Abstract
Extragnathic xanthomas are seen in the bones or as soft tissue masses. They are often associated with hyperlipidemia and are considered as reactive or metabolic lesions. Only 19 cases of xanthomas of the jaws have been reported so far in the English literature. A total of ten cases of central xanthoma of the jaw bones were identified from the Oral and Maxillofacial Pathology biopsy services of the University of Washington and the Tufts University School of Dental Medicine, between the years 2000–2016. The demographic and clinical information on these cases was tabulated logically on the basis of age, gender, location and presence or absence of symptoms, extragnathic lesions and serum hyperlipidemia. Radiographic and histopathological features were also examined. The findings in these cases were correlated with those available from the previously reported cases. Majority of cases are seen in the second and third decades of life. There is no gender predilection. Jaw lesions presented as solitary radiolucencies with a predilection for the posterior mandible. Unlike maxillary lesions, pain and expansion are inconsistent findings in mandibular lesions. Jaw lesions are not associated with extragnathic bone or soft tissue involvement or a hyperlipidemia. The central xanthoma of the jaws is a unique benign tumor. Histopathologically, many other jaw lesions contain variable numbers of foamy histiocytes. Therefore, a diagnosis of a central xanthoma of the jaws must be made after excluding all other such histiocyte containing lesions. This requires correlation of histopathological findings with clinical and radiographic features.
Keywords: Xanthoma, Jaw, Gnathic, Bones, Central, Histiocytes
Introduction
A xanthoma is a rare soft tissue and bone condition consisting of a predominant collection of lipid-rich foamy histiocytes. Lesions have been described in the axial and appendicular bones in patients with and without hyperlipidemia [1]. Xanthomatosis is a term used for multiple bone lesions and for xanthomas with accompanying soft tissue involvement. Xanthomas and Xanthomatosis have been classified as metabolic conditions of bone [2].
Increasingly, the central xanthoma of the jaw bones is being recognized as an entity with features unique enough to warrant separation from conditions such as the benign fibrous histiocytoma (BFH) and non-ossifying fibroma (NOF), with which it is often confused. In all 19 cases reported so far (Table 1) and in the 10 cases comprising this study, there was no association with any other bony or soft tissue lesions. Also, from the available data, none of the patients had hyperlipidemia. These features appear to distinguish the central xanthoma of the jaw bones from its extragnathic counterpart.
Table 1.
Demographic and clinical presentation of 19 previously reported cases of central xanthoma of jaw bones
| Authors | Year | Age | Sex | Site | Symptoms | Extraoral involvement | Hyperlipidemia |
|---|---|---|---|---|---|---|---|
| Rudy and Scheingold [3] | 1964 | 49 | F | Rt. mandible | Painless swelling | No | No |
| Mosby et al. [4, 5] | 1983 | 28 | M | L. mandible | None | No | Not available |
| Harsanyi and Larsson [6] | 1988 | 16 | F | Rt. mandible | Painless swelling | No | No |
| 23 | M | L. mandible | None | No | Not available | ||
| 27 | F | Rt. mandible | Painless swelling | No | No | ||
| 13 | F | Rt. mandible | Painless swelling | No | Not available | ||
| 12 | F | Anterior mandible | Painless swelling | No | No | ||
| 15 | F | L. mandible | None | No | No | ||
| 72 | F | L. mandible | Painless swelling | No | No | ||
| Slootweg et al. [7] | 1993 | 49 | M | L. mandible | Painless swelling | Not available | Not available |
| Mateo et al. [8] | 2004 | 11 | M | L. mandible | Painless swelling | No | No |
| Ramos-Perez et al. [9] | 2011 | 25 | M | L. mandible | None | No | No |
| Daley et al. [10] | 2015 | 56 | M | Anterior and left mandible | Swelling with numbness of lower left lip | No | No |
| 24 | M | L. mandible | None | No | No | ||
| 47 | M | L. mandible | None | No | No | ||
| 48 | M | Anterior maxilla | Painless swelling | No | No | ||
| 22 | M | Rt. Mandible | None | No | No | ||
| De Araujo et al. [11] | 2015 | 14 | F | L. mandible | None | No | No |
| Morel et al. [12] | 2016 | 40 | F | L. mandible | Swelling, pain | No | No |
Total number of cases: 19. Gender: Males: 10, Females: 9. Age range and mean age: 11-72 years, 41.5 years. Jaw involved: Maxilla 1, Mandible: 18. Swelling: Present in 11/19 cases (Information not available in 1 case). Symptoms: Asymptomatic in 17/19 cases. Pain in 1/19 cases. Numbness of lip in 1/19 cases. Extraoral xanthoma/xanthomatosis: Not present in 18/19 cases (Information not available in 1 case). Hyperlipidemia: Absent in 15/19 cases. (Information not available in 4 cases)
We present 10 additional cases of central xanthoma of the jaw bones. Salient clinical, radiographic and histopathological features are described and compared to the previously reported 19 cases. Emphasis is laid on differentiating the central xanthoma of the jaw from other histiocyte containing jaw conditions based on their clinical and histopathological features. A case is made to consider the central xanthoma of the jaw bones as a benign neoplasm.
