Abstract
Purpose
Neighborhood-level socioeconomic disadvantage and lower individual-level socioeconomic status are associated with poorer sleep health in adults. However, few studies have examined the association between neighborhood-level disadvantage and sleep in adolescents, a population at high-risk for sleep disturbances.
Methods
The current study is the first to examine how objective (i.e. via census tract-level data) and subjective measures of neighborhood disadvantage are associated with sleep in a racially/ ethnically and socioeconomically diverse sample of 2,493 youth [Non-Hispanic White (20%), Hispanic (46%), Asian (21%), and Multiracial/ Other (13%)].
Results
Findings indicated that greater perceived neighborhood-level social cohesion and lower neighborhood-level poverty were associated with better sleep outcomes in adolescents. However, there was some evidence that the magnitude of the associations differed according to family-level socioeconomic status and race/ ethnicity.
Conclusions
Findings suggest that subjective and objective neighborhood characteristics may affect the sleep health of older adolescents, with certain demographic subgroups being particularly vulnerable.
Keywords: Adolescents, Sleep, Neighborhoods, Socioeconomic Status, Poverty, Social Environments
Sleep problems in youth are associated with a wide variety of adverse consequences, including increased risk of depression and anxiety, poorer academic functioning, obesity, cardiovascular risk factors, and motor vehicle accidents (Curcio et al., 2006; Ivanenko et al., 2005; Javaheri et al., 2011; Wong et al., 2015). In fact, the impact of driver sleepiness on serious motor-vehicle related injuries and fatalities is comparable to that of driving under the influence of alcohol (Powell et al., 2001). Adolescence is a critical time for examining sleep health because this is a particularly vulnerable period for the development of sleep problems and sleep patterns that can persist into adulthood (Carskadon et al., 2004). Findings indicate that minority adolescents (primarily African American or Hispanic) and adolescents from lower SES (socioeconomic status) families or single-parent homes, are at increased risk for sleep problems, including insufficient sleep duration, poor quality sleep, and greater variability in sleep patterns (Keyes et al., 2015; Matthews et al., 2014; Moore et al., 2011; Troxel et al., 2014) as compared to their non-Hispanic white or higher SES counterparts. Therefore, it is important to examine underlying social determinants of adolescent sleep problems in order to identify high-risk groups and potential novel targets of intervention to improve adolescent health trajectories and population health more generally.
Increasingly, it is recognized that beyond individual-level social determinants of health, neighborhood level factors also contribute to diverse indicators of health. In particular, a burgeoning literature suggests that neighborhood level factors (including neighborhood-level SES), as well as subjective measures of neighborhood characteristics (including greater social disorder and lower neighborhood cohesion), are associated with poorer sleep quality in adults (Brouillette et al., 2011; Hale et al., 2010; Hale et al., 2013; Hill et al., 2009). Theoretically, disadvantaged neighborhoods, which are characterized by low levels of social cohesion and safety and high levels of neglect, disrepair, and crime, may lead to heightened feelings of vigilance and psychological distress—opponent processes of sleep (Hale et al., 2010; Hale et al., 2013). These negative affective states, in turn, may lead to chronic activation of the physiological stress response and exposure to stress hormones associated with impaired sleep. Such environmental influences on sleep may be particularly salient among adolescents, as this is a time of increasing autonomy from parents and greater influence from the broader social context, as well as dramatic changes in sleep and circadian biology (Carskadon et al., 2004). As such, and consistent with the objectives of Healthy People 2020 (2016), there have been increasing calls from researchers and policy-makers for greater consideration of neighborhood-level effects on child and adolescent health disparities, including sleep health (Panel on High-Risk Youth et al., 1993).
