558.50 |
| NM_001083602 | PTCH1 | Patched 1 | −1.49 | 2.58E-03 | 570.46 |
| NM_207352 | CYP4V2 | Cytochrome P450, family 4, subfamily V, polypeptide 2 | −0.86 | 2.71E-03 | 579.03 |
| NR_029392 | KRT16P2 | Keratin 16 pseudogene 2 | −0.54 | 2.97E-03 | 594.00 |
| NM_001172646 | PLCB4 | Phospholipase C, β4 | −1.39 | 3.03E-03 | 598.52 |
| NM_002089 | CXCL2 | Chemokine (C-X-C motif) ligand 2 | −1.34 | 3.39E-03 | 620.43 |
| NM_001496 | GFRA3 | GDNF family receptor α3 | −1.38 | 3.40E-03 | 620.75 |
| NM_001668 | ARNT | Aryl hydrocarbon receptor nuclear translocator | −1.37 | 3.42E-03 | 622.12 |
| NM_021151 | CROT | Carnitine O-octanoyltransferase | −1.18 | 3.47E-03 | 624.70 |
| NM_001949 | E2F3 | E2F transcription factor 3 | −1.36 | 3.53E-03 | 628.70 |
| NM_002307 | LGALS7 | Lectin, galactoside-binding, soluble, 7 | −1.32 | 3.56E-03 | 630.07 |
| NM_001704 | BAI3 | Brain-specific angiogenesis inhibitor 3 | −1.37 | 3.57E-03 | 630.78 |
| NM_001978 | DMTN | Erythrocyte membrane protein band 4.9 (dematin) | −1.35 | 3.62E-03 | 633.47 |
| NM_183001 | SHC1 | SHC (Src homology 2 domain containing) transforming protein 1 | −0.90 | 3.64E-03 | 634.32 |
| NM_001185156 | IL24 | Interleukin 24 | −1.39 | 3.71E-03 | 637.18 |
| NM_004048 | B2M | β-2-microglobulin | −1.27 | 3.73E-03 | 637.88 |
| NM_001004456 | OR1M1 | Olfactory receptor, family 1, subfamily M, member 1 | −1.60 | 3.85E-03 | 644.36 |
| NM_002133 | HMOX1 | Heme oxygenase (decycling) 1 | −1.33 | 3.97E-03 | 649.35 |
| NM_002457 | MUC2 | Mucin 2, oligomeric mucus/gel-forming | −1.31 | 4.02E-03 | 651.72 |
| NM_001198 | PRDM1 | PR domain containing 1, with ZNF domain | −1.39 | 4.05E-03 | 653.14 |
| NM_001136022 | NFATC4 | Nuclear factor of activated T cells, cytoplasmic, calcineurin-dependent 4 | −1.43 | 4.06E-03 | 653.68 |
| NM_001454 | FOXJ1 | Horkhead box J1 | −1.38 | 4.11E-03 | 656.34 |
| NM_002006 | FGF2 | Fibroblast growth factor 2 (basic) | −1.35 | 4.11E-03 | 656.64 |
| NM_177996 | EPB41L1 | Erythrocyte membrane protein band 4.1-like 1 | −0.97 | 4.19E-03 | 659.94 |
| NM_004417 | DUSP1 | Dual specificity phosphatase 1 | −1.25 | 4.38E-03 | 669.42 |
| NM_201282 | EGFR | Epidermal growth factor receptor | −0.88 | 4.53E-03 | 676.59 |
| NM_004416 | DTX1 | Deltex homolog 1 (Drosophila) | −1.25 | 4.68E-03 | 682.88 |
| NM_003128 | SPTBN1 | Spectrin, β, non-erythrocytic 1 | −1.29 | 4.75E-03 | 685.70 |
| NM_001807 | CEL | Carboxyl ester lipase (bile salt-stimulated lipase) | −1.36 | 4.94E-03 | 693.06 |
| NM_207336 | ZNF467 | Zinc finger protein 467 | −0.86 | 4.95E-03 | 693.44 |
| NM_002381 | MATN3 | Matrilin 3 | −1.32 | 5.00E-03 | 695.99 |
| NM_002317 | LOX | Lysyl oxidase | −1.32 | 5.00E-03 | 696.01 |
| NM_024766 | CAMKMT | Calmodulin-lysine N-methyltransferase | −1.15 | 5.07E-03 | 699.15 |
| NM_003667 | LGR5 | Leucine-rich repeat containing G protein-coupled receptor 5 | −1.29 | 5.27E-03 | 707.84 |
| NM_002535 | OAS2 | 2′-5′-Oligoadenylate synthetase 2, 69/71 kDa | −1.30 | 5.27E-03 | 708.15 |
| NM_145041 | TMEM106A | Transmembrane protein 106A | −1.10 | 5.27E-03 | 708.30 |
| NM_003061 | SLIT1 | Slit homolog 1 (Drosophila) | −1.30 | 5.36E-03 | 711.28 |
| NM_013292 | MYLPF | Myosin light chain, phosphorylatable, fast skeletal muscle | −1.21 | 5.40E-03 | 712.71 |
| NM_004310 | RHOH | Ras homolog gene family, member H | −1.26 | 5.55E-03 | 719.34 |
| NM_002483 | CEACAM6 | Carcinoembryonic antigen-related cell adhesion molecule 6 | −1.30 | 5.71E-03 | 725.32 |
| NM_005531 | IFI16 | Interferon, γ-inducible protein 16 | −1.23 | 5.87E-03 | 732.01 |
| NM_133471 | PPP1R18 | Protein phosphatase 1, regulatory subunit 18 | −1.13 | 5.88E-03 | 732.45 |
| NM_006398 | UBD | Ubiquitin D | −1.22 | 5.89E-03 | 732.86 |
| NM_004994 | MMP9 | Matrix metallopeptidase 9 (gelatinase B, 92 kDa gelatinase, 92 kDa type IV collagenase) | −1.24 | 5.90E-03 | 733.00 |
| NR_003531 | MEG3 | Maternally expressed 3 (non-protein coding) | −0.79 | 5.98E-03 | 736.40 |
| NM_012171 | TSPAN17 | Tetraspanin 17 | −1.22 | 6.10E-03 | 741.06 |
| NM_032599 | FAM71F1 | Family with sequence similarity 71, member F1 | −1.14 | 6.13E-03 | 742.39 |
| NM_019074 | DLL4 | δ-like 4 (Drosophila) | −1.19 | 6.16E-03 | 743.53 |
