Abstract
Patient-provider communication impacts adherence to therapy. We explored older adults' communication with their providers, preferences for communication, and views on communication attributes and decision aid characteristics, by conducting four focus groups. Several participants reported they had received insufficient information about their sleep apnea diagnosis and treatment options. Most participants felt that it would be helpful to have treatment information tailored to their needs, including information on the negative impact of treatment on comfort and convenience and disclosure about common barriers to adherence. Participants provided desired characteristics for a decision aid, including their preferred delivery method, content, and format. These findings have implications for how to design useful decision aids for older adults with newly diagnosed sleep apnea.
Keywords: sleep apnea, communication, shared decision making, adherence
Background
Sleep apnea (SA) is prevalent among older adults, and positive airway pressure (PAP) therapy is the most commonly-prescribed therapy for it. Alternative therapies include oral appliances, surgical procedures, and nasal expiratory positive airway pressure. Although some patients are successfully treated with these therapies, many reject treatment entirely or have limited adherence due to physical (e.g., discomfort), psychosocial (e.g., lack of perceived need), and/or financial barriers (e.g., out-of-pocket costs) (Sawyer et al., 2011). When patients reject or do not adhere to treatment, they often receive no treatment, which is associated with sleep disturbance, daytime symptoms, and for some, increased cardiovascular morbidity and mortality (Martinez-Garcia et al., 2012). Several studies have examined technological, psychosocial, pharmacological, educational, and multidimensional strategies to improve acceptance and adherence to SA therapy (Smith, Dauz, Clements, Werkowitch, & Whitman, 2009; Aloia et al., 2001; Lettieri et al., 2009; Sparrow, Aloia, Demolles, & Gottlieb, 2010; Sawyer et al., 2011). Most of these strategies have focused on ways to improve adherence to PAP after the decision to prescribe PAP therapy has been made (Meurice et al., 2007; Golay et al., 2006).
Characteristics of the patient-provider relationship can influence adherence to therapies (Gallagher & Levinson, 2004). Provider explanations about a medical diagnosis or treatment are associated with favorable outcomes (Orth, Stiles, Scherwitz, Hennrikus, & Vallbona, 1987). Communication that elicits patient treatment preferences and goals of care and involves patients in selecting their therapy can promote adherence to therapy and improve patient satisfaction (Smith et al., 1998;Weiland et al., 2012). Engaging patients in discussions about treatment may be particularly helpful when the set of treatment options include a mixture of favorable and unfavorable attributes, as is the case for SA. Therefore, increasing the quality of patient-provider communication may be especially useful for SA patients.
Communication in the setting of consultative, specialty visits, which is the typical type of visit for SA, can be challenging. Most patients presenting with SA are meeting their sleep clinic providers for the first time, so the patient has not had an opportunity to discuss care goals with the provider (Collins et al., 2009). Sleep providers can learn about a patient's goals of care by reviewing medical records and talking with the patient during the visit, but a number of factors may limit the amount and type of information exchanged about the consequences of untreated SA and the risks and benefits of available SA treatment options. These factors include visit length and setting as well as patients' and providers' sociodemographics, attitudes regarding patients' rights to medical information, role expectations, preferences for communication and decision-making, and use of strategies to control the encounter such as changing topics, interrupting, and ignoring questions (Beisecker & Beisecker, 1990;Beisecker, 1990). Communication tools could facilitate discussions about goals of care and treatment options.
Patient decision aids are defined by the International Patient Decision Aid Standards Collaboration as “tools designed to help people participate in decision making about health care options” (International Patient Decision Aid Standards Collaboration, 2012). Decision aids can facilitate dialogue about disease and treatments, increase patient knowledge about treatment options, increase the accuracy of patients' risk perceptions about treatments, and improve patient-provider communication (Stacey et al., 2014). Most decision aids, which may be presented in formats such as videos, pamphlets, or web-based, include sections that specifically address the risks and benefits of treatment options (International Patient Decision Aid Standards (IPDAS) Collaboration, 2012). Decision aids that include a values clarification component increase the proportion of patients achieving decisions that are informed and consistent with their values and goals of care (Stacey et al., 2014). These decision aid effects may be particularly beneficial for individuals with multiple complex medical and psychiatric comorbidities, who may be forced to make more risk-benefit tradeoffs (e.g., a patient with upper extremity paralysis who needs help setting up PAP nightly may trade-off independence for a reduction in daytime sleepiness associated with PAP). A decision aid for adults with SA developed by researchers in Europe provides information on disease prevalence, risk factors, SA effects on daily life, and effects of different SA treatments.(Pelletier-Fleury, Gafni, Krucien, & Fleury, 2012) There are no known studies that have examined the patient-provider relationship as a determinant of SA treatment acceptance and adherence among older adults, a group more likely to have multiple complex medical and psychiatric comorbidities. In addition, older adults have been slower to adopt consumer health technologies and mobile devices than younger generations (LeRouge, Van, Seale, & Wright, 2014). No decision aids with content specifically tailored to an older adult population (e.g., SA treatment effects among adults > 65 years) are available.
