Abstract
Background
Femoroacetabular impingement (FAI) is a morphological abnormality of the hip joint that results in functional impairments during various activities of daily living (ADL) such as walking.
Purpose/Hypothesis
The purpose of this study was to determine if lower extremity joint loading differed between patients with FAI and controls and to determine whether these altered biomechanical parameters were associated with intra-articular abnormalities. It was hypothesized that patients with FAI would exhibit altered lower extremity joint loading during walking when compared with healthy controls and that these altered joint loading patterns would be associated with intra-articular abnormalities.
Study Design
Controlled laboratory study.
Methods
Lower extremity kinetics was assessed during walking at a self-selected speed in 15 presurgical patients with FAI and 34 healthy controls matched for age and body mass index. All participants underwent unilateral hip magnetic resonance imaging (MRI) to assess hip joint abnormalities. Hip joint abnormalities were assessed using a semiquantitative MRI-based scoring system. Self-reported outcomes of pain and function were obtained using the Hip disability and Osteoarthritis Outcome Score (HOOS), and physical performance was measured using the 6-minute walk test (6MWT). Group differences were assessed using an independent t test and analysis of variance. In the patients with FAI, associations of joint kinetics with HOOS subscores and intra-articular abnormalities were assessed using the Pearson (r) and Spearman (ρ) correlation coefficients, respectively.
Results
Compared with the control group, the FAI group exhibited a significantly increased severity of acetabular (FAI: 1.87 ± 1.55; control: 0.47 ± 0.79; P < .001) and femoral (FAI: 3.27 ± 2.79; control: 1.21 ± 1.55; P = .002) cartilage abnormalities, increased levels of pain (FAI: 65.0 ± 18.8; control: 98.2 ± 3.4; P = .001), and reduced function (FAI: 67.2 ± 21.5; control: 98.9 ± 3.4; P < .001) but similar walking speeds (FAI: 1.55 ± 0.19 m/s; control: 1.63 ± 0.22 m/s; P = .20) and 6MWT performance (FAI: 628.0 ± 91.2 m; control: 667.2 ± 73.4 m; P = .13). The FAI group demonstrated increased hip flexion moment impulses (FAI: 0.14 ± 0.04 N·m·s/kg; control: 0.11 ± 0.03 N·m·s/kg; P = .03), peak ankle dorsiflexion moments (FAI: 1.64 ± 0.16 N·m/kg; control: 1.46 ± 0.31 N·m/kg; P = .04), and ankle dorsiflexion moment impulses (FAI: 0.39 ± 0.07 N·m·s/kg; control: 0.31 ± 0.07 N m s/kg; P = .01) compared with the control group. Within the FAI group, an increased hip flexion moment impulse during walking was significantly correlated with increased pain (r = −0.60, P = .03), decreased ADL (r = −0.57, P = .04), and increased severity of acetabular cartilage abnormalities (ρ = 0.82, P < .01).
Conclusion
Patients with FAI exhibited altered hip and ankle joint loading patterns during walking. These data suggest that patients with FAI demonstrate both local and distal joint alterations during walking and that hip joint loading is directly related to hip joint abnormalities.
Clinical Relevance
The results of this study suggest that the hip flexion moment impulse may be an important biomechanical parameter to understand FAI, as the hip flexion moment impulse during walking was shown to be directly related to hip joint abnormalities on MRI.
Keywords: femoroacetabular impingement (FAI), gait, kinetics, cartilage abnormalities, hip function
Femoroacetabular impingement (FAI) is a morphological abnormality in which an abnormal contact area between the femoral head and acetabulum causes mechanical impingement of the hip joint.9 FAI presents itself in 3 forms (cam, pincer, and mixed types) and can cause significant disability, pain, and altered function during activities of daily living (ADL).9,36 Cam-type FAI is the result of an osseous deformity at the femoral head-neck junction, and pincer-type FAI is classified as overcoverage of the femoral head by the acetabulum. Finally, mixed-type FAI is a combination of both the cam and pincer types. The repetitive impact caused by the mechanical impingement during motions involving hip flexion and internal rotation may lead to acetabular labral injuries17 or other hip joint abnormalities. If FAI is not properly managed or treated, the condition may lead to degenerative effects of the hip joint such as osteoarthritis (OA).1,9,14,36 Another approach to studying the effects of FAI on hip joint health and function is through the use of magnetic resonance imaging (MRI) to assess articular cartilage degeneration in the FAI population.11,19–21 Studies using MRI have demonstrated that there is a high incidence of hip joint cartilage abnormalities and labral lesions in the FAI population.11,21 Gait assessments of patients with FAI during ADL may provide researchers and clinicians with the knowledge needed to detect this condition at an early stage and possibly reduce the need for surgical intervention.
Gait assessments in the FAI population, using kinematic and kinetic parameters, have not provided consistent results.2,6,10,13,15,27 It has been reported that patients with FAI demonstrated reduced range of motion of the hip joint in the sagittal plane6,13,27 and significantly less peak hip extension10 during gait compared with controls. A previous study found that patients with FAI demonstrated reduced external hip flexion moments during gait compared with controls10; yet, this result has not been supported by similar studies.6,13,15 A combination of gait and MRI-based assessments may therefore improve clinical understanding of the effects of FAI on lower extremity mechanics.
The altered lower extremity mechanics present in the FAI population during gait and the relationship of these biomechanical parameters with intra-articular abnormalities are unknown. Therefore, the purpose of this study was to assess the effects of FAI on lower extremity joint loading during gait, intra-articular abnormalities, and the possible relationship of these biomechanical parameters with hip joint abnormalities assessed with MRI. We hypothesized that patients with FAI would demonstrate altered lower extremity joint loading and an increased severity of hip joint abnormalities and that these altered joint loading patterns would be associated with hip joint abnormalities such as articular cartilage lesions and labral tears. More specifically, we hypothesized increased hip joint loading during gait and increased severity of hip joint abnormalities (eg, cartilage lesions) and that hip joint loading would be associated with hip joint pain and function in FAI patients.
