Abstract
Aim:
This study aimed to assess the effect of petroleum ether extract (PEE), ethyl acetate extract (EthE), and ethanol extract (EAE) of Trichilia monadelpha stem bark on bone histomorphology in arthritis.
Methods:
Percentage inhibition of edema and arthritic scores in complete Freund’s adjuvant-induced (0.1 ml of 5 mg/ml1 of heat-killed Mycobacterium tuberculosis in paraffin oil-injected subplantar into the right hind paw) arthritic Sprague-Dawley rats treated with PEE, EthE, or EAE (10,30, and 100 mg/kg1, respectively), dexamethasone (0.3-3.0 mg/kg1), or methotrexate (0.1-1.0 mg/kg1) over a 28-day period were estimated. Rat paws were radiographed and scored. Body weights were taken and paw tissues were harvested for histopathological studies.
Results:
The extracts significantly (P ≤ 0.01-0.0001) and dose dependently reduced the polyarthritic phase of arthritis. EAE and PEE significantly (P ≤ 0.01-0.0001) minimized edema spread from acute arthritic phase (days 0-10) to polyarthritic phase (days 10-28). EthE improved which deteriorated body weight in arthritis. All extracts significantly (P ≤ 0.05-0.01) improved arthritic score; reducing erythema, swelling and joint rigidity, and also significantly (P ≤ 0.05-0.01) reduced hyperplasia, pannus formation, and exudation of inflammatory cells into synovial spaces.
Conclusion:
The stem bark extracts of T. monadelpha reduce bone tissue damage and resorption associated with adjuvant-induced arthritis, hence could be useful in managing arthritis in humans.
KEY WORDS: Arthritic paw radiography, erythema, subchondral erosion, periostitis, osteolysis, Trichilia monadelpha
INTRODUCTION
Rheumatoid arthritis (RA) is a chronic inflammatory autoimmune disease of the joints that leads to changes in bone metabolism [1]. The primary target of this inflammatory disease is the synovial membrane of the joints. RA leads to cartilage and bone erosion and joint deformity; manifesting signs and symptoms such as pain, swelling and redness, and fatigue [2]. It can affect other organs of the body resulting in disability and mortality [3]. Globally, RA affects about 1% of adult population [4] and poses a heavy economic burden with disease progression [5].
Non-steroidal anti-inflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs), corticosteroids, and cytokine-targeted drugs have been used to manage RA [6,7]. These drugs target specifically at reducing inflammation and relieving pain by blocking cyclooxygenase-mediated prostaglandins release (i.e, the NSAIDs) and control of joint inflammation by suppressing inflammatory-induced bone erosion (glucocorticoids and DMARDs) [8,9]. However, these drugs are associated with undesirable side effects such as gastric ulceration and precipitation of asthma and renal disease and are unaffordable to a lot of individuals [10], hence this search for natural products that are efficacious, but with less side effects, and affordable to the majority of the populace. Trichilia monadelpha (Meliaceae), one such plant, has been used trado-medically to manage chronic inflammatory diseases for decades [11,12]. The stem bark has anti-inflammatory [13] and analgesic effects [13,14]. It improves sperm viability [15] and is relatively non-toxic [13]. Phytochemical analysis conducted revealed the presence of alkaloids, terpenoids, phytosterols, coumarins, tannins, cardiac glycosides, anthraquinones, saponins, flavonoids, and reducing sugars in the petroleum ether, ethyl acetate, and hydroethanolic extracts [13,16].
This study, therefore, assesses the effects of petroleum ether extract (PEE), ethyl acetate extract (EthE), and ethanol extract (EAE) of T. monadelpha stem bark in complete Freund’s adjuvant (CFA)-induced arthritis in Sprague-Dawley rats.
MATERIALS AND METHODS
Experimental Animals
Male Sprague-Dawley rats (150-200 g) obtained from Noguchi Memorial Institute for Medical Research, University of Ghana, Legon, were kept in the animal house of the Department of Pharmacology, KNUST, Kumasi, Ghana. Animals were housed in aluminum cages and given normal rat diet (Agricare Ltd., Tanoso, Kumasi) and water to consume ad libitum. Rats were kept according to the National Institute of Health Guidelines for the Care and Use of Laboratory Animals (NIH, Department of Health and Human Services publication no. 85-23, revised 1985). The study was approved by the Institutional Review Board on animal experimentation.
Extract Preparation and Dosing
A voucher specimen of extraction of the stem bark of T. monadelpha was kept in the herbarium, Faculty of Pharmacy (No. FP/079/10) as described by Ben et al., 2013 [16]. The PEE, EthE, and EAEs were each triturated with Tween-80 (3 drops) in normal saline and administered orally to rats at doses ranging from 10 to 100 mg/kg1.