The purpose of this study was to describe 1) older adult patients' perceptions of communication about SA occurring in encounters with sleep center staff and 2) older adult patients' beliefs, attitudes, and preferences for patient-provider communication styles and decision making regarding SA treatment. We also sought to explore older adult patients' desired characteristics for a tool (i.e., patient decision aid) for improving communication about SA and SA treatment options.
Methods
Study Participants and Recruitment
We conducted four focus groups of patients from two health systems (Department of Veterans Affairs [VA] and academic) in Los Angeles in April and May 2014. Both health systems have comprehensive sleep centers and offer the most common SA treatments (i.e., PAP, oral appliances, surgery). At both health systems, patients met individually with their physician, and patient education on SA was provided during the visits. Within the VA, respiratory therapists provided patients education about PAP equipment during one-on-one visits. In the academic health care system, information about PAP equipment was provided by durable medical equipment companies, whose education formats ranged from one-on-one to group visits. Although some of the providers have dual affiliations with the VA and the academic health system, the overwhelming majority of the physicians were providing care in only one of the healthcare care systems.
Recruitment posters and flyers were displayed in patient waiting areas at both health systems asking those interested to call our research center. A trained research staff member described the study and screened the patient for eligibility. Patients were eligible if they were 65 years or older, had been diagnosed with SA on a sleep study, and had not been told by a physician that they have dementia. The VA Greater Los Angeles Healthcare System and UCLA Health System institutional review boards approved the study (VA #2013-091198; UCLA #13-001132). Verbal consent was obtained at the time of the focus groups. Study participants were financially compensated for participation.
Theoretical Framework
The Theory of Planned Behavior (TPB) (Aizen, 1985) served as the overarching framework for the overall research study, which aims to develop a patient decision aid related to SA treatment. The research study began with the focus groups described in this paper. According to this framework, attitudes, subjective norms (e.g., referent beliefs about what behaviors others expect), and perceived behavioral control (e.g., perception of personal influences on the behavior and perceived difficulties performing the behavior) influence intention to use SA therapy, which in turn affects adherence to therapy. Adherence affects health outcomes. This framework was used to develop the focus group discussion guide.
Focus Group Sessions
The focus group sessions contained a mix of patients from both sites and were held in conference rooms at the VA. At the beginning of each session, participants completed a questionnaire asking for information about their SA treatment and demographic information. The focus groups were conducted by an experienced focus group moderator with content expertise in sleep medicine (JLM). Focus groups were conducted using a detailed guide of open-ended questions and covered three core issues: 1) types of patient-provider discourse that occurred when the patients first learned of their SA diagnoses, 2) preferences on discourse about SA diagnosis and treatment, including information the patients wish they had known about SA when they were first diagnosed with SA, and 3) perspectives on patient decision aids in the context of SA treatment (see Table 3). Participants were shown examples of patient decision aids developed for other medical conditions. Patient decision aid formats shown included paper, video, and online interactive content. The sessions lasted 90 minutes and were audio-recorded. After each session, the research staff (JLM, CHF, CT) discussed major themes that arose during the session and new understandings about the domains that emerged.
Table 3. Focus Group Discussion Guide.
1. Now I'd like you to think back to when you first learned that you have sleep apnea. Visualize yourself back in the room at a doctor's office, on the telephone, or wherever it was that you learned that you have sleep apnea.
|
2. I'd like you to think back to the weeks or months following your initial diagnoses with sleep apnea. Some of you may have started a treatment for sleep apnea, while others might not have. Tell me about what you did? How did that go?
|
| 3. We're developing an information tool to help patients understand the different options available to people with sleep apnea. The initial version will be a pen and paper version. It will contain pictures and text about the risks and benefits of different options. Questions within the tool will encourage patients to carefully consider whether each option matches their own personal healthcare goals. The tool is not meant to be a substitute for discussions with healthcare providers. Rather, it is a tool to encourage patients and healthcare providers to make informed decisions about healthcare, working together. What are your thoughts on a sleep apnea information tool like the one I just described?
