Abstract
Inosine monophosphate dehydrogenase type II (IMPDH2) has been shown to play critical roles in the development and progression of several human cancers. However, little is known about IMPDH2 expression and its clinical significance in nasopharyngeal carcinoma (NPC). Western blotting, qRT-PCR and immunohistochemistry were employed to evaluate IMPDH2 expression in NPC cell lines and tissues. In our study, elevated expression of IMPDH2 was observed at both the protein and mRNA levels in NPC cell lines than in NPEC2 Bmi-1. IMPDH2 protein expression was markedly higher in NPC tissues than in adjacent non-tumorous tissues. Moreover, IMPDH2 expression in NPC correlated with several clinicopathological parameters, including T classification (P = 0.023), TNM stage (P = 0.020), distant metastasis (P = 0.001) and death (P = 0.002). Further Cox regression analysis suggested that IMPDH2 expression was an independent prognostic factor for overall survival (P = 0.001) and disease-free survival (P < 0.001). In addition, stratified survival analysis showed that high expression of IMPDH2 could be a prognostic factor for NPC patients with TNM stage I/II (OS: P = 0.012; DMFS: P = 0.007), TNM stage III/IV (OS: P = 0.028; DMFS: P = 0.020). Our study demonstrates IMPDH2 may be served as an independent prognostic biomarker for NPC patients, in which high IMPDH expression suggests poor prognosis of NPC patients.
Introduction
Nasopharyngeal carcinoma (NPC) is one of the most prevalent human head and neck malignancies in Southern China, Southeast Asia and North Africa1–3. Due to its nonspecific symptoms in the early stage, the majority of NPC patients are present with advanced stage disease when first diagnosed. To date, the clinical TNM staging system for NPC is most commonly used to evaluate prognosis. Intriguingly, the prognosis of NPC patients with the same stage of disease often varies4, 5. Therefore, a large number of investigations on NPCs have focused on the discovery of specific biomarkers which could be utilized as more effective prognostic predictors. To date, however, highly sensitive and specific prognostic biomarkers remain unavailable for early diagnosis and individualized treatment of patients with NPC.
Inosine monophosphate dehydrogenase (IMPDH) is a rate-limiting enzyme which catalyzes a crucial step in the de novo biosynthesis of purine nucleotides6, indicating that it is essential for DNA synthesis7. Previous studies have demonstrated that IMPDH was associated with cell growth, malignant transformation and differentiation8–10. In mammalian species, it has two ubiquitously expressed isoforms, IMPDH1 and IMPDH2, which are encoded by distinct genes with 85% of their amino acid sequence conserved11. IMPDH1 is constitutively expressed in normal cells, whereas expression of IMPDH2 is frequently elevated in malignant cells12, 13. Therefore, we focus our study on IMPDH2 as malfunction of IMPDH are primarily due to the up-regulation of this isoform in malignant cells.
Accumulating evidence had demonstrated the involvement of IMPDH2 in different types of malignancies. For instance, enhanced IMPDH2 expression was observed in methotrexate (MTX)-resistant erythroleukemia K562 cells and colorectal cancer cells14, 15. The study by Fellenberg et al. suggested that IMPDH2 could be used as a promising candidate for the stratification of osteosarcoma patients into low- and high-risk groups16. Recently, the protein expression level of IMPDH2 was found to be significantly upregulated in prostate, kidney and bladder cancers and could be a potential biomarker for these diseases2, 17. However, to the best of our knowledge, the expression status of IMPDH2 and its clinical significance in NPC remain unknown.
In the current study, immunohistochemistry (IHC) was utilized to examine the expression level of IMPDH2 in NPC tissues and adjacent normal nasopharyngeal tissues. Receiver operating characteristic (ROC) curve analysis was performed to define the cut-off value for separating IMPDH2 expression into increased- and decreased-expression groups. In addition, the relationship between IMPDH2 expression and various clinicopathologic parameters was evaluated to investigate the prognostic impacts of IMPDH2 in NPC patients.
Results
IMPDH1 and IMPDH2 expression in NPC cell lines
Western blotting and qRT-PCR was employed to evaluate the expression levels of IMPDH1 and IMPDH2 protein and mRNA in NPC cell lines including CNE1, CNE2, C666, HONE1, and SUNE1, and an immortalized primary nasopharyngeal epithelial cell line (NPEC2 Bmi-1). As described in Fig. 1A,B, the expression levels of IMPDH1 protein and mRNA in CNE1, CNE2, HONE1, and SUNE1 were lower than that in the NPEC2 Bmi-1. Interestingly, the protein and mRNA levels of IMPDH1 in C666 were higher than that in NPEC2 Bmi-1. However, to our knowledge, the C666 cell line was the only native EBV-infected NPC cell line among these NPC cell lines. These results suggest that high expression of IMPDH1 in C666 may be associated with EBV-infected NPC cell line. By contrast, we performed western blotting and qRT-PCR to assess the protein and mRNA levels of IMPDH2 in NPC cell lines and NPEC2 Bmi-1. As shown in Fig. 1C,D, the expression levels of IMPDH2 protein and mRNA in NPC cell lines were highly expressed, compared to NPEC2 Bmi-1.
Figure 1.