Drugs and Chemicals used
Heat-killed Mycobacterium tuberculosis, mixed strains C, DT, and PN (Ministry of Agriculture, Fisheries and Food, U.K) were used to induce arthritis. Dexamethasone (DEX) (Wuhan Grand, China) and methotrexate (MET) (Dabur Pharma, India) were the reference drugs used for the treatment of arthritis.
CFA-induced Arthritis
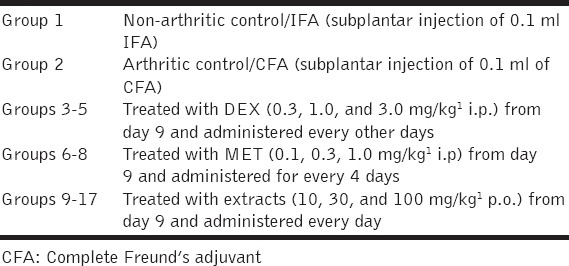
Adjuvant arthritis was induced as previously described by Pearson, 1956 [17], with modification according to Woode et al., 2008 [18]. In brief, rats were assigned to 17 groups (n=8) and injected with a 0.1 ml suspension of CFA (5 mg/ml1 of heat-killed M. tuberculosis in paraffin oil) into the right hind paw. Arthritic control group received only subplantar injection of CFA, while non-arthritic control/incomplete Freund’s Adjuvant (IFA) group received only subplantar injection of 0.1 ml IFA (sterile paraffin oil). PEE, EthE, or EAE (10, 30, and 100 mg/kg1 p.o.), DEX (0.3-3.0 mg/kg1 i.p.) or MET (0.1-1.0 mg/kg1 i.p.,) were administered to rats in the various groups, respectively, after establishment of arthritis, i.e., on day 10 [Table 1].
Table 1.
Experimental grouping and treatment in adjuvant-induced arthritis
Ipsilateral (injected) and contralateral (non-injected) paw volumes were measured using a water displacement plethysmometer (IITC Life Science Equipment, Woodland Hills, USA). This was before subplantar injection of CFA (day 0) and every other day for 28 days after subplantar injection of CFA and IFA. Data obtained for ipsilateral and contralateral paw volumes were individually recorded as percentage of change from their values at day 0 and then averaged for each treatment group. These were presented as the effect of drugs on the time course and the total edema response of adjuvant-induced arthritis for the 28-day period. Total paw volume for each treatment was calculated in arbitrary unit as area under the curve (AUC) to determine the percentage inhibition as per the formula below:

The initial body weight and arthritic score of rats were taken on day 0 after grouping and every other day for 28 days of the experiment, followed by subplantar injection of 0.1 ml CFA. Radiographic images of the paws were taken. Paw tissues were harvested after the 28th day for histopathological assessment.
Body Weight and Arthritic Score
Body weight and arthritic scores were recorded for each hind joint and the tail by a consistent observer blinded to the treatment received by the animals. Scoring was performed on a 0-5 scale [Table 2].
Table 2.
Description and scoring of induced arthritis in Sprague-Dawley rats

X-ray Radiography
On day 28, the animals were anesthetized by intraperitoneal injection of 20 mg/kg1 pentobarbitone. Radiographic images of the hind limbs were taken using a Faxitron X-ray machine (Hewlett-Packard, Buffalo Grove, IL) with a 0.5 mm focal spot, beryllium window, and X OMAT TL (onscreen) film. The focal film distance was 61 cm, and exposures were made over 30 s at 45 kVp and 3 mA. Radiographs were analyzed by a board-certified radiologist who was blinded to the treatment groups. Quantitative scores were generated for radiographic changes in the joints in the following areas: Soft tissue volume, joint space, subchondral erosion, periostitis, osteolysis, subluxation, and degenerative joint changes. The values were based on increasing severity of demineralization [Table 3].
Table 3.
Mode of scoring of radiographs for arthritic paws of Sprague-Dawley rats

Histopathology
Hind limbs of arthritic rats were removed and fixed in 10% buffered formalin. The limbs were decalcified in 5% formic acid, processed for paraffin embedding, sectioned at 5 μm thickness, and later stained with hematoxylin and eosin for examination under a light microscope. The histopathological change of joints was blindly graded by a pathologist and assigned a score of 0-3 [Table 4].
Table 4.