|
Focus Group Data Analysis
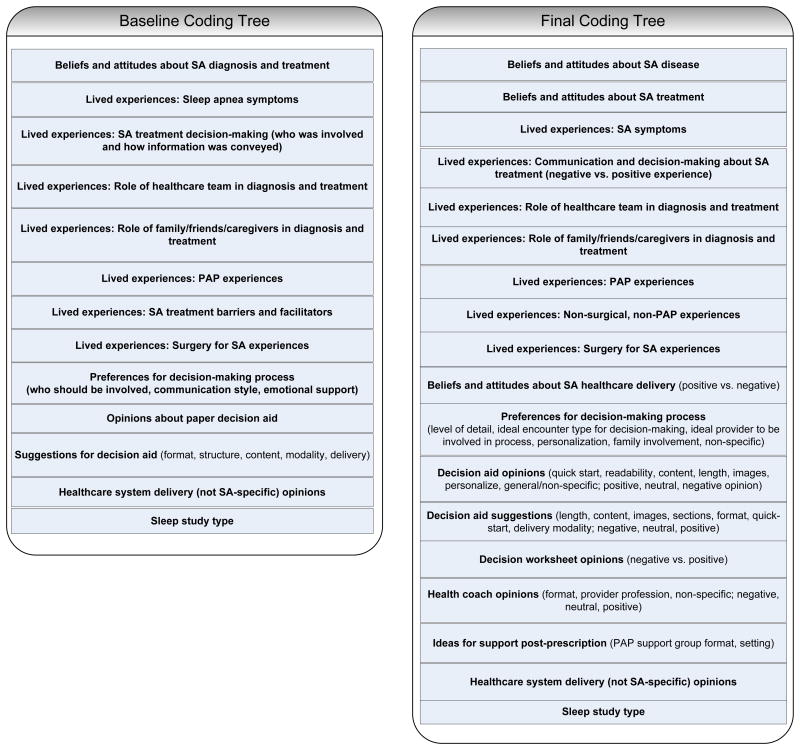
The audio-recordings were transcribed and subsequently reviewed by two team members (CHF, KJ) to identify major themes and to develop an initial coding tree (NVivo 10). During the development of the initial coding tree, coders were blinded to the codes of the other coder. The team (CHF, KJ, CT, JLM) discussed the coding tree during a group meeting and based upon this discussion, made modifications to the coding tree. Then, each transcript was read by two team members independently (CHF, KJ, and/or CT) and manually coded for instances of each code. The coding tree was iteratively revised as each transcript was coded until the coding tree was finalized. Differences in coding were discussed with a third team member and resolved by consensus. The baseline and final coding trees are presented in Figure 1. Throughout data analysis, we acknowledged the need to safeguard against preconceived ideas derived from clinical experience. To limit this risk, one of the team members who observed all of the focus groups, helped develop the coding tree, and coded the transcripts did not have prior direct clinical experience with patients with SA. We openly discussed whether the coding tree represented the key themes of the focus group discussions and whether the quotes selected for the manuscript are representative of the focus group content.
Figure 1. Baseline and final coding trees (SA=sleep apnea, PAP=positive airway pressure).
We examined frequencies of items from the questionnaires distributed to focus group participants. Those data were analyzed using Stata/SE13.1 (StatCorp LP, College Station, Texas).
Results
Description of Participants
Of the thirty-five patients (86% male) who participated (Table 1), 77% had only used PAP, while 20% had tried more than one type of SA therapy (Table 2). Eighty-eight percent of participants had been treated for at least one year. Half of the participants reported using their SA therapy nightly (Table 2). During the focus groups, participants discussed symptoms that were typical of SA (e.g., apneic episodes, excessive daytime sleepiness, nighttime awakenings, snoring, fatigue, and motor vehicle crashes) and described well-known mechanical barriers to SA therapy. Because most patients had used PAP only, the majority of comments were related to comfort and convenience barriers to the use of PAP. However, some patients who had tried oral appliances or surgery also described anatomical barriers to fitting oral appliances or undergoing surgery.
Table 1. Participant Demographic (N=35)*.
| Variable | Frequency (%) | |
|---|---|---|
| Gender | Male | 30 (86%) |
| Female | 5 (14%) | |
| Age | 65-69 years | 23 (66%) |
| 70-74 years | 7 (20%) | |
| 75 years or older | 5 (14%) | |
| Education | Less than high school | 2 (6%) |
| High school or equivalent | 3 (9%) | |
| Vocational/technical school (2-year) | 4 (11%) | |
| Some college | 14 (40%) | |
| Bachelor's degree | 8 (23%) | |
| Master's degree | 3 (9%) | |
| Doctoral degree | 1 (3%) | |
| Race/Ethnicity | White | 20 (57%) |
| Black | 4 (11%) | |
| Hispanic | 8 (23%) | |
| More than 1 race/ethnicity | 1 (3%) | |
| Missing | 10 (29%) | |
Participant demographics were similar across the focus groups, so data from the four focus groups were pooled together.