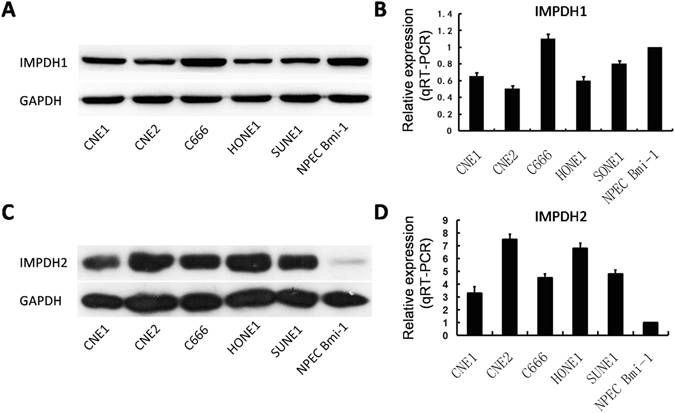
Expression of IMPDH1 and IMPDH2 in NPC cell lines. (A) The expression level of IMPDH1 protein in CNE1, CNE2, C666, HONE1, SUNE1 and NPEC2 Bmi-1 was detected by western blotting. (B) The expression level of IMPDH1 mRNA in CNE1, CNE2, C666, HONE1, SUNE1 and NPEC2 Bmi-1 was evaluated by quantitative RT-PCR. (C) The expression level of IMPDH2 protein in CNE1, CNE2, C666, HONE1, SUNE1 and NPEC2 Bmi-1 was detected by western blotting. (D) The expression level of IMPDH2 mRNA in CNE1, CNE2, C666, HONE1, SUNE1 and NPEC2 Bmi-1 was evaluated by quantitative RT-PCR.
IMPDH2 expression in NPC tissues
The expression of IMPDH2 protein was detected by IHC in NPC tissues and adjacent normal nasopharyngeal tissues. Compared with adjacent non-tumorous nasopharyngeal tissues, NPC tissues exhibited higher expression levels of IMPDH2 protein (Fig. 2A,B). The four categories of the intensity of IMPDH2 immunostaining were described in Fig. 3a–d.
Figure 2.
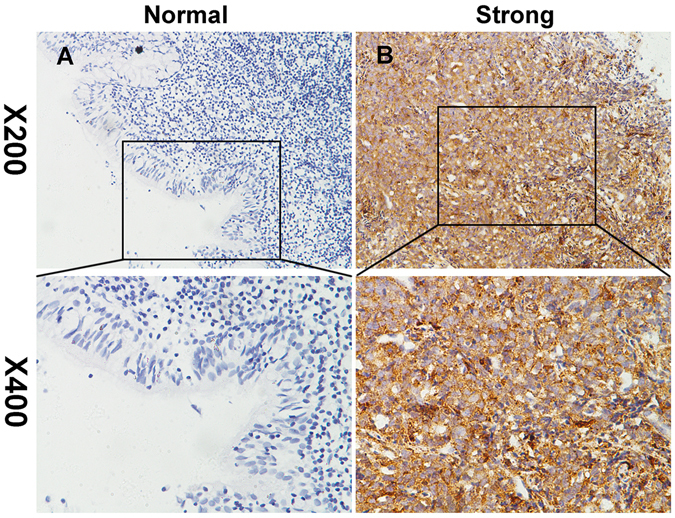
Representative images of IMPDH2 expression in NPC tissues via immunohistochemistry. IMPDH2 was absent or only weakly detected in adjacent normal nasopharyngeal tissues (A), whereas its upregulation was mainly detected in NPC tissues (B) (original magnification, x200 and x400).
Figure 3.
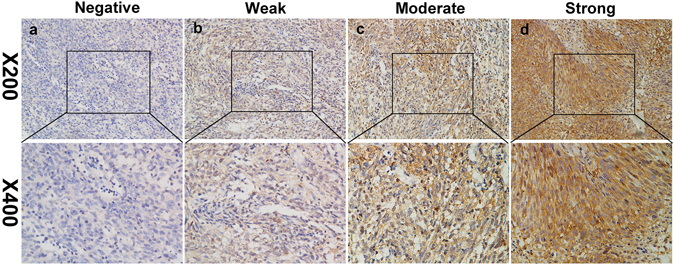
Expression of IMPDH2 in NPC tissues by IHC. The representative images show different staining intensities of IMPDH2: (a) negative staining, (b) weak staining, (c) moderate staining, and (d) strong staining (original magnification, x200 and x400).
Definition of cutoff score for high IMPDH2 expression in NPC
To better estimate the expression of IMPDH2 in NPC tissues, ROC curve analysis for the clinical features was employed to determine an optimal cutoff value for high IMPDH2 expression. As shown in Fig. 4A–G, ROC curve analysis for survival status had the closest distance from the curve to the point (0.0, 1.0). Therefore, the optimized cut-off value for high IMPDH2 expression was 145. Tumors with scores above this cutoff value were considered to have high IMPDH2 expression, leading to the greatest number of tumors correctly classified, based on the presence or absence of a positive clinical outcome. According to the definition of cutoff score, increased expression of IMPDH2 was observed in 123/226 (54.4%) of NPC tissues.
Figure 4.