Mode of scoring of photomicrographs of arthritic paws of Sprague-Dawley rats

Statistical Analysis
Statistical analysis of data was done using Sigma Plot version 12.3 (Systat Software Inc. Chicago USA). Significant differences in paw volumes, body weight, arthritic scores, and AUCs for parameters measured were ascertained using 1-way and 2-way analysis of variance and Holm-Sidak’s post hoc test. Values plotted were mean ± SEM. P ≤ 0.05 and higher F values (F ≥ 4.0) were considered statistically significant.
RESULTS
CFA-induced Arthritis
CFA injection into the paws of rats produced a biphasic response observed as paw swelling or edema of the ipsilateral and contralateral paws. The first phase is the acute phase, characterized by unilateral edema of the ipsilateral paws. The subsequent phase, polyarthritic/chronic phase, is characterized by edema of the contralateral paws. All arthritic control animals showed acute inflammatory edema at the ipsilateral (injected paws) paws around days 9-10 followed by subsequent chronic polyarthritic phase which begins around days 10-12. Throughout the 28-day experiment, there was no significant change in the paw volume of the non-inflamed control groups injected with IFA.
Acute-phase Inflammation
PEE, EthE, EAE, DEX, and MET significantly (P ≤ 0.01-0.0001; F3,28=5.79-60.53) reduced acute-phase inflammation [Figure 1a, c and e; Figure 2a and c]. However, while PEE and EAE ameliorated the edema in the ipsilateral paws by 92.7% and 76.2%, respectively, at 100 mg/kg1, EthE effect was not significant (38.8% at 100 mg/kg1) [Figure 1b, d and f]. DEX and MET significantly ameliorated edema in the ipsilateral paws, i.e., 100% inhibition at 3 mg/kg1 and 80.0% inhibition at 1 mg/kg1, respectively [Figure 2b and d].
Figure 1.

Effects of the petroleum ether extract (PEE), ethyl acetate extract (EthE), and ethanol extract (EAE) of T. monadelpha stem bark on complete Freund’s adjuvant -induced arthritis. Graphs a, c, and e show the time course curves of PEE, EAE, and EthE treatments (bigger curve depicts acute phase while inserts depict polyarthritic phase). Graphs b, d, and f show the area under the time course curves. Each bar plotted is the mean±SEM (n = 8). ***P ≤ 0.001, **P ≤ 0.01: *P ≤ 0.05. †††P ≤ 0.001, ††P ≤ 0.01: †P ≤ 0.05. One-way and two-way analysis of variance followed by Holm-Sidak’s post hoc test
Figure 2.

Effects of dexamethasone (DEX) and methotrexate (MET) on complete Freund’s adjuvant-induced arthritis. Graphs a and c show the time course curves of DEX and MET treatments (bigger curve depicts acute phase while inserts depict polyarthritic phase). Graphs b and d show the area under the time course curves. Each bar plotted is the mean±SEM (n=8). ***P ≤ 0.001, **P ≤ 0.01, *P ≤ 0.05, †††P ≤ 0.001, ††P ≤ 0.01, †P ≤ 0.05. One-way and two-way analysis of variance followed by Holm-Sidak’s post hoc test
Polyarthritic/Chronic-phase Inflammation
PEE, EthE, EAE, DEX, and MET significantly (P ≤ 0.01-0.0001; F3,28= 5.57-57.76) reduced polyarthritic/chronic-phase inflammation [Figure 1a, c and e; Figure 2a and c]. PEE, EAE, DEX, and MET also significantly (P ≤ 0.01-0.0001; F3,42=4.69-10.43) minimized the progression of the inflammation from the acute to the polyarthritic phases, [Figure 1b and f; Figure 2b and d]. PEE, EthE, and EAE ameliorated the edema in the contralateral paws, with inhibitory effects of 98.0, 69.1, and 70.8%, respectively, at 100 mg/kg1 [Figure 1b, d and f]. DEX and MET also caused 125.3% inhibition at 3 mg/kg1 and 94.7% inhibition at 1 mg/kg1, respectively [Figure 2b and d]. PEE and EAE showed greater potency and efficacy comparable to DEX and MET [Table 5].
Table 5.
The effective dose (ED50) and percentage maximal effect (Emax) of T. monadelpha stem bark extracts and reference drugs in CFA-induced arthritis in Sprague-Dawley rats

Body Weight
The CFA group experienced weight loss with excess swelling, erythema, and joint rigidity in both ipsilateral and contralateral paws. While EthE, DEX, and MET significantly (P ≤ 0.05-0.0001; F3,28= 4.28-17.32) improved the body weights of the rats [Figure 3c, d, and e], PEE and EAE did not [Figure 3a and b].
Figure 3.