METHODS
Participants
Fifteen symptomatic patients with FAI (11 male; mean age, 40.1 ± 7.5 years; mean body mass index [BMI], 25.2 ± 3.5 kg/m2) and 34 healthy controls matched for age and BMI (19 male; mean age, 43.2 ± 12.4 years; mean BMI, 24.0 ± 3.5 kg/m2) participated in this study. All patients with FAI were referred to this study by the University of California, San Francisco (UCSF) Orthopaedic Clinic. FAI was diagnosed based on radiological findings by 2 musculoskeletal radiologists (B.J.S., T.M.L.), as described below, as well as positive clinical signs of impingement (eg, positive flexion adduction and internal rotation [FADIR] test finding) determined during a physical examination by an orthopaedic surgeon (A.L.Z.).9,14,24 All patients with FAI were tested before arthroscopic surgery. The test limb of the patients with FAI was the limb that would undergo arthroscopic surgery. MRI and radiographs were used to measure alpha and lateral center-edge angles, respectively, to classify all patients with FAI as cam, pincer, or mixed type. An alpha angle of >55°7,35,37 measured on oblique axial MRI scans and a lateral center-edge angle of ≥35°23 on anterior-posterior pelvis radiographs were used to classify patients with FAI as either cam or pincer type, respectively. The patients with mixed-type FAI demonstrated radiological signs of both cam- and pincer-type FAI. Patients with FAI were excluded from this study if they had (1) contraindications to MRI; (2) total joint replacement of any lower extremity joint; (3) previous hip surgery on the affected side; (4) pain at any other lower extremity joint; (5) neurological, spine, or lower extremity conditions that would affect their performance during dynamic tasks performed in this study; and (6) any radiographic signs of hip OA on the affected side (Kellgren-Lawrence [KL] score12 of >1 or <2 mm of joint space).
All control participants’ data were part of a longitudinal observational study on hip OA. Each control participant received an anteroposterior weightbearing radiograph and was analyzed using the KL score.12 A total of 54 participants were screened for the current study, but only those without radiographic signs of hip OA (KL score ≤1) bilaterally and without any positive clinical signs of impingement (negative FADIR test finding) were included as control participants. Twenty participants were excluded from the current study, as they exhibited a KL score >1 or a positive FADIR test finding. The test limb in the control participants was assigned randomly. Similar to the patients with FAI, all control participants underwent MRI of the tested hip joint, and these MRI scans were used to assess for radiological signs of FAI. Controls were excluded if they had any of the following: (1) contraindications to MRI; (2) total joint replacement of any lower extremity joint; (3) previous hip trauma; (4) pain at any other lower extremity joint; (5) neurological, spine, or lower extremity conditions that would affect their performance during dynamic tasks performed in this study; and (6) any radiographic signs of knee or ankle OA.
All participants provided written informed consent before inclusion in the study. Our study was approved by the UCSF Committee on Human Research.
Self-Reported Outcomes
Each participant provided self-reported measures of pain and ADL using the Hip disability and Osteoarthritis Outcome Score (HOOS).22 The HOOS is a reliable and valid measure of hip joint function in those with hip OA.22 The HOOS subscores are based on a scale from 0 to 100, where 0 represents severe hip pain or poor function and 100 represents no hip pain or function issues.
Physical Performance
The 6-minute walk test (6MWT) was used to evaluate physical performance in both the patients with FAI and control participants. The 6MWT was shown to be related to pain and function in those with hip OA.26,31 Each participant was instructed to cover as much distance as possible while walking during a 6-minute time frame.16 The total distance, measured in meters, achieved by each participant was recorded and used to compare physical performance between both the FAI and control groups.
MRI Assessment
Each patient with FAI and control participant underwent unilateral hip MRI of the test limb. MRI was performed using a 3-T MRI scanner (MR750; GE Healthcare) and an 8-channel cardiac coil (GE Healthcare). Each participant was positioned supine on the MRI scanner and secured with straps to ensure a consistent position. Also, each participant’s feet were secured together to minimize any hip rotation during scanning. Sagittal, oblique coronal, and oblique axial MRI scans were obtained using an intermediate-weighted, fat-suppressed, fast spin echo sequence with a repetition time of 2400 to 3700 milliseconds, echo time of 60 milliseconds, field of view of 14 to 20 cm, matrix size of 288 × 224, and slice thickness of 3 to 4 mm.18
A previously validated, semiquantitative, MRI-based scoring system (Scoring hip osteoarthritis with MRI [SHOMRI])18 was used to assess abnormalities in the articular cartilage and labrum of the hip joint separately, and a total score for both the acetabular and femoral cartilage layers was calculated. The SHOMRI system18 has been previously used in assessments of hip joint abnormalities in patients with hip OA.8,16,28,29 Two musculoskeletal radiologists (B.J.S., T.M.L.), with a combined 30 years of experience, performed the assessments of hip joint abnormalities with interclass and intraclass coefficients of >0.90. The acetabular and femoral cartilage layers were divided into 4 and 6 subregions, respectively, using the sagittal and oblique coronal MRI scans.18 Articular cartilage lesions were scored in each of these regions using a 3-point scale. A score of 0 represents no cartilage loss, a score of 1 represents partial-thickness loss, and a score of 2 represents full-thickness loss. Each of the acetabular and femoral cartilage subregions was scored.