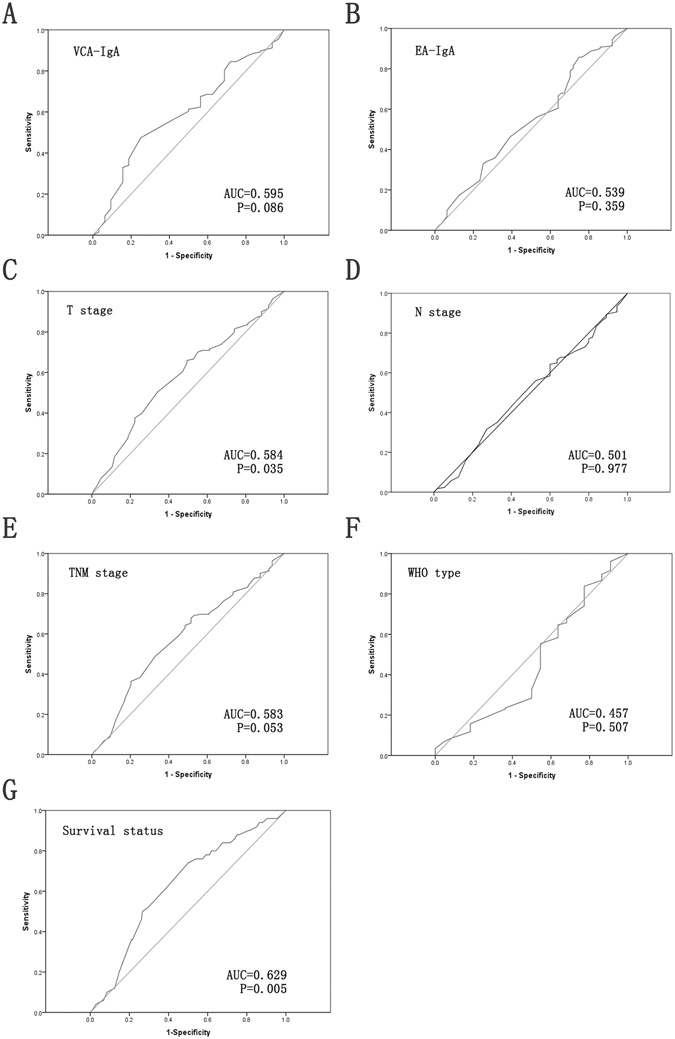
ROC curve analysis was performed to determine the cutoff score for increased IMPDH2 expression. The sensitivity and specificity for each outcome were plotted: VCA-IgA (A), EA-IgA (B), T classification (C), N classification (D), TNM stage (E), WHO type (F) and survival status (G).
The association between IMPDH2 expression and clinicopathological parameters of NPC patients
The chi-square test/Fisher’s exact test was performed to investigate the relationship between IMPDH2 expression and clinicopathological characteristics in 226 cases with NPC (Table 1). Our results suggested significant correlations between IMPDH2 expression and four clinical characteristics including T classification (P = 0.023), TNM stage (P = 0.020), distant metastasis (P = 0.001) and death (P = 0.002). However, we found no statistically significant correlations between IMPDH2 expression and the rest of clinicopathological features, such as age, gender, VCA-IgA, EA-IgA, and WHO type.
Table 1.
Correlation between IMPDH2 expression and clinical and pathological characters in NPC patients.
| Variable | All cases N = 226 (%) | IMPDH2 protein | P value | ||
|---|---|---|---|---|---|
| Low expression N = 103 (%) | High expression N = 123 (%) | χ2 | |||
| Age(years) | 0.054 | 0.817 | |||
| ≤44 | 116 (51.3) | 52 (44.8) | 64 (55.2) | ||
| >44 | 110 (48.7) | 51 (46.4) | 59 (53.6) | ||
| Mean ± SD(44.4 ± 11.4) | |||||
| Gender | 1.097 | 0.295 | |||
| Female | 52 (23.0) | 27 (51.9) | 25 (48.1) | ||
| Male | 174 (77.0) | 76 (43.7) | 98 (56.3) | ||
| VCA-IgA | 1.713 | 0.191 | |||
| <1:80 | 32 (14.2) | 18 (56.3) | 14 (43.7) | ||
| ≥1:80 | 194 (85.8) | 85 (43.8) | 109 (56.2) | ||
| EA-IgA | 0.705 | 0.401 | |||
| <1:10 | 64 (28.3) | 32 (50.0) | 32 (50.0) | ||
| ≥1:10 | 162 (71.7) | 71 (43.8) | 91 (56.2) | ||
| T classification | 5.188 | 0.023* | |||
| T1-2 | 85 (37.6) | 47 (55.3) | 38 (44.7) | ||
| T3-4 | 141 (62.4) | 56 (39.7) | 85 (60.3) | ||
| N classification | 0.362 | 0.547 | |||
| N0 | 55 (24.3) | 27 (49.1) | 28 (50.9) | ||
| N1-3 | 171 (75.7) | 76 (44.4) | 95 (55.6) | ||
| TNM stage | 5.390 | 0.020* | |||
| I-II | 64 (28.3) | 37 (57.8) | 27 (42.2) | ||
| III-IV | 162 (71.7) | 66 (40.7) | 96 (59.3) | ||
| WHO type | <0.001 | 0.990 | |||
| I + II | 22 (9.7) | 10 (45.5) | 12 (54.5) | ||
| III | 204 (90.3) | 93 (45.6) | 111 (54.4) | ||
| Distant metastasis | 10.561 | 0.001* | |||
| Yes | 61 (27.0) | 17 (27.9) | 44 (72.1) | ||
| No | 165 (73.0) | 86 (52.1) | 79 (47.9) | ||
| Death | 9.919 | 0.002* | |||
| Yes | 50 (22.1) | 13 (26.0) | 37 (74.0) | ||
| No | 176 (77.9) | 90 (51.1) | 86 (48.9) | ||
VCA-IgA: viral capsid antigen immunoglobulin A; EA-IgA: early antigen immunoglobulin A; WHO: World Health Organization; P-values*were calculated using the chi-square test or Fisher’s exact test.
