Abstract
Attention-deficit/hyperactivity disorder (ADHD) is highly comorbid with and predictive of externalizing behavior, yet is most often examined categorically, not dimensionally. We tested a recently proposed trait impulsivity model by dimensionally examining measures of childhood inattention and hyperactivity/impulsivity separately as predictors of later externalizing behavior in an all-female longitudinal sample of 228 young women. We also examined influences of parenting and peer relations, given the transactional nature and importance of environmental factors. We analyzed the relative contribution of hyperactive/impulsive (HI) and inattentive (IA) symptoms of girls with and without childhood-diagnosed ADHD (M age = 9.5; 140 ADHD and 88 Comparison) to the development of externalizing behaviors in adolescence (M age = 14.2) and early adulthood (M age = 19.6). Authoritarian parenting was examined as a moderator and adolescent externalizing behavior as a mediator of the relation between childhood HI and later externalizing behavior. Childhood HI symptoms significantly predicted multiple externalizing behaviors in adolescence and early adulthood, after accounting for IA and covariates (ΔR2 ranged from 2.6% to 7.5%). Mother’s authoritarian parenting moderated this relation. Adolescent externalizing behavior mediated the relation between childhood HI symptoms and early adult externalizing behavior. In no case did childhood IA significantly predict externalizing behavior after accounting for HI symptoms. Findings support a trait impulsivity model, as HI symptoms, but not IA symptoms, significantly predicted later externalizing behavior. Results support the importance of dimensional predictors of developmental trajectories. We discuss implications for assessment, intervention, and future research.
Keywords: Attention-deficit/hyperactivity disorder (ADHD), externalizing behavior, hyperactivity, impulsivity, longitudinal, trait impulsivity
Externalizing psychopathology spans a wide domain of behaviors, including impulsivity, oppositionality, aggression, delinquency, and antisocial/criminal actions. Its impact on society is both significant and costly (Foster, Jones, & Conduct Problems Prevention Research Group, 2005; Hinshaw & Scheffler, 2014; Pelham, Foster, & Robb, 2007). Attention-deficit/hyperactivity disorder (ADHD) is strongly associated, concurrently and subsequently, with other externalizing syndromes (Angold, Costello, & Erkanli, 1999; Jensen, 2003; Kessler, Chiu, Demler, & Walters, 2005). It is still unclear, however, how closely related these supposedly distinct syndromes are (Ahmad & Hinshaw, 2016; Hinshaw, 1987). Two key challenges for the field include (a) accounting for the high occurrence of what are assumed to be different, behaviorally based externalizing syndromes in one individual at the same time (homotypic comorbidity) and (b) accounting for the manifestation of externalizing syndromes throughout development (heterotypic continuity; Beauchaine & McNulty, 2013). Addressing these challenges is our key objective. In addition, much of the research on ADHD and externalizing behavior has utilized cross-sectional data and focused on boys, meaning that female manifestations and developmental mechanisms are largely unknown. Overall, investigating the relation between dimensionally measured ADHD symptom patterns and externalizing behavior over childhood, adolescence, and early adulthood, particularly in girls, is a priority.
Historically, in terms of categorical diagnoses within the fields of clinical psychology and psychiatry, the terrain of externalizing syndromes has included ADHD, oppositional defiant disorder (ODD), and conduct disorder (CD) in childhood and adolescence, as well as antisocial personality disorder (ASPD) in early adulthood (Achenbach & Edelbrock, 1984; Krueger, Markon, Patrick, Benning, & Kramer, 2007). In related fields, researchers have used constructs including aggression (physical/violent behavior), delinquency (juvenile rule-breaking and non-violent criminal behavior), and criminality. A consistent theme in prospective studies of such behavior is that ADHD is both comorbid with and predictive of these other externalizing behaviors over time, at least in males (see, e.g., Loeber, Burke, & Pardini, 2009; Moffitt & Caspi, 2001). In particular, childhood hyperactive/impulsive and oppositional behavior is associated with severe levels of adolescent externalizing behavior, such that children with ADHD (particularly those with comorbid ODD) are likely to engage in aggressive and delinquent behavior during adolescence (Bagwell, Molina, Pelham, & Hoza, 2001). However, far less is known about the behaviors exhibited by such adolescents once they enter early adulthood: Do such behaviors continue, or are they likely to desist following adolescence?
In addition to the strongly heritable roots of ADHD-related behavior patterns, two important contextual factors are likely to transact with these behaviors and contribute to developmental progressions: (a) maladaptive parenting and (b) negative peer/social relationships. Both have also been associated with later antisocial behavior, particularly in adolescence and early adulthood (Moffitt & Caspi, 2001; Murray & Farrington, 2010). In childhood, ADHD is strongly associated with problems regarding both of these contextual factors (Barkley, 2014; Molina et al., 2009). Such children often engage with their parents (who, given the high heritability of the relevant symptoms, often display such characteristics themselves) in a reciprocal pattern of negative interaction, wherein a child’s hyperactive/impulsive and oppositional behaviors elicit negative feedback from parents, and vice versa (Patterson, 2002). Such patterns are highly predictive of later externalizing behaviors, such as delinquency and aggression (Deault, 2010; Hoeve et al., 2009; Rothbaum & Weisz, 1994). Conversely, supportive parenting is protective against later externalizing behavior (Pettit, Bates, & Dodge, 1997). In essence, especially for children with ADHD-related symptoms, harsh/authoritarian parenting in childhood is associated with increased risk for externalizing behaviors, whereas more supportive, authoritative parenting is associated with decreased risk.
A similar pattern exists between childhood ADHD, peer conflict, and the development of later externalizing behavior (Laird, Jordan, Dodge, Pettit, & Bates, 2001; Moffitt & Caspi, 2001). Childhood ADHD is a strong predictor of peer conflict, related largely to the impulsive and aggressive behaviors that accompany the syndrome (e.g., Hinshaw & Melnick, 1995). Adolescents who are rejected by their peers are often marginalized and tend to associate with deviant peers, which in turn spur the development of other externalizing behaviors (Bagwell et al., 2001; Laird et al., 2001). Despite strong evidence that both parenting and peer conflict are associated with later externalizing behavior, research into early adulthood is still lacking.
Sex differences in externalizing behavior are apparent, with boys much more likely than girls to exhibit early and more severe forms of such behavior (Loeber & Hay, 1997; Moffitt & Caspi, 2001; see also Moffitt, Caspi, Rutter, & Silva, 2001). As a result, the vast majority of the longitudinal research into externalizing behavior, including ADHD, has focused on boys (Burke, Loeber, & Birmaher, 2002; Loeber et al., 2009). Indeed, relatively little is known about relevant developmental progressions for girls (see Broidy et al., 2003; Hinshaw, 2002b). Within the limited prospective research on young women with childhood ADHD (see Babinski et al., 2011; Biederman et al., 2010; Hinshaw et al., 2012), ADHD does appear to predict later externalizing behavior, yet less is known about potential developmental mechanisms (but see Owens & Hinshaw, 2016). Understanding such processes is a priority, given overall increases in externalizing behavior among girls in recent years (e.g., Hinshaw & Kranz, 2009).
There is growing support for investigating ADHD (and psychopathology more general) dimensionally, as the core symptoms are nearly always continuously distributed across a population (Coghill & Sonuga-Barke, 2012). Indeed, utilizing symptom dimensions and other transdiagnostic constructs may advance knowledge faster and more reliably (Insel et al., 2010). This approach appears particularly salient for ADHD, given strong support for its underlying symptom dimensions: hyperactive/impulsive (HI) and inattentive/disorganized (IA). Investigations measuring ADHD dimensionally reveal that HI symptoms are reliably associated with later externalizing behavior (Greven, Asherson, Rijsdijk, & Plomin, 2011; Kuja-Halkola, Lichtenstein, D’Onofrio, & Larsson, 2015; Lee & Hinshaw, 2006), yet such evidence is less apparent for IA symptoms (see Beauchaine, Hinshaw, & Pang, 2010; Diamond, 2005).
Common genetic/behavioral factors appear to cut across current externalizing diagnostic categories. Factor analyses of externalizing behavior have revealed a common, highly heritable trait in both child and adult samples (Krueger, Markon, Patrick, & Iacono, 2005; Tuvblad, Zheng, Raine, & Baker, 2009). In addition, both genetic and shared environmental factors contribute to a large amount of the variance found in externalizing behavior in childhood. There is an important exception here: shared environmental contributions are vanishingly small in ADHD (Burt, 2009; Kuja-Halkola et al., 2015), with increased importance of non-shared environmental factors by early adulthood (Larsson, Larsson, & Lichtenstein, 2004; Loeber et al., 2009). Crucially, among the externalizing behaviors, ADHD-related symptoms also have the earliest age of onset and the highest heritability (~.76) (Faraone et al., 2005; Kessler, Berglund, et al., 2005). Thus, early-appearing ADHD symptoms might transact with increasingly important environmental factors over time to produce a range of externalizing behavior patterns.