| NM_002405 | MFNG | MFNG O-fucosylpeptide 3-β-N-acetylglucosaminyltransferase | −1.31 | 6.30E-03 | 749.05 |
| NM_015000 | STK38L | Serine/threonine kinase 38-like | −1.21 | 6.32E-03 | 750.10 |
| NM_018416 | FOXJ2 | Forkhead box J2 | −1.20 | 6.36E-03 | 751.65 |
| NM_016135 | ETV7 | Ets variant 7 | −1.21 | 6.38E-03 | 752.29 |
| NM_015886 | PI15 | Peptidase inhibitor 15 | −1.21 | 6.39E-03 | 752.62 |
| NM_002543 | OLR1 | Oxidized low density lipoprotein (lectin-like) receptor 1 | −1.30 | 6.40E-03 | 752.88 |
| NM_005023 | PGGT1B | Protein geranylgeranyltransferase type I, β-subunit | −1.24 | 6.53E-03 | 757.78 |
| NM_172390 | NFATC1 | Nuclear factor of activated T cells, cytoplasmic, calcineurin-dependent 1 | −1.02 | 6.57E-03 | 759.52 |
| NM_017766 | CASZ1 | Castor zinc finger 1 | −1.20 | 6.78E-03 | 767.06 |
| NM_144633 | KCNH8 | Potassium voltage-gated channel, subfamily H (eag-related), member 8 | −1.12 | 6.86E-03 | 770.19 |
| NM_025125 | TMEM254 | Chromosome 10 open reading frame 57 | −1.14 | 6.87E-03 | 770.43 |
| NM_182909 | FILIP1L | Filamin A interacting protein 1-like | −0.92 | 6.89E-03 | 771.28 |
| NM_173503 | EFCAB3 | EF-hand calcium binding domain 3 | −1.02 | 6.92E-03 | 772.10 |
| NM_144673 | CMTM2 | CKLF-like MARVEL transmembrane domain containing 2 | −1.12 | 6.95E-03 | 773.54 |
| NM_021819 | LMAN1L | Lectin, mannose-binding, 1-like | −1.17 | 6.95E-03 | 773.62 |
| NM_022804 | SNURF | SNRPN upstream reading frame | −1.16 | 6.99E-03 | 775.02 |
| NM_021633 | KLHL12 | Kelch-like 12 (Drosophila) | −1.17 | 7.01E-03 | 775.60 |
| NM_021966 | TCL1A | T cell leukemia/lymphoma 1A | −1.16 | 7.23E-03 | 782.50 |
| NM_032637 | SKP2 | S phase kinase-associated protein 2 (p45) | −1.14 | 7.27E-03 | 784.16 |
| NM_022648 | TNS1 | Tensin 1 | −1.16 | 7.32E-03 | 785.88 |
| NM_004213 | SLC28A1 | Solute carrier family 28 (sodium-coupled nucleoside transporter), member 1 | −1.27 | 7.46E-03 | 790.45 |
| NM_033088 | STRIP1 | Family with sequence similarity 40, member A | −1.14 | 7.49E-03 | 791.43 |
| NM_022304 | HRH2 | Histamine receptor H2 | −1.16 | 7.62E-03 | 796.01 |
| NM_021105 | PLSCR1 | Phospholipid scramblase 1 | −1.18 | 7.65E-03 | 797.28 |
| NM_024768 | EFCC1 | Coiled-coil domain containing 48 | −1.15 | 7.66E-03 | 797.48 |
| NM_006290 | TNFAIP3 | Tumor necrosis factor, α-induced protein 3 | −1.22 | 7.68E-03 | 798.22 |
| NM_030639 | BHLHB9 | Basic helix-loop-helix domain containing, class B, 9 | −1.14 | 7.69E-03 | 798.53 |
| NM_004246 | GLP2R | Glucagon-like peptide 2 receptor | −1.26 | 7.79E-03 | 802.00 |
| NM_032873 | UBASH3B | Ubiquitin-associated and SH3 domain containing B | −1.14 | 7.79E-03 | 802.14 |
| NM_001963 | EGF | Epidermal growth factor | −1.35 | 7.84E-03 | 803.92 |
| NM_052904 | KLHL32 | Kelch-like 32 (Drosophila) | −1.13 | 7.89E-03 | 805.79 |
| NM_006125 | ARHGAP6 | Rho GTPase activating protein 6 | −1.23 | 7.90E-03 | 806.11 |
| NM_032772 | ZNF503 | Zinc finger protein 503 | −1.14 | 7.95E-03 | 807.90 |
| NM_024886 | C10orf95 | Chromosome 10 open reading frame 95 | −1.15 | 7.99E-03 | 809.09 |
| NM_152703 | SAMD9L | Sterile α motif domain containing 9-like | −1.09 | 8.02E-03 | 809.77 |
| NM_032752 | ZNF496 | Zinc finger protein 496 | −1.14 | 8.03E-03 | 810.31 |
| NM_138456 | BATF2 | Basic leucine zipper transcription factor, ATF-like 2 | −1.13 | 8.04E-03 | 810.45 |
| NM_172370 | DAOA | D-amino acid oxidase activator | −1.04 | 8.07E-03 | 811.67 |
| NM_005747 | CELA3A | Chymotrypsin-like elastase family, member 3A | −1.23 | 8.07E-03 | 811.75 |
| NM_033101 | LGALS12 | Lectin, galactoside-binding, soluble, 12 | −1.14 | 8.14E-03 | 813.87 |
| NM_012224 | NEK1 | NIMA (never in mitosis gene a)- related kinase 1 | −1.21 | 8.21E-03 | 816.40 |
| NM_020436 | SALL4 | Sal-like 4 (Drosophila) | −1.19 | 8.31E-03 | 819.74 |
| NM_138980 | MAPK10 | Mitogen-activated protein kinase 10 | −1.13 | 8.34E-03 | 820.62 |
| NM_020896 | OSBPL5 | Oxysterol binding protein-like 5 | −1.18 | 8.41E-03 | 822.84 |
| NM_052897 | MBD6 | Methyl-CpG binding domain protein 6 | −1.14 | 8.52E-03 | 826.04 |
| NM_207419 | C1QTNF8 | C1q and tumor necrosis factor related protein 8 | −0.82 | 8.58E-03 | 827.94 |