The relationship of high IMPDH2 expression with poor survival in NPC patients
The relationship between IMPDH2 expression in NPC patients and the survival time of these patients was analyzed by Kaplan-Meier analysis and the log-rank test (Fig. 5A–F). The log-rank test showed that the survival time was different between high and low IMPDH2 expression groups. The median overall survival (OS) time was 52.2 months for the patients with high IMPDH2 expression, significantly shorter than that for the patients exhibiting low IMPDH2 expression (64.4 months) (log-rank test, P = 0.001, Fig. 5A). Furthermore, high IMPDH2 expression group had poorer distant metastasis-free survival (DMFS) time than low IMPDH2 expression group (log-rank test, P < 0.001, Fig. 5B). Moreover, we deployed survival analysis towards the level of IMPDH2 expression in subgroups of NPC patients against TNM stages. Our results revealed that high expression of IMPDH2 could be a prognostic factor for NPC patients with TNM stage I/II (OS: P = 0.012, Fig. 5C; DMFS: P = 0.007, Fig. 5D), TNM stage III/IV (OS: P = 0.028, Fig. 5E; DMFS: P = 0.020, Fig. 5F).
Figure 5.
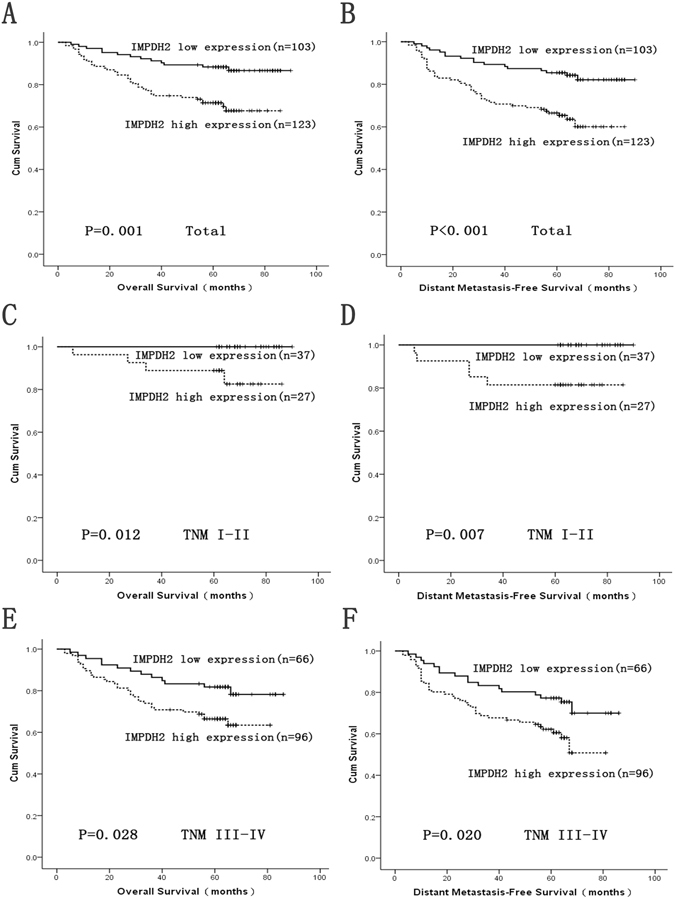
Survival analysis of IMPDH2 expression by Kaplan-Meier method (log rank test). Overall survival (OS) rate and distant metastasis-free survival (DMFS) rate in total (A,B) NPC patients with low/high IMPDH2 expression. OS rate and DMFS rate in TNM stage I-II (C,D), TNM stage III-IV (E,F) NPC patients with low/high IMPDH2 expression.
In addition, the prognostic value of IMPDH2 expression was analyzed using univariate analysis model and multivariate Cox regression against OS and DMFS (Table 2). The univariate analysis results confirmed the impact of IMPDH2 expression and TMN stages on survival. The Cox regression further suggested IMPDH2 expression and TMN stages as independent prognostic factors for OS and DMFS in NPC patients. Therefore, the results demonstrated that the IMPDH2 expression level was closely associated with the prognosis of NPC.
Table 2.
Univariate and multivariate Cox regression analysis of prognostic factors in 226 NPC patients.