Beauchaine and McNulty (2013) propose that an early-appearing, highly heritable, neurobiologically based, higher-order factor termed trait impulsivity confers considerable risk for the manifestation and development of externalizing behavior. Trait impulsivity typically manifests in childhood as ADHD-related symptoms and then progresses—via reciprocal interactions with key environmental factors (e.g., harsh/negative parenting; peer conflict; discordant neighborhoods)—into oppositional, aggressive, and antisocial behaviors in a subset of children (Beauchaine & McNulty, 2013). Although this model suggests that trait impulsivity can be operationalized during childhood via existing, well-validated measures of ADHD symptoms – in particular the HI dimension (see also Burns, de Moura, Beauchaine, & McBurnett, 2014; Neuhaus & Beauchaine, in press) – differentiating the relative impact of HI vs. IA on the development of later externalizing behavior still requires empirical testing.
Our purpose herein is to utilize a large, well-characterized longitudinal sample of girls with and without ADHD to explore predictors and outcomes for a range of externalizing behavior from childhood to early adulthood. Leveraging the trait impulsivity model, we utilize dimensional measures of childhood HI and IA to explore potential developmental progressions of externalizing behavior, including oppositionality, delinquency, aggression, antisocial behavior, and ultimately arrests and incarceration. The current sample is particularly well-suited for this line of inquiry, consisting of girls who are enriched for both IA and HI symptoms and utilizing multi-informant, multi-domain measures of predictors and outcomes.
We hypothesize, first, that childhood symptoms of HI will predict increased externalizing behavior in adolescence (conduct problems, aggression, delinquency, and deviant peer association) and early adulthood (conduct problems, delinquency, deviant peer association, antisocial behavior, and criminality), but symptoms of IA will not. Second, given findings that parenting during childhood are associated with later externalizing behavior, we hypothesize that parenting will moderate the relation between childhood HI symptoms later externalizing behavior, such that higher levels of authoritarian parenting during childhood will escalate the predictive association between HI symptoms and externalizing behavior. Given the co-occurrence of parenting and childhood ADHD symptoms at the same time point, as well as their relative independence during childhood, moderator analyses are indicated. Third, in order to help explain developmental progressions from childhood ADHD symptoms to adult externalizing behavior, we hypothesize that adolescent externalizing behaviors (conduct problems, aggression, delinquency), and adolescent peer conflict, will mediate the association between childhood HI symptoms and early-adult externalizing behavior. We utilize mediational analyses in this case given that our adolescent behaviors were measured after the childhood behavior predictors but before the early-adult behavioral outcomes.
Method
Participants and Procedure
The sample consists of participants from the Berkeley Girls with ADHD Longitudinal Study (BGALS), who were recruited from the greater San Francisco Bay Area for naturalistic, research-based 5-week summer camps between 1997 and 1999, and who were then prospectively followed 5- and 10-years later (for more details and additional demographic information, see Hinshaw, 2002a; Hinshaw, Owens, Sami, & Fargeon, 2006; Hinshaw et al., 2012). After a multi-gated screening procedure at baseline, the final sample consisted of 228 girls (ages 6–12, M age = 9.5), 140 of whom received a diagnosis of ADHD plus 88 age- and ethnicity-matched comparisons. The sample was ethnically diverse (57% Caucasian, 28% African American, 11% Latina, and 4% Asian American). After baseline assessments (W1), families were invited to participate in follow-up assessments roughly five years (W2; M age = 14.2 years, N = 209, retention rate = 92%) and 10 years later (W3; M age = 19.6 years, N = 216, retention rate = 95%). Data were obtained from a rigorous assessment procedure, interview and questionnaires covering multiple domains of functioning, clinician observations, self-report, and peer and parent/teacher reported information. To the greatest extent possible, multi-informant evaluation strategies were utilized across all waves. Three differences were significant for the non-retained subsample of 12 participants compared to the W3 sample: household income and full-scale IQ (FSIQ) was lower, and W1 teacher-reported ADHD symptoms were higher.
Measures - Wave 1 (Childhood)
ADHD Symptoms
At baseline, ADHD symptoms were assessed dimensionally using the Swanson, Nolan, and Pelham Rating Scale (4th ed.; SNAP-IV; Swanson, 1992). For the present study, ADHD symptoms (9 symptoms of HI and 9 symptoms of IA) were obtained from both mother and teacher report. First, mean symptom severity ratings were generated for HI and IA symptom dimensions (range from 0 to 3) separately for mother and teacher. Mother and teacher ratings were strongly correlated for IA, r(224) = .785, p < 001, and HI, r(224) = .660, p < 001. We then created a mother + teacher composite mean symptom severity score for the HI dimension (M = 1.00, SD = 0.84) and the IA dimension (M = 1.44, SD = 0.97).
Wave 1 Covariates
To adjust for the effects of potential confounders, all analyses employed stringent covariates (see also Hinshaw et al., 2012), including child’s age, ethnicity, family income, mother’s education, and FSIQ, obtained from the Wechsler Intelligence Scale for Children (3rd ed., Wechsler, 1991). Finally, although oppositionality is theoretically consistent with the trait impulsivity model, we also covaried W1 ODD symptoms for the first hypothesis when evaluating the independent effects of HI on externalizing behaviors at W2 and W3. In order to reduce effects of shared method variance between ADHD and ODD on the basis of the SNAP-IV, W1 ODD symptoms were taken from the Diagnostic Interview Schedule for Children (4th ed.; DISC-IV; Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000), instead of the SNAP-IV, r(225) = .740, p < 001, by totaling the number of symptoms endorsed by parents.
Wave 1 Parenting
In order to test moderation effects for Hypothesis 2, we utilized parenting information from the Ideas About Parenting measure (IAP; Heming, Cowan, & Cowan, 1990), which contains 70 items. After a principal component analysis, three parenting factors emerged for mother-reported information: Authoritarian, Authoritative, and Overwhelmed/Unsure (see Hinshaw, 2002a; Hinshaw, Zupan, Simmel, Nigg, & Melnick, 1997). For the purpose of this study, we included only the Authoritarian factor (containing 17 items with factor loadings > .30, α = .76).
Measures - Wave 2 (Adolescence)
Conduct Problems
At the W2 follow-up, conduct problems were measured dimensionally by totaling parent-reported symptoms for Conduct Disorder from the DISC-IV structured clinical interview (M = 0.77, SD = 1.39).
Aggression and Delinquency
Aggression and Delinquency ratings were obtained from both parents and teachers with the widely-used Child Behavior Checklist (CBCL) and Teacher Report Form (TRF; Achenbach, 1991a, 1991b). We analyze these narrow-band measures separately at the W2 time point – as opposed to using the broad-band Externalizing scale – in order to explore potentially different developmental pathways from adolescent to early adult externalizing behavior. Both the Aggression (M = 57.9, SD = 8.7) and Delinquency (M = 57.0, SD = 7.7) scores were derived from mean T scores of the CBCL and the TRF.
Self-Reported Delinquency
During adolescence, the number of delinquent acts committed was obtained from a version of the Self-Reported Delinquency scale (SRD; Elliott, Huizinga, & Ageton, 1985). This version of the widely-used measure contains 36 questions regarding a range of behaviors committed in the previous 6 months (endorsed as either yes or no). All acts endorsed with a yes were then tallied into three non-overlapping subscales: Overt, Covert, and Substance Use. The Covert subscale contains items such as running away from home, skipping school, stealing, cheating, and destruction of property. The Overt subscale contains items such as being unruly, carrying/using a weapon, and attacking or using force against others. Given the theoretical importance of distinguishing covert from overt acts (see Loeber et al., 2009), and as substance use is not the focus of the present study, we include only the Overt (8 items, α = .44, M = 0.26, SD =0.60) and Covert (20 items, α = .64 M = 0.59, SD = 1.11) SRD subscales. We note that the alpha levels are lower here given that these are counts of various acts committed as opposed to a Likert scale of frequencies of behavior for each item.
Deviant Peer Association
Information on each participant’s association with deviant peers was obtained as an outcome measure of W2 and W3 externalizing behavior. This subscale of 15 items (α = .93) comes from a project-derived measure based on the Peer Delinquency Scale used in the Pittsburgh Youth Study (Loeber, Farrington, Stouthamer-Loeber, & Van Kammen, 1998). Participants report how many friends engage in behaviors such as skipping school, stealing, or damaging property. We calculated the mean value of all items, based on a 5-point metric ranging from none, few, half, most, to all (M = 0.41, SD = 0.51).
Peer Conflict
A W2 peer conflict composite measure was created in order to test for possible mediation effects (Hypothesis 3), derived from an adolescent self-report and parent-report measure. In the project-derived Social Relations Interview, adolescents reported on three questions regarding peer rejection by stating the frequency of the following activities over the previous year: 1) being hit, pushed, shoved, kicked or having their hair pulled; 2) being called names or teased to their face; 3) having other peers talk about them behind their backs or spread rumors about them. Intercorrelations ranged from .27 to .55 (N = 199). We also used a project-based Social Relationships Questionnaire (SRQ), wherein parents described their adolescent’s relationships and friendships (Hinshaw et al., 2006). The peer conflict subscale was based on a principal components analysis, yielding a six-item factor (α = .83) from a total of 12 items, which correlated with the adolescent-reported Social Relations Interview peer conflict subscale at r(191) = .30 (p < .001). Both scales were standardized and then summed.