The time course curves of the effects of (a) the petroleum ether extract, (b) the ethyl acetate extract, (c) the ethanol extract of T. monadelpha stem bark, (d) dexamethasone and (e) methotrexate treatments on body weight of complete Freund’s adjuvant-induced arthritis rats. The insert of the graphs in a boxplot derived from the area under time course curves. Each point and boxplot represents the mean±SEM (n=5). ***P ≤ 0.001, **P ≤ 0.01, *P ≤ 0.05, (one-way analysis of variance followed by Holm-Sidak’s post hoc test)
Arthritic Score
PEE, EthE, and EAE significantly reduced (P < 0.05-0.01; F= 3.77-5.77) arthritic score. The effect was, however, not comparable to DEX and MET (P < 0.0001; F3,28=13.34-32.16), which were more potent [Figure 4a-e].
Figure 4.

The time course curves of the effects of (a) the petroleum ether extract, (b) the ethyl acetate extract, (c) the ethanol extract of T. monadelpha stem bark, (d) dexamethasone and (e) methotrexate treatments on arthritic score in complete Freund’s adjuvant -induced arthritis rats. The insert of the graphs in a boxplot derived from the area under time course curves. Each point and boxplot represents the mean±SEM (n=5). ***P ≤ 0.001, **P ≤ 0.01: *P ≤ 0.05, (one-way analysis of variance followed by Holm-Sidak’s post hoc test)
X-ray Radiography
Radiographs of rats from CFA group displayed arthritic changes characterized by soft-tissue swelling with bone demineralization occurring mostly at the tibiotarsal joint which are indications of bone damage, in both ipsilateral and contralateral paws, compared with IFA group, which had intact bone structure. Radiographs of rats from PEE, EthE, EAE (average score of 2.0 ± 0.9), DEX, and MET-treated (average score of 0.7 ± 0.7) groups showed minimal bone damage. CFA group had the highest arthritic score (4.0 ± 0.3) indicating severe bone enlargement with active osteophytosis in the bone metaphysis, osteolysis, focal areas of excessive bone resorption, subchondral erosion, and subluxation, while the IFA control recorded the lowest score, indicating that the bones were intact [Table 6].
Table 6.
Arthritic scores of arthritic paws (ipsilateral and contralateral) obtained by X-ray radiography after CFA-induced arthritis and treatment with T. monadelpha stem bark extracts and reference drugs

Histopathological Studies
Induced arthritis resulted in synovial hyperplasia, pannus formation, exudation of inflammatory cells (observed as accumulation of abundant monomorphonuclear and polymorphonuclear leukocytes into the joint space), and erosion of bone and cartilage. PEE, EthE, and EAE treatment resulted in a dose-dependent reduction (P ≤ 0.05-0.001; F4,9=6.99-65.14) in inflammation with the morphology of the synovium looking normal [Figure 5a, b and c]. DEX and MET improved the morphology of the tissue significantly (P ≤ 0.01; F4,9=17.75-18.75) [Figure 5d and e].
Figure 5.

Histopathological score for bone erosion, inflammatory cell infiltration, pannus formation, synovial hyperplasia, and fibrosis of arthritic rats treated with (a) the petroleum ether extract, (b) the ethyl acetate extract, (c) the ethanol extract of T. monadelpha stem bark, (d) dexamethasone and (e) methotrexate incomplete Freund’s adjuvant, complete Freund’s adjuvant. Bars plotted represent mean score±SEM (n = 8). ***P ≤ 0.001; **P ≤ 0.01; *P ≤ 0.05 compared to complete Freund’s adjuvant group. (one-way analysis of variance followed by Holm-Sidak’s post hoc test)
DISCUSSION
Adjuvant-induced arthritis in rats is an experimental model for therapeutic and pathogenetic studies of chronic forms of arthritis [19-22]. Chronic arthritis is usually associated with bone loss, due in part to systemic or local actions of interleukin (IL)-6 and tumor necrosis factor-α (TNF-α) [20]. These cytokines stimulate the release of tissue-destroying matrix metalloproteinases as well as by inhibiting the production of endogenous inhibitors of these metalloproteinases, the net result being joint damage. Pathological features of this disorder include edema, infiltration of mononuclear and polymorphonuclear cells into the joint (synovial spaces), pannus formation, periostitis, and erosion of cartilage and bone [21].
In this study, adjuvant-injected paw was typified by a rapid onset of inflammation evident within 24 h of adjuvant injection, which continued to increase up to day 21 post-induction. This allowed for the study of acute inflammatory reactions locally (at the site of injection), i.e., in the ipsilateral paw, as well as the immunological reaction that develops later in the contralateral paw and various organs [22]. The arthritic rats showed soft-tissue swelling around the ankle joints during arthritis, and it was considered edema of those particular tissues. As the disease progressed, a more diffused demineralization developed in the extremities [23]. This was observed from the X-ray of the control group. Secondary lesions of adjuvant arthritis occurred after a delay of approximately 10 days and were characterized by inflammation of non-injected sites (right hind legs, ears, and tail) and further increases in the volume of the injected hind leg.