| NM_005933 | KMT2A | myeloid/lymphoid or mixed-lineage leukemia (trithorax homolog, Drosophila) | −1.23 | 8.59E-03 | 828.40 |
| NM_181712 | KANK4 | KN motif and ankyrin repeat domains 4 | −0.96 | 8.61E-03 | 828.96 |
| NM_017777 | MKS1 | Meckel syndrome, type 1 | −1.20 | 8.61E-03 | 829.20 |
| NM_176677 | NHLRC4 | NHL repeat containing 4 | −0.99 | 8.67E-03 | 831.05 |
| NM_025130 | HKDC1 | Hexokinase domain containing 1 | −1.14 | 8.71E-03 | 832.53 |
| NM_017654 | SAMD9 | Sterile α motif domain containing 9 | −1.21 | 8.92E-03 | 838.42 |
| NM_052864 | TIFA | TRAF-interacting protein with forkhead-associated domain | −1.14 | 8.94E-03 | 838.99 |
| NM_015569 | DNM3 | Dynamin 3 | −1.21 | 8.95E-03 | 839.17 |
| NM_139047 | Mitogen-activated protein kinase 8 | −1.12 | 8.99E-03 | 840.70 | |
| NM_207173 | NPSR1 | Neuropeptide S receptor 1 | −0.87 | 9.03E-03 | 841.91 |
| NM_015444 | TMEM158 | Transmembrane protein 158 (gene/pseudogene) | −1.21 | 9.03E-03 | 841.90 |
| NM_017523 | XAF1 | XIAP-associated factor 1 | −1.21 | 9.10E-03 | 844.23 |
| NM_006931 | SLC2A3 | Solute carrier family 2 (facilitated glucose transporter), member 3 | −1.22 | 9.11E-03 | 844.45 |
| NM_019018 | FAM105A | Family with sequence similarity 105, member A | −1.19 | 9.13E-03 | 845.15 |
| NM_153042 | KDM1B | Lysine (K)-specific demethylase 1B | −1.08 | 9.18E-03 | 846.40 |
| NM_033056 | PCDH15 | Protocadherin-related 15 | −1.14 | 9.23E-03 | 848.31 |
| NM_014157 | CCDC113 | Coiled-coil domain containing 113 | −1.21 | 9.25E-03 | 848.53 |
| NM_144962 | PEBP4 | Phosphatidylethanolamine-binding protein 4 | −1.12 | 9.31E-03 | 850.61 |
| NM_145862 | CHEK2 | Checkpoint kinase 2 | −1.09 | 9.36E-03 | 852.29 |
| NM_182524 | ZNF595 | Zinc finger protein 595 | −0.93 | 9.41E-03 | 853.59 |
| NM_014858 | TMCC2 | Transmembrane and coiled-coil domain family 2 | −1.21 | 9.46E-03 | 855.35 |
| NM_144990 | SLFNL1 | Schlafen-like 1 | −1.11 | 9.47E-03 | 855.60 |
| NM_022147 | RTP4 | Receptor (chemosensory) transporter protein 4 | −1.16 | 9.49E-03 | 856.25 |
| NM_022873 | IFI6 | Interferon, α-inducible protein 6 | −1.16 | 9.73E-03 | 863.03 |
| NM_152685 | SLC23A1 | Solute carrier family 23 (nucleobase transporters), member 1 | −1.09 | 9.73E-03 | 863.10 |
| NM_152278 | TCEAL7 | Transcription elongation factor A (SII)-like 7 | −1.09 | 9.84E-03 | 866.45 |
| NM_019035 | PCDH18 | Protocadherin 18 | −1.19 | 9.95E-03 | 869.75 |
| NM_153183 | NUDT10 | Nudix (nucleoside diphosphate linked moiety X)-type motif 10 | −1.07 | 9.99E-03 | 870.83 |
Table III.
Significant functional categories of upregulated and downregulated genes.
| A, Upregulated genes | ||||
|---|---|---|---|---|
| P-value | Bonferroni | Benjamini | FDR | |
| GO category | ||||
| Cell fate commitment | 7.2E-07 | 8.9E-04 | 8.9E-04 | 1.2E-03 |
| Negative regulation of cell differentiation | 2.9E-05 | 3.5E-02 | 1.2E-02 | 4.7E-02 |
| Differentiation | 6.8E-05 | 1.7E-02 | 1.7E-02 | 8.8E-02 |
| Developmental protein | 9.2E-05 | 2.4E-02 | 1.2E-02 | 1.2E-01 |
| Notch signaling pathway | 1.0E-04 | 2.6E-02 | 8.7E-03 | 1.3E-01 |
| Intestine | 2.4E-04 | 6.0E-02 | 1.5E-02 | 3.1E-01 |
| KEGG pathway | ||||
| Notch signaling pathway | 3.5E-05 | 2.7E-03 | 2.7E-03 | 3.7E-02 |
| B, Downregulated genes | ||||
| GO category | ||||
| Regulation of cell death | 5.9E-07 | 9.2E-04 | 4.6E-04 | 9.8E-04 |
| Regulation of cell proliferation | 1.8E-04 | 2.4E-01 | 1.9E-02 | 2.9E-01 |
| Regulation of cell migration | 2.0E-04 | 2.7E-01 | 1.9E-02 | 3.3E-01 |
| KEGG pathway | ||||
| Pathways in cancer | 1.9E-04 | 1.6E-02 | 1.6E-02 | 2.1E-01 |
GO, Gene Ontology; KEGG, Kyoto Encyclopedia of Genes and Genomes; FDR, false discovery rate.
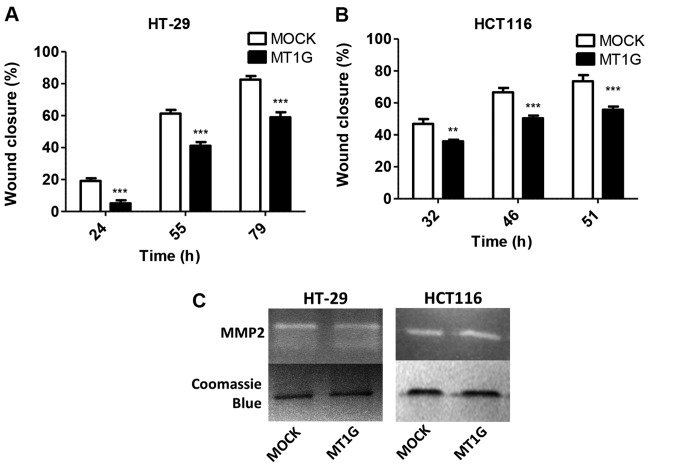
Given the finding of downregulated genes in the cell migration category, we performed migration ‘scratch’ assays in the HT-29 and HCT116 cell lines overexpressing MT1G, and found in both cell lines a statistically significant reduction in migration rates upon MT1G overexpression (Fig. 2A and B). Gelatin zymography using conditioned media from these cells, however, revealed no differences in MMP2 activity (Fig. 2C).