Labral abnormalities were scored on the sagittal, oblique coronal, and axial MRI scans in 4 subregions using a 6-point scale, where 0 represents a normal labrum, 1 represents an abnormal signal/fraying, 2 represents a simple tear, 3 represents labrocartilage separation, 4 represents a complex tear, and 5 represents maceration of the labrum. The scores within each subregion were summed together to determine a total labrum score.
Gait Analysis
Three-dimensional position data were collected at 250 Hz using a 10-camera motion capture system (Vicon), and ground-reaction force data were collected synchronously at 1000 Hz using 2 in-ground force plates (AMTI). A marker set consisting of 41 retroreflective markers15 was used to collect 3-dimensional position data. Calibration markers were placed bilaterally at the greater trochanter, medial and lateral femoral epicondyles, medial and lateral malleoli, and first metatarsal head. Pelvic tracking was performed using retroreflective markers placed at the anterior superior iliac spines, iliac crests, and L5/S1 joint. Segment tracking was performed using rigid body clusters, consisting of 4 markers each, placed at the lateral thighs and shanks. In addition, clusters consisting of 3 markers each were placed on the heel shoe counters and, along with the marker at the fifth metatarsal head, were used for tracking of the foot. A 1-second static calibration trial was obtained, and then all calibration markers were removed.
Each participant was asked to perform 5 successful walking trials at a self-selected speed. A trial was considered successful if the participant’s entire foot of the test limb made a clean strike on one of the force plates and their speed was within ±5% of their first successful trial (Figure 1). All raw marker position and ground-reaction force data were filtered using a fourth-order Butterworth filter at 6 Hz and 50 Hz, respectively.28 The standing calibration trial was used to create a 7-segment kinematic model consisting of the pelvis, bilateral thighs, shanks, and feet in Visual3D (v5.00.16; C-Motion). Local joint coordinate systems were created, and an unweighted least squares method was used to describe segment position and orientation.30 Joint coordinates were solved using a Cardan sequence of X-Y′-Z″, representing the medial-lateral, anterior-posterior, and superior-inferior directions, respectively. Joint angles were normalized to the standing calibration trial. Initial contact was defined as the time point at which the vertical ground-reaction force exceeded 20 N. The stance phase of gait was defined as initial contact to toe-off and time normalized to 101 points. Peak external joint moments and joint moment impulses in the sagittal plane were assessed during the stance phase of gait and compared between the patients with FAI and healthy controls. External joint moments in the sagittal plane were normalized by mass (N·m/kg) in which hip flexion, knee extension, and ankle dorsiflexion were considered positive. Joint moment impulses (N·m·s/kg) were calculated as the integral of a particular joint moment (Figure 2) with respect to time (s). The joint moment impulse has been previously used to assess joint loading during walking in various pathological conditions including patellofemoral joint OA33,34 and knee joint OA.5
Figure 1.
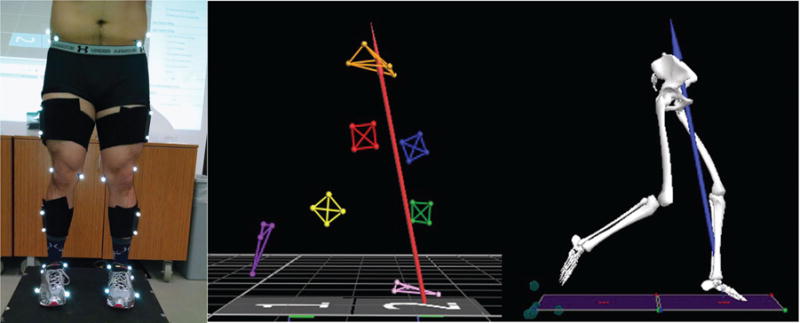
Retroreflective markers were placed on anatomic landmarks on each participant to track the positions of the pelvis, thighs, shanks, and feet (left). These marker position data were then tracked with a motion capture system (middle) and used to create a 7-segment musculoskeletal model to calculate lower extremity joint moments during walking (right).
Figure 2.
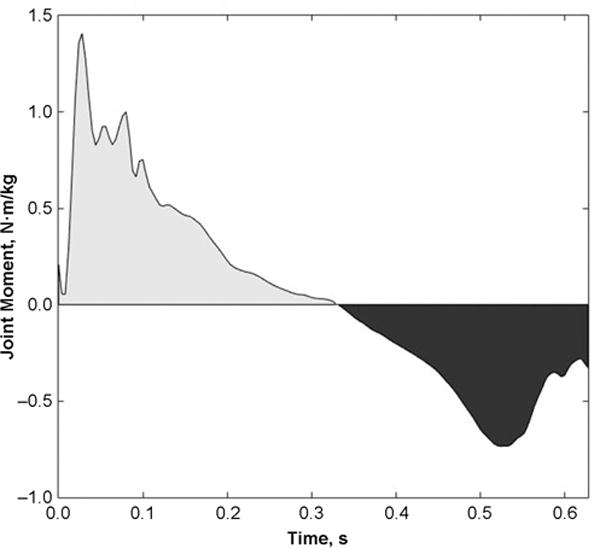
A representation of the external hip joint moment (N·m/kg) in the sagittal plane of a patient with femoroacetabular impingement during the stance phase of gait as a function of time. The joint moment impulse (N·m·s/kg) was calculated using the integral of a particular joint moment (ie, hip flexion or extension) with respect to time. In the plot above, the joint moment data within the lighter and darker regions were used to calculate hip flexion and extension moment impulses, respectively.