Materials and Methods
This study is a case series and the sample was derived from the population of specimens acquired between the years 2000 and 2016 in the Oral and Maxillofacial Pathology service at the University of Washington School of Dentistry. One case was identified from the Oral Pathology biopsy service of Tufts University. To identify the cases, pathology records were searched for diagnosis including terminology such as non-Langerhans cell histiocytosis, benign histiocytic lesion, atypical histiocytic proliferation, histiocytic infiltrate consistent with xanthogranulomatosis, benign fibroosseous process with xanthomatous reaction, and xanthoma of bone. Slides were examined and the histopathological features were correlated with the available clinical and radiographic information. This information was used to exclude other potential lesions that may show the presence of xanthoma cells. Cases were excluded if the histopathologic examination showed fascicles of spindle cells or foamy histiocytes in focal clusters with predominance of fibrous tissue. As a result of this search, 10 cases were finally accepted. Information on the demographic and clinical presentation was tabulated while carefully observing patient privacy. The study variables were grouped into logical sets including age, gender, location of the lesion (maxilla, mandible, anterior, right side, left side), presence or absence of symptoms (including pain, swelling, loose teeth, any other), extraoral lesions and hyperlipidemia status. Available radiographic features and the histopathological findings of each lesion were recorded. The radiographic features were grouped into logical sets including location of the lesion, number of lesions, unilocular or multilocular, status of the periphery of the lesion(s) (circumscribed, sclerotic, punched out, diffuse), presence or absence of cortical perforation and effects on adjoining structures such as teeth, floor of the sinus, inferior dental canal. All slides were of formalin fixed tissue and stained with routine hematoxylin and eosin stains. All cases had either CD68 or CD163 to confirm the histiocytic/macrophage lineage of the cells. Some cases had additional immunohistochemical markers to exclude other potential histiocyte containing lesions. Descriptive findings were compared. Due to the retrospective nature of the study, clarification of some clinical and radiographic findings when not originally given was not possible.
Results
Of the 10 cases, (Table 2) six cases were seen in females and four were seen in males. The age range was from 12 to 63 years with a mean of 37.5 years. Eight cases were seen in the mandible and 2 in the maxilla, accounting for a ratio of 4:1. Nine lesions were seen in the posterior segment of the jaw bones while 1 presented in the anterior maxilla. All 8 mandibular lesions were discovered incidentally as a part of routine dental examination as patients were asymptomatic and did not exhibit any swelling. However, the 2 maxillary lesions were both painful and the anterior maxillary lesion was expansile. The teeth at that location were extracted 7 years prior to presentation of this lesion. The lesion of the left maxilla resorbed bone and was associated with mobility of the teeth. There was no information regarding pulp vitality testing. From the available clinical and radiographic findings, there was no history of loco-regional trauma, dental caries, endodontic treatment or tooth related pain. There was no extraoral involvement in 9 cases. Nine cases were also not associated with any other systemic conditions including hyperlipidemia or hypercholesteremia. This information was not available in one case.
Table 2.
Demographic and clinical presentation of 10 cases of central xanthoma of the jaws
| Case | Age | Gender | Site | Symptoms | Extraoral involvement | Hyperlipidemia |
|---|---|---|---|---|---|---|
| 1 | 22 | F | Rt. mandible | No | Not available | Not available |
| 2 | 25 | M | L. mandible | No | No | No |
| 3 | 15 | M | Rt. mandible | No | No | No |
| 4 | 12 | F | Rt. mandible | No | No | No |
| 5 | 58 | F | Anterior maxilla | Swelling, pain | No | No |
| 6 | 49 | F | L. mandible | No | No | No |
| 7 | 36 | M | Rt. mandible | No | No | No |
| 8 | 35 | M | L. mandible | No | No | No |
| 9 | 53 | F | L. maxilla | Loose teeth, mild pain | No | No |
| 10 | 63 | F | L. mandible | No | No | No |
Age range: 12–63 years, Mean age = 37.5 years, Male to female ratio = 1:1.5, Mandible to Maxilla ratio = 4:1
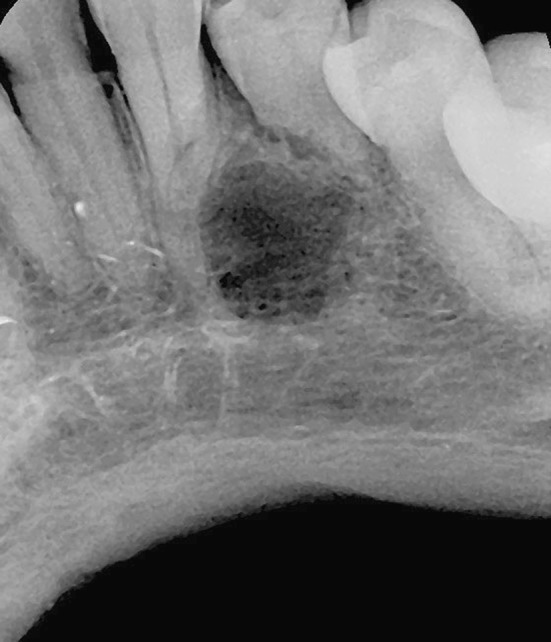
Radiographically, all cases (Table 3) presented as a solitary radiolucency with circumscribed peripheries. The smallest lesion measured approximately 1 cm in diameter (Fig. 1) while the largest lesion was of the left posterior maxilla and extended from the mesial aspect of the 1st premolar root to the left pterygomaxillary fissure anteroposteriorly and from the rim of the alveolar ridge to a point approximately half way into the lateral wall of the left maxillary antrum (Fig. 2). One mandibular lesion was described as multilocular while all other 9 cases were unilocular. The borders of both the maxillary lesions were non sclerotic. Of the 8 mandibular lesions, 5 showed distinct punched out borders (Figs. 1, 3a–d, 4) while 2 lesions showed a sclerotic border. Radiographs from one mandibular case were not available. One lesion in the mandible showed a significant punched out lingual cortical defect. The mandibular canal was displaced inferiorly and its roof was resorbed by the lesion (Fig. 3a–d). A communication with the buccal bifurcation of the molar root was noted on the CT image in this case (Fig. 3c). This was interpreted as being secondary to lesional expansion. As described by the clinician, the single multilocular mandibular lesion (case 2) showed scalloping between the roots of teeth 30 and 31. A copy of this X-ray was not available for confirmation. The lesion of the left maxilla caused splaying and some resorption of roots of the teeth. The floor of the maxillary sinus was also elevated (Fig. 2). Two cases of the mandible showed root resorption (Figs. 3a, 4) and 1 of these cases also showed divergence of the roots of the teeth (Fig. 4).