Figure 2.
Wound healing ‘scratch’ assays in (A) HT-29 and (B) HCT116 MT1G+ cells showing decreased migration capacity, but no difference in MMP2 activity as measured by (C) gelatin zymography; *p<0.05, **p<0.01 and ***p<0.001.
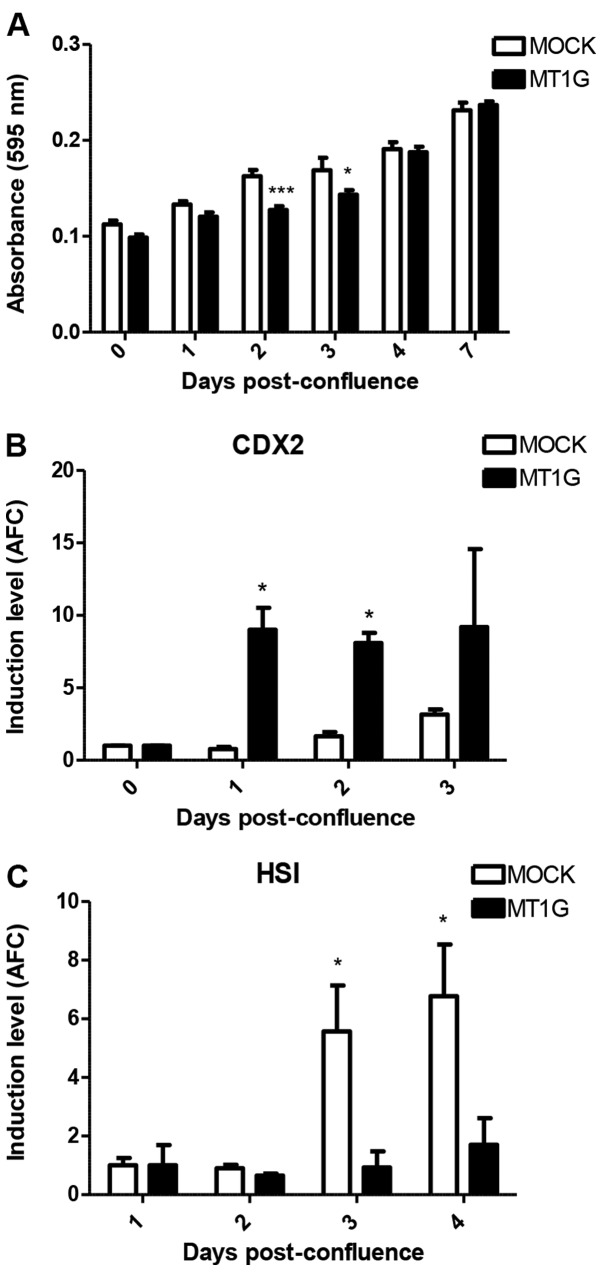
Next, in order to further investigate the involvement of MT1G in the differentiation of HT-29 cells, we used two different and well-known cell culture conditions to stimulate the in vitro differentiation of these cells: sodium butyrate (BUT) treatment (19) and post-confluent cell growth (20). We used TFF3 and MUC2 mRNA expression as surrogate markers for the goblet cell lineage, and HSI and CA1 mRNAs, along with enzymatic alkaline-phosphatase activity (ALP) for enterocytes.
Involvement of MT1G in butyrate-mediated differentiation of HT-29 cells
Sodium butyrate is a well-known inducer of differentiation in CRC cell lines (21), and indeed, as shown in Fig. 3A, treatment with this agent dose-dependently induced differentiation as assessed by ALP activity. Concordantly, this agent also induced MT1G and MT2A mRNA levels, in close correlation to ALP activity (Pearson r=0.993, p=0.007 for MT1G and r=0.999, p=0.0006 for MT2A; Fig. 3B). To determine whether the induction of MTs has a functional role in butyrate-induced differentiation, we used siRNAs to inhibit the induction of only MT1G (si1G.1 and si1G.2) or of all MT1 and MT2 isoforms (siMTs), as previously described (12). Fig. 3C shows that siRNA pre-treatment partially mitigated MT1G induction after BUT treatment and markedly, also diminished the induction of CDX2 (Fig. 3D), and of goblet-cell marker TFF3 (Fig. 3E). Notably, BUT treatment had no effect on mRNA levels of MUC2, as has been previously reported by others (17) (data not shown). In contrast, although the enterocyte-specific markers HSI and CA1 were markedly upregulated at 2 mM BUT, silencing of MTs had no effect on their induction (Fig. 3F and G), or on the cell-cycle arrest mediator CDKN1A/p21 (data not shown), whereas ALP activity was only slightly, but significantly reduced (Fig. 3H).
Figure 3.
Butyrate mediates the differentiation of HT-29 cells. (A) Assessment of ALP enzymatic activity, 72 h after treatment. (B) Induction of MT1G and MT2A mRNA expression measured by qRT-PCR 72 h after treatment. (C-G) Expression of MT1G, CDX2, TFF3, HSI and CA1 as well as (H) ALP activity after siRNA-mediated silencing of MT1G or all MTs. AFC, average fold-change; *p<0.05, **p<0.01 and ***p<0.001.
We next treated HT-29 MOCK and MT1G+ cells with butyrate. Notably, as depicted in Fig. 4A, whereas CDX2 mRNA levels were similarly induced, MT1G overexpression markedly enhanced the induction of TFF3 (Fig. 4B), whereas it blunted that of HSI (Fig. 4C). Therefore, both silencing and overexpression of MT1G support the hypothesis that this gene favors goblet over enterocyte differentiation upon butyrate treatment of HT-29 cells.
Figure 4.
(A) CDX2, (B) TFF3 and (C) HSI expression in MOCK and MT1G+ cells upon butyrate treatment. AFC, average fold-change; *p<0.05, **p<0.01 and ***p<0.001.