Table 2. Participant Treatment Characteristics (N=35).
| Variable | Frequency (%) |
|---|---|
| Sleep apnea therapy | |
| Positive airway pressure only | 27 (77%) |
| Oral appliance only | 1 (3%) |
| Positive airway pressure and oral appliance | 5 (14%) |
| Positive airway pressure and nasal expiratory positive airway pressure | 2 (6%) |
| Treatment duration | |
| < 1 year | 3 (9%) |
| 1-5 years | 11 (31%) |
| 5-10 years | 8 (23%) |
| >10 years | 12 (34%) |
| Don't know | 1 (3%) |
| Self-report therapy use (past 30 days) | |
| Every night | 18 (51%) |
| Most nights | 7 (20%) |
| Some nights | 5 (14%) |
| No nights | 5 (14%) |
Description of Communication Between Patients and Healthcare Providers
Communication about the causes of SA and the risks of living with SA ranged from very negative to very positive. Participant responses indicated a desire to have more information when receiving the diagnosis for the first time, including an explanation of the implications of having a SA diagnosis, the risks of not adhering to therapy, and how to use the PAP device.
-
Positive experiences: Some participants clearly remembered receiving their diagnosis of SA and/or discussing the risks of untreated SA, even in cases diagnosed more than one year ago. In some cases, the patient was simply told that she/he had a SA diagnosis, but in other cases, a description of SA and the risks of untreated SA were conveyed:
“[The doctor] said ‘I want to explain to you what we've found in the tests that you took home.’ He says, ‘You have sleep apnea.’”
“You definitely have sleep apnea. And I said, ‘Why do you say that?’ He said, 'Because I ran this test on you all night. And your heart [sic] stopped at least 80 times in the first hour. And one of these times, without some kind of help, you're going to fade away.”
-
Negative experiences: Other participants recalled that very little information was provided, and communication about SA and the risks of untreated SA prior to being given a PAP device was limited:
“They just checked me over and sent me home.”
“I went to my doctor, explained to him I was having problems sleeping. They sent me here for the test. My doctor got back to me and brought me back out here. Just told me that I have sleep apnea and to come pick up the machine. And I picked it up.”
Similarly, communication about the available treatment options and the risks and benefits of SA treatments also varied.
-
Positive experiences: In these discussions, providers informed patients about the reason for using or not using a particular therapy and acknowledged that more than one option was available:
“They said it was better for your heart and things like that.”
“Then he laid out the different options I had. Surgery, which he did not recommend because he says it usually doesn't work. He talked about the CPAP machine. And then a dental thing. And told me the main reason of using such a tool is besides not sleeping well, he explained that it affects your heart. You could have a …heart attack, because you're putting a lot of stress on your heart because you're not breathing.”
-
Negative experiences: These discussions were characterized by a lack of exchange of information about treatment options in general and about second- and third-line options:
“I was told CPAP or nothing.”
“I asked if there was any other treatment. The only thing they said was a CPAP machine and different masks. That's it.”
“They gave the CPAP, and that was my only option. But that's not true. There's many, many options.”
Participants' Beliefs, Attitudes, and Preferences for Patient-Provider Communication and Decision-Making
Some participants believed that they should be provided with more information about their diagnosis and treatment to make them more knowledgeable, which in turn could provide them with more power over their condition and make the decision-making process a joint effort.
“We need to know in detail.”
“Knowledge is power. When you know something, you're able to handle it better and make better decisions. And you feel less anxious and nervous about things if you understand.”
“I just think it's a joint effort.”
However, some participants' attitudes reflected skepticism that physicians would provide more details about SA diagnosis and treatment due time constraints, physician tactics to limit their question asking, and lack of consideration of their overall health concerns.
“The doctors don't have time.”
“Most doctors will say, okay, this is it. Here's your paper, sign here.”
“They don't take into consideration, nor do they look into your medical records to find out what is the real problem.”
Participants expressed their expectations and preferences for patient-provider communication in the context of SA diagnosis and treatment.
-
Provide more details: The vast majority felt that more details would be helpful:
“I'd like to have the doctor explain to me the diagnosis, not just from saying, well, you have this and this is to happen. No, tell me how, what and when and what I can do to take care of it.”