Measures - Wave 3 (Early Adulthood)
Repeated measures from W2
The following W2 measures were repeated at W3: Self-Reported Delinquency (W3 Overt SRD: α = .53, M = 0.28, SD = 0.87; W3 Covert SRD: α = .52, M = 1.22, SD = 1.37), Deviant Peer Association (α = .82, M = 0.72, SD = 0.46), and Conduct Problems. For W3 Conduct Problems, two key changes from W2 were: (a) the version of the DISC-IV used was the Young Adult Version (DISC–IV–YA; Shaffer et al., 2000); and (b), data were available from both parents and participants in most cases. Thus, we utilized a best estimate in which a given symptom was considered present if it was endorsed by either the participant or the parent (Piacentini, Cohen, & Cohen, 1992). We then calculated a total symptom count score (M = .90, SD = 1.39).
Antisocial behavior (ASB)
Antisocial behavior (ASB) was measured dimensionally during early adulthood utilizing the Antisocial Personality Disorder symptoms from the DISC–IV–YA. Similar to W3 Conduct Problems, a best estimate approach was utilized such that a given symptom was considered present if it was endorsed by either the participant or the parent. We then tallied a total symptom count score (M = 2.33, SD = 2.14).
Criminality
At W3 we ascertained whether participants had been either arrested or incarcerated since W2. This dichotomous variable (1 = yes; 0 = no) was derived from both a self-reported and parent-reported measure. If the young adult or her parents indicated that she had been arrested or incarcerated since W2, then the criminality value was set to 1. A total of 26 young women had reported either being arrested or incarcerated by their W3 visit.
Data Analytic Plan
First, zero-order correlations were conducted for all study variables. To test Hypothesis 1, hierarchical linear regressions were performed to compare the independent contributions of HI vs. IA to later externalizing behavior. All covariates were entered at Step 1, IA was entered at Step 2, and HI was entered last at Step 3 (this procedure was then repeated, entering HI at Step 2 and IA at Step 3). For the dichotomous W3 outcome of Criminality, a binary logistic regression was performed, utilizing the same three-step approach as above. To test Hypothesis 2, we performed hierarchical regressions to examine whether mother-reported Authoritarian parenting moderated the effect of HI on adolescent (W2) and early adult (W3) outcomes. All covariates and W1 IA were entered at Step 1, HI and Authoritarian Parenting at Step 2, and finally an HI X Authoritarian Parenting interaction term at Step 3. We centered all variables using the sample mean and applied a Bonferroni correction to maintain a familywise error rate of α = .05.
Finally, to test mediation effects for Hypothesis 3, we utilized a bootstrap procedure to identify indirect effects (IEs) between W1 HI and all W3 outcomes (Preacher & Hayes, 2008), via the PROCESS macro for SPSS (Hayes, 2013). This statistical simulation generates a new random sample from the data, calculating a point estimate of the indirect effect for that sample. This procedure is repeated 20,000 times, with replacement, generating a 95% bias-corrected confidence interval for the overall sampling distribution of IEs. Statistical significance was inferred if the confidence interval for the indirect effect did not include zero.
Results
Zero-Order Correlations
Zero-order correlations for all continuous variables are presented in Table 1. Correlations among the W1 and W2 variables were moderately strong and in the anticipated direction. Adolescent parent/teacher reported delinquency was moderately correlated with Covert and Overt SRD, r(203) = .33 and .31, respectively, p < .001. Of note, there was noticeable instability in repeated measures of externalizing behaviors from W2 to W3: whereas Conduct Problems stability was small but significant, r(197) = .25, p < .001, neither Covert nor Overt SRD was stable over time; r(193) ranged from .01 to .09, p = ns. We note that the overall base rates for Overt and Covert SRD at W2 are low, which also accounts for our lower alpha values. For Covert SRD, mean, median, SD and range are: .59, 0, 1.1, and 0–6 (of 20 items total), respectively; Overt SRD: .26, 0, 0.60, and 0–3 (of 8 items total), respectively.
Table 1.
Intercorrelations Between Predictors, Covariates, and Outcome Variables
| Measure | Wave 1
|
Wave 2
|
Wave 3
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15a | |
| 1. W1 IA | .76d | .59d | .28d | .46d | .42d | .01 | .12 | .10 | .22c | .38d | −.03 | .07 | .07 | .12 | |
| 2. W1 HI | .60d | .41d | .60d | .46d | .01 | .12 | .05 | .38d | .42d | .09 | .22c | .15b | .16b | ||
| 3. W1 ODD | .38d | .54d | .41d | .02 | .11 | .03 | .28d | .37d | −.02 | .13 | −.05 | .21c | |||
|
| |||||||||||||||
| 4. W2 Conduct | .62d | .67d | .27d | .19c | .13 | .25d | .28d | .04 | .16b | .10 | .34d | ||||
| 5. W2 Aggression | .78d | .20c | .20c | .17b | .32d | .30d | −.02 | .17b | .11 | .17b | |||||
| 6. W2 Delinquency | .33d | .31d | .33d | .27d | .33d | −.02 | .19c | .17b | .23c | ||||||
| 7. W2 SRD - Covert | .54d | .52d | .09 | .22c | .09 | .08 | .20c | .33d | |||||||
| 8. W2 SRD - Overt | .43d | .01 | .09 | .01 | .06 | .22c | .21c | ||||||||
| 9. W2 Deviant Peers | .13 | .19c | −.01 | .03 | .26d | .29d | |||||||||
|
| |||||||||||||||
| 10. W3 Conduct | .56c | .31c | .46c | .42c | .31c | ||||||||||
| 11. W3 ASB | .22c | .26c | .33c | .33c | |||||||||||
| 12. W3 SRD - Covert | .15b | .41c | .09 | ||||||||||||
| 13. W3 SRD - Overt | .30c | .04 | |||||||||||||
| 14. W3 Deviant Peers | .22c | ||||||||||||||
| 15. W3 Criminality | |||||||||||||||
Note: IA = inattentive symptoms; HI = hyperactive/impulsive symptoms; ODD = oppositional symptoms; SRD self-reported delinquency; ASB = antisocial behavior
For dichotomous variable, point-biserial correlation values are provided
p < .05
p < .01
p < .001
Hypothesis 1: Adolescent Externalizing Outcomes
Results of hierarchical regression analyses of W1 IA and HI as predictors of W2 externalizing behaviors are presented in Table 2. For each W2 outcome, the total variance accounted for by the overall model ranged from 6% (for Covert SRD) to a high of 41.9% (for Aggression). For all W2 outcomes, higher levels of childhood HI predicted higher levels of externalizing behavior, but this relation was significant only for Conduct Problems, Aggression, and Delinquency. After accounting for W1 IA, ODD and covariates, W1 HI contributed a significant amount of variance to W2 Conduct Problems, ΔR2 = .041, p = .002. Similarly, W1 HI uniquely accounted for 7.2% of the variance for W2 Aggression, p < .001, and 2.6% W2 Delinquency, p = .009. W1 HI did not predict W2 Covert or Overt SRD, or Deviant Peer Association. Of note, W1 IA was not a significant predictor of any W2 externalizing behavior; and for all but one outcome (W2 Delinquency), the associations were actually negative. Post-hoc analyses revealed that W1 HI also accounted for more variance in all W2 externalizing behaviors than did W1 ODD, with W1 ODD independently predicting only W2 Conduct Problems, ΔR2 = .038, p = .002, and W2 Aggression, ΔR2 = .045, p < .001.
Table 2.