A therapeutic treatment regimen was followed in this research by initiating treatment from day 10 to day 28. All treatments with extracts, especially PEE and EAE, were effective in reducing the primary edema by day 18. The non-injected paw developed secondary lesion by day 14 post-adjuvant injection as a result of immune response to the bacterial adjuvant [17]. Treatment of adjuvant-injected rats with the extracts showed a significant reduction of secondary paw inflammation (compared with arthritic controls). These observations suggest that the extracts have very significant anti-inflammatory activity, comparable to DEX and/or MET. These drugs (DEX and MET) target specifically two major aspects, namely reducing inflammation and relieving pain by blocking cyclooxygenase (COX)-mediated prostaglandins release and control of joint inflammation by suppressing inflammatory-induced bone erosion. This finding is in line with earlier publications which indicate that preparations of the stem bark of T. monadelpha have been used in Ghanaian traditional medicine to treat pain and inflammation for many years and their efficacies are widely acclaimed in different communities in Ghana [13,14,24-26].
Earlier phytochemical screening conducted revealed the presence of alkaloids, terpenoids, phytosterols, and reducing sugars in all the extracts studied. EAE and EthE also contained tannins, cardiac glycosides, anthraquinones, and saponins [16]. The anti-inflammatory activity exhibited by the extracts could be attributed to the combined effects of some of these phytochemicals. Many alkaloids have been ascertained to have anti-inflammatory activity using in vivo models such as carrageenan-induced pedal edema, 5-HT-induced pedal edema, xylene-induced ear edema, among others, and in vitro model including inhibitory activity on COX-1 and COX-2 and inhibitory activity on prostaglandin E2 (PGE2) and NO production [27]. This indicates diverse mechanisms by which alkaloids exert anti-inflammatory effect. Terpenoids and cardiac glycosides have the ability to modulate critical cell signaling pathways involved in the inflammatory response of the body such as nuclear transcription factor-kappa B activation [28,29], significant inhibition of cytokine production, and inhibition of T-cell immune responses among others [30]. A mixture of tannins (hydrolysable and non-hydrolysable) have been demonstrated to have apparent anti-inflammatory activity in carrageenan- and dextran-induced rat paw edema, cotton pellet granuloma test, and adjuvant-induced polyarthritis in rats. It is thought to be due to antagonism of the permeability-increasing effects of some inflammatory mediators, thus inhibiting the migration of leukocytes to an inflammatory site [31]. Anthraquinones were also found to possess anti-inflammatory activity after their inhibitory activities on NO production, COX-2, and PGE2 which was determined in a lipopolysaccharide-induced inflammation model and in carrageenan-induced paw edema [32]. Reduction of paw swelling from the 3rd week onward may have been due to immunological protection rendered by the plant extracts, preventing systemic spread and ultimately reducing the destruction of joints as seen in the arthritic scores for the photographs and the radiographs. The phytochemicals in the extracts could have contributed to the immunological protection due to their significant anti-inflammatory properties which suppresses the generation and spread of pro-inflammatory agents [27].
Reduced bone structure and increased re-absorption cause bone loss in adjuvant-induced arthritis in rats [33,34]. Results of radiographic scores clearly showed increased bone loss in arthritic groups. The extracts, especially PEE, and reference drug treatment decreased bone loss due to arthritis. This suggests a suppression of synovitis and protection of bone structure resulting in joint protection [9,35,36]. This effect conforms to one of the therapeutic strategies of managing arthritis. The major target for inflammatory process in adjuvant-induced arthritis is the synovium which results in tissue inflammation as a result of infiltration of the tissue with multiple immune cells and cytokines [37]. The tissue inflammation is observed as expansion of the synovial tissue and pannus formation that invades the bone and cartilage, destroying the tissue as it proceeds [38]. This process promotes osteoclastogenesis that leads to focal articular bone erosion at the site of pannus formation, as well as systemic bone loss similar to osteoporosis [38,39]. Inflammatory tissue invasion, into the subchondral bone, results in involvement of many cell types such as fibroblasts, lymphocytes, and monocytes [37]. Monocytes are the precursors of osteoclasts which bring about reabsorption of bone through the acidic disillusion of bone mineral and enzymatic destruction of bone matrix. This reabsorption of the bone by osteoclasts is due to the synthesis of proteases by the synovial fibroblasts, neutrophils, and the chondrocytes. Studies have shown that at the sites of bone erosion, large multinucleated osteoclastic cells resorb subchondral bone. Osteoclast formation is as a result of exposure of inflammatory cytokines present in synovial tissue [37]. The extracts were able to reduce cell infiltration, thereby ameliorating tissue inflammation in the rat synovial tissue, in a similar manner as DEX and MET, due to their potent anti-inflammatory activity.