“I want options. At least I'll know if this is not working, there's someplace else to go, instead of giving up for an extended period of time.”
-
Fully disclose the common barriers to treatment: Several participants wanted healthcare providers to be up front about barriers to therapy and to provide anticipatory guidance about the therapies and about alternative therapies.
“This problem here is the sales pitch. Initially, it's oh, oh, wow, I'm totally sold on the CPAP as my treatment. Then, wait, I realize I've got to wear this mask? Where was the mask in the sales pitch? The providers are not truthful up front.”
“You should not hide the negatives. You're up front, maybe right from the beginning.”
-
Tailor the information: Participants expressed a desire for information about treatment options to be specifically tailored to each patient's needs and communicated with a personal touch. They also wanted to know which option is recommended for their particular situation:
“Some people have personal issues with claustrophobia (or other conditions that may be a barrier). You need to address that.”
“It should be a personal interaction.”
“I just want the healthcare professional that's going to have learned all this stuff, when they tell me this is what will work for you. I'm going to say okay. If this is what it's going to be, this is what it'll be. And if it doesn't work, then I tell them this isn't working. Then I figure it's their place to come up with the next step.”
Participants' Perspectives About Decision Aids
Participants provided a variety of perspectives about their level of interest in a SA decision aid. Most participants expressed interest in a SA decision aid. They felt that information provided about SA and treatment options to newly-diagnosed patients could help patients communicate with providers about their disease and treatment options. However, a few participants felt that they could obtain information through existing sources on the Internet or that the sleep center provider should already be providing the information without the use of a decision aid.
“A lot of people, they don't understand what's going on. That's why you think they don't ask questions and get to the bottom of it.”
“Wish I would've had this decision aid at the beginning.”
“It seems to me that what you're suggesting—this information about SA— just Google it.”
“Why can't the person that's talking to you—the doctor—give you all this information, without making another step of people that have to go through all this?”
“A technician could take time to explain.”
Participants described the types of decision aid characteristics that would make a decision aid useful. As shown in Table 4, these characteristics align with the participants' communication preferences, beliefs, and attitudes described above.
Table 4. Crosswalk: Communication Preferences – Decision Aid Characteristics.
| Communication Preferences | Decision Aid Characteristics |
|---|---|
| Provide details of diagnoses, treatment options, risks of failing to adhere to treatments, | Content: List and provide details of treatment options. Describe risks of untreated sleep apnea. |
| Disclose common barriers to treatment | Provide information about the most common barriers to treatment. |
| Tailor information | Provide both general information about sleep apnea as well as patient-specific information. |
| Provide a variety of delivery methods |
|
-
Content describing OSA and treatment options: Participants agreed that they would like to see a list of the treatment options and relevant questions that might be discussed with a provider. Not only did they want a description of the options, they also wanted information about what might happen if the SA is left untreated.
“Do a FAQ, because that would be efficient. The same questions everybody's going to ask in the beginning.”
“What does it do to your body if you don't use this? Because a lot of people don't know that.”
-
Content describing common barriers to treatment:
“A page that says you're home, you're frustrated, and you've stopped using the machine: a reinforcement.”
“If you have dry mouth, this should be addressed. If you develop dry mouth, these are our suggestions and recommendations.”
-
Content tailored to individual needs:
“I think what's more valuable are questions that you might be discussing with your doctor, like, I'm claustrophobic.”
“Part of this book should be general for everybody. But then also a section should be separate just for the individual and his issues.”
-
Delivery modality: The participants provided a range of recommendations on the method for delivering a decision aid. Some suggested an in-person group format that would include patients who already have SA and could share their experiences with newly-diagnosed patients, whereas others wanted to access the decision aid and worksheet at home through a DVD or the Internet.
“Why not have a group that we can discuss sleep apnea?”
“If you are going to have a discussion with brand-new people, then it would be very important to have one or two or however many you think who are already using it, to help with the explanation and share their experiences.”
“Well, can you also make it available so somebody can punch it in their computer and read it?”
“Just give them a CD.”
“One program on a website would save a whole lot.”
“I would much rather have a video than paper and pencil.”
-
Format (i.e., length, visual appearance, readability): Many participants expressed a preference for a decision aid that is short in length and felt that a summary sheet (e.g., a quick start guide) would be helpful. They felt that a format that would enable them to quickly choose just the sections relevant to them would be helpful. Illustrations and images were suggested.
“Lots of illustrations.”
“A lot of people don't read anymore at all, you know.”