Statistical Analysis
Intra-articular abnormalities, walking speed, self-reported HOOS pain and ADL subscores, and 6MWT distances were assessed using independent t tests. All joint kinetics in the sagittal plane were compared between the patients with FAI and control participants using univariate analysis of variance. Upon determination of the significantly different joint kinetic parameters in the sagittal plane between the FAI and control groups, correlations between these significant joint kinetic parameters, hip joint abnormalities, and self-reported outcomes were determined. The Spearman correlation coefficient (ρ) was determined between the joint kinetic parameters in the sagittal plane and hip joint pathological abnormalities (ie, cartilage and labrum scores), while the Pearson correlation coefficient (r) was used to assess the association of these kinetic variables with HOOS pain and ADL subscores. All statistical analyses were performed using SPSS (v21; IBM Corp), and alpha was set a priori at the .05 level.
RESULTS
The FAI cohort exhibited increased levels of pain (P = .001) and decreased ability to perform ADL (P < .001), as measured by the HOOS (Table 1). The patients with FAI exhibited similar walking speeds (P = .20) and 6MWT distances (P = .13) as the control participants. The mean alpha and lateral center-edge angles for the patients with FAI were 58.7° ± 15.5° and 35.9° ± 9.4°, respectively. There were 10, 4, and 1 patients with mixed-, pincer-, and cam-type FAI, respectively.
TABLE 1.
Demographics, Walking Speeds, and Outcome Measures for the Study Groupsa
| FAI Group | Control Group | P Value | |
|---|---|---|---|
| Age, y | 40.1 ± 7.5 | 43.2 ± 12.4 | .39 |
| Body mass index, kg/m2 | 25.2 ± 3.5 | 24.0 ± 3.5 | .28 |
| Sex, male:female, n | 11:4 | 19:15 | .24 |
| Walking speed, m/s | 1.55 ± 0.19 | 1.63 ± 0.22 | .20 |
| 6MWT, m | 628.0 ± 91.2 | 667.2 ± 73.4 | .13 |
| HOOS pain subscore | 65.0 ± 18.8 | 98.2 ± 3.4 | .001 |
| HOOS ADL subscore | 67.2 ± 21.5 | 98.9 ± 3.4 | <.001 |
| Alpha angle, deg | 58.7 ± 15.5 | 55.2 ± 11.8 | .89 |
| Lateral center-edge angle, deg | 35.9 ± 9.4 | 31.4 ± 5.20 | .10 |
Data are reported as mean ± SD unless otherwise indicated. Bolded P values indicate a statistically significant difference between groups (P ≤ .05). 6MWT, 6-minute walk test; ADL, activities of daily living; FAI, femoroacetabular impingement; HOOS, Hip disability and Osteoarthritis Outcome Score.
The patients with FAI demonstrated an increased severity of acetabular (P < .001) and femoral (P = .002) cartilage abnormalities compared with the control participants, but both groups demonstrated a similar severity of labral abnormalities (P = .77) (Table 2). Compared with the control participants, a larger portion of the patients with FAI demonstrated acetabular (FAI: 80.0%; control: 32.4%) and femoral (FAI: 80.0%; control: 52.9%) cartilage abnormalities, but a smaller portion of the patients with FAI exhibited labral abnormalities (FAI: 86.7%; control: 94.1%). For both the FAI and control groups, the largest occurrence of acetabular cartilage abnormalities occurred in the superomedial region (FAI: 40.0%; control: 17.6%) (Table 3). The largest occurrence of femoral cartilage abnormalities in the FAI group (53.3%) was exhibited in the lateral region of the femoral cartilage layer, while the largest occurrence of femoral cartilage abnormalities was exhibited in the superomedial region in the control group (32.4%). In the patients with FAI, the largest occurrence of labral abnormalities occurred in the anterior region (73.3%), but in the control participants, the largest occurrence of labral abnormalities occurred in the anterosuperior region (79.4%).
TABLE 2.
| FAI Group | Control Group | P Value | |
|---|---|---|---|
| Total score for acetabular cartilage abnormalities | 1.87 ± 1.55 | 0.47 ± 0.79 | <.001 |
| Total score for femoral cartilage abnormalities | 3.27 ± 2.79 | 1.21 ± 1.55 | .002 |
| Total score for labral abnormalities | 6.60 ± 5.11 | 6.24 ± 3.55 | .77 |
Data are reported as mean ± SD. Bolded P values indicate a statistically significant difference between groups (P ≤ .05). FAI, femoroacetabular impingement; SHOMRI, Scoring hip osteoarthritis with MRI.
TABLE 3.
Distribution of Hip Joint Abnormalitiesa
| FAI Group (n = 15) | Control Group (n = 34) | |
|---|---|---|
| Acetabular cartilage | ||
| Anterior | 5 (33.3) | 5 (14.7) |
| Posterior | 4 (26.7) | 0 (0.0) |
| Superolateral | 5 (33.3) | 5 (14.7) |
| Superomedial | 6 (40.0) | 6 (17.6) |
| Femoral cartilage | ||
| Anterior | 5 (33.3) | 5 (14.7) |
| Posterior | 4 (26.7) | 2 (5.9) |
| Lateral | 8 (53.3) | 10 (29.4) |
| Superolateral | 7 (46.7) | 7 (20.6) |
| Superomedial | 7 (46.7) | 11 (32.4) |
| Inferior | 4 (26.7) | 5 (14.7) |
| Labrum | ||
| Anterior | 11 (73.3) | 26 (76.5) |
| Posterior | 5 (33.3) | 6 (17.6) |
| Anterosuperior | 9 (60.0) | 27 (79.4) |
| Superior | 10 (66.7) | 19 (55.9) |
Data are reported as n (%). FAI, femoroacetabular impingement.