Chronic arthritis is usually associated with weight loss. This may be due to the systemic or local action of inflammatory cytokines such as TNF-α and IL-1ß [20,40] produced primarily by monocytes and macrophages [41]. The high concentrations of TNF-α and IL-1ß exert a powerful influence on whole-body protein and energy metabolism. Although the specific mechanism(s) is not known, TNF-α is thought to stimulate muscle catabolism [42]. The increased catabolism raises resting energy expenditure, which leads to weight loss and reduced lean body mass, especially if energy and protein requirements are not met; a phenomenon recognized as “rheumatoid cachexia.” Changes in body weight, therefore, have also been used to assess the course of disease and response to therapy of anti-inflammatory drugs [43]. The extracts significantly improved body weight of arthritic rats, indicating a reduction of catabolism caused by the inflammatory cytokines and hence their therapeutic potential in the management of RA.
CONCLUSION
This study has demonstrated that PEE, EthE, and EAEs of the stem bark of T. monadelpha have interesting antiarthritic property by reducing bone tissue damage and resorption in Freund’s complete adjuvant-induced arthritis and hence the extracts are worth further investigating as they could be very useful to humans.
ACKNOWLEDGMENTS
We are grateful for the technical support of the Department of Pharmacology, CHS, KNUST, and the X-ray and Ultrasound Department of the KNUST Hospital, Kumasi, Ghana.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Corrado A, Neve A, Maruotti N, Cantatore FP. Bone effects of biologic drugs in rheumatoid arthritis. Clin Dev Immunol. 2013;2013:945945. doi: 10.1155/2013/945945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Silman AJ, Hochberg MC. Epidemiology of the Rheumatic Diseases. 2nd ed. New York: Oxford University Press; 2001. pp. 31–71. [Google Scholar]
- 3.Hess A, Axmann R, Rech J, Finzel S, Heindl C, Kreitz S, et al. Blockade of TNF-a rapidly inhibits pain responses in the central nervous system. Proc Natl Acad Sci U S A. 2011;108:3731–6. doi: 10.1073/pnas.1011774108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McInnes IB, Schett G. The pathogenesis of rheumatoid arthritis. N Engl J Med. 2011;365:2205–19. doi: 10.1056/NEJMra1004965. [DOI] [PubMed] [Google Scholar]
- 5.Bansback N, Marra CA, Finckh A, Anis A. The economics of treatment in early rheumatoid arthritis. Best Pract Res Clin Rheumatol. 2009;23:83–92. doi: 10.1016/j.berh.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Furst DE, Munster T. Nonsteroidal antiinflammatory drugs, disease-modifying antirheumatic drugs, nonopioid analgesics, and drugs used in gout. In: Katzung BG, editor. Basic and Clinical Pharmacology. 8th ed. New York: McGraw-Hill; 2001. pp. 596–623. [Google Scholar]
- 7.Fairchild KD, Singh IS, Patel S, Drysdale BE, Viscardi RM, Hester L, et al. Hypothermia prolongs activation of NF-kappaB and augments generation of inflammatory cytokines. Am J Physiol Cell Physiol. 2004;287:C422–31. doi: 10.1152/ajpcell.00507.2003. [DOI] [PubMed] [Google Scholar]
- 8.Kirwan JR. The effect of glucocorticoids on joint destruction in rheumatoid arthritis. The Arthritis and Rheumatism Council Low-Dose Glucocorticoid Study Group. N Engl J Med. 1995;333:142–6. doi: 10.1056/NEJM199507203330302. [DOI] [PubMed] [Google Scholar]
- 9.Atzeni F, Sarzi-Puttini P. Early rheumatoid arthritis. Reumatismo. 2007;59:100–17. doi: 10.4081/reumatismo.2007.100. [DOI] [PubMed] [Google Scholar]
- 10.Fries JF, Williams CA, Morfeld D, Singh G, Sibley J. Reduction in long-term disability in patients with rheumatoid arthritis by disease-modifying antirheumatic drug-based treatment strategies. Arthritis Rheum. 1996;39:616–22. doi: 10.1002/art.1780390412. [DOI] [PubMed] [Google Scholar]