Hierarchical Regressions: Predicting Adolescent Externalizing Behavior
| Wave 2 Outcome | Overall Model
|
Wave 1 Inattentiona
|
Wave 1 Hyperactivity/Impulsivityb
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F | df | p | R2 | F change | p | βc | ΔR2d | F change | p | βc | ΔR2e | |
| Conduct Problems | 7.28 | 8,193 | <.001 | .232 | 1.53 | .218 | −.19 | .006 | 10.23 | .002** | .56 | .041 |
| Aggression | 17.57 | 8,195 | <.001 | .419 | .27 | .602 | −.45 | .001 | 24.25 | <.001*** | 4.74 | .072 |
| Delinquency | 10.00 | 8,195 | <.001 | .291 | .29 | .593 | .45 | .001 | 7.05 | .009** | 2.51 | .026 |
| SRD - Covert | 4.24 | 8,191 | <.001 | .151 | 2.75 | .099 | −.22 | .012 | 2.10 | .149 | .22 | .009 |
| SRD - Overt | 1.59 | 8,191 | .130 | .062 | .46 | .497 | −.05 | .002 | 1.01 | .317 | .09 | .005 |
| Deviant Peers | 6.05 | 8,190 | <.001 | .203 | .22 | .637 | −.03 | .001 | 2.23 | .137 | .10 | .009 |
Note: SRD = self-reported delinquency.
p < .01;
p < .001
W1 Inattention entered at last step in model, after entering all covariates, W1 Oppositionality, and W1 Hyperactivity/Impulsivity
W1 Hyperactivity/Impulsivity entered at last step in model, after entering all covariates, W1 Oppositionality, and W1 Inattention
Beta reflects association to outcome variable after simultaneous control of all other variables in model
Change in R2 takes into account all covariates, W1 ODD, and W1 HI
Change in R2 takes into account all covariates, W1 ODD, and W1 IA
Hypothesis 1: Early Adult Externalizing Outcomes
Hierarchical regression analyses from W1 HI and IA to W3 externalizing behaviors are presented in Table 3. For each W3 continuous outcome, the overall model variance ranged from 7% (for W3 Covert SRD) to a high of 23.7% (for W3 ASB). Parallel to W2, for all W3 externalizing behaviors, higher levels of childhood HI predicted higher levels of early adult externalizing behavior. After adjusting for W1 covariates, as well as W1 IA and ODD, W1 HI independently accounted for a significant amount of W3 Conduct Problems, ΔR2 = .075, p < .001, W3 ASB, ΔR2 = .036, p = .003, and W3 Overt SRD, ΔR2 = .050, p = .001. After Bonferroni corrections, W1 HI did not attain significance for W3 Covert SRD, p = .045, ΔR2 = .019, or W3 Deviant Peer Associations, p = .038, ΔR2 = .021, in early adulthood, though effect sizes were moderate and in the expected direction. As was the case at W2, W1 IA did not account for W3 increases in any early adult externalizing behaviors. In fact, higher levels of W1 IA were marginally associated with lower levels of Overt SRD after applying a Bonferroni correction, ΔR2 = .030, p = .012, β = −.27.
Table 3.
Hierarchical Regressions: Predicting Early Adulthood Externalizing Behavior
| Wave 3 Outcome | Overall Model
|
Wave 1 Inattentiona
|
Wave 1 Hyperactivity/Impulsivityb
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F | df | p | R2 | F change | p | βc | ΔR2d | F change | p | βc | ΔR2e | |
| Conduct Problems | 5.35 | 8,200 | <.001 | .176 | 2.72 | .101 | −.26 | .011 | 18.23 | <.001*** | .79 | .075 |
| Antisocial Behavior | 7.75 | 8,200 | <.001 | .237 | .48 | .488 | .16 | .002 | 9.32 | .003** | .82 | .036 |
| SRD - Covert | 2.01 | 8,197 | .047 | .076 | .81 | .369 | −.15 | .004 | 4.07 | .045 | .38 | .019 |
| SRD - Overt | 2.69 | 8,197 | .008 | .099 | 6.48 | .012* | −.27 | .030 | 10.93 | .001** | .40 | .050 |
| Deviant Peers | 2.05 | 8,191 | .043 | .079 | .11 | .737 | .02 | .001 | 4.37 | .038 | .14 | .021 |
| Wave 3 Dichotomous Outcome | Overall Model
|
Wave 1 Inattentiona
|
Wave 1 Hyperactivityb
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| χ2 | p | n | OR | p | βc | OR | p | βc | |
| Criminality | 14.16 | .078 | 205 | .81 | .599 | −.22 | 1.41 | .414 | .34 |
Note: SRD = self-reported delinquency; OR = odds ratio
p < .05;
p < .01;
p < .001
W1 Inattention entered at last step in model, after entering all covariates, W1 Oppositionality, and W1 Hyperactivity/Impulsivity
W1 Hyperactivity/Impulsivity entered at last step in model, after entering all covariates, W1 Oppositionality, and W1 Inattention
Beta reflects association to outcome variable after simultaneous control of all other variables in model
Change in R2 takes into account all covariates, W1 ODD, and W1 HI
Change in R2 takes into account all covariates, W1 ODD, and W1 IA
Hypothesis 2: Moderation Effects
Moderation effects were tested for all significant outcomes found at W2 and W3 (for a total of 6 tests of moderation). Analyses revealed that mother’s Authoritarian Parenting moderated the effect of W1 HI on W2 Delinquency, ΔR2 = .037, p = .003. Examination of simple slopes (see Fig. 1) revealed that higher levels of mother’s Authoritarian Parenting (+1 SD) were associated with a higher association between childhood HI and W2 Delinquency, β = 5.2, compared to lower levels of Authoritarian Parenting (−1 SD), β = 1.1. A similar pattern emerged for W2 Aggression, ΔR2 = .017, p = .032, but this interaction was not significant after applying a Bonferroni correction. Analyses regarding W2 Conduct Problems did not reveal significant interactions. For early adult externalizing outcomes, only W3 Overt SRD showed a significant moderation effect, ΔR2 = .062, p < .001. However, examination of simple slopes revealed the opposite pattern from W2 (see Fig. 2): Higher levels of mother’s Authoritarian Parenting (+1 SD) were associated with a weaker relation between childhood HI and Overt SRD, β = .15, compared to lower levels of Authoritarian Parenting (−1 SD), β = .76. Neither W3 Conduct Problems nor W3 ASB revealed significant interactions.
Fig. 1.
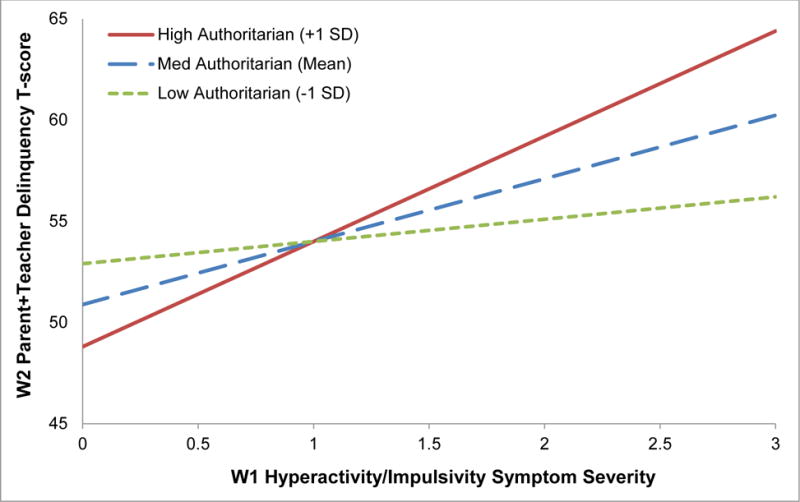
Adolescent delinquency (as reported by parents and teachers) as a function of childhood hyperactive/impulsive symptoms, grouped by level of mother’s authoritarian parenting (1 SD above mean, at mean, 1 SD below mean)
Fig. 2.
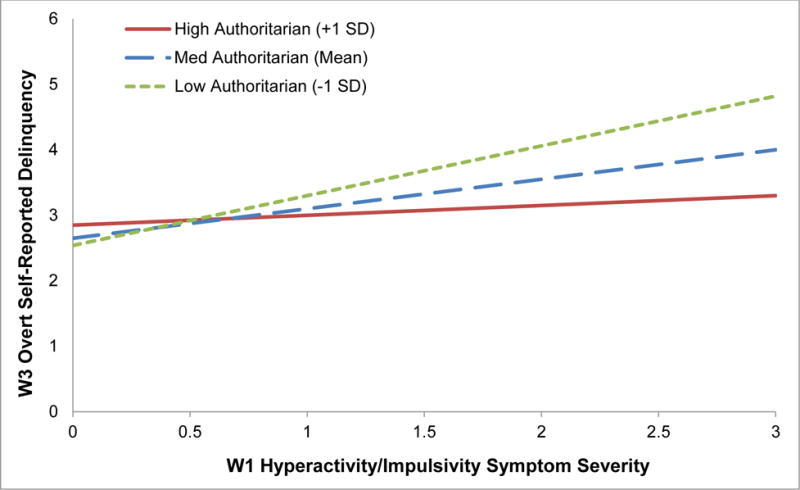
Early adult self-reported overt delinquency as a function of childhood hyperactive/impulsive symptoms, grouped by level of mother’s authoritarian parenting (1 SD above mean, at mean, 1 SD below mean)
Hypothesis 3: Mediation Effects
We conducted tests of indirect effects related to key adolescent (W2) externalizing behaviors as mediators of the association between childhood (W1) HI symptoms and early adult externalizing behaviors. We first tested separate mediational models for four W2 behaviors (Conduct Problems, Aggression, Delinquency, and Peer Conflict), by two W3 outcome variables (ASB and Criminality), for a total of 8 tests of mediation. For each, all W1 covariates were included in the model as well as W1 IA.