| Variable | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P-value | HR | 95% CI | P-value | |
| Overall survival | ||||||
| Age (>44 years vs. ≤44 years) | 1.246 | 0.714–2.173 | 0.438 | |||
| Sex (male vs. female) | 0.868 | 0.462–1.634 | 0.662 | |||
| VCA-IgA (≥1:80 vs. <1:80) | 1.043 | 0.469–2.318 | 0.918 | |||
| EA-IgA (≥1:10 vs. <1:10) | 1.083 | 0.584–2.009 | 0.799 | |||
| WHO type (III vs. I-II) | 0.558 | 0.262–1.189 | 0.131 | |||
| TNM stage (III-IV vs. I-II) | 5.415 | 1.945–15.075 | 0.001* | 4.761 | 1.704–13.304 | 0.003* |
| IMPDH2 expression (High vs. Low) | 2.794 | 1.481–5.269 | 0.002* | 2.428 | 1.284–4.590 | 0.006* |
| Distant metastasis-free survival | ||||||
| Age (>44 years vs. ≤44 years) | 1.003 | 0.607–1.657 | 0.990 | |||
| Sex (male vs. female) | 1.035 | 0.570–1.880 | 0.911 | |||
| VCA-IgA (≥1:80 vs. <1:80) | 1.366 | 0.622–3.003 | 0.437 | |||
| EA-IgA (≥1:10 vs. <1:10) | 1.214 | 0.686–2.149 | 0.505 | |||
| WHO type (III vs. I-II) | 0.615 | 0.303–1.249 | 0.179 | |||
| TNM stage (III-IV vs. I-II) | 5.507 | 2.196–13.811 | <0.001* | 4.881 | 1.938–12.295 | 0.001* |
| IMPDH2 expression (High vs. Low) | 2.654 | 1.511–4.663 | 0.001* | 2.300 | 1.306–4.051 | 0.004* |
VCA-IgA: viral capsid antigen immunoglobulin A; EA-IgA: early antigen immunoglobulin A; WHO: World Health Organization; *P-values were calculated using univariate and multivariate cox regression analyses.
Discussion
Currently, tumor TNM stage is the most commonly and widely used predictive factor for the prognosis of NPC patients. However, the TNM staging alone is inadequate to accurately predict the clinical outcomes of the patients with NPC. Furthermore, the existing molecular markers for NPC have not fully satisfied the clinical prognostic needs. Therefore, it is of great significance to search for novel diagnostic and prognostic markers to refine the individualized treatment of NPC patients.
Accumulating evidence has shown that expression of IMPDH2 was significantly increased in various types of malignancies12, 13, 18–20. These findings reveal a potential carcinogenic role of IMPDH2 in multiple human malignancies. To date, however, the expression status of IMPDH2 in NPC and its relationship with the clinicopathological parameters have not been elucidated. In the current study, we first performed immunohistochemistry to evaluate the expression status of IMPDH2 in a cohort of 226 NPC patients. IMPDH2 was significantly up-regulated in NPC paraffin-embedded tissues compared with that in adjacent normal tissues. In particular, overexpression of IMPDH2 protein was detected in 54.4% (123/226) of NPC tissues. By contrast, the expression level of IMPDH2 in the adjacent nasopharyngeal tissues was low or absent. We also observed that IMPDH2 was highly expressed at both the protein and mRNA levels in NPC cell lines compared with NPEC2 Bmi-1. These findings suggest that high expression of IMPDH2 may provide a selective advantage in the NPC tumorigenic processes.
In previous studies, the expression of IMPDH2 was found to be markedly elevated and closely associated with tumor progression and unfavorable prognosis in various different types of malignancies2, 14, 16, 17. IMPDH2 was reported to be overexpressed in the subgroup of patients with poor response to chemotherapy, rendering it an independent prognostic factor for chemotherapy response and event-free survival16. He et al. demonstrated that high IMPDH2 expression was frequently observed in colorectal cancer tissues and might play a crucial role in colorectal carcinogenesis14. High IMPDH2 expression might be involved in tumor metastasis and progression in patients with prostate, bladder and kidney cancer2, 17. In the present study, we observed that increased expression of IMPDH2 was significantly associated with T classification, TNM stage, distant metastasis and patient death, which suggested that overexpression of IMPDH2 might be involved in the progression of NPC. Additionally, the Kaplan-Meier analysis and log rank test demonstrated that enhanced expression of IMPDH2 significantly correlated with shorter OS and poorer DMFS in patients with NPC. Further stratified analysis revealed that elevated expression of IMPDH2 could predict the unfavorable outcome in NPC patients with TNM stage I/II and III/IV. More importantly, multivariate Cox regression analysis showed that high IMPDH2 expression was identified as an independent prognostic factor for OS and DMFS in NPC. Hence, our study suggested the potential use of IMPDH2 expression in addition to existing classifications to predict OS and DMFS in patients with NPC.
With respect to the function of the IMPDH gene, as a rate-limiting enzyme in the de novo guanine nucleotide biosynthesis, IMPDH has been implicated in cell proliferation, differentiation and the development of chemoresistance. Inhibition of IMPDH contributed to depletion of guanine nucleotide pools, followed by decreased synthesis of DNA and RNA21. A study by Takebe N et al. demonstrated that inhibition of IMPDH had been able to induce caspase-dependent apoptosis and cell-cycle arrest in multiple myeloma cells22. Furthermore, IMPDH inhibitors, such as tiazofurin and benzamide riboside, has been found to induce terminal differentiation in several types of human cancer cells23, 24 and has been successfully applied in clinical trials25, 26. On the other hand, overexpression of IMPDH2 induced a strong chemoresistance in osteosarcoma cells which was mediated partly by upregulation of anti-apoptotic proteins, leading to inhibition of the mitochondrial apoptotic signaling pathway27. In addition, researchers found the sensitivity of HT29 human colon cancer cells were significantly increased towards chemotherapy by down-regulating the IMPDH2 gene expression in the resistant cells28. As a consequence, IMPDH2 gene expression by more effective inhibitors in combination with chemotherapy may have the potential to provide an effective treatment to overcome chemoresistance.