Discussion
We found that patients' perceptions of communication about SA with their sleep providers ranged widely. We also found that older patients desire information about the risks of untreated SA disease when they are initially diagnosed, their treatment options (not just the first-line option), and the most common barriers to treatment. Study participants expressed an interest in a patient decision aid for improving communication about SA and SA treatments and offered suggestions for making the patient decision useful and easy to use.
For many participants, the exchange of information about their SA diagnosis consisted of brief, declarative statements (“you've got sleep apnea”), while others received a description about the physiological effects of the SA diagnosis (e.g., number of apneas per hour) and risks of untreated SA (e.g., death). Of note, these comments reflect participants' perceptions of the discussion about their SA diagnosis rather than actual recordings of the discussion that occurred. Communication about the availability of treatment options varied. Many discussions were framed as if PAP were the only treatment option for SA, which led one patient who rejected his PAP to forego any treatment for an extended period, because he was not aware that other options were available and therefore, did not follow up with his provider. Our results suggest that some patients are not informed consumers of their sleep apnea treatment, which has important ethical and quality of care implications that deserve attention. The American Academy of Sleep Medicine's clinical guidelines for the long-term care of SA therapy state that “the patient should be an active participant in the decision on treatment type and taught to contribute to the management of his or her own disease.”(Epstein et al., 2009, page 268). In contrast, other participants described a discussion that included a set of choices (i.e., PAP plus other treatment options). For some participants, the discussion about treatment options was personalized, factoring in the individual's other healthcare issues and personal preferences. However, in other cases, the discussion felt like a “one size fits all” approach. Our findings are similar to reports from studies of other conditions, which suggest a lack of involvement in the decision-making process for some patients. For example, a study involving decision making in physical therapy found that shared decision-making was not common, although patients expressed a preference for this approach (Dierckx, Deveugele, Roosen, & Devisch, 2013).
We elicited the types of content that patients want when they receive their SA diagnosis. Patients want information about the effects of untreated SA presented to them at the time of diagnosis. There was a general consensus that patients should be informed by their healthcare providers about the availability of different treatment options, not just the first-line option. These results are similar to those reported from a population-based survey of preferences for decision making, in which 96% of respondents indicated a preference to be offered choices and to be asked for their opinions (Levinson, Kao, Kuby, & Thisted, 2005). Information to promote self-management and troubleshooting of SA device-associated problems was also considered important to many study participants to help them with their daily decisions about whether or not to use their therapy. Our results suggest that patients also want to know if the treatment modality will be optimal for their specific situation.
This study supports the development of strategies to improve communication about SA and its therapies. Our findings are similar to those reported by Goff and colleagues, who conducted in-depth interviews with patients to explore patients' beliefs and preferences about medications to uncover factors that contribute to medication adherence (Goff, Mazor, Meterko, Dodd, & Sabin, 2008) . They found that patients wanted to know their medication options and understand the risks and benefits of each option and that lack of communication decreased confidence in a physician's recommendations. Our results are also similar to those found by Lau and colleagues, who studied medication adherence among older women with osteoporosis. They identified information exchange and relationships with health care providers as key factors that influence adherence to therapy (Lau et al., 2008). Prior studies have found empirical evidence supporting a link between communication and adherence. A meta-analysis of empirical studies on physician's communication and patient adherence found that poor communication is associated with a 19% higher risk of non-adherence and that training physicians in communication skills results in a 1.62 higher odds of patient adherence compared with no training (Zolnierek & Dimatteo, 2009). A tool that improves communication between older patients and their sleep health care providers has the potential to influence patients' knowledge and attitudes towards SA treatments and acceptance and adherence to SA therapy, although a recent Cochrane Database Review on decision aids found that the effects of decision aids on adherence are inconclusive (Stacey et al., 2014). Since studies suggest that adherence levels are determined early in the course of SA treatment (Weaver & Grunstein, 2008), a strategy implemented at the time of diagnosis is ideal. Participants voiced a desire for information about SA treatment options relevant to their conditions and were receptive to a patient decision aid/health promotion tool. A decision aid specific to older adults that offers SA information that is derived from studies that included older adults, who often have comorbid conditions, may be needed. Participants differed in preferences when discussing the format for delivering this tool. Some felt that a face-to-face, group format would be an efficient delivery method, while others felt that online or DVD formats that could be accessed at home would be better. Many participants were skeptical that their physicians would be able to provide sufficient information about the different treatment options during a typical clinic visit.