For the W3 outcome of ASB, only W2 Conduct Problems (Fig. 3a) and W2 Delinquency (Fig. 3b) were significant partial mediators. For W2 Conduct Problems, I.E. = .167, S.E. = .098, 95% CI = [.0117, .4043], the overall model accounted for 25% of the variance: F(7, 188) = 8.49, p < .001. For W2 Delinquency, I.E. = .157, S.E. = .090, 95% CI = [.0176, .3842], 22% of the variance was accounted for: F(7, 190) = 7.92, p < .001. With both W2 Conduct Problems and Delinquency in the same model, neither alone showed a significant indirect effect, but there was a significant overall indirect effect, I.E. = .201, S.E. = .108, 95% CI = [.0265, .4559]. Neither W2 Aggression nor W2 Peer Conflict mediated the association between W1 HI and W3 ASB, even though W1 HI was a significant predictor of W2 Peer Conflict via path a; ΔR2 = .034, Fchange = 8.83, p = .003 for HI, compared to ΔR2 = .029, Fchange = 7.55, p = .007 for ODD.
Fig. 3a.
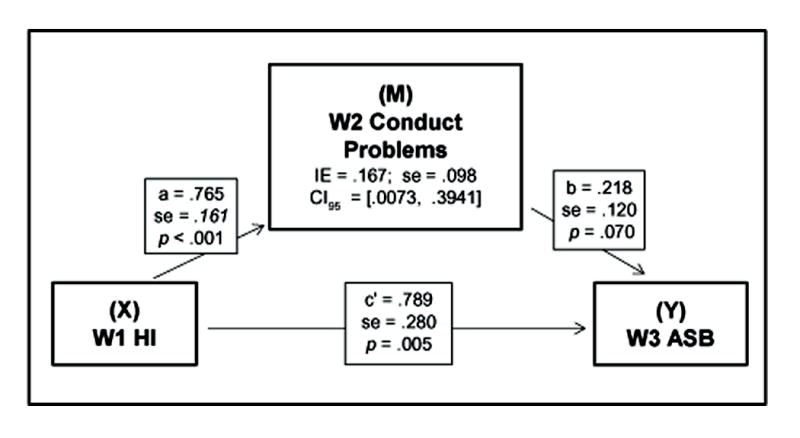
The relation between childhood hyperactive/impulsive symptoms and early adulthood antisocial behavior is mediated by adolescent conduct problems
Fig. 3b.
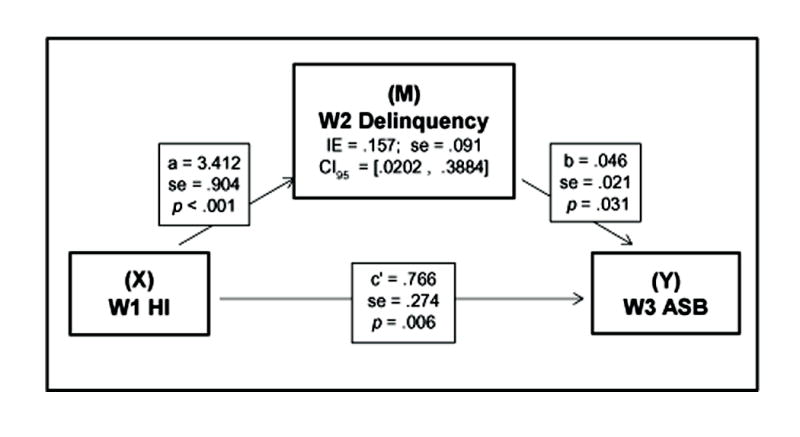
The relation between childhood hyperactive/impulsive symptoms and early adulthood antisocial behavior is mediated by adolescent delinquency
For the W3 outcome of Criminality, the only significant adolescent mediator was W2 Conduct Problems, I.E. = .387, S.E. = .181, 95% CI = [.0989, .7634]. Finally, we conducted a hypothesized multiple mediation test for W1 HI, parallel mediators of W2 Conduct Problems and W3 ASB, and the outcome of W3 Criminality (see Fig. 4). Both hypothesized mediators showed significant indirect effects when included in the same model; overall I.E. = .947, S.E. = .439, 95% CI = [.3568, 1.7601].
Fig. 4.
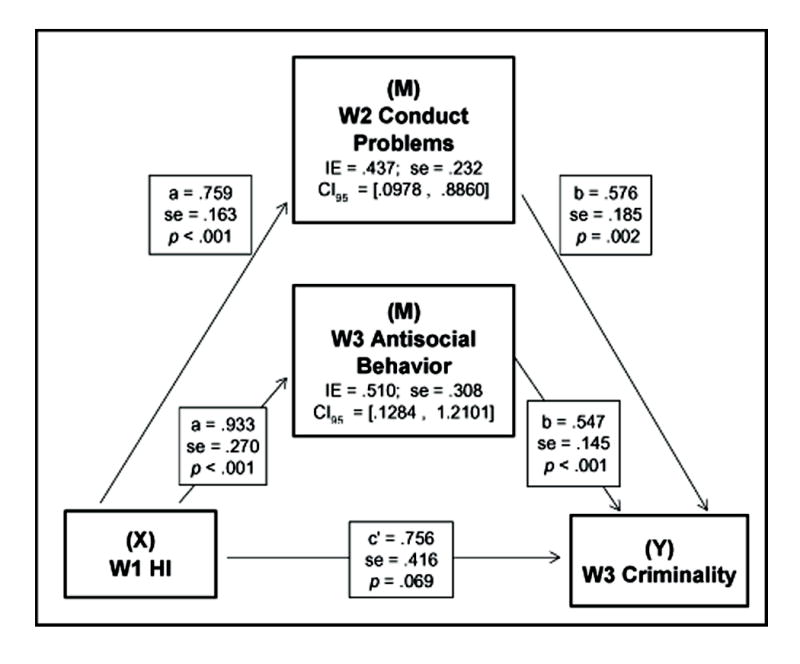
The relation between childhood hyperactive/impulsive symptoms and early adulthood criminal behavior is mediated by adolescent conduct problems and early adult antisocial behavior. For the overall model, IE = .946, se = .440, 95% CI = [.3636, 1.7794].
I.E. = indirect effect (a*b); se = standard error; CI = bias-corrected confidence interval; c’ = direct effect
Discussion
Our core objective was to leverage a model of trait impulsivity to examine childhood ADHD symptoms as a predictor of externalizing behavior into adolescence and early adulthood, via a large longitudinal sample of young women with and without childhood ADHD. Importantly, we utilized dimensional measures of IA and HI. The present findings support and clarify the trait impulsivity model, in that childhood ADHD symptoms were predictive of a number of later externalizing behaviors, including delinquency, aggression, and antisocial behavior. Further, these findings support the contention that HI symptoms, and not IA symptoms, predict later externalizing behavior (see Diamond, 2005; Ahmad & Hinshaw, 2016;). Indeed, in almost all cases, the regression slope between IA and a range of adolescent and early adult externalizing behaviors was close to zero or in fact negative. It may well be the case that once HI symptoms are taken into account, little residual variance is left for IA to predict such externalizing outcomes (Burns et al., 2014). On the other hand, with IA accounted for, HI symptoms continue to predict these outcomes at moderate to strong levels. We should note that, because we have included the stringent covariate of W1 ODD symptoms in our models, the effect sizes reported for our W1 HI predictor to various W2 and W3 outcomes may indeed underestimate the actual magnitude of prediction. For example, removing W1 ODD as a covariate when predicting W2 Conduct Problems, W1 HI variance increases from 4.1% to 7.8% (although overall model variance decreases from 23.2% to 19.3%). This is not surprising, given the shared liability between hyperactivity/impulsivity and oppositionality (Burns et al., 2014).
Our findings also support the contention that even though HI symptoms noticeably decline by early adulthood—in general and in the present sample (Faraone, Biederman, & Mick, 2006; Hinshaw et al., 2012)—heterotypic continuity of externalizing behaviors is salient in girls and young women. Of note, all the externalizing behaviors in adolescence that were significantly predicted by childhood HI were reported by parents/teachers, yet in early adulthood childhood HI significantly predicted behaviors reported by both parents and the young women themselves. These results are consistent with evidence that adolescents are less likely to accurately self-report externalizing behaviors, especially those who exhibit high levels of ADHD symptoms (Barkley, Fischer, Edelbrock, & Smallish, 1990; Sibley et al., 2010). In addition, regarding the self-reported delinquency measure, although mean levels of Covert Self-Reported Delinquency (e.g., lying, stealing, running away from home, destruction of property, etc.) for the overall sample did increase slightly from adolescence to early adulthood, there was no significant correlation or continuity in this behavior over time. Further, although mean levels of Overt Self-Reported Delinquency (indexing physical and violent behavior toward others) were relatively stable for the overall sample from adolescence to early adulthood, there was also no significant correlation between this adolescent and early adulthood behavior. These findings could imply that either individuals did not reliably self-report at both time points or that individual behaviors indeed changed over time (while leaving the overall sample means relatively unchanged).