The patients with FAI demonstrated increased hip flexion moment impulses (F1,47 = 5.20, P = .03), peak ankle dorsiflexion moments (F1,47 = 4.39, P = .04), and ankle dorsiflexion moment impulses (F1,47 = 11.5, P = .001) compared with the control participants (Table 4). In addition, although not significant, the patients with FAI demonstrated an increased knee extension moment impulse (F1,47 = 3.73, P = .06) (Figure 3). The patients with FAI exhibited an increased duration of hip flexion moments (F1,47 = 6.16, P = .02) and knee extension moments (F1,47 = 5.05, P = .03) during the stance phase.
TABLE 4.
Peak Joint Moment, Joint Moment Impulse, and Joint Moment Duration in the Sagittal Plane During the Stance Phase of Gaita
| FAI Group | Control Group | P Value | |
|---|---|---|---|
| Peak joint moment, N · m/kg | |||
| Hip flexion | 1.36 ± 0.26 | 1.29 ± 0.39 | .56 |
| Hip extension | −0.72 ± 0.21 | −0.81 ± 0.27 | .27 |
| Knee flexion | −0.59 ± 0.22 | −0.69 ± 0.27 | .19 |
| Knee extension | 0.69 ± 0.11 | 0.63 ± 0.17 | .18 |
| Ankle dorsiflexion | 1.64 ± 0.16 | 1.46 ± 0.31 | .04 |
| Ankle plantar flexion | −0.32 ± 0.12 | −0.34 ± 0.11 | .47 |
| Joint moment impulse, N·m·s/kg | |||
| Hip flexion | 0.14 ± 0.04 | 0.11 ± 0.03 | .03 |
| Hip extension | 0.10 ± 0.04 | 0.12 ± 0.04 | .35 |
| Knee flexion | 0.07 ± 0.02 | 0.09 ± 0.03 | .12 |
| Knee extension | 0.10 ± 0.02 | 0.08 ± 0.03 | .06 |
| Ankle dorsiflexion | 0.39 ± 0.07 | 0.31 ± 0.07 | .001 |
| Ankle plantar flexion | 0.02 ± 0.01 | 0.03 ± 0.01 | .62 |
| Joint moment duration, s | |||
| Hip flexion | 0.33 ± 0.09 | 0.27 ± 0.07 | .02 |
| Hip extension | 0.29 ± 0.08 | 0.33 ± 0.07 | .13 |
| Knee flexion | 0.27 ± 0.03 | 0.29 ± 0.06 | .30 |
| Knee extension | 0.35 ± 0.06 | 0.31 ± 0.06 | .03 |
| Ankle dorsiflexion | 0.50 ± 0.06 | 0.47 ± 0.07 | .15 |
| Ankle plantar flexion | 0.12 ± 0.03 | 0.13 ± 0.03 | .50 |
Data are reported as mean ± SD. Bolded P values indicate a statistically significant difference between groups (P ≤ .05). Positive joint moment values represent external hip flexion, knee extension, and ankle dorsiflexion moments, respectively. FAI, femoroacetabular impingement.
Figure 3.
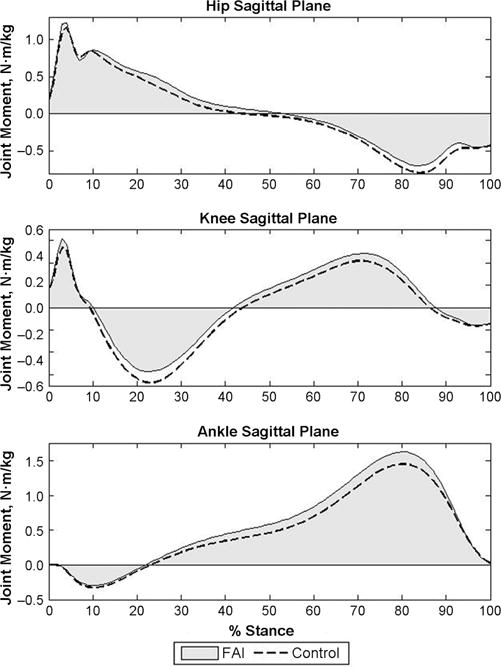
Joint moments in the sagittal plane during the stance phase of gait for the femoroacetabular impingement (FAI) and control cohorts. Positive external joint moments represent hip flexion, knee extension, and ankle dorsiflexion.
Within the FAI cohort, an increased hip flexion moment impulse during walking was significantly correlated with decreased HOOS pain subscores (increased pain; r = −0.60, P = .03), decreased ADL subscores (reduced function; r = −0.57, P = .04), and increased severity of acetabular cartilage abnormalities (ρ = 0.82, P < .01). There were no significant correlations between ankle joint kinetics, intra-articular joint abnormalities, and HOOS pain or ADL subscores.
DISCUSSION
In this study, joint kinetics in the sagittal plane was found to be altered in presurgical patients with FAI, compared with a control group, during free-speed walking. More specifically, the patients with FAI demonstrated increased peak ankle dorsiflexion moments, hip flexion moment impulses, and ankle dorsiflexion moment impulses during walking as well as an increased severity of cartilage abnormalities, pain, and reduced function. Patients with FAI who exhibited an increased hip flexion moment impulse during walking also demonstrated an increased severity of acetabular cartilage abnormalities, pain, and reduced function. Altered ankle joint kinetics in the patients with FAI may suggest distal joint compensations to optimally perform ADL such as walking. From the current study, it is impossible to determine if these altered joint loading patterns in the patients with FAI are causative or compensatory mechanisms of mechanical impingement at the hip joint, but the results of the current study provide insight into a possible relationship between hip joint loading and morphological abnormalities.