Table 3.
Radiographic features of 10 cases of central xanthoma of the jaws
| Case | Site | Unilocular or Multilocular | Periphery | Border | Perforation | Effect on teeth, adjacent structures |
|---|---|---|---|---|---|---|
| 1 | Rt. mandible | Unilocular | Circumscribed | Punched out | No | Scalloping between roots of teeth |
| 2 | L. mandible | Multilocular | Circumscribed | Sclerotic | No | No |
| 3 | Rt. mandible | Unilocular | Circumscribed | Not available | No | No |
| 4 | Rt. mandible | Unilocular | Circumscribed | Sclerotic | No | No |
| 5 | Anterior maxilla | Unilocular | Circumscribed | Non sclerotic | No | Teeth extracted 7 years ago |
| 6 | L. mandible | Unilocular | Circumscribed | Punched out | No | No |
| 7 | Rt. mandible | Unilocular | Circumscribed | Punched out | Yes, lingual and roof of inferior dental canal | Root resorption, Inferior dental canal displaced inferiorly |
| 8 | L. mandible | Unilocular | Circumscribed | Punched out | No | No |
| 9 | L. maxilla | Unilocular | Circumscribed | Non sclerotic | No | Roots splayed, resorption, sinus floor elevated |
| 10 | L. mandible | Unilocular | Circumscribed | Punched out | No | Roots splayed, resorption |
All cases presented as solitary radiolucencies
Fig. 1.

(Case 8) Panoramic radiograph showing a solitary, unilocular radiolucency at the apex of tooth #18/19. The lesion is well circumscribed and without marginal sclerosis. Clinically and radiographically, the teeth in the vicinity of the lesion were entirely normal. There was no history of trauma
Fig. 2.

(Case 9) Panoramic radiograph showing an extensive left posterior maxillary unilocular lesion. The lesion appears circumscribed but the anterior margin lacks sclerosis and is not sharply defined. Clinically, the teeth were mobile but showed no caries. There was no overt radiographic evidence of caries. Some subgingival calculus was present. However, the alveolar ridge was uninterrupted and the epicenter of the lesion was in the bone of the maxilla. There was no history of trauma
Fig. 3.
(Case 7) a Panoramic radiograph showing a circumscribed, unilocular radiolucency with punched-out margins lacking sclerosis. The lesion is associated with roots of tooth #31. Root resorption is seen. The inferior alveolar canal is relocated inferiorly and its roof is resorbed. b CT axial view showing a punched-out lingual perforation. c CT coronal view showing communication with buccal bifurcation of roots, inferior displacement of mandibular canal and lingual perforation. d CT 3-D reconstruction showing the lingual perforation and the mandibular canal contents open along the inferior border of the mandible. Tooth #31 was unaffected by dental caries or trauma
Fig. 4.
(Case 10) Radiograph showing a circumscribed, unilocular radiolucency lacking marginal sclerosis. Root resorption is seen. There was no history of trauma. Teeth in the vicinity of the lesion showed no evidence of dental caries
Being lesions of the alveolar bone with proximity to roots of teeth, a presumptive working diagnosis included cysts and benign tumors of odontogenic origin.