- 11.Lemmens RH. Plant Resources of Tropical Africa. Vol. 1. Leiden, Netherland: Prota Foundation Wageningen, Netherlands/Backhuys Publishers; 2008. pp. 501–3. [Google Scholar]
- 12.Busia K. Ghana herbal pharmacopoeia. Ghana: Cantonments, Accra-Ghana: Science and Technology Policy Research Institute, Council for Scientific and Industrial Research; 2007. pp. 230–233. [Google Scholar]
- 13.Ainooson GK, Owusu G, Woode E, Ansah C, Annan K. Trichilia monadelpha bark extracts inhibit carrageenan-induced foot-oedema in the 7-day old chick and the oedema associated with adjuvant-induced arthritis in rats. Afr J Tradit Complement Altern Med. 2011;9:8–16. doi: 10.4314/ajtcam.v9i1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Woode E, Amoh-Barimah AK, Abotsi WK, Ainooson GK, Owusu G. Analgesic effects of stem bark extracts of Trichilia monadelpha (Thonn.) JJ De Wilde. Indian J Pharmacol. 2012;44:765–73. doi: 10.4103/0253-7613.103299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oyelowo OT, Bolarinwa OL, Morenikeji OA. Assessment of sperm indices and testosterone level on the effect of Trichilia monadelpha extract in male albino rats. Afr J Pharm Pharm. 2011;5:1956–8. [Google Scholar]
- 16.Ben IO, Woode E, Abotsi WK, Boakye-Gyasi E. Preliminary phytochemical screening and in vitro antioxidant properties of Trichilia monadelpha (Thonn.) JJ De Wilde (Meliaceae) J Med Biomed Sci. 2013;2:6–15. [Google Scholar]
- 17.Pearson CM. Development of arthritis, periarthritis and periostitis in rats given adjuvants. Proc Soc Exp Biol Med. 1956;91:95–101. doi: 10.3181/00379727-91-22179. [DOI] [PubMed] [Google Scholar]
- 18.Woode E, Ainooson GK, Boakye-Gyasi E, Ansah C, Obiri DD, Koffour GA, et al. Anti-arthritic and antioxidant properties of the ethanolic stem bark extract of Newbouldia laevis (P Beauv.) Seaman ex Bureau (Bignoniaceae) J Med Plants Res. 2008;2:180–8. [Google Scholar]
- 19.Halim TY, Song KW, Barnett MJ, Forrest DL, Hogge DE, Nantel SH, et al. Positive impact of selective outpatient management of high-risk acute myelogenous leukemia on the incidence of septicemia. Ann Oncol. 2007;18:1246–52. doi: 10.1093/annonc/mdm112. [DOI] [PubMed] [Google Scholar]
- 20.Chamundeeswari D, Vasantha J, Gopalakrishnan S, Sukumar E. Free radical scavenging activity of the alcoholic extract of Trewia polycarpa roots in arthritic rats. J Ethnopharmacol. 2003;88:51–6. doi: 10.1016/s0378-8741(03)00143-0. [DOI] [PubMed] [Google Scholar]
- 21.Williams RO. Rodent models of arthritis: Relevance for human disease. Clin Exp Immunol. 1998;114:330–2. doi: 10.1046/j.1365-2249.1998.00785.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Klareskog L. What can we learn about rheumatoid arthritis from animal models?Springer Semin Immunopathol. 1989;11:315–33. doi: 10.1007/BF00197310. [DOI] [PubMed] [Google Scholar]
- 23.Begum VH, Sadique J. Long term effect of herbal drug Withania somnifera on adjuvant induced arthritis in rats. Indian J Exp Biol. 1988;26:877–82. [PubMed] [Google Scholar]
- 24.Abbiw DK. Useful Plants of Ghana: West African Uses of Wild and Cultivated Plants. Royal Botanic Gardens: Intermediate Technology Publications; 1990. [Google Scholar]
- 25.Dokosi OB. Herbs of Ghana. Accra: Ghana Universities Press; 1998. [Google Scholar]
- 26.Ben IO, Woode E, Koffuor GA, Boakye-Gyasi E, Ehigiator BE. Effect of Trichilia monadelpha (Thonn.) J. J. De Wilde (Meliaceae) extracts on haematology, cytokines and oxidative stress biomarkers in rats adjuvant-induced arthritis. Pharmacologia. 2016;7:32–43. [Google Scholar]