The main limitation of this study is that the participants were recruited using convenience sampling from only two different healthcare systems (both located in the same city) and most participants were male. This sampling strategy may have resulted in omission of extreme or deviant perspectives on the topic, thereby limiting generalizability of the findings. Another limitation is that we did not directly observe or record patient-provider encounters. Patient recall may differ from actual patient-provider encounters. Studies suggest that patients often recall only a fraction of the content discussed with their provider (Flocke & Stange, 2004). The length of time that elapsed between the focus groups and the initial discussion about diagnosis and treatment, which was probably > 10 years for one-third of participants, may have further reduced patient recall. However, even if patients did receive information about treatment options, the discussion and content were not memorable. We did not perform validation checks with participants or field experts. This qualitative study's sample size was not sufficient for quantitatively estimating the frequencies of the different types of patient-provider communication patterns or the number of patients who prefer certain types of decision making styles and due to the qualitative design, the study did not include standardized measures of patient-provider communication. Finally, some participants described healthcare system and payer issues they encountered, but because the focus group discussions emphasized the discourse between the patient and provider, these comments were too limited to analyze; future studies should explore the impact of insurance and other structural issues.
In conclusion, we explored the ways in which the diagnosis of SA was communicated with patients and the types of information patients received about treatment options. We learned that many patients received little information about their diagnosis and were not informed about alternative treatment options. Participants were enthusiastic about a patient decision aid, which would provide information about SA and treatment options. These findings suggest that a decision aid could improve patient-provider communication about SA treatments and help older adults with SA make decisions about their care that would be better informed and participatory in nature.
Acknowledgments
Research reported in this publication was supported by The Beeson Career Development in Aging Research Award Program (K23AG045937), the National Institute on Aging, American Federation for Aging Research, The John A. Hartford Foundation, and The Atlantic Philanthropies. Ron D. Hays was supported in part by the NIA (P30-AG021684) and the NIMHD (2 P20-MD000182).
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Aizen I. Action control: From cognition to behavior. New York: Springer-Verlag; 1985. From intentions to actions: A theory of planned behavior; pp. 11–39. [Google Scholar]
- Aloia MS, Di DL, Ilniczky N, Perlis ML, Greenblatt DW, Giles DE. Improving compliance with nasal CPAP and vigilance in older adults with OAHS. Sleep Breath. 2001;5:13–21. doi: 10.1007/s11325-001-0013-9. [DOI] [PubMed] [Google Scholar]
- Beisecker AE. Patient power in doctor-patient communication: What do we know? Health Commun. 1990;2:105–122. [Google Scholar]
- Beisecker AE, Beisecker TD. Patient information-seeking behaviors when communicating with doctors. Med Care. 1990;28:19–28. doi: 10.1097/00005650-199001000-00004. [DOI] [PubMed] [Google Scholar]
- Collins J, Farrall E, Turnbull DA, Hetzel DJ, Holtmann G, Andrews JM. Do we know what patients want? The doctor-patient communication gap in functional gastrointestinal disorders. Clin Gastroenterol Hepatol. 2009;7:1252–4. 1254. doi: 10.1016/j.cgh.2009.06.025. [DOI] [PubMed] [Google Scholar]
- Dierckx K, Deveugele M, Roosen P, Devisch I. Implementation of shared decision making in physical therapy: observed level of involvement and patient preference. Phys Ther. 2013;93:1321–1330. doi: 10.2522/ptj.20120286. [DOI] [PubMed] [Google Scholar]
- Epstein LJ, Kristo D, Strollo PJ, Jr, Friedman N, Malhotra A, Patil SP, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5:263–276. [PMC free article] [PubMed] [Google Scholar]
- Flocke SA, Stange KC. Direct observation and patient recall of health behavior advice. Prev Med. 2004;38:343–349. doi: 10.1016/j.ypmed.2003.11.004. [DOI] [PubMed] [Google Scholar]
- Gallagher TH, Levinson W. A prescription for protecting the doctor-patient relationship. Am J Manag Care. 2004;10:61–68. [PubMed] [Google Scholar]
- Goff SL, Mazor KM, Meterko V, Dodd K, Sabin J. Patients' beliefs and preferences regarding doctors' medication recommendations. J Gen Intern Med. 2008;23:236–241. doi: 10.1007/s11606-007-0470-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golay A, Girard A, Grandin S, Metrailler JC, Victorion M, Lebas P, et al. A new educational program for patients suffering from sleep apnea syndrome. Patient Educ Couns. 2006;60:220–227. doi: 10.1016/j.pec.2005.01.007. [DOI] [PubMed] [Google Scholar]
- International Patient Decision Aid Standards (IPDAS) Collaboration. 2012 Update of the IPDAS Collaboration Background Document. 2012 doi: 10.1177/0272989X211035681. Retrieved from http://ipdas.ohri.ca/resources.html. [DOI] [PMC free article] [PubMed]
- International Patient Decision Aid Standards Collaboration. What are Patient Decision Aids? 2012 Jun 20; Retrieved from http://ipdas.ohri.ca/what.html.