In summary, we revealed for the first time that IMPDH2 protein was markedly expressed in NPC, and elevated expression of IMPDH2 was closely associated with unfavorable prognosis in NPC. These data suggested that the expression levels of IMPDH2 protein, as detected by IHC, could be identified as a prognostic biomarker for the clinical outcome of NPC patients and a potential therapeutic target in NPC. However, further investigation is needed to elucidate the molecular mechanisms on the oncogenic function of IMPDH2 for NPC.
Materials and Methods
Patients and tissue specimens
Paraffin-embedded specimens from 226 patients with primary NPC were obtained from Sun Yat-Sen University Cancer Center between 2001 and 2004. These patients’ clinical and pathological data, such as age, gender, VCA-IgA, EA-IgA, T classification, N classification, TNM stage and WHO type, were also included in this study (Table 1). None of these patients had previous malignant disease, second primary tumor, any history of radiotherapy, chemotherapy or surgical treatment. The 226 patients included 174 males (77.0%) and 52 females (23%) with ages ranging from 15 to 77 years (mean, 44 years). The tumor stages were defined according to the seventh edition of the American Joint Committee on Cancer Staging manual. All patients were treated with conventional two-dimensional radiotherapy with or without chemotherapy. The follow-up data were obtained by telephone or from the outpatient records. Overall survival (OS) was defined as the time from the date of diagnosis to the date of NPC-related death. Distant metastasis-free survival (DMFS) was defined as the interval from the date of diagnosis to the date of distant metastasis/metastases. The study was approved by the Institutional Research Ethics Committee of Sun Yat-Sen University Cancer Center and written informed consent was obtained from all subjects. All experimental methods were carried out in accordance with approved guidelines of Sun Yat-Sen University Cancer Center.
Immunohistochemistry
Immunohistochemical analysis was carried out to examine the IMPDH2 expression levels with a standard two-step method in 226 NPC tissue specimens. The paraffin-embedded NPC specimens were dried at 65 °C for 2 h. Subsequently, the slides were deparaffinised in xylene, rehydrated through a series of graded alcohol and immersed in 3% hydrogen peroxide for 15 min to block the endogenous peroxidase activity. Then the slides were boiled in citrate antigen retrieval solution (pH 6.5) for 20 min in a microwave oven for antigen retrieval. After washing three times for 5 min in phosphate buffered saline (PBS), the sections were incubated with a primary antibody against IMPDH2 (1:800 dilution; Abcam Antibodies, Epitomics, U.S.A.) at 4 °C overnight. After rinsing three times, the tissue sections were sequentially incubated with a secondary antibody for 1 hour at room temperature. After three further washes in PBS, the sections were stained with 3,3-diaminobenzidine (DAB), counterstained with Mayer’s haematoxylin, dehydrated and mounted. A negative control was obtained by replacing the primary antibody with PBS. Known immunostaining-positive slides were used as the positive controls.
IHC evaluation
Protein expression levels of IMPDH2 were evaluated by Semi-quantitative IHC detection. A brown particle in cytoplasm was considered as positive labeling. In brief, the staining intensity was classified as 0 (no staining), 1+ (weak), 2+ (moderate) or 3+ (strong) (I0, I1–3). Then, the proportion of tumor cells with that intensity was divided by the total number of tumor cells and recorded in 5% increments from 0 to 100 (P0, P1–3). Each IHC score was calculated based on the staining intensity and the proportion of the area stained according to the equation: IHC score = I1 × P1 + I2 × P2 + I3 × P3 (range 0–300). The evaluation of immunohistochemical results was performed by three independent pathologists who were blinded to the clinicopathological data. The same methods were applied for both tumorous and adjacent non-tumorous specimens.
Selection of cutoff score
Receiver operating characteristic (ROC) curve analysis was applied to determine a cutoff score for IMPDH2 expression, by using a 0, 1- criterion. Briefly, the sensitivity and specificity for the evaluated outcome were plotted to generate various ROC curves. The score with the shortest distance from the curve to the point (i.e., 0.0, 1.0) at both maximum sensitivity and specificity was selected as the cutoff score to determine the greatest number of tumors which were correctly classified as having or not having the clinical outcome. For the purpose of the ROC curve analysis, the clinicopathologic parameters were dichotomised as follows: VCA-IgA (<1:80 vs. ≥1:80), EA-IgA (<1:10 vs. ≥1:10), T stage (T1 + T2 vs. T3 + T4), N stage (N0 vs. N1 + N2 + N3), TNM stage (I + II vs. III + IV), WHO type (I + II vs. III) and survival status [NPC-related death vs. others (censored, alive or death from other causes)].
Cell lines and cell cultures
The immortalized nasopharyngeal epithelial cells (NPECs) induced by Bmi-1 (NPEC2 Bmi-1) were established and grown in keratinocyte/serum-free medium (Invitrogen). The NPC cell lines CNE1, CNE2, C666, HONE1 and SUNE1 were maintained in RPMI-1640 medium supplemented with 10% fetal bovine serum (FBS) (Gibco, USA). The cell lines were cultured in a humidified incubator at 37 °C with 5% CO2.