A portion of the previous studies that investigated hip joint kinetics in patients with FAI did not demonstrate any altered joint kinetics,2,6,13,15 while one previous study demonstrated reduced peak hip flexion moments in patients with FAI.10 Also, the magnitudes of the kinetic variables in the current study are larger than those presented in previous work2,10 and may be caused by differences in experimental methods or age of the patients with FAI between these studies. The patients with FAI in the current study demonstrated altered loading at the hip joint during walking. Contrary to the study by Hunt et al,10 the FAI group in the current study did not demonstrate any differences in peak hip flexion moments during walking compared with the control group. More specifically, the patients with FAI in the current study exhibited a higher hip flexion moment impulse during walking compared with controls because of a significantly longer duration of the hip flexion moment during the stance phase. This result suggests that patients with FAI experience higher hip joint loading over longer periods of each stride. An increased hip flexion moment impulse indicates altered hip joint loading and may also suggest altered distal joint compensations, as the ankle dorsiflexion moment impulse was higher, during walking in patients with FAI. The joint moment impulse was previously demonstrated to be an important indicator of joint loading in other pathological conditions,5,33,34 and the results of this study may suggest that the joint moment impulse is an important biomechanical parameter in the FAI population as well. Future studies including musculoskeletal modeling will provide estimates of the muscle and joint contact forces exhibited during walking in patients with FAI and provide a better understanding of the overall loading patterns within the hip joint.
Dissimilar to previous literature,2 the FAI group in the current study demonstrated increased peak ankle dorsiflexion moments and ankle dorsiflexion moment impulses compared with the control group. The altered ankle joint kinetics may suggest a compensatory mechanism used in walking by the FAI group to perform the walking task at a similar speed as the control group by generating increased forces at the ankle joint to allow for the progression of the center of mass over the base of support during the second half of the stance phase. When considering physical performance, the 6MWT distances achieved by the FAI group were similar to the distances achieved by the control group and indicate that while patients in the FAI group report increased pain and reduced function, they are still able to walk comparable distances compared with the controls. When considering the lack of differences in performance of the 6MWT, the increased peak ankle dorsiflexion moment and ankle dorsiflexion moment impulse in the FAI group may further suggest that the patients with FAI are compensating at the distal lower extremity in the presence of a painful hip to walk at a similar speed as the control group. It should also be noted that the patients with FAI demonstrated trends of increased knee extension moment impulses and may help to further support the notion of distal joint compensations in those with FAI. The altered knee and ankle joint kinetics in the FAI group were not associated with hip function or pain, and therefore, it may be possible that these altered distal joint mechanics were present before the patients with FAI became symptomatic. The results of the current study, along with previous work demonstrating altered knee and ankle joint kinetics during walking in patients with FAI,2 suggest that future studies should include analyses of the distal joints of the lower extremity in understanding the effects of FAI on walking performance and pain.
The use of semiquantitative MRI-based scoring methods such as the SHOMRI18 system provides a noninvasive assessment of hip joint abnormalities such as cartilage lesions and labral tears. Similar to a previous study in which acetabular cartilage abnormalities were present in approximately 79% of patients with FAI,21 acetabular cartilage abnormalities were present in 80.0% of the patients with FAI in the current study. A majority of these acetabular cartilage abnormalities occurred in the superomedial region and corresponds with previous work in which a higher occurrence of acetabular cartilage defects occurred in the middle superior zone of the acetabulum.11 Also, previous work demonstrated that approximately 70% of an asymptomatic population demonstrate labral abnormalities.25 In the current study, over 70% of participants in both the FAI (86.7%) and control (94.1%) groups demonstrated labral abnormalities, but the total amount of labral abnormalities within the FAI and control groups was not different. The results of the current study further validate that hip morphological characteristics influence the pattern of hip articular cartilage injuries,11 but the mechanism that causes cartilage damage remains unknown. Within the FAI cohort of the current study, the hip flexion moment impulse was significantly correlated to acetabular cartilage abnormalities, pain, and function. More specifically, patients with FAI with an increased hip flexion moment impulse demonstrated an increased severity of acetabular cartilage abnormalities, increased pain, and reduced function. The increased hip flexion moment impulse during walking may suggest an extended amount of loading that is applied to the anterior-superior and middle-superior regions of the acetabulum and result in greater acetabular cartilage abnormalities observed in the current study and in previous work.11,21 In addition, an increased severity of acetabular cartilage abnormalities may lead to increased levels of pain within the FAI cohort. Although the results of this study are not able to suggest causation for acetabular cartilage abnormalities, because of its cross-sectional analysis, the results of this study suggest that the hip flexion moment impulse is an important biomechanical parameter that may help explain the increased risk of the onset of hip OA in patients with FAI.1,9,14,36 Intervention programs, such as physical therapy, may consider strategies that aim to reduce the hip flexion moment impulse in patients with FAI to diminish acetabular cartilage abnormalities and the possible risk of the onset of hip OA.