We also tested moderators and mediators of the developmental progression of externalizing behavior. First, we found a moderating effect of parenting (Hypothesis 2), such that higher levels of mother’s authoritarian parenting during childhood were associated with delinquent behavior five years later (during adolescence) for girls with higher levels of childhood HI symptoms, compared to lower levels of authoritarian parenting. This finding is consistent with prior research showing that authoritarian parenting during childhood increases the risk of externalizing behavior in adolescence (Leve, Kim, & Pears, 2005; Thompson, Hollis, & Dagger, 2003). However, a surprising finding was that this association reversed five years later: By early adulthood, high levels of mother’s authoritarian parenting were associated with a prediction from childhood HI symptoms to lower levels of overt delinquency. There are at least two possible explanations. First, parents and teachers were the informants for the adolescent delinquency measure, whereas the young women self-reported in early adulthood (see Loeber, Green, Lahey, & Stouthamer-Loeber, 1991; Sibley et al., 2010). The previously noted adolescent under-reporting of externalizing behavior could plausibly continue into early adulthood, by which time some young women might be more accustomed to under-reporting these behaviors. Second, if the results cannot be explained by informant bias, it is possible that harsh/demanding parenting might actually be protective for girls with higher levels of HI once they enter early adulthood. In other words, for more hyperactive/impulsive girls, harsh parenting during childhood might elicit more externalizing behavior in adolescence—consistent with findings from Moffitt and colleagues (2001) regarding an increase in adolescent externalizing behavior for girls – but ultimately show the “intended” effect of subsequently decreasing such externalizing behavior by early adulthood. Such interpretations are speculative, given the lack of research on childhood parenting as a moderator of early adult externalizing behavior, especially in girls.
Mediational analyses (Hypothesis 3) also support the concept of heterotypic continuity in the developmental progression of externalizing behavior, with adolescent conduct and delinquent behaviors mediating the relation between (a) childhood HI and (b) young adult antisocial and criminal behaviors. There appears to be a developmental progression from childhood HI to adolescent conduct and delinquent behavior, and subsequently to early adult antisocial and criminal behavior—similar to findings in boys (Beauchaine et al., 2010; Forsman, Larsson, Andershed, & Lichtenstein, 2007; Loeber et al., 2009). Unexpectedly, adolescent peer conflict did not mediate the relation between childhood HI and early adult externalizing behavior, even though childhood HI was the single strongest predictor of adolescent peer conflict. It may be that more proximate mediating factors, such as school problems and deviant peers, played a more salient role in this developmental progression. Also, neighborhood information (which is important for deviant peer association; see Beyers, Bates, Pettit, & Dodge, 2003; Burke et al., 2002; Loeber & Hay, 1997) was not available. Overall, our findings support the importance of transactional, psychosocial factors in the development of externalizing behavior.
Importantly, the present study examined a range of externalizing behavior patterns, from overt vs. covert forms of delinquent behavior, indicators of criminality, and broad-band indicators of conduct problems. A core critique of categorical systems in defining externalizing behaviors is that they yield supposedly distinct syndromes, potentially inflating supposed comorbidity in conditions like ADHD (e.g., Beauchaine et al., 2010). It may well be that, via developmental, dimensional examinations of models like trait impulsivity, these supposedly distinct conditions actually reveal a form of heterotypic continuity, whereby core vulnerabilities (early appearing trait impulsivity) interact with a range of contextual factors, to yield an unfolding of progressively more severe forms of externalizing behavior with time. Finally, we were surprised at the lack of significant findings related to peer conflict as a potential mediator, despite childhood HI being strongly predictive of adolescent peer conflict. Perhaps, in the unfolding of externalizing behavior patterns over time, this factor is not as important as it has been shown in prior samples of males (Laird et al., 2001; but see also Okado & Bierman, 2014)
Several limitations are worth noting. Although behavioral measures are a critical component in identifying ADHD symptoms during childhood, no objective indicators of HI or IA were available for the present study. Such information warrants additional study. It is also unclear whether impulsivity or hyperactivity predicts externalizing behavior across development. One challenge with the DSM is that only 3 out of the 9 HI symptoms are related to impulsivity. Although ADHD-related symptoms (especially HI) decrease over time (Barkley, 2014; Faraone et al., 2006), space limitations precluded analysis of the continuity of IA and HI symptoms into adolescence and early adulthood (see, for example, Hinshaw et al., 2012; Miller, Loya, & Hinshaw, 2013; Owens & Hinshaw, 2016). Next, in order to follow developmentally appropriate measurement strategies, we used parent and teacher reports to index externalizing behavior prior to adulthood, but parent and self-reports for the W3 externalizing outcomes. Nearly all examinations of behavior disorders, across developmental spans, must contend with informant variance. It is clear that self-report is not optimal for capturing many ADHD-related and externalizing symptoms during childhood, but with the emergence of adulthood, better correspondence between parent- and self-reports has been observed (see Barkley, Murphy, & Fischer, 2008). Finally, given the time between each wave (roughly 5 years), a number of additional mediating factors were likely to affect developmental trajectories but could not be incorporated into the present models (e.g., substance use and academic/school problems).
Overall, our findings highlight the importance of identifying childhood symptoms of HI as a potential precursor to later, more severe delinquent, antisocial and potentially criminal behavior. Parenting factors are likely to interact with such behavioral vulnerability in predicting developmental trajectories (Beauchaine & McNulty, 2013). Findings also underscore the importance of investing in and providing greater access to early interventions – such as multimodal parent management training – as a preventive approach against later, more serious behaviors (Deault, 2010; Hoeve et al., 2009). The costs of failing to do so are significant, affecting not only the individual but also large public systems including law enforcement, juvenile and criminal justice, child social welfare, and educational systems (Foster et al., 2005; Pelham et al., 2007). An additional benefit of approaches involving parents is the opportunity to improve parenting practices, with positive influences on later behaviors (Beyers et al., 2003; Formoso, Gonzales, & Aiken, 2000). The transactional nature of child and adolescent psychopathology requires such attention to psychosocial processes in evidence-based treatments.
Supplementary Material
Acknowledgments
We are grateful to the young women who have participated in our longitudinal study, as well as the many research assistants, graduate students and staff who have made this research possible. We also thank Elizabeth Owens, Ph.D., Allison Harvey, Ph.D., and Ann Kring, Ph.D.
Funding Information: This research was supported by funding from National Institute of Mental Health Grants R01 45064 (to S.P.H.) and T32 MH089919 (to S.I.A).
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
References
- Achenbach TM. Manual for the child behavior checklist/4–18 and 1991 profile. Burlington, VT: Department of Psychiatry, University of Vermont; 1991a. [Google Scholar]
- Achenbach TM. Manual for the teacher’s report form and 1991 profile. Burlington, VT: Department of Psychiatry, University of Vermont; 1991b. [Google Scholar]
- Achenbach TM, Edelbrock CS. Psychopathology of childhood. Annual Review of Psychology. 1984;35:227–256. doi: 10.1146/annurev.ps.35.020184.001303. http://doi.org/10.1146/annurev.ps.35.020184.001303. [DOI] [PubMed] [Google Scholar]
- Ahmad SI, Hinshaw SP. Attention-deficit/hyperactivity disorder: Similarities to and differences from other externalizing disorders. In: Beauchaine TP, Hinshaw SP, editors. The Oxford handbook of externalizing spectrum disorders. New York: Oxford University Press; 2016. pp. 19–37. [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40(1):57–87. http://doi.org/10.1111/1469-7610.00424. [PubMed] [Google Scholar]
- Babinski DE, Pelham WE, Molina BSG, Gnagy EM, Waschbusch DA, Yu J, Karch KM. Late adolescent and young adult outcomes of girls diagnosed with ADHD in childhood: An exploratory investigation. Journal of Attention Disorders. 2011;15(3):204–214. doi: 10.1177/1087054710361586. http://doi.org/10.1177/1087054710361586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagwell CL, Molina BSG, Pelham WE, Hoza B. Attention-deficit hyperactivity disorder and problems in peer relations: Predictions from childhood to adolescence. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(11):1285–1292. doi: 10.1097/00004583-200111000-00008. http://doi.org/10.1097/00004583-200111000-00008. [DOI] [PubMed] [Google Scholar]