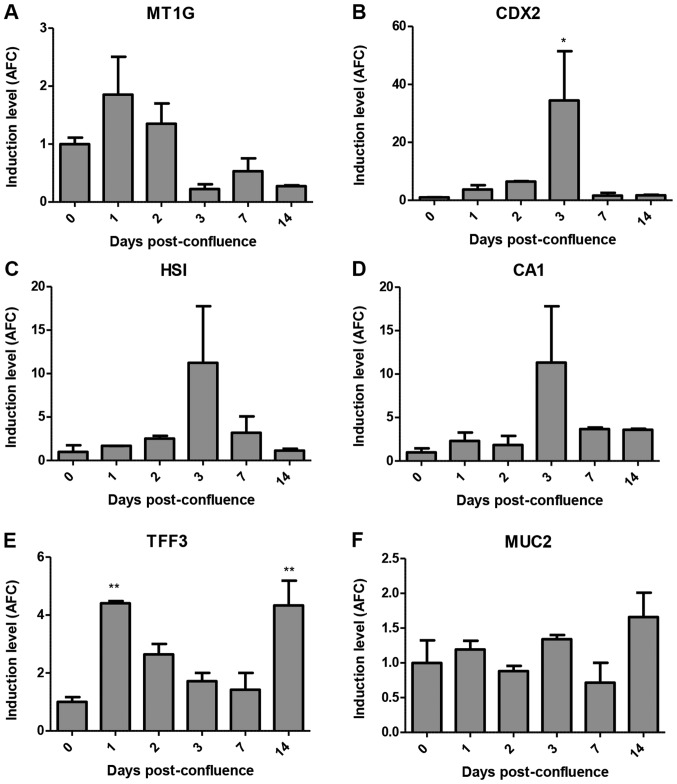
Involvement of MT1G in post-confluent differentiation of HT-29 cells
Next, we studied the expression of MT1G in the post-confluent growth of HT-29 cells, where this cell line is known to differentiate poorly (20). In this setting, MT1G mRNA was transiently induced at day 1 post-confluence, after which its expression was significantly reduced (Fig. 5A). In contrast, CDX2 and enterocyte-specific genes HSI and CA1 were transiently induced at day 3, two days after MT1G induction (Fig. 5B-D). Notably, TFF3 expression mirrors MT1G expression, until day 14 when it is induced again (Fig. 5E). These time-course analyses again favored the association of MT1G induction with goblet over enterocyte differentiation. Notably, as with BUT treatment, MUC2 expression was not altered in this context (Fig. 5F). We were unable to perform siRNA-mediated silencing of MT1G in this setting, as cells did not survive in a totally confluent state for >1 day after transfection.
Figure 5.
Expression of (A) MT1G, (B) CDX2, (C) HIS, (D) CA1, (E) TFF3 and (F) MUC2 upon differentiation stimulated by post-confluent growth of HT-29 cells. AFC, average fold-change; *p<0.05, **p<0.01 and ***p<0.001.
When growing HT-29 MOCK and MT1G+ cells post-confluence, we noted no difference in the induction of ALP activity between these two cell lines (Fig. 6A). Notably however, in the latter, CDX2 mRNA was induced at significantly higher levels (Fig. 6B) whereas HSI induction was abolished (Fig. 6C). While we noted no differences in the induction of TFF3 mRNA (data not shown), our data also implies a role for MT1G expression in counteracting enterocyte differentiation of HT-29 cells.
Figure 6.
Effects of stable MT1G expression on post-confluent growth of HT-29 cells. (A) ALP activity. (B) CDX2 and (C) HSI expression. AFC, average fold-change; *p<0.05, **p<0.01 and ***p<0.001.
Labile zinc levels in butyrate-treated and post-confluent HT-29 cells
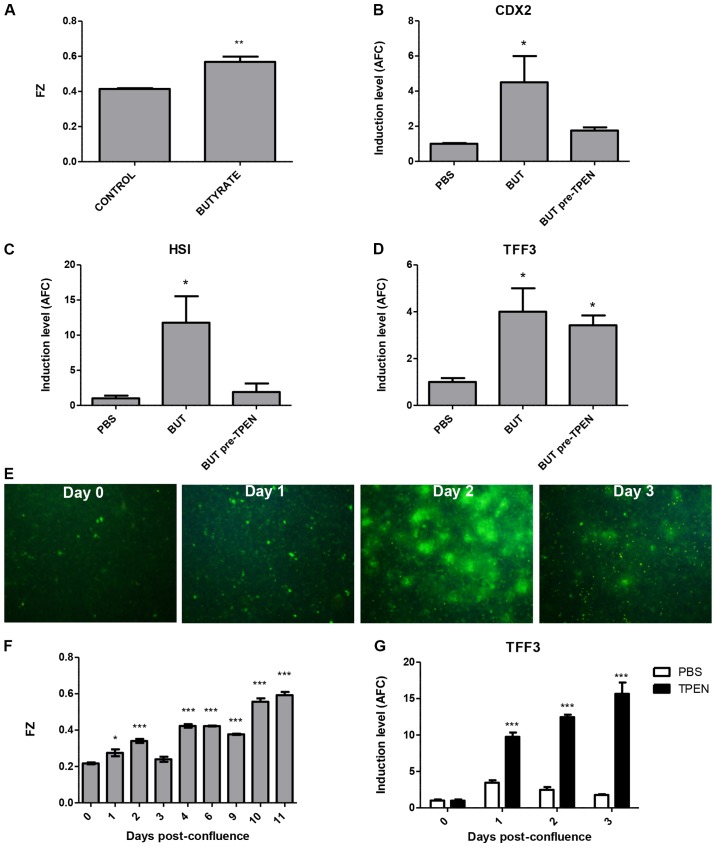
Given the close relationship between MTs and zinc biology, we analyzed the levels of intracellular labile zinc in both models of differentiation, using the zinc-specific fluorophore FZ. Notably, after 72 h of 2 mM BUT treatment, FZ intensity was significantly induced in the HT-29 cells (Fig. 7A). We used TPEN treatment to chelate intracellular labile zinc before the addition of butyrate, and found that this abolished both CDX2 and HSI mRNA induction (Fig. 7B and C), but had no effect on TFF3 levels (Fig. 7D). In the post-confluence model, as shown by fluorescence microscopy in Fig. 7E and by fluorimetry in Fig. 7F, FZ intensity was induced at day 2 and progressively increased thereafter. Given that TPEN exposure for >6 h is toxic to HT-29 cells, we used daily 5-h TPEN treatments to evaluate the effect of labile zinc on goblet and enterocyte markers. Notably, TFF3 mRNA expression was significantly induced at days 1–3 post-confluence in TPEN-treated cells (Fig. 7G), whereas there was no effect on either CDX2 or HSI levels (not shown).