Western blotting
Equal amounts of whole-cell lysates were separated by SDS-polyacrylamide gel electrophoresis (PAGE) and subsequently transferred onto a polyvinylidene difluoride (PVDF) membrane (Pall Corp., Port Washington, NY). The membrane was blocked with 5% skimmed milk and then incubated with primary mouse monoclonal antibodies against IMPDH2 (1:1000 dilution, Abcam Co Ltd, USA) and GAPDH (1:1000 dilution; Abcam, Cambridge, MA, USA), respectively. After thoroughly washing the membrane, it was then incubated with the secondary anti-mouse antibody from Santa Cruz Biotechnology (Santa Cruz Biotechnology, CA, USA). Finally, the immunoreactive proteins were detected by an enhanced chemiluminescence (ECL) western blotting detection protocol.
Quantitative real-time polymerase chain reaction (qRT-PCR)
Total RNA was extracted from the NPC cell lines using Trizol regent (Invitrogen, Grand Island, NY, USA) and cDNA was synthesized by SuperScript Reverse Transcriptase kit (Promega, Madison, WI, USA) according to the manufacturer’s instruction. The primer sequences used to amplify IMPDH2 were: 5′-GCT CCT GTG CCT GAT GGA AT-3′ and 5′-CGG GCT CCT CCC CAA AAT AA-3′. GAPDH was used as an internal control for normalization.
Statistical analysis
Statistical analyses were performed with SPSS 19.0 (IBM). P values less than 0.05 were considered to be statistically significant. Overall survival (OS) was defined as the interval between surgery and death or between surgery and the last observation. Distant metastasis-free survival (DMFS) was defined as the time from surgery to distant metastasis or death due to NPC. The Chi-square test or Fisher’s exact test was performed to evaluate the correlation between IMPDH2 expression and the clinicopathological variables. The cumulative survival distributions were estimated using the Kaplan-Meier analysis and the log-rank test. The significance of various clinicopathological characteristics was evaluated using univariate Cox regression model. These statistically significant variables based on the univariate analysis were selected for reassessment in the multivariate Cox proportional hazard regression model.
Electronic supplementary material
Acknowledgements
This work was supported by grants from the Nature Science Foundation of China (No. 81401991) and the Science and Technology Foundation of Guangdong Province, China (Grant No. 2014A020212143).
Author Contributions
J.X.Z. and S.Y. designed the study. Y.X., S.Y.D., C.C., Y.G. and M.Y. collected the tissue samples and patient follow-up information. Y.X., Z.S.Z. and K.B.W. executed western blotting, qRT-PCR, ROC curve analysis and IHC experiments. Analysis of clinical data was performed by J.R., H.W.W. and S.Y., Y.X. and J.X.Z. drafted the article. All authors read and approved the final manuscript.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Yi Xu, Zhousan Zheng and Ying Gao contributed equally to this work.
Electronic supplementary material
Supplementary information accompanies this paper at doi:10.1038/s41598-017-00887-1
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sheng Ye, Email: yes20111212@163.com.
Jiaxing Zhang, Email: zjxlundy@hotmail.com.
References
- 1.Takagi M, Imamoto N. Control of nuclear size by NPC proteins. Adv Exp Med Biol. 2014;773:571–91. doi: 10.1007/978-1-4899-8032-8_26. [DOI] [PubMed] [Google Scholar]
- 2.Zhou L, et al. Enhanced expression of IMPDH2 promotes metastasis and advanced tumor progression in patients with prostate cancer. Clin Transl Oncol. 2014;16:906–913. doi: 10.1007/s12094-014-1167-9. [DOI] [PubMed] [Google Scholar]
- 3.Luo J, et al. Secular trends of nasopharyngeal carcinoma incidence in Singapore, Hong Kong and Los Angeles Chinese populations, 1973–1997. Eur J Epidemiol. 2007;22:513–521. doi: 10.1007/s10654-007-9148-8. [DOI] [PubMed] [Google Scholar]
- 4.Patel, S. G. & Shah, J. P. TNM staging of cancers of the head and neck: striving for uniformity among diversity. CA Cancer J Clin55 242, 261, 264 (2005). [DOI] [PubMed]
- 5.Tatsumi-Tamori A, Yoshizaki T, Miwa T, Furukawa M. Clinical evaluation of staging system for nasopharyngeal carcinoma: comparison of fourth and fifth editions of UICC TNM classification. Ann Otol Rhinol Laryngol. 2000;109:1125–9. doi: 10.1177/000348940010901208. [DOI] [PubMed] [Google Scholar]
- 6.Dostalek M, Gohh RY, Akhlaghi F. Inosine monophosphate dehydrogenase expression and activity are significantly lower in kidney transplant recipients with diabetes mellitus. Ther Drug Monit. 2013;35:374–83. doi: 10.1097/FTD.0b013e3182852697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Probst C, et al. Development of a recombinant cell-based indirect immunofluorescence assay (RC-IFA) for the determination of autoantibodies against “rings and rods”-associated inosine-5′-monophosphate dehydrogenase 2 in viral hepatitis C. Clin Chim Acta. 2013;418:91–96. doi: 10.1016/j.cca.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 8.Itoh O, et al. Induction by the guanosine analogue oxanosine of reversion toward the normal phenotype of K-ras-transformed rat kidney cells. Cancer Res. 1989;49:996–1000. [PubMed] [Google Scholar]