There are limitations within the present study. It should be noted that the statistical methods employed in the current study may lead to an increased risk of type I errors, and therefore, the results of this study should be taken with caution. The current study did not obtain hip joint muscle strength or electromyography (EMG) data, which should be included in future studies involving patients with FAI, as previous work has shown that those with FAI exhibit reduced hip flexion muscle strength and altered EMG activity of hip muscles.4 An assessment of lower extremity EMG and strength will provide a better understanding of the neuromuscular alterations that occur, during ADL such as walking, in the FAI population. In addition, future studies assessing the effects of FAI during walking should analyze trunk segment biomechanics, as patients with FAI may demonstrate altered trunk mechanics, which could in turn contribute to altered hip joint loading. The current study included patients with cam-, pincer-, and mixed-type FAI, but a comparison between FAI types was not performed because of the limited size of the FAI cohort in this study. In the current study, both the FAI and control groups exhibited a similar percentage of participants with labral abnormalities. It should be noted that a previous study demonstrated that approximately 70% of asymptomatic participants present with labral abnormalities.25 Therefore, it is possible that the increased incidence of acetabular cartilage abnormalities, in addition to the labral abnormalities in the patients with FAI, may be a potential factor that causes those with FAI to experience severe hip joint pain and reduced function. Future studies should aim to understand the effects of each different type of FAI, as well as potential sex differences within the FAI group, on lower extremity biomechanics. FAI has been suggested to be an early precursor to hip OA,1,9,14,36 and therefore, when possible, future biomechanical studies involving patients with FAI should include quantitative MRI-based measurements3,32 (ie, T1ρ and T2 relaxation times), as these quantitative MRI-based measurements are able to identify early degenerative changes that occur before gross morphological changes.8
CONCLUSION
Patients with FAI exhibited altered hip and ankle joint kinetics during free-speed walking compared with control participants. In particular, patients with FAI demonstrated increased peak ankle dorsiflexion moments and ankle dorsiflexion moment impulses during the stance phase of gait, which may suggest a distal joint compensatory mechanism. The patients with FAI also demonstrated an increased hip flexion moment impulse during walking, and this altered loading at the hip joint was associated with an increased severity of acetabular cartilage abnormalities, increased pain, and reduced function. Future studies should include analyses of the entire lower extremity to understand the effects of FAI on distal joint function during ADL.
Acknowledgments
The authors acknowledge Aaron Sparks, MS, CSCS, for his assistance with data collection.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was supported by the National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases (P50 AR060752).
The content of this study is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 2.Brisson N, Lamontagne M, Kennedy MJ, Beaulé PE. The effects of cam femoroacetabular impingement corrective surgery on lower-extremity gait biomechanics. Gait Posture. 2013;37:258–263. doi: 10.1016/j.gaitpost.2012.07.016. [DOI] [PubMed] [Google Scholar]
- 3.Carballido-Gamio J, Link TM, Li X, et al. Feasibility and reproducibility of relaxometry, morphometric, and geometrical measurements of the hip joint with magnetic resonance imaging at 3T. J Magn Reson Imaging. 2008;28:227–235. doi: 10.1002/jmri.21411. [DOI] [PubMed] [Google Scholar]
- 4.Casartelli NC, Maffiuletti NA, Item-Glatthorn JF, et al. Hip muscle weakness in patients with symptomatic femoroacetabular impingement. Osteoarthritis Cartilage. 2011;19:816–821. doi: 10.1016/j.joca.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 5.Chang AH, Moisio KC, Chmiel JS, et al. External knee adduction and flexion moments during gait and medial tibiofemoral disease progression in knee osteoarthritis. Osteoarthritis Cartilage. 2015;23:1099–1106. doi: 10.1016/j.joca.2015.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diamond LE, Wrigley TV, Bennell KL, Hinman RS, O’Donnell J, Hodges PW. Hip joint biomechanics during gait in people with and without symptomatic femoroacetabular impingement. Gait Posture. 2016;43:198–203. doi: 10.1016/j.gaitpost.2015.09.023. [DOI] [PubMed] [Google Scholar]
- 7.Domayer S, Ziebarth K, Chan J, Bixby S, Mamisch T, Kim Y. Femoroacetabular cam-type impingement: diagnostic sensitivity and specificity of radiographic views compared to radial MRI. Eur J Radiol. 2011;80:805–810. doi: 10.1016/j.ejrad.2010.10.016. [DOI] [PubMed] [Google Scholar]
- 8.Gallo MC, Wyatt C, Pedoia V, et al. T1r and T2 relaxation times are associated with progression of hip osteoarthritis. Osteoarthritis Cartilage. 2016;24:1399–1407. doi: 10.1016/j.joca.2016.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 10.Hunt MA, Guenther JR, Gilbart MK. Kinematic and kinetic differences during walking in patients with and without symptomatic femoroacetabular impingement. Clin Biomech. 2013;28:519–523. doi: 10.1016/j.clinbiomech.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 11.Kaya M, Suzuki T, Emori M, Yamashita T. Hip morphology influences the pattern of articular cartilage damage. Knee Surg Sports Traumatol Arthrosc. 2016;24(6):2016–2023. doi: 10.1007/s00167-014-3297-6. [DOI] [PubMed] [Google Scholar]
- 12.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kennedy MJ, Lamontagne M, Beaulé PE. Femoroacetabular impingement alters hip and pelvic biomechanics during gait: walking biomechanics of FAI. Gait Posture. 2009;30:41–44. doi: 10.1016/j.gaitpost.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 14.Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome: a clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73:423–429. doi: 10.1302/0301-620X.73B3.1670443. [DOI] [PubMed] [Google Scholar]