Figure 7.
Labile zinc induction upon differentiation. (A) Butyrate induces intracellular labile zinc levels in HT-29 cells, as measured by fluorimetry using the Fluozin-3AM (FZ) probe. (B and C) Both CDX2 and HSI induction by butyrate are blunted by TPEN pre-treatment, whereas there is no effect on (D) TFF3 expression. (E and F) Labile zinc levels are also increased in the post-confluency differentiation model of HT-29 cells, as measured by (E) epifluorescence microscopy (F) and fluorimetry. (G) Daily doses of TPEN stimulate TFF3 expression of post-confluent cultures. AFC, average fold-change; *p<0.05, **p<0.01 and ***p<0.001.
In summary, labile zinc was induced in both models of intestinal differentiation, and its chelation by TPEN treatment either inhibited enterocyte differentiation (butyrate model) or induced the expression of goblet-cell markers (post-confluency model).
Discussion
In the present study, we uncovered a new role for MT1G in altering the differentiation properties of the HT-29 cell line. We previously showed that induction of MTs by HDACi agents such as trichostatin A and sodium butyrate (BUT) is at least partly responsible for their cytostatic effects on human CRC cell lines, and that exogenous MT1G overexpression in the colorectal HCT116 cell line resulted in growth inhibition in nude mouse xenografts (12). Notably, whereas MT1G overexpression did not alter the in vivo xenograft growth rate of HT-29 cells, it markedly increased the number of goblet cells and differentiation markers of these tumors, both of the goblet and the enterocyte lineages. These effects were not readily observed in 2D culture (data not shown), suggesting that additional signals from the tumor microenvironment may be needed to fulfill this effect. The reasons for the different observed phenotypic consequences of MT1G overexpression in these two cell lines are unclear, but a possible explanation may stem from the differences in endogenous MT1G expression: HCT116 cells do not express MT1G due to promoter hypermethylation and therefore the impact of MT1G overexpression may be stronger than that in HT-29 cells, which express low, but detectable mRNA levels (8).
In an effort to understand the molecular mechanisms underlying the altered differentiation of MT1G+ tumors, we performed mRNA expression profiling by cDNA microarrays. The expression of several genes involved in the regulation of cell differentiation was found to be altered, particularly in the Notch signaling pathway, whose inhibition is well known to stimulate goblet cell differentiation in the intestine through activation of ATOH1 (22). Notably, markers of different sets of intestinal stem cell markers were differentially dysregulated in MT1G+ tumors, with upregulation of HOPX (expressed in quiescent stem cells) and downregulation of Lgr5 (in crypt base columnar stem cells), again suggesting altered differentiation hierarchies (23,24). Further studies are warranted to explore this in further detail.
To further characterize the involvement of MT1G in colorectal differentiation, we relied on two well-studied cell culture conditions: sodium butyrate and post-confluent growth. We showed that endogenous MT1G induction was required for the induction of goblet cell markers by butyrate, and was temporally associated with such markers in the confluency model. Moreover, stable exogenous MT1G overexpression favored goblet and blunted enterocyte differentiation in both models. Previous studies have shown MTs to be upregulated in vitro upon CRC differentiation (25), and demonstrated a role for MTs in modulating differentiation in different tissues, such as human salivary gland tumor cells (where MT1F overexpression resulted in slower growing and more differentiated tumors) (26), leukemic (27) neurons and glial (28), and T cells (29). However, to the best of our knowledge, this is the first study showing a direct functional involvement of a metallothionein isoform in CRC differentiation.
Labile zinc ions have been recognized as secondary messengers capable of transducing a wide variety of intracellular signals (30,31), including differentiation (32–34). MTs can regulate labile zinc concentrations and zinc transfer to different cellular organelles (35), as well as respond to changes in intracellular zinc ions (36). We showed in the present study that labile zinc was increased during differentiation induced both by butyrate and confluency, and that this was required for enterocyte differentiation by butyrate, whereas it blunted goblet marker induction in post-confluency. While the reason behind the differences observed in both models are unclear, the overall effects of zinc induction favor an enterocyte over goblet differentiation. Notably, although labile zinc increases have already been reported to occur during butyrate-mediated differentiation of the HT-29 cell line and have been associated to defined stages of the cell cycle (37), in the present study, we reported for the first time a functional consequence of labile zinc induction in this process. Previous studies in other tissues have shown that MTs transiently translocate to the nucleus during early phases of differentiation to release the zinc ions necessary for zinc-dependent transcription factors to execute the differentiation programs of adipocytes and myoblasts (38,39). Although we previously showed that MTs in HT-29 are localized to the cytoplasm (8), we were not able to detect a nuclear shift in either of the differentiation models that we used in the present study (data not shown), although this possibility should be studied in further detail.
Taking into account our results, we hypothesize that MT1G induction during differentiation may play a role in the chelation and re-distribution of intracellular labile zinc, perhaps modulating the activity of zinc-requiring transcription factors and enzymes, and stimulating the differentiation program of colorectal cells. In vitro, our results showed that MT1G favors a goblet over enterocyte differentiation, although our mouse xenografts assays suggest that in vivo the differentiation into enterocytes is also stimulated, perhaps as a compensatory mechanism or in a non-cell autonomous manner. The precise mechanisms whereby this occurs and the participation of MT1G (and other MTs) in labile zinc redistribution during differentiation need to be studied in further detail. Moreover, tumor classifications based on gene signatures associated with different cell types suggest that tumors of the more differentiated ‘goblet-’ or ‘enterocyte-like’ subtypes have a better prognosis than undifferentiated ‘stem-like’ subtype, as well as different responses to therapeutic agents. Therefore, better understanding of the molecular mechanisms that govern the differentiation processes of tumor cells may be of clinical relevance.