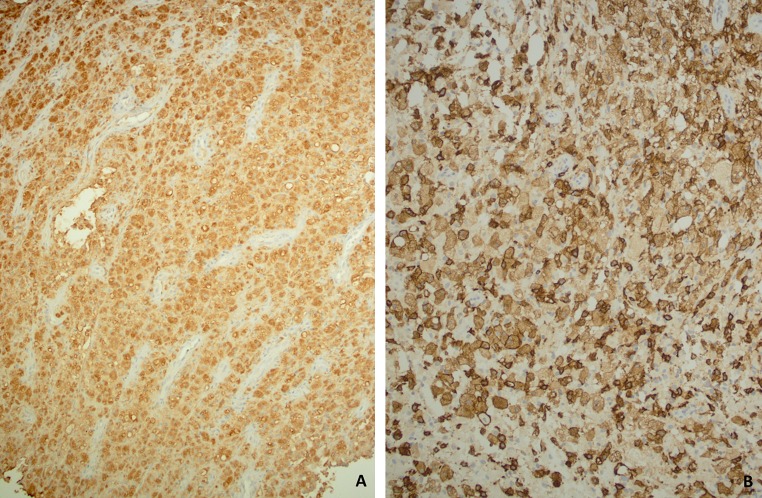
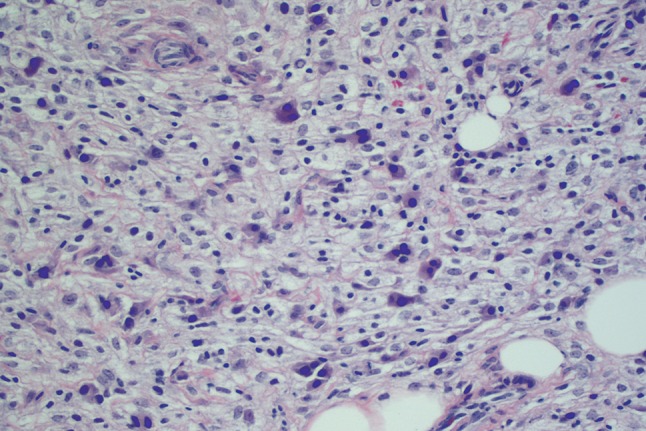
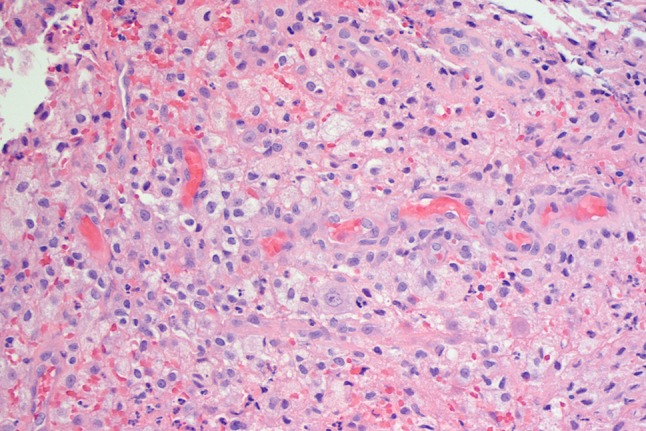
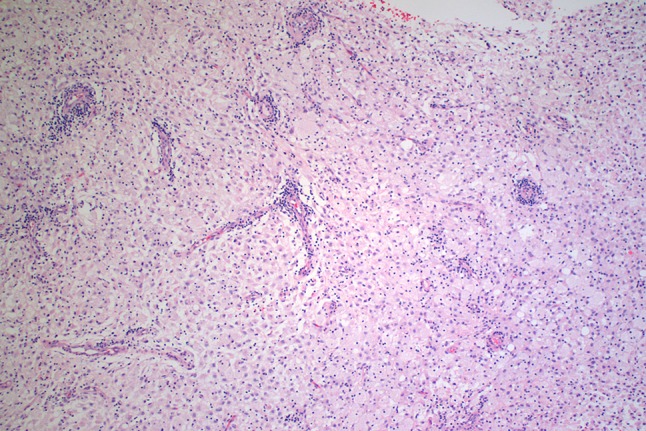
Histopathologically, the “Xanthoma” cells were arranged in loose (Fig. 5) or compact sheets (Fig. 6). One case showed a vague nodularity separated by fibrous septa (Fig. 7). None of the cases showed encapsulation and the xanthoma cells contacted the bone directly (Fig. 8). The xanthoma cells were large, round to oval with a fairly well-defined cytoplasmic membrane. The cytoplasm varied from foamy to granular (Fig. 9) to being more homogenous (Fig. 6). The cells with a granular or foamy cytoplasm tended to show cytoplasmic vacuolation (Figs. 5, 9). The nuclei of the cells with a foamy or granular cytoplasm were mostly small, intensely dark with condensed chromatin (Fig. 5). Cells with a more homogenous cytoplasm tended to look epithelioid with a larger vesiculated nucleus containing a prominent nucleolus (Fig. 6). One case showed a fairly uniform distribution of angulated cells with a dark amphophilic cytoplasm and containing from 1 to 3 dark blue condensed nuclei (Fig. 10). Inflammation, including the presence of scattered neutrophils was seen in the case with the buccal bifurcation communication (Figs. 3c, 11). A perivascular lymphocytic arrangement was noted in one case (Fig. 12). A single sinusoidal cavity surrounded by granulation type plump fibroblasts and 1 or 2 giant cells was seen in one case (Fig. 13). Entrapped pieces of host bone were seen in 2 cases (Fig. 14a, b). None of the cases displayed any pleomorphism or mitoses. The xanthoma cells, including the dark angulated cells seen in Fig. 10 were uniformly, strongly positive for either CD68 or CD163 thereby highlighting their macrophage/histiocytic lineage. CD68 being an anti-lysosomal antibody showed a coarse cytoplasmic reactivity (Fig. 15a), while CD163 being a cell surface glycoprotein marker offered a more intense cell membrane expression (Fig. 15b).
Fig. 5.

Loose sheets of foamy histiocytes with dark nuclei. Many cells show cytoplasmic vacuoles. H and E ×40
Fig. 6.

Cohesive sheets of epithelioid histiocytes with a more homogenous amphophilic cytoplasm. Nuclei are large and vesiculated with a prominent nucleolus. H and E ×40
Fig. 7.

One case showed a vague nodularity created by irregular bands of fibrous septa. H and E ×10
Fig. 8.

The xanthoma cells contact host bone directly. H and E ×10
Fig. 9.

The xanthoma cells show fairly well-defined cytoplasmic membranes. The cytoplasm is foamy or granular. The nuclei are prominent and dark. Inflammatory cellular infiltrate is mild. H and E ×20
Fig. 10.
(Case 10) One case showed scattered but prominent dark cells with 1–3 homogenously dark blue nuclei. H and E ×40
Fig. 11.
(Case 7) The case with communication with the buccal bifurcation of the roots of the molar tooth showed a mild neutrophilic infiltrate. H and E ×40
Fig. 12.