- 9.Knight RD, et al. Inosine monophosphate dehydrogenase and myeloid cell maturation. Blood. 1987;69:634–9. [PubMed] [Google Scholar]
- 10.Jackson RC, Weber G, Morris HP. IMP dehydrogenase, an enzyme linked with proliferation and malignancy. Nature. 1975;256:331–333. doi: 10.1038/256331a0. [DOI] [PubMed] [Google Scholar]
- 11.Floryk D, Tollaksen SL, Giometti CS, Huberman E. Differentiation of human prostate cancer PC-3 cells induced by inhibitors of inosine 5′-monophosphate dehydrogenase. Cancer Res. 2004;64:9049–9056. doi: 10.1158/0008-5472.CAN-04-1553. [DOI] [PubMed] [Google Scholar]
- 12.Zimmermann A, Gu JJ, Spychala J, Mitchell BS. Inosine monophosphate dehydrogenase expression: transcriptional regulation of the type I and type II genes. Adv Enzyme Regul. 1996;36:75–84. doi: 10.1016/0065-2571(95)00012-7. [DOI] [PubMed] [Google Scholar]
- 13.Nagai M, et al. Selective up-regulation of type II inosine 5′-monophosphate dehydrogenase messenger RNA expression in human leukemias. Cancer Res. 1991;51:3886–90. [PubMed] [Google Scholar]
- 14.He Y, et al. Identification of IMPDH2 as a tumor-associated antigen in colorectal cancer using immunoproteomics analysis. Int J Colorectal Dis. 2009;24:1271–9. doi: 10.1007/s00384-009-0759-2. [DOI] [PubMed] [Google Scholar]
- 15.Moosavi MA, Yazdanparast R, Sanati MH, Nejad AS. 3-Hydrogenkwadaphnin targets inosine 5′-monophosphate dehydrogenase and triggers post-G1 arrest apoptosis in human leukemia cell lines. Int J Biochem Cell Biol. 2005;37:2366–79. doi: 10.1016/j.biocel.2005.04.020. [DOI] [PubMed] [Google Scholar]
- 16.Fellenberg J, Bernd L, Delling G, Witte D, Zahlten-Hinguranage A. Prognostic significance of drug-regulated genes in high-grade osteosarcoma. Mod Pathol. 2007;20:1085–94. doi: 10.1038/modpathol.3800937. [DOI] [PubMed] [Google Scholar]
- 17.Zou J, et al. Elevated expression of IMPDH2 is associated with progression of kidney and bladder cancer. Med Oncol. 2015;32:373. doi: 10.1007/s12032-014-0373-1. [DOI] [PubMed] [Google Scholar]
- 18.Gharehbaghi K, et al. p210 bcr-abl confers overexpression of inosine monophosphate dehydrogenase: an intrinsic pathway to drug resistance mediated by oncogene. Leukemia. 1994;8:1257–63. [PubMed] [Google Scholar]
- 19.Natsumeda Y, Carr SF. Human type I and II IMP dehydrogenases as drug targets. Ann N Y Acad Sci. 1993;696:88–93. doi: 10.1111/j.1749-6632.1993.tb17144.x. [DOI] [PubMed] [Google Scholar]
- 20.Nagai M, Natsumeda Y, Weber G. Proliferation-linked regulation of type II IMP dehydrogenase gene in human normal lymphocytes and HL-60 leukemic cells. Cancer Res. 1992;52:258–61. [PubMed] [Google Scholar]
- 21.Laliberte J, Yee A, Xiong Y, Mitchell BS. Effects of guanine nucleotide depletion on cell cycle progression in human T lymphocytes. Blood. 1998;91:2896–904. [PubMed] [Google Scholar]
- 22.Takebe N, et al. IMP dehydrogenase inhibitor mycophenolate mofetil induces caspase-dependent apoptosis and cell cycle inhibition in multiple myeloma cells. Mol Cancer Ther. 2006;5:457–66. doi: 10.1158/1535-7163.MCT-05-0340. [DOI] [PubMed] [Google Scholar]
- 23.Sidi Y, et al. Growth inhibition and induction of phenotypic alterations in MCF-7 breast cancer cells by an IMP dehydrogenase inhibitor. Br J Cancer. 1988;58:61–63. doi: 10.1038/bjc.1988.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Olah E, et al. Induction of erythroid differentiation and modulation of gene expression by tiazofurin in K-562 leukemia cells. Proc Natl Acad Sci USA. 1988;85:6533–7. doi: 10.1073/pnas.85.17.6533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jayaram HN, Cooney DA, Grusch M, Krupitza G. Consequences of IMP dehydrogenase inhibition, and its relationship to cancer and apoptosis. Curr Med Chem. 1999;6:561–74. [PubMed] [Google Scholar]
- 26.Wright DG, et al. Tiazofurin effects on IMP-dehydrogenase activity and expression in the leukemia cells of patients with CML blast crisis. Anticancer Res. 1996;16:3349–51. [PubMed] [Google Scholar]
- 27.Fellenberg J, Kunz P, Sahr H, Depeweg D. Overexpression of inosine 5′-monophosphate dehydrogenase type II mediates chemoresistance to human osteosarcoma cells. PLoS One. 2010;5:e12179. doi: 10.1371/journal.pone.0012179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Penuelas S, Noe V, Ciudad CJ. Modulation of IMPDH2, survivin, topoisomerase I and vimentin increases sensitivity to methotrexate in HT29 human colon cancer cells. FEBS J. 2005;272:696–710. doi: 10.1111/j.1742-4658.2004.04504.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