Overall, in the present study, we unveiled a pro-differentiation effect of MT1G on various CRC cells, thus proposing a new mechanism whereby MT1G may act as a tumor suppressor in this tumor type. Moreover, we established a functional consequence of transient increases in labile zinc upon differentiation stimuli, and support the need of further studies relating zinc signaling and differentiation, that may ultimately underlie tumor cell phenotypes and response to therapies.
Acknowledgements
The present study was funded by the Consejo Nacional de Investigaciones Científicas y Técnicas (CONICET) (PIP no. 845-10 to M.B.), the Agencia Nacional de Promoción Científica y Tecnológica (ANPCyT) (IP-PAE 2007, to J.M.), the Fundación Cáncer, the Fundación P. Mosoteguy, the Fundación Sales, and the Fundación María Calderón de la Barca, Buenos Aires, Argentina.
Glossary
Abbreviations
- BUT
sodium butyrate
- CRC
colorectal cancer
- FZ
fluozin 3-AM
- MMPs
matrix metalloproteinases
- TPEN
N,N,N',N'-tetrakis(2-pyridylmethyl) ethylenediamine
- MTs
metallothioneins
References
- 1.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 2.Dalerba P, Kalisky T, Sahoo D, Rajendran PS, Rothenberg ME, Leyrat AA, Sim S, Okamoto J, Johnston DM, Qian D, et al. Single-cell dissection of transcriptional heterogeneity in human colon tumors. Nat Biotechnol. 2011;29:1120–1127. doi: 10.1038/nbt.2038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sadanandam A, Lyssiotis CA, Homicsko K, Collisson EA, Gibb WJ, Wullschleger S, Ostos LC, Lannon WA, Grotzinger C, Del Rio M, et al. A colorectal cancer classification system that associates cellular phenotype and responses to therapy. Nat Med. 2013;19:619–625. doi: 10.1038/nm.3175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pedersen MO, Larsen A, Stoltenberg M, Penkowa M. The role of metallothionein in oncogenesis and cancer prognosis. Prog Histochem Cytochem. 2009;44:29–64. doi: 10.1016/j.proghi.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 5.Eckschlager T, Adam V, Hrabeta J, Figova K, Kizek R. Metallothioneins and cancer. Curr Protein Pept Sci. 2009;10:360–375. doi: 10.2174/138920309788922243. [DOI] [PubMed] [Google Scholar]
- 6.Dziegiel P, Pula B, Kobierzycki C, Stasiolek M, Podhorska-Okolow M. Metallothioneins in normal and cancer cells. Adv Anat Embryol Cell Biol. 2016;218:1–117. doi: 10.1007/978-3-319-27472-0_1. [DOI] [PubMed] [Google Scholar]
- 7.Gumulec J, Raudenska M, Adam V, Kizek R, Masarik M. Metallothionein - immunohistochemical cancer biomarker: A meta-analysis. PLoS One. 2014;9:e85346. doi: 10.1371/journal.pone.0085346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arriaga JM, Levy EM, Bravo AI, Bayo SM, Amat M, Aris M, Hannois A, Bruno L, Roberti MP, Loria FS, et al. Metallothionein expression in colorectal cancer: Relevance of different isoforms for tumor progression and patient survival. Hum Pathol. 2012;43:197–208. doi: 10.1016/j.humpath.2011.04.015. [DOI] [PubMed] [Google Scholar]
- 9.Arriaga JM, Bravo IA, Bruno L, Bayo Morales S, Hannois A, Sanchez Loria F, Pairola F, Huertas E, Roberti MP, Rocca YS, et al. Combined metallothioneins and p53 proteins expression as a prognostic marker in patients with Dukes stage B and C colorectal cancer. Hum Pathol. 2012;43:1695–1703. doi: 10.1016/j.humpath.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 10.Janssen AM, van Duijn W, Oostendorp-Van De Ruit MM, Kruidenier L, Bosman CB, Griffioen G, Lamers CB, van Krieken JH, van De Velde CJ, Verspaget HW. Metallothionein in human gastrointestinal cancer. J Pathol. 2000;192:293–300. doi: 10.1002/1096-9896(2000)9999:9999<::AID-PATH712>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 11.Bianchini M, Levy E, Zucchini C, Pinski V, Macagno C, De Sanctis P, Valvassori L, Carinci P, Mordoh J. Comparative study of gene expression by cDNA microarray in human colorectal cancer tissues and normal mucosa. Int J Oncol. 2006;29:83–94. [PubMed] [Google Scholar]
- 12.Arriaga JM, Greco A, Mordoh J, Bianchini M. Metallothionein 1G and zinc sensitize human colorectal cancer cells to chemotherapy. Mol Cancer Ther. 2014;13:1369–1381. doi: 10.1158/1535-7163.MCT-13-0944. [DOI] [PubMed] [Google Scholar]
- 13.Cleveland WS, Devlin SJ, Grosse E. Regression by local fitting: Methods, properties, and computational algorithm. J Econom. 1988;37:87–114. doi: 10.1016/0304-4076(88)90077-2. [DOI] [Google Scholar]
- 14.Yang YH, Dudoit S, Luu P, Lin DM, Peng V, Ngai J, Speed TP. Normalization for cDNA microarray data: A robust composite method addressing single and multiple slide systematic variation. Nucleic Acids Res. 2002;30:e15. doi: 10.1093/nar/30.4.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dennis G, Jr, Sherman BT, Hosack DA, Yang J, Gao W, Lane HC, Lempicki RA. DAVID: Database for Annotation, Visualization, and Integrated Discovery. Genome Biol. 2003;4:3. doi: 10.1186/gb-2003-4-9-r60. [DOI] [PubMed] [Google Scholar]
- 16.Huang W, Sherman BT, Lempicki RA. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat Protoc. 2009;4:44–57. doi: 10.1038/nprot.2008.211. [DOI] [PubMed] [Google Scholar]
- 17.Velcich A, Palumbo L, Jarry A, Laboisse C, Racevskis J, Augenlicht L. Patterns of expression of lineage-specific markers during the in vitro-induced differentiation of HT29 colon carcinoma cells. Cell Growth Differ. 1995;6:749–757. [PubMed] [Google Scholar]
- 18.Troeberg L, Nagase H. Zymography of metalloproteinases. Curr Protoc Protein Sci. 2004;21 doi: 10.1002/0471140864.ps2115s33. Unit 21.15. [DOI] [PubMed] [Google Scholar]