One case showed a distinct perivascular lymphocytic infiltrate. H and E ×10
Fig. 13.

A solitary sinusoid-like cavity surrounded by granulation-type tissue and occasional multinucleated cells. H and E ×20
Fig. 14.
Pieces of lamellated host bone lying within sheets of xanthoma cells (a, b). H and E ×20
Fig. 15.
Xanthoma cells are uniformly, densely CD68 (a) and CD163 (b) positive. Immunohistochemistry ×20
All 10 cases were treated with open aggressive curettage that extended to debulk the lesion in its entirety and involve adjacent marrow and normal host bone. Follow-up on cases ranged from 12 years to less than a year. Sixty percent of our cases (N = 6) had a follow-up of at least 5 years. There was no evidence of recurrence in these cases and 4 cases were treated within the past 2 years.
Discussion
A total of 19 cases of primary/central xanthoma of the jaw bones have been described in the English literature (Table 1). Here, we present 10 more cases of central xanthoma of the jaws. Gleaning through the combined available demographic and clinical presentation information, some definitive findings emerge.
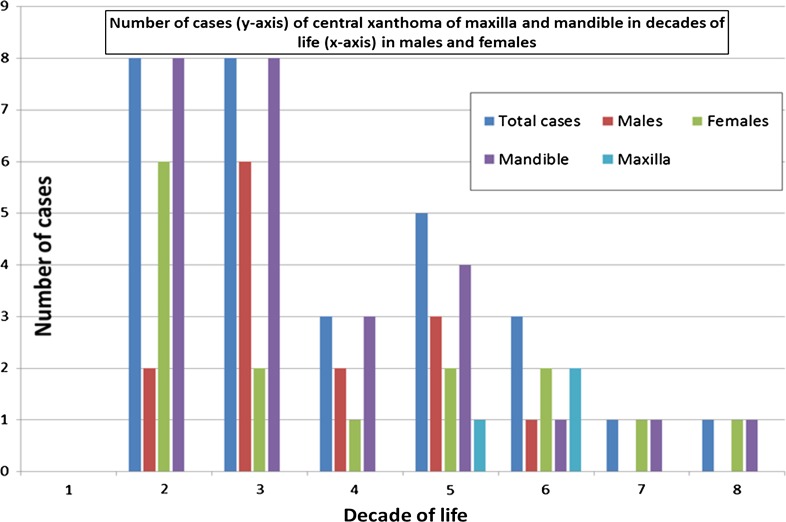
Jaw lesions were seen across a wide age range from 11 to 72 years with a mean of 33.95 years. However, 55 % of cases (16 out of 29) were seen in the 2nd and 3rd decades of life. All of the maxillary lesions presented in the 5th and 6th decade of life. Overall, there appears to be no gender predilection. However, the lesions in the 7th and 8th decade of life were all diagnosed in females (Fig. 16). The lesions have close to a 9:1 predilection for the mandible. Eighty-six percent of cases (25 out of 29) affected the posterior jaw. Of the 3 cases of the maxilla, 67 % (2 cases) were diagnosed in the anterior jaw. Jaw expansion was seen in 41 % of cases (12 out of 29 cases). This included both the anterior maxillary lesions. Eighty-six percent of cases (25 out of 29 cases) were asymptomatic. Both the lesions of the maxilla in the present series were associated with varying degrees of pain. Twenty-seven cases presented as solitary lesions with no other skeletal or soft tissue involvement. This information was not available in 2 cases. A normal lipid profile was recorded in 24 cases. This information was not available in 5 cases (Tables 1, 2).
Fig. 16.
Chart showing number of cases of central xanthoma of the maxilla and mandible in decades of life among males and females (N = 29)
The radiographic appearance described in the previously reported cases was highly variable. Descriptors used included terms such as unilocular, multilocular, radiolucency, honey comb mixed pattern, ground glass lesion, diffuse lesion, mixed density lesion, slightly sclerotic margins, corticated, no cortication, scalloped, poorly defined without sclerosis, irregular margins, ill-defined opacity, radiolucency with small opaque foci, etc. One case of the anterior maxilla showed labial plate perforation [10].
Histopathologically, at least partial encapsulation was noted in 4 cases reported by Daley et al. [10]. In the cases reported by other authors, information about a capsule was either not available or the lesion was found to not have a capsule. None of the cases in our series showed a capsule. The xanthoma cells were in direct contact with the host bone (Fig. 8). In all cases, the xanthoma cells were the dominant cell type and they were arranged in cohesive or loose sheets. Some cases showed sparse amount of fibroblastic connective tissue. One case in the present series showed a vague multinodularity with fibrous septa (Fig. 7). None of the cases showed a fascicular or storiform arrangement of the fibrous tissue. Majority of cases lacked any significant inflammation. Two of the previously reported cases showed cholesterol granulomas with giant cells. Only 1 case in the present series (case 7) showed some inflammation. The lesion in this case was continuous with the furcation of the tooth and had also perforated the lingual cortex (Fig. 11). One case in the present series showed a perivascular concentration of inflammatory cells (Fig. 12). Intralesional hemorrhage was reported in 7 cases from the previous studies and in 2 cases from our series. Hemorrhage was limited and not a defining feature of the histology in these cases. The xanthoma cells infiltrated the host bone trabeculae and in 5 cases from the previous studies, metaplastic ossification was seen surrounding tiny host bone pieces. Small pieces of host bone were seen in 9 out of 10 of our cases (Fig. 14a, b).