- 15.Kumar D, Dillon A, Nardo L, Link TM, Majumdar S, Souza RB. Differences in the association of hip cartilage lesions and cam-type femoroacetabular impingement with movement patterns: a preliminary study. PM R. 2014;6:681–689. doi: 10.1016/j.pmrj.2014.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kumar D, Wyatt C, Chiba K, et al. Anatomic correlates of reduced hip extension during walking in individuals with mild-moderate radiographic hip osteoarthritis. J Orthop Res. 2015;33:527–534. doi: 10.1002/jor.22781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lavigne M, Parvizi J, Beck M, Siebenrock KA, Ganz R, Leunig M. Anterior femoroacetabular impingement, part I: techniques of joint preserving surgery. Clin Orthop Relat Res. 2004;418:61–66. [PubMed] [Google Scholar]
- 18.Lee S, Nardo L, Kumar D, et al. Scoring hip osteoarthritis with MRI (SHOMRI): a whole joint osteoarthritis evaluation system. J Magn Reson Imaging. 2015;41:1549–1557. doi: 10.1002/jmri.24722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li AE, Jawetz ST, Greditzer HG, 4th, Burge AJ, Nawabi DH, Potter HG. MRI for the preoperative evaluation of femoroacetabular impingement. Insights Imaging. 2016;7(2):187–198. doi: 10.1007/s13244-015-0459-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Link TM, Schwaiger BJ, Zhang AL. Regional articular cartilage abnormalities of the hip. AJR Am J Roentgenol. 2015;205:502–512. doi: 10.2214/AJR.15.14463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meermans G, Konan S, Haddad FS, Witt JD. Prevalence of acetabular cartilage lesions and labral tears in femoroacetabular impingement. Acta Orthop Belg. 2010;76:181–188. [PubMed] [Google Scholar]
- 22.Nilsdotter A, Lohmander L, Klassbo M, Roos E. Hip disability and Osteoarthritis Outcome Score (HOOS): validity and responsiveness in total hip replacement. BMC Musculoskelet Disord. 2003;4:10. doi: 10.1186/1471-2474-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Philippon MJ, Ejnisman L, Ellis HB, Briggs KK. Outcomes 2 to 5 years following hip arthroscopy for femoroacetabular impingement in the patient aged 11 to 16 years. Arthroscopy. 2012;28:1255–1261. doi: 10.1016/j.arthro.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 24.Philippon MJ, Maxwell RB, Johnston TL, Schenker M, Briggs KK. Clinical presentation of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2007;15:1041–1047. doi: 10.1007/s00167-007-0348-2. [DOI] [PubMed] [Google Scholar]
- 25.Register B, Pennock AT, Ho CP, Strickland CD, Lawand A, Philippon MJ. Prevalence of abnormal hip findings in asymptomatic participants: a prospective, blinded study. Am J Sports Med. 2012;40:2720–2724. doi: 10.1177/0363546512462124. [DOI] [PubMed] [Google Scholar]
- 26.Rydevik K, Fernandes L, Nordsletten L, Risberg MA. Functioning and disability in patients with hip osteoarthritis with mild to moderate pain. J Orthop Sports Phys Ther. 2010;40:616–624. doi: 10.2519/jospt.2010.3346. [DOI] [PubMed] [Google Scholar]
- 27.Rylander JH, Shu B, Andriacchi TP, Safran MR. Preoperative and postoperative sagittal plane hip kinematics in patients with femoroacetabular impingement during level walking. Am J Sports Med. 2011;39(Suppl):36s–42s. doi: 10.1177/0363546511413993. [DOI] [PubMed] [Google Scholar]
- 28.Samaan MA, Teng H-L, Kumar D, et al. Acetabular cartilage defects cause altered hip and knee joint coordination variability during gait. Clin Biomech. 2015;30:1202–1209. doi: 10.1016/j.clinbiomech.2015.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schwaiger BJ, Gersing AS, Lee S, et al. Longitudinal assessment of MRI in hip osteoarthritis using SHOMRI and correlation with clinical progression. Semin Arthritis Rheum. 2016;45:648–655. doi: 10.1016/j.semarthrit.2016.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Spoor CW, Veldpaus FE. Rigid body motion calculated from spatial co-ordinates of markers. J Biomech. 1980;13:391–393. doi: 10.1016/0021-9290(80)90020-2. [DOI] [PubMed] [Google Scholar]
- 31.Stratford PW, Kennedy DM, Woodhouse LJ. Performance measures provide assessments of pain and function in people with advanced osteoarthritis of the hip or knee. Phys Ther. 2006;86:1489–1496. doi: 10.2522/ptj.20060002. [DOI] [PubMed] [Google Scholar]
- 32.Subburaj K, Valentinitsch A, Dillon AB, et al. Regional variations in MR relaxation of hip joint cartilage in subjects with and without femoralacetabular impingement. Magn Reson Imaging. 2013;31:1129–1136. doi: 10.1016/j.mri.2013.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Teng H-L, MacLeod TD, Kumar D, Link TM, Majumdar S, Souza RB. Individuals with isolated patellofemoral joint osteoarthritis exhibit higher mechanical loading at the knee during the second half of the gait cycle. Clin Biomech. 2015;30:383–390. doi: 10.1016/j.clinbiomech.2015.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Teng H-L, MacLeod TD, Link TM, Majumdar S, Souza RB. Higher knee flexion moment during the second half of the stance phase of gait is associated with the progression of osteoarthritis of the patellofemoral joint on magnetic resonance imaging. J Orthop Sports Phys Ther. 2015;45:656–664. doi: 10.2519/jospt.2015.5859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tibor LM, Liebert G, Sutter R, Impellizzeri FM, Leunig M. Two or more impingement and/or instability deformities are often present in patients with hip pain. Clin Orthop Relat Res. 2013;471:3762–3773. doi: 10.1007/s11999-013-2918-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Werlen S, Leunig M, Ganz R. Magnetic resonance arthrography of the hip in femoroacetabular impingement: technique and findings. Oper Tech Orthop. 2005;15:191–203. [Google Scholar]
- 37.Yamasaki T, Yasunaga Y, Shoji T, Izumi S, Hachisuka S, Ochi M. Inclusion and exclusion criteria in the diagnosis of femoroacetabular impingement. Arthroscopy. 2015;31:1403–1410. doi: 10.1016/j.arthro.2014.12.022. [DOI] [PubMed] [Google Scholar]