- Barkley RA. Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment. 4th. New York: Guilford Press; 2014. [Google Scholar]
- Barkley RA, Fischer M, Edelbrock CS, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria: I. An 8-year prospective follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry. 1990;29(4):546–557. doi: 10.1097/00004583-199007000-00007. http://doi.org/10.1097/00004583-199007000-00007. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Murphy KR, Fischer M. ADHD in adults: What the science says. New York: Guilford Press; 2008. [Google Scholar]
- Beauchaine TP, Hinshaw SP, Pang KL. Comorbidity of attention-deficit/hyperactivity disorder and early-onset conduct disorder: Biological, environmental, and developmental mechanisms. Clinical Psychology: Science and Practice. 2010;17(4):327–336. http://doi.org/10.1111/j.1468-2850.2010.01224.x. [Google Scholar]
- Beauchaine TP, McNulty T. Comorbidities and continuities as ontogenic processes: Toward a developmental spectrum model of externalizing psychopathology. Development and Psychopathology. 2013;25(4 Pt 2):1505–1528. doi: 10.1017/S0954579413000746. http://doi.org/10.1017/S0954579413000746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beyers JM, Bates JE, Pettit GS, Dodge KA. Neighborhood structure, parenting processes, and the development of youths’ externalizing behaviors: A multilevel analysis. American Journal of Community Psychology. 2003;31:35–53. doi: 10.1023/a:1023018502759. http://doi.org/10.1023/A:1023018502759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biederman J, Petty CR, Monuteaux MC, Fried R, Byrne D, Mirto T, Faraone SV. Adult psychiatric outcomes of girls with attention deficit hyperactivity disorder: 11-year follow-up in a longitudinal case-control study. American Journal of Psychiatry. 2010;167:409–417. doi: 10.1176/appi.ajp.2009.09050736. http://doi.org/10.1176/appi.ajp.2009.09050736. [DOI] [PubMed] [Google Scholar]
- Broidy LM, Tremblay RE, Brame B, Fergusson DM, Horwood JL, Laird RD, Vitaro F. Developmental trajectories of childhood disruptive behaviors and adolescent delinquency: A six-site, cross-national study. Developmental Psychology. 2003;39(2):222–245. doi: 10.1037//0012-1649.39.2.222. http://doi.org/10.1037/0012-1649.39.2.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke JD, Loeber R, Birmaher B. Oppositional defiant disorder and conduct disorder: A review of the past 10 years, part II. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41(11):1275–1293. doi: 10.1097/00004583-200211000-00009. http://doi.org/10.1097/00004583-200211000-00009. [DOI] [PubMed] [Google Scholar]
- Burns GL, de Moura MA, Beauchaine TP, McBurnett K. Bifactor latent structure of ADHD/ODD symptoms: Predictions of dual-pathway/trait-impulsivity etiological models of ADHD. Journal of Child Psychology and Psychiatry. 2014;55(4):393–401. doi: 10.1111/jcpp.12165. http://doi.org/10.1111/jcpp.12165. [DOI] [PubMed] [Google Scholar]
- Burt SA. Rethinking environmental contributions to child and adolescent psychopathology: A meta-analysis of shared environmental influences. Psychological Bulletin. 2009;135(4):608–637. doi: 10.1037/a0015702. http://doi.org/10.1037/a0015702. [DOI] [PubMed] [Google Scholar]
- Coghill D, Sonuga-Barke EJS. Annual research review: Categories versus dimensions in the classification and conceptualisation of child and adolescent mental disorders–implications of recent empirical study. Journal of Child Psychology and Psychiatry. 2012;53(5):469–489. doi: 10.1111/j.1469-7610.2011.02511.x. http://doi.org/10.1111/j.1469-7610.2011.02511.x. [DOI] [PubMed] [Google Scholar]
- Deault LC. A systematic review of parenting in relation to the development of comorbidities and functional impairments in children with attention-deficit/hyperactivity disorder (ADHD) Child Psychiatry and Human Development. 2010;41(2):168–92. doi: 10.1007/s10578-009-0159-4. http://doi.org/10.1007/s10578-009-0159-4. [DOI] [PubMed] [Google Scholar]
- Diamond A. Attention-deficit disorder (attention-deficit/hyperactivity disorder without hyperactivity): A neurobiologically and behaviorally distinct disorder from attention-deficit/hyperactivity disorder (with hyperactivity) Development and Psychopathology. 2005;17(3):807–825. doi: 10.1017/S0954579405050388. http://doi.org/10.1017/S0954579405050388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott DS, Huizinga D, Ageton SS. Explaining delinquency and drug use. Beverly Hills, CA: Sage Publications; 1985. [Google Scholar]
- Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: A meta-analysis of follow-up studies. Psychological Medicine. 2006;36:159–165. doi: 10.1017/S003329170500471X. http://doi.org/10.1017/S003329170500471X. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Perlis RH, Doyle AE, Smoller JW, Goralnick JJ, Holmgren MA, Sklar P. Molecular genetics of attention-deficit/hyperactivity disorder. Biological Psychiatry. 2005;57(11):1313–1323. doi: 10.1016/j.biopsych.2004.11.024. http://doi.org/10.1016/j.biopsych.2004.11.024. [DOI] [PubMed] [Google Scholar]
- Formoso D, Gonzales NA, Aiken LS. Family conflict and children’s internalizing and externalizing behavior: Protective factors. American Journal of Community Psychology. 2000;28(2):175–199. doi: 10.1023/A:1005135217449. http://doi.org/10.1023/A:1005135217449. [DOI] [PubMed] [Google Scholar]
- Forsman M, Larsson H, Andershed H, Lichtenstein P. The association between persistent disruptive childhood behaviour and the psychopathic personality constellation in adolescence: A twin study. British Journal of Developmental Psychology. 2007;25(3):383–398. http://doi.org/10.1348/026151006X158799. [Google Scholar]
- Foster EM, Jones DE, Conduct Problems Prevention Research Group The high costs of aggression: Public expenditures resulting from conduct disorder. American Journal of Public Health. 2005;95(10):1767–1772. doi: 10.2105/AJPH.2004.061424. JOUR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greven CU, Asherson P, Rijsdijk FV, Plomin R. A longitudinal twin study on the association between inattentive and hyperactive-impulsive ADHD symptoms. Journal of Abnormal Child Psychology. 2011;39(5):623–632. doi: 10.1007/s10802-011-9513-7. http://doi.org/10.1007/s10802-011-9513-7. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford Press; 2013. [Google Scholar]
- Heming G, Cowan PA, Cowan CP. Ideas about parenting. In: Touliatos J, Perlmutter BF, Straus MA, editors. Handbook of Family Measurement Techniques. Thousand Oaks, CA: Sage Publications; 1990. pp. 362–363. [Google Scholar]
- Hinshaw SP. On the distinction between attentional deficits/hyperactivity and conduct problems/aggression in child psychopathology. Psychological Bulletin. 1987;101(3):443–463. http://doi.org/http://dx.doi.org/10.1037/0033-2909.101.3.443. [PubMed] [Google Scholar]
- Hinshaw SP. Preadolescent girls with attention-deficit/hyperactivity disorder: I. Background characteristics, comorbidity, cognitive and social functioning, and parenting practices. Journal of Consulting and Clinical Psychology. 2002a;70(5):1086–1098. doi: 10.1037//0022-006x.70.5.1086. http://doi.org/10.1037/0022-006X.70.5.1086. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP. Process, mechanism, and explanation related to externalizing behavior in developmental psychopathology. Journal of Abnormal Child Psychology. 2002b;30(5):431–46. doi: 10.1023/a:1019808712868. http://doi.org/10.1023/A:1019808712868. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, Kranz R. The triple bind: Saving our teenage girls from today’s pressures. New York: Ballantine Books; 2009. [Google Scholar]
- Hinshaw SP, Melnick SM. Peer relationships in boys with attention-deficit hyperactivity disorder with and without comorbid aggression. Development and Psychopathology. 1995;7(4):627–647. http://doi.org/10.1017/S0954579400006751. [Google Scholar]
- Hinshaw SP, Owens EB, Sami N, Fargeon S. Prospective follow-up of girls with attention-deficit/hyperactivity disorder into adolescence: Evidence for continuing cross-domain impairment. Journal of Consulting and Clinical Psychology. 2006;74(3):489–499. doi: 10.1037/0022-006X.74.3.489. http://doi.org/10.1037/0022-006X.74.3.489. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, Owens EB, Zalecki C, Huggins SP, Montenegro-Nevado AJ, Schrodek E, Swanson EN. Prospective follow-up of girls with attention-deficit/hyperactivity disorder into early adulthood: Continuing impairment includes elevated risk for suicide attempts and self-injury. Journal of Consulting and Clinical Psychology. 2012;80(6):1041–1051. doi: 10.1037/a0029451. http://doi.org/10.1037/a0029451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinshaw SP, Scheffler RM. The ADHD explosion: Myths, medication, money, and today’s push for performance. New York: Oxford University Press; 2014. [Google Scholar]
- Hinshaw SP, Zupan BP, Simmel C, Nigg JT, Melnick S. Peer Status in boys with and without attention-deficit hyperactivity disorder: Predictions from overt and covert antisocial behavior, social isolation, and authoritative parenting beliefs. Child Development. 1997;68(5):880–896. doi: 10.1111/j.1467-8624.1997.tb01968.x. http://doi.org/10.2307/1132039. [DOI] [PubMed] [Google Scholar]