The central xanthoma of the jaws is characterized primarily by a proliferation of histiocytes that may be accompanied with a mild inflammatory cellular infiltrate. Based on the sampling of tissue, these findings are seen in a diverse list of conditions including periapical inflammatory lesions, benign fibrous histiocytoma, non-ossifying fibroma of bone, and fibrous dysplasia. Foamy histiocytes also populate intrabony lesions of lipid reticuloendotheliosis. Cases of Langerhans cell histiocytosis and Rosai-Dorfman disease also show a proliferation of histiocytic cells. Cases of a rare bone condition with histiocytes, Erdheim-Chester disease of the jaw bones have also been described. Therefore, a diagnosis of a central xanthoma of the jaw bones is challenging and requires elimination of the aforementioned conditions. This process of elimination requires careful assessment of the clinical, radiographic, and histopathological findings in each case individually.
Periapical inflammatory conditions such as granulomas and cysts may show a variable presence of foamy histiocytes. Periapical cysts show an epithelial lining and both cysts and granulomas may show the presence of a rich inflammatory cellular infiltrate that may also contain plasma cells, Russell bodies, pyronine bodies, neutrophils, eosinophils and mast cells. Cholesterol clefts and cholesterol granuloma formation with multinucleated foreign body giant cells may also be seen frequently as would pieces of root canal filling material. Also, these lesions are associated with non-vital teeth secondary to trauma or dental caries or with failing endodontically treated teeth [13].
CD68 positive histiocytes may be seen in both the benign fibrous histiocytoma (BFH) and the non-ossifying fibroma (NOF). The BFH is the intrabony counterpart of the more common soft tissue BFH. Most cases are diagnosed from the 4th to the 8th decade of life. The ilium and the ribs are the most frequently affected bones in the body. Pain is the most frequent presenting symptom at these locations [14]. Jaw lesions may or may not be painful but show progressive expansion of the posterior mandible including the angle and ramus area [15, 16]. Histopathologically, the foam cells are usually seen in small focal clusters and the dominant microscopic appearance is of a spindle cell proliferation arranged in whorls and storiform fascicles [14–16]. Thick collagen band entrapment and multinucleated giant cells are almost always seen [14–16]. Hemorrhage and hemosiderin pigment may also be found [14]. The NOF is seen in children and teens as a painless metaphyseal fibrous cortical defect of long tubular bones of the lower limbs with unfused growth plates. The majority of the appendicular lesions are discovered incidentally when X-rays are taken for other reasons such as sports injuries [14]. However, rare jaw lesions present as expansile, asymptomatic radiolucencies with a sclerotic border [17]. The histopathological appearance is identical to that of the BFH. The predominant cells are fibroblastic spindle cells arranged in a storiform pattern with interspersed giant cells. Foamy histiocytes are seen in small clusters [14, 17]. Hemorrhage and hemosiderin pigment with aneurysmal bone cyst-like areas may also be seen [14]. Absence of a whorling or a storiform fascicular spindle cell population, multinucleated giant cells and thick collagen band entrapment and presence of sheets of xanthoma cells rather than small focal clusters of foamy histiocytes distinguishes the central xanthoma of the jaw bones from the BFH and the NOF.
In fibrous dysplasia, depending on the biopsy sampling, a sheet-like infiltrate of foamy histiocytes may be seen. This is a secondary change that may be accompanied by giant cells, hemorrhage, and myxoid areas. These changes occur in association with an expansile lesion that in the craniofacial bones tends to be radiopaque with a ground glass appearance. A biopsy of the more opaque bone tends to show the characteristic woven bone within cellular fibrous connective tissue. The woven bone shows a haphazard pattern of mineralization under polarized light microscopy [14].
Sheets of lipid filled histiocytes are seen in the bone marrow of lipid reticuloendotheliosis such as Gaucher and Niemann-Pick disease. These rare inherited disorders are mostly encountered in the Ashkenazi Jewish population. In Gaucher disease, the histiocytes show abundant bluish cytoplasm whose texture resembles wrinkled silk. These cells replace the bone marrow resulting in anemia and thrombocytopenia. Patients show growth retardation, painful bone infarcts, hepatosplenomegaly, and bone deformities [2, 13, 14]. The “sea blue” histiocyte is the predominant cell type seen in Niemann-Pick disease. Patients present with hepatosplenomegaly and neurologic features. Life expectancy is limited to the first two decades, especially in the neuronopathic form of the disease [13]. Therefore, correlation of the histopathological findings with the clinical presentation easily distinguishes these conditions from the primary xanthoma of the jaw bones.
Posterior mandibular radiolucencies with a well-demarcated border are the presenting jaw lesions in Langerhans cell histiocytosis. The cell that defines this process is the Langerhans cell histiocyte with an abundant eosinophilic cytoplasm containing a kidney bean or coffee bean shaped indented nucleus. When seen ‘face on’, the nucleus shows a prominent linear groove across its length. Sheets of these cells are admixed with other macrophages, lymphocytes and a rich population of eosinophils. The eosinophils may be focally plentiful producing the so called eosinophilic abscesses. The Langerhans cell histiocyte demonstrates a highly specific reactivity to CD207 (langerin). Rarely, demonstration of the Birbeck-Broadbent granules by electron microscopy may be required to confirm the diagnosis [18].
In addition to macrophage markers CD68 and CD163, the large foamy histiocytes of Rosai-Dorfman disease are also reactive to S100 protein. Their cytoplasm shows vacuoles containing unaltered leukocytes (emperipolesis or lymphophagocytosis). Phagocytosed plasma cells, red blood cells and neutrophils may also be seen within such intracytoplasmic vacuoles [18, 19]. The phagocytosed cells are conspicuous because they are S100 negative [19].