- Lau E, Papaioannou A, Dolovich L, Adachi J, Sawka AM, Burns S, et al. Patients' adherence to osteoporosis therapy: exploring the perceptions of postmenopausal women. Can Fam Physician. 2008;54:394–402. [PMC free article] [PubMed] [Google Scholar]
- LeRouge C, Van SC, Seale D, Wright K. Baby boomers' adoption of consumer health technologies: survey on readiness and barriers. J Med Internet Res. 2014;16:e200. doi: 10.2196/jmir.3049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lettieri CJ, Shah AA, Holley AB, Kelly WF, Chang AS, Roop SA. Effects of a short course of eszopiclone on continuous positive airway pressure adherence: a randomized trial. Ann Intern Med. 2009;151:696–702. doi: 10.7326/0003-4819-151-10-200911170-00006. [DOI] [PubMed] [Google Scholar]
- Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making. A national study of public preferences. J Gen Intern Med. 2005;20:531–535. doi: 10.1111/j.1525-1497.2005.04101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez-Garcia MA, Campos-Rodriguez F, Catalan-Serra P, Soler-Cataluna JJ, Almeida-Gonzalez C, De la CMI, et al. Cardiovascular mortality in obstructive sleep apnea in the elderly: role of long-term continuous positive airway pressure treatment: a prospective observational study. Am J Respir Crit Care Med. 2012;186:909–916. doi: 10.1164/rccm.201203-0448OC. [DOI] [PubMed] [Google Scholar]
- Meurice JC, Ingrand P, Portier F, Arnulf I, Rakotonanahari D, Fournier E, et al. A multicentre trial of education strategies at CPAP induction in the treatment of severe sleep apnoea-hypopnoea syndrome. Sleep Med. 2007;8:37–42. doi: 10.1016/j.sleep.2006.05.010. [DOI] [PubMed] [Google Scholar]
- Orth JE, Stiles WB, Scherwitz L, Hennrikus D, Vallbona C. Patient exposition and provider explanation in routine interviews and hypertensive patients' blood pressure control. Health Psychol. 1987;6:29–42. doi: 10.1037//0278-6133.6.1.29. [DOI] [PubMed] [Google Scholar]
- Pelletier-Fleury N, Gafni A, Krucien N, Fleury B. The development and testing of a new communication tool to help clinicians inform patients with obstructive sleep apnoea syndrome about treatment options. J Sleep Res. 2012;21:577–583. doi: 10.1111/j.1365-2869.2012.01015.x. [DOI] [PubMed] [Google Scholar]
- Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver TE. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev. 2011;15:343–356. doi: 10.1016/j.smrv.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith CE, Dauz E, Clements F, Werkowitch M, Whitman R. Patient education combined in a music and habit-forming intervention for adherence to continuous positive airway (CPAP) prescribed for sleep apnea. Patient Educ Couns. 2009;74:184–190. doi: 10.1016/j.pec.2008.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith RC, Lyles JS, Mettler J, Stoffelmayr BE, Van Egeren LF, Marshall AA, et al. The effectiveness of intensive training for residents in interviewing. A randomized, controlled study. Ann Intern Med. 1998;128:118–126. doi: 10.7326/0003-4819-128-2-199801150-00008. [DOI] [PubMed] [Google Scholar]
- Sparrow D, Aloia M, Demolles DA, Gottlieb DJ. A telemedicine intervention to improve adherence to continuous positive airway pressure: a randomised controlled trial. Thorax. 2010;65:1061–1066. doi: 10.1136/thx.2009.133215. [DOI] [PubMed] [Google Scholar]
- Stacey D, Legare F, Col NF, Bennett CL, Barry MJ, Eden KB, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2014;1:CD001431. doi: 10.1002/14651858.CD001431.pub4. [DOI] [PubMed] [Google Scholar]
- Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5:173–178. doi: 10.1513/pats.200708-119MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiland A, Van de Kraats RE, Blankenstein AH, Van Saase JL, Van der Molen HT, Bramer WM, et al. Encounters between medical specialists and patients with medically unexplained physical symptoms; influences of communication on patient outcomes and use of health care: a literature overview. Perspect Med Educ. 2012;1:192–206. doi: 10.1007/s40037-012-0025-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47:826–834. doi: 10.1097/MLR.0b013e31819a5acc. [DOI] [PMC free article] [PubMed] [Google Scholar]