- 19.Augeron C, Laboisse CL. Emergence of permanently differentiated cell clones in a human colonic cancer cell line in culture after treatment with sodium butyrate. Cancer Res. 1984;44:3961–3969. [PubMed] [Google Scholar]
- 20.Zweibaum A, Pinto M, Chevalier G, Dussaulx E, Triadou N, Lacroix B, Haffen K, Brun JL, Rousset M. Enterocytic differentiation of a subpopulation of the human colon tumor cell line HT-29 selected for growth in sugar-free medium and its inhibition by glucose. J Cell Physiol. 1985;122:21–29. doi: 10.1002/jcp.1041220105. [DOI] [PubMed] [Google Scholar]
- 21.Chung YS, Song IS, Erickson RH, Sleisenger MH, Kim YS. Effect of growth and sodium butyrate on brush border membrane-associated hydrolases in human colorectal cancer cell lines. Cancer Res. 1985;45:2976–2982. [PubMed] [Google Scholar]
- 22.VanDussen KL, Carulli AJ, Keeley TM, Patel SR, Puthoff BJ, Magness ST, Tran IT, Maillard I, Siebel C, Kolterud Å, et al. Notch signaling modulates proliferation and differentiation of intestinal crypt base columnar stem cells. Development. 2012;139:488–497. doi: 10.1242/dev.070763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barker N, Ridgway RA, van Es JH, van de Wetering M, Begthel H, van den Born M, Danenberg E, Clarke AR, Sansom OJ, Clevers H. Crypt stem cells as the cells-of-origin of intestinal cancer. Nature. 2009;457:608–611. doi: 10.1038/nature07602. [DOI] [PubMed] [Google Scholar]
- 24.Takeda N, Jain R, LeBoeuf MR, Wang Q, Lu MM, Epstein JA. Interconversion between intestinal stem cell populations in distinct niches. Science. 2011;334:1420–1424. doi: 10.1126/science.1213214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vecchini F, Pringault E, Billiar TR, Geller DA, Hausel P, Felley-Bosco E. Decreased activity of inducible nitric oxide synthase type 2 and modulation of the expression of glutathione S-transferase α, bcl-2, and metallothioneins during the differentiation of CaCo-2 cells. Cell Growth Differ. 1997;8:261–268. [PubMed] [Google Scholar]
- 26.Hecht D, Jung D, Prabhu VV, Munson PJ, Hoffman MP, Kleinman HK. Metallothionein promotes laminin-1-induced acinar differentiation in vitro and reduces tumor growth in vivo. Cancer Res. 2002;62:5370–5374. [PubMed] [Google Scholar]
- 27.Bagheri Maghdooni P, Govaerts I, De Ley M. Role of metallothionein in differentiation of leukemia cells. Mol Biol Rep. 2011;38:3017–3022. doi: 10.1007/s11033-010-9967-7. [DOI] [PubMed] [Google Scholar]
- 28.Nishikawa M, Mori H, Hara M. Reduced zinc cytotoxicity following differentiation of neural stem/progenitor cells into neurons and glial cells is associated with upregulation of metallothioneins. Environ Toxicol Pharmacol. 2015;39:1170–1176. doi: 10.1016/j.etap.2015.04.009. [DOI] [PubMed] [Google Scholar]
- 29.Wu C, Pot C, Apetoh L, Thalhamer T, Zhu B, Murugaiyan G, Xiao S, Lee Y, Rangachari M, Yosef N, et al. Metallothioneins negatively regulate IL-27-induced type 1 regulatory T cell differentiation. Proc Natl Acad Sci USA. 2013;110:7802–7807. doi: 10.1073/pnas.1211776110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Murakami M, Hirano T. Intracellular zinc homeostasis and zinc signaling. Cancer Sci. 2008;99:1515–1522. doi: 10.1111/j.1349-7006.2008.00854.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yamasaki S, Sakata-Sogawa K, Hasegawa A, Suzuki T, Kabu K, Sato E, Kurosaki T, Yamashita S, Tokunaga M, Nishida K, et al. Zinc is a novel intracellular second messenger. J Cell Biol. 2007;177:637–645. doi: 10.1083/jcb.200702081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Beyersmann D, Haase H. Functions of zinc in signaling, proliferation and differentiation of mammalian cells. Biometals. 2001;14:331–341. doi: 10.1023/A:1012905406548. [DOI] [PubMed] [Google Scholar]
- 33.Dubben S, Hönscheid A, Winkler K, Rink L, Haase H. Cellular zinc homeostasis is a regulator in monocyte differentiation of HL-60 cells by 1 alpha,25-dihydroxyvitamin D3. J Leukoc Biol. 2010;87:833–844. doi: 10.1189/jlb.0409241. [DOI] [PubMed] [Google Scholar]
- 34.Wolford JL, Chishti Y, Jin Q, Ward J, Chen L, Vogt S, Finney L. Loss of pluripotency in human embryonic stem cells directly correlates with an increase in nuclear zinc. PLoS One. 2010;5:e12308. doi: 10.1371/journal.pone.0012308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maret W. Metals on the move: Zinc ions in cellular regulation and in the coordination dynamics of zinc proteins. Biometals. 2011;24:411–418. doi: 10.1007/s10534-010-9406-1. [DOI] [PubMed] [Google Scholar]
- 36.Kindermann B, Döring F, Pfaffl M, Daniel H. Identification of genes responsive to intracellular zinc depletion in the human colon adenocarcinoma cell line HT-29. J Nutr. 2004;134:57–62. doi: 10.1093/jn/134.1.57. [DOI] [PubMed] [Google Scholar]
- 37.Krezel A, Maret W. Zinc-buffering capacity of a eukaryotic cell at physiological pZn. J Biol Inorg Chem. 2006;11:1049–1062. doi: 10.1007/s00775-006-0150-5. [DOI] [PubMed] [Google Scholar]
- 38.Schmidt C, Beyersmann D. Transient peaks in zinc and metallothionein levels during differentiation of 3T3L1 cells. Arch Biochem Biophys. 1999;364:91–98. doi: 10.1006/abbi.1999.1107. [DOI] [PubMed] [Google Scholar]
- 39.Apostolova MD, Ivanova IA, Cherian MG. Metallothionein and apoptosis during differentiation of myoblasts to myotubes: Protection against free radical toxicity. Toxicol Appl Pharmacol. 1999;159:175–184. doi: 10.1006/taap.1999.8755. [DOI] [PubMed] [Google Scholar]