Rare cases of Erdheim-Chester disease of the jaws have been described. Sheets of foamy histiocytes with a finely granular cytoplasm are associated with bone trabeculae in this disorder. Occasional multinucleated giant cells may be seen. The histiocytes express macrophage markers CD68 and CD163 and are negative to S100 protein and Langerhans cell markers. Rare cases may show admixed clusters of Langerhans cells. Erdheim-Chester disease is a multi-system condition affecting mostly adult males who present with bilateral lower appendicular long bone pain. Other common systemic findings include diabetes insipidus, neurologic symptoms, exophthalmos, and a retroperitoneal mass. Virtually any organ may be affected. 100 % of cases express a BRAF V600E mutation [14, 20].
While Daley et al. [10] concluded that the central xanthoma of the jaw bones is a unique entity; they were equivocal about it being a benign tumor. We agree that the central xanthoma of the jaw bones is a unique process and the following findings are characteristic of its uniqueness.
Over 50 % of the central xanthomas of the jaw bones occur in the 2nd and 3rd decades of life while the highest relative incidence of extragnathic xanthomas and xanthomatosis is in the 4th to 6th decades of life [2].
Central xanthomas of the jaw bones have a 9:1 predilection for the mandible over the maxilla.
Lesions affect males and females equally while the extragnathic xanthomas and xanthomatosis are predominantly a male disorder with a male to female ratio of 2:1 [2].
Xanthomas of both primary and secondary hyperlipidemia, hypercholesterolemia and systemic lipid diseases have distinct reported mechanism and etiology. The intrabony xanthomas reported with hyperlipidosis also have a genetic mutation of the Low Density Lipoprotein Receptor [21]. The central xanthoma of the jaw bones is not associated with a systemic lipid disorder and the hypothetical lipid leakage from the vascularity into the surrounding tissue is therefore not expected in these individuals.
Lesions contain sheets of xanthoma cells with little fibrous tissue.
-
There is no history of trauma, infection or other preexisting intrabony pathology.
In addition, the following findings might suggest that the central xanthoma of the jaw bones is an aggressive or neoplastic process that is distinct from the extragnathic lesions including those associated with xanthomatosis.
The growth is progressive and when large enough to be associated with teeth, causes splaying and resorption of roots. The inferior dental canal is also displaced (case 7).
It causes significant bone destruction, cortical perforation (case 7) and extension into surrounding structures (case 9).
Daley et al. [10] cite findings from their cases such as presence of inflammatory cells, hemorrhage or hemosiderin pigment formation, metaplastic ossification and “occasional cholesterol granulomas” to favor a reactive process. In the results of histopathological evaluation of their cases, they say that the hemorrhage is “recent and possibly surgical”. Also in the legend to Fig. 5 (their case 5), they explain that focal hemosiderin deposits were never a prominent feature. While their Figs. 2, 3, 4 and 5 of their cases 2–5 are characteristic for a central xanthoma of the jaws, in their Fig. 1c where they encountered cholesterol granulomas also shows a very prominent densely collagenous wall. The microscopic appearance of a paucicellular, dense collagenous wall in combination with the luminal cholesterol clefts and foamy histiocytes is what one encounters with inflammatory lesions of dental origin.
Conclusions
The central xanthoma of the jaws presents more frequently in the 2nd and 3rd decades of life with a distinct predilection for the posterior mandible. It affects males and females equally. It has a distinct predilection for the bone of the posterior mandible. Jaw expansion is seen in less than half the number of cases and pain is infrequent. Maxillary lesions show a tendency towards a painful expansion of the anterior jaw. In our series, majority of the mandibular lesions presented as unilocular radiolucencies without cortication thereby giving a punched out appearance. The central xanthoma of the jaw bones is not associated with a systemic lipid disorder. Histopathologically, the central xanthoma of the jaws shows sheets of CD68 and CD163 positive and S100, CD1a and CD207 negative histiocytes with little inflammation. Fibrous tissue is minimal and there is no whorling or fascicular fibroblastic cellularity. Giant cells, cholesterol granulomas, hemorrhage and hemosiderin pigment formation are all infrequent findings. Intralesional bone trabeculae and metaplastic ossification around tiny spicules of host bone may be seen. Bizarre cells and mitosis are not seen. In the jaw bones, the diagnosis requires exclusion of several other histiocyte containing lesions.
Once the biopsy has confirmed an intraosseous xanthoma, curettage and complete excision can be performed. In large lesions, due to the potential for fractures, intermaxillary fixation or weight sharing plates can be applied. Immediate bone grafting can be undertaken with a complete surgical excision. Although recurrences have not been reported, due to the complex anatomy of the upper jaw and its surrounding structures, it would be prudent to follow-up on treated cases of the maxilla.
Acknowledgments
Dr. Thomas B. Dodson for his editorial support of the manuscript.
Funding
This study was supported in part by the Research and Education Fund of the Department of Oral and Maxillofacial Surgery, University of Washington School of Dentistry.
Compliance with Ethical Standards
Conflict of interest
No conflict of interest to disclose.