- Hoeve M, Dubas JS, Eichelsheim VI, Van Der Laan PH, Smeenk W, Gerris JRM. The relationship between parenting and delinquency: A meta-analysis. Journal of Abnormal Child Psychology. 2009;37(6):749–775. doi: 10.1007/s10802-009-9310-8. http://doi.org/10.1007/s10802-009-9310-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, Wang P. Research Domain Criteria (RDoC): Toward a new classification framework for research on mental disorders. American Journal of Psychiatry. 2010;167(7):748–751. doi: 10.1176/appi.ajp.2010.09091379. http://doi.org/10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Jensen PS. Comorbidity and child psychopathology: Recommendations for the next decade. Journal of Abnormal Child Psychology. 2003;31(3):293–300. doi: 10.1023/a:1023281513936. http://doi.org/10.1023/A:1023281513936. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters E. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. http://doi.org/http://dx.doi.org/10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, Benning SD, Kramer MD. Linking antisocial behavior, substance use, and personality: An integrative quantitative model of the adult externalizing spectrum. Journal of Abnormal Psychology. 2007;116(4):645–666. doi: 10.1037/0021-843X.116.4.645. http://doi.org/10.1037/0021-843X.116.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, Iacono WG. Externalizing psychopathology in adulthood: A dimensional-spectrum conceptualization and its implications for DSM–V. Journal of Abnormal Psychology. 2005;114(4):537–550. doi: 10.1037/0021-843X.114.4.537. http://doi.org/10.1037/0021-843X.114.4.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuja-Halkola R, Lichtenstein P, D’Onofrio BM, Larsson H. Codevelopment of ADHD and externalizing behavior from childhood to adulthood. Journal of Child Psychology and Psychiatry. 2015;56(6):640–647. doi: 10.1111/jcpp.12340. http://doi.org/http://dx.doi.org/10.1111/jcpp.12340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laird RD, Jordan KY, Dodge KA, Pettit GS, Bates JE. Peer rejection in childhood, involvement with antisocial peers in early adolescence, and the development of externalizing behavior problems. Development and Psychopathology. 2001;13(2):337–354. doi: 10.1017/s0954579401002085. http://doi.org/10.1017/S0954579401002085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsson JO, Larsson H, Lichtenstein P. Genetic and environmental contributions to stability and change of ADHD symptoms between 8 and 13 years of age: A longitudinal twin study. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(10):1267–1275. doi: 10.1097/01.chi.0000135622.05219.bf. http://doi.org/10.1097/01.chi.0000135622.05219.bf. [DOI] [PubMed] [Google Scholar]
- Lee SS, Hinshaw SP. Predictors of adolescent functioning in girls with attention deficit hyperactivity disorder (ADHD): The role of childhood ADHD, conduct problems, and peer status. Journal of Clinical Child and Adolescent Psychology. 2006;35(3):356–368. doi: 10.1207/s15374424jccp3503_2. http://doi.org/10.1207/s15374424jccp3503_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leve LD, Kim HK, Pears KC. Childhood Temperament and Family Environment as Predictors of Internalizing and Externalizing Trajectories From Ages 5 to 17. Journal of Abnormal Child Psychology. 2005;33(5):505–520. doi: 10.1007/s10802-005-6734-7. http://doi.org/10.1007/s10802-005-6734-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeber R, Burke JD, Pardini DA. Development and etiology of disruptive and delinquent behavior. Annual Review of Clinical Psychology. 2009;5:291–310. doi: 10.1146/annurev.clinpsy.032408.153631. http://doi.org/10.1146/annurev.clinpsy.032408.153631. [DOI] [PubMed] [Google Scholar]
- Loeber R, Farrington DP, Stouthamer-Loeber M, Van Kammen WB. Antisocial behavior and mental health problems: Explanatory factors in childhood and adolescence. Mahwah, NJ: Lawrence Erlbaum Associates; 1998. [Google Scholar]
- Loeber R, Green SM, Lahey BB, Stouthamer-Loeber M. Differences and similarities between children, mothers, and teachers as informants on disruptive child behavior. Journal of Abnormal Child Psychology. 1991;19(1):75–95. doi: 10.1007/BF00910566. [DOI] [PubMed] [Google Scholar]
- Loeber R, Hay D. Key issues in the development of aggression and violence from childhood to early adulthood. Annual Review of Psychology. 1997;48:371–410. doi: 10.1146/annurev.psych.48.1.371. http://doi.org/10.1146/annurev.psych.48.1.371. [DOI] [PubMed] [Google Scholar]
- Miller M, Loya F, Hinshaw SP. Executive functions in girls with and without childhood ADHD: Developmental trajectories and associations with symptom change. Journal of Child Psychology and Psychiatry. 2013;54(9):1005–1015. doi: 10.1111/jcpp.12074. http://doi.org/10.1111/jcpp.12074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A. Childhood predictors differentiate life-course persistent and adolescence-limited antisocial pathways among males and females. Development and Psychopathology. 2001;13(2):355–375. doi: 10.1017/s0954579401002097. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Rutter M, Silva P. Sex differences in antisocial behaviour: Conduct disorder, delinquency and violence in the Dunedin Longitudinal Study. New York: Cambridge University Press; 2001. [Google Scholar]
- Molina BSG, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS, Houck PR. The MTA at 8 years: Prospective follow-up of children treated for combined-type ADHD in a multisite study. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48(5):484–500. doi: 10.1097/CHI.0b013e31819c23d0. http://doi.org/10.1097/CHI.0b013e31819c23d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray J, Farrington DP. Risk factors for conduct disorder and delinquency: Key findings from longitudinal studies. Canadian Journal of Psychiatry. 2010;55(10):633–642. doi: 10.1177/070674371005501003. [DOI] [PubMed] [Google Scholar]
- Neuhaus E, Beauchaine TP. Impulsivity and vulnerability to psychopathology. In: Beauchaine TP, Hinshaw SP, editors. Child and adolescent psychopathology. 3rd. Hoboken, NJ: Wiley; in press. [Google Scholar]
- Okado Y, Bierman KL. Differential risk for late adolescent conduct problems and mood dysregulation among children with early externalizing behavior problems. Journal of Abnormal Child Psychology. 2014;43(4):735–747. doi: 10.1007/s10802-014-9931-4. http://doi.org/10.1007/s10802-014-9931-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens EB, Hinshaw SP. Childhood conduct problems and young adult outcomes among women with childhood attention-deficit/hyperactivity disorder (ADHD) Journal of Abnormal Psychology. 2016;125(2):220–232. doi: 10.1037/abn0000084. http://doi.org/10.1037/abn0000084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson GR. The early development of coercive family process. In: Reid JB, Patterson GR, Snyder J, editors. Antisocial behavior in children and adolescents: A developmental analysis and model for intervention. Washington, DC: American Psychological Association; 2002. pp. 25–44. http://doi.org/10.1037/10468-002. [Google Scholar]
- Pelham WE, Foster EM, Robb JA. The economic impact of attention-deficit/hyperactivity disorder in children and adolescents. Ambulatory Pediatrics. 2007;7(1S):121–131. doi: 10.1016/j.ambp.2006.08.002. http://doi.org/10.1016/j.ambp.2006.08.002. [DOI] [PubMed] [Google Scholar]
- Pettit GS, Bates JE, Dodge KA. Supportive parenting, ecological context, and children’s adjustment: A seven-year longitudianl study. Child Development. 1997;68(5):908–923. doi: 10.1111/j.1467-8624.1997.tb01970.x. [DOI] [PubMed] [Google Scholar]
- Piacentini JC, Cohen P, Cohen J. Combining discrepant diagnostic information from multiple sources: Are complex algorithms better than simple ones? Journal of Abnormal Child Psychology. 1992;20(1):51–63. doi: 10.1007/BF00927116. http://doi.org/10.1007/BF00927116. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Rothbaum F, Weisz JR. Parental caregiving and child externalizing behavior in nonclinical samples: A meta-analysis. Psychological Bulletin. 1994;116(1):55–74. doi: 10.1037/0033-2909.116.1.55. http://doi.org/10.1037/0033-2909.116.1.55. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39(1):28–38. doi: 10.1097/00004583-200001000-00014. http://doi.org/10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Sibley MH, Pelham WE, Molina BSG, Waschbusch DA, Gnagy EM, Babinski DE, Biswas A. Inconsistent self-report of delinquency by adolescents and young adults with ADHD. Journal of Abnormal Child Psychology. 2010;38(5):645–656. doi: 10.1007/s10802-010-9404-3. http://doi.org/10.1007/s10802-010-9404-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson JM. School-based assessments and interventions for ADD students. Irvine, CA: KC Publishing; 1992. [Google Scholar]
- Thompson A, Hollis C, Dagger DR. Authoritarian parenting attitudes as a risk for conduct problems. European Child & Adolescent Psychiatry. 2003;12(2):84–91. doi: 10.1007/s00787-003-0324-4. http://doi.org/10.1007/s00787-003-0324-4. [DOI] [PubMed] [Google Scholar]
- Tuvblad C, Zheng M, Raine A, Baker LA. A common genetic factor explains the covariation among ADHD ODD and CD symptoms in 9–10 year old boys and girls. Journal of Abnormal Child Psychology. 2009;37(2):153–167. doi: 10.1007/s10802-008-9278-9. JOUR. http://doi.org/10.1007/s10802-008-9278-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. Wechsler intelligence scale for children. 3rd. New York: The Psychological Corporation; 1991. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