- 27.Souto AL, Tavares JF, da Silva MS, Diniz Mde F, de Athayde-Filho PF, Barbosa Filho JM. Anti-inflammatory activity of alkaloids: An update from 2000 to 2010. Molecules. 2011;16:8515–34. doi: 10.3390/molecules16108515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang Q, Huang W, Jozwik C, Lin Y, Glasman M, Caohuy H, et al. Cardiac glycosides inhibit TNF-a/NF-kB signaling by blocking recruitment of TNF receptor-associated death domain to the TNF receptor. Proc Natl Acad Sci U S A. 2005;102:9631–6. doi: 10.1073/pnas.0504097102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de las Heras B, Hortelano S. Molecular basis of the anti-inflammatory effects of terpenoids. Inflamm Allergy Drug Targets. 2009;8:28–39. doi: 10.2174/187152809787582534. [DOI] [PubMed] [Google Scholar]
- 30.Ku CM, Lin JY. Anti-inflammatory effects of 27 selected terpenoid compounds tested through modulating Th1/Th2 cytokine secretion profiles using murine primary splenocytes. Food Chem. 2013;141:1104–13. doi: 10.1016/j.foodchem.2013.04.044. [DOI] [PubMed] [Google Scholar]
- 31.Mota ML, Thomas G, Barbosa Filho JM. Anti-inflammatory actions of tannins isolated from the bark of Anacardium occidentale L. J Ethnopharmacol. 1985;13:289–300. doi: 10.1016/0378-8741(85)90074-1. [DOI] [PubMed] [Google Scholar]
- 32.Choi RJ, Ngoc TM, Bae K, Cho HJ, Kim DD, Chun J, et al. Anti-inflammatory properties of anthraquinones and their relationship with the regulation of P-glycoprotein function and expression. Eur J Pharm Sci. 2013;48:272–81. doi: 10.1016/j.ejps.2012.10.027. [DOI] [PubMed] [Google Scholar]
- 33.Findlay DM, Haynes DR. Mechanisms of bone loss in rheumatoid arthritis. Mod Rheumatol. 2005;15:232–40. doi: 10.1007/s10165-005-0412-z. [DOI] [PubMed] [Google Scholar]
- 34.Mäkinen H, Kautiainen H, Hannonen P, Möttönen T, Leirisalo-Repo M, Laasonen L, et al. Sustained remission and reduced radiographic progression with combination disease modifying antirheumatic drugs in early rheumatoid arthritis. J Rheumatol. 2007;34:316–21. [PubMed] [Google Scholar]
- 35.Hoffmann JC, Herklotz C, Zeidler H, Bayer B, Rosenthal H, Westermann J. Initiation and perpetuation of rat adjuvant arthritis is inhibited by the anti-CD2 monoclonal antibody (mAb) OX34. Ann Rheum Dis. 1997;56:716–22. doi: 10.1136/ard.56.12.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sharma PK, Hota D, Pandhi P. Biologics in rheumatoid arthritis. J Assoc Physicians India. 2004;52:231–6. [PubMed] [Google Scholar]
- 37.Cantley MD, Smith MD, Haynes DR. Pathogenic bone loss in rheumatoid arthritis: Mechanisms and therapeutic approaches. Int J Clin Rheumatol. 2009;4:561–82. [Google Scholar]
- 38.Walsh NC, Crotti TN, Goldring SR, Gravallese EM. Rheumatic diseases: The effects of inflammation on bone. Immunol Rev. 2005;208:228–51. doi: 10.1111/j.0105-2896.2005.00338.x. [DOI] [PubMed] [Google Scholar]
- 39.Romas E, Gillespie MT. Inflammation-induced bone loss: Can it be prevented?Rheum Dis Clin North Am. 2006;32:759–73. doi: 10.1016/j.rdc.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 40.Choy EH, Panayi GS. Cytokine pathways and joint inflammation in rheumatoid arthritis. N Engl J Med. 2001;344:907–16. doi: 10.1056/NEJM200103223441207. [DOI] [PubMed] [Google Scholar]
- 41.Koch AE, Kunkel SL, Strieter RM. Cytokines in rheumatoid arthritis. J Investig Med. 1995;43:28–38. [PubMed] [Google Scholar]
- 42.Rall LC, Rosen CJ, Dolnikowski G, Hartman WJ, Lundgren N, Abad LW, et al. Protein metabolism in rheumatoid arthritis and aging. Effects of muscle strength training and tumor necrosis factor alpha. Arthritis Rheum. 1996;39:1115–24. doi: 10.1002/art.1780390707. [DOI] [PubMed] [Google Scholar]
- 43.Winder CV, Lembke LA, Stephens MD. Comparative bioassay of drugs in adjuvant-induced arthritis in rats: Flufenamic acid, mefenamic acid, and phenylbutazone. Arthritis Rheum. 1969;12:472–82. doi: 10.1002/art.1780120503. [DOI] [PubMed] [Google Scholar]