Contributor Information
Yeshwant B. Rawal, Phone: 1 206 221 3960, Email: ybrawal@uw.edu
Srinivasa R. Chandra, Email: chandra4@uw.edu
James M. Hall, Email: jmhall11@aol.com
References
- 1.Alden KJ, McCarthy EF, Weber KL. Xanthoma of bone: a report of three cases and review of the literature. Iowa Orthop J. 2008;28:58–64. [PMC free article] [PubMed] [Google Scholar]
- 2.Wold LE, Unni KK, Sim FH, Sundaram M, Adler C, editors. Atlas of Orthopedic Pathology. 2. Philadelphia: Saunders; 2008. pp. 3–191. [Google Scholar]
- 3.Rudy HN, Scheingold SS. Solitary xanthogranuloma of the mandible; report of a case. Oral Surg Oral Med Oral Pathol. 1964;18:262–271. doi: 10.1016/0030-4220(64)90436-0. [DOI] [PubMed] [Google Scholar]
- 4.Mosby EL, Albright JE, Messer EJ, Nealis MF, Werning JT. Clincopathologic conferences. Case 44, part I. J Oral Maxillofac Surg. 1983;41(3):180–181. doi: 10.1016/0278-2391(83)90077-0. [DOI] [PubMed] [Google Scholar]
- 5.Mosby EL, Albright JE, Messer EJ, Nealis MF, Werning JT. Case 44, part II: xanthoma of the mandible. J Oral Maxillofac Surg. 1983;41(4):268–270. doi: 10.1016/0278-2391(83)90274-4. [DOI] [PubMed] [Google Scholar]
- 6.Harsanyi BB, Larsson A. Xanthomatous lesions of the mandible: osseous expression of non-X histiocytosis and benign fibrous histiocytoma. Oral Surg Oral Med Oral Pathol. 1988;65(5):551–566. doi: 10.1016/0030-4220(88)90138-7. [DOI] [PubMed] [Google Scholar]
- 7.Slootweg PJ, Swart JG, van Kaam N. Xanthomatous lesion of the mandible. Report of a case. Int J Oral Maxillofac Surg. 1993;22(4):236–237. doi: 10.1016/S0901-5027(05)80644-7. [DOI] [PubMed] [Google Scholar]
- 8.Marqués Mateo M, Puche Torres M, Miragall Alba L, Iglesias Gimilio ME, Pascual Gil JV. Primary mandibular bone xanthoma. A case report. Int J Oral Maxillofac Surg. 2004;33(8):806–807. doi: 10.1016/j.ijom.2003.12.006. [DOI] [PubMed] [Google Scholar]
- 9.de Moraes Ramos-Perez FM, de Pádua JM, Silva-Sousa YT, de Almeida OP, da Cruz Perez DE. Primary xanthoma of the mandible. Dentomaxillofac Radiol. 2011;40(6):393–396. doi: 10.1259/dmfr/51850495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Daley T, Dunn G, Darling MR. Central xanthoma of the jaws: a clinicopathologic entity? Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;119(1):92–100. doi: 10.1016/j.oooo.2014.09.018. [DOI] [PubMed] [Google Scholar]
- 11.de Araujo MR, Scariot R, Uetanabaro L, Luvison Gomes da Silva L, Giovanini AF. Primary mandibular xanthoma: case report. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120(4):e177–e182. doi: 10.1016/j.oooo.2015.01.015. [DOI] [PubMed] [Google Scholar]
- 12.Morel D, Kelsch RD, Nolan PJ. Primary xanthoma of the mandible: report of a rare case. Head Neck Pathol. 2016;10(2):245–251. doi: 10.1007/s12105-015-0643-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and maxillofacial pathology. 3. St. Louis: Saunders; 2009. [Google Scholar]
- 14.Czerniak B. Bone tumors. 2. Philadelphia: Elsevier; 2016. [Google Scholar]
- 15.Heo MS, Cho HJ, Kwon KJ, Lee SS, Choi SC. Benign fibrous histiocytoma in the mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97(2):276–280. doi: 10.1016/j.tripleo.2003.07.002. [DOI] [PubMed] [Google Scholar]
- 16.Shoor H, Pai KM, Shergill AK, Kamath AT. Benign fibrous histiocytoma: a rare case involving jaw bone. Contemp Clin Dent. 2015;6(Suppl 1):S266–S268. doi: 10.4103/0976-237X.166828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bowers LM, Cohen DM, Bhattacharyya I, Pettigrew JC, Jr, Stavropoulos MF. The non-ossifying fibroma: a case report and review of the literature. Head Neck Pathol. 2013;7(2):203–210. doi: 10.1007/s12105-012-0399-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hicks J, Flaitz CM. Langerhans cell histiocytosis: current insights in a molecular age with emphasis on clinical oral and maxillofacial pathology practice. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100(2 Suppl):S42–S66. doi: 10.1016/j.tripleo.2005.06.016. [DOI] [PubMed] [Google Scholar]
- 19.Kademani D, Patel SG, Prasad ML, Huvos AG, Shah JP. Intraoral presentation of Rosai-Dorfman disease: a case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93(6):699–704. doi: 10.1067/moe.2002.123495. [DOI] [PubMed] [Google Scholar]
- 20.Petrikowski CG, McGaw WT. Erdheim-Chester disease of the jaws: literature review and case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90(3):389–398. doi: 10.1067/moe.2000.107537. [DOI] [PubMed] [Google Scholar]
- 21.Han Y, Gao W, Liang P, Wang S, Chen Y, Qiu J. Clinical features of bilateral temporal bone xanthoma with LDLR gene mutation. Int J Pediatr Otorhinolaryngol. 2015;79(7):1148–1151. doi: 10.1016/j.ijporl.2015.04.020. [DOI] [PubMed] [Google Scholar]