However, only a handful of studies to date have investigated neighborhood-level factors and adolescent sleep, and the existing studies have not included both objective and subjective neighborhood characteristics, have limited assessments of sleep, and have not included racially/ ethnically diverse samples, including Hispanics and Asians (Felden et al., 2015). In particular, living in a low SES neighborhood is associated with increased risk of certain sleep disorders, such as obstructive sleep apnea (OSA), which may reflect the direct effects of exposures to environmental toxins that can increase risk of sleep-related breathing disorders (Brouillette et al., 2011). Using data from the National Survey of Children’s Health (NSCH) (Singh and Kenney, 2013; Smaldone et al., 2007) and the Mobile Youth Survey (Umlauf et al., 2014), several studies found that neighborhood safety and exposure to violence may be associated with increased frequency of inadequate sleep or sleep problems in both children and adolescents. Importantly, however, although the NSCH data provides a comprehensive assessment of a variety of neighborhood characteristics including social conditions, and built environment characteristics, the validity of assessing inadequate sleep via parent report is questionable particularly for older adolescents. Nevertheless, Bagley and colleagues (2016) found similar results using objectively measured sleep efficiency (via wrist actigraphy) and subjectively measured sleep quality and problems. The use of objective and subjective measures of sleep are significant strengths of Bagley’s study; however, several important questions remain as there was limited assessment of neighborhood characteristics, and limited racial/ ethnic diversity in this sample which lacked Asian and Hispanic youth. Considering broader racial/ethnic differences in the association between neighborhood-level factors and sleep is important, given prior research showing that racial/ ethnic minorities have higher rates of sleep problems (Matthews et al., 2014; Roberts et al., 2006) as compared to non-Hispanic whites and Asians, and are more likely to live in impoverished neighborhoods compared to non-Hispanic whites, even after accounting for individual-level SES (Pattillo, 2005). Furthermore, as Jarrin and colleagues (2014) articulate, families with lower socioeconomic status have less organized houses, with more noise pollution, particularly in urban environments and less knowledge about sleep hygiene, all of which can contribute to increased risk for sleep disturbance. Thus, there may be important interactions between neighborhood-level disadvantage and family-level SES that potentiate the risk for sleep disturbances in adolescents. Only a handful of studies exist on neighborhood factors and sleep (as reviewed in Felden et al., 2015). Of these studies, few have considered both objective and subjective neighborhood characteristics, most have utilized samples of children and/ or younger adolescents and have limited racial/ ethnic diversity, and few have examined multiple sleep outcomes germane to adolescent health and development or examined the degree to which indicators of family-SES such as maternal education or race/ ethnicity may moderate observed associations between neighborhood characteristics and adolescent sleep.
Therefore, the purpose of the present study is to extend the limited existing literature on neighborhood factors and sleep by examining both subjective (i.e., perceived neighborhood social cohesion, safety, and monitoring) and objective (i.e., census-tract determined percent living below the federal poverty level) neighborhood characteristics and sleep in a racially/ ethnically diverse sample of older adolescents from Southern California. We include key sleep domains that have been identified as particularly important for adolescent health and functioning (National Sleep Foundation, 2000): self-reported sleep timing (bedtimes), sleep duration and variability in sleep duration (weekdays vs. weekends), and sleep quality. We expected that adolescents who lived in neighborhoods where they perceived greater neighborhood disadvantage (as indicated by lower social cohesion, perceived safety, and monitoring) and where a greater percentage of households were living below the federal poverty line would report later bedtimes, shorter sleep duration, poorer sleep quality, and would exhibit greater difference in weekend versus weekday sleep duration, as this difference score may be an indicator of “weekend oversleep” for sleep-deprived teens (Hasler and Clark, 2013). Furthermore, we explored whether the strength of the associations between neighborhood-level characteristics and sleep characteristics differed by maternal education, which has been used as an indicator of family-level SES in prior research (Korupp et al., 2002) or the adolescent’s race/ ethnicity. Consistent with Jarrin and colleagues’ work (2014), we hypothesized that the influence of neighborhood-level disadvantage on sleep would be stronger among those adolescents who identify as Hispanic or “other” or those who have a mother with lower educational attainment, by contributing to increased stress in the home and potentially decreased parental involvement or education concerning healthy sleep practices.
Methods
Adolescents from this study originated from 16 middle schools across three school districts in southern California that were part of a large, ongoing longitudinal study with a school-based intervention that occurred in 2008 (D’Amico et al., 2012). As previously reported (D’Amico et al., 2012), 92% of parents returned a consent form at the baseline and 71% gave permission for their child to participate in the baseline survey. Of consented students, 94% completed the baseline survey, which is higher or comparable to other school-based survey completion rates with this population (Kandel et al., 2004). We continued to follow two cohorts of youth (the original 6th grade cohort, and the original 7th grade cohort) as they transitioned into high school. For this study, we used web surveys that were administered from May 2014 to May 2015 when youth were on average 17.3 years old (n=2,493). Missingness was less than 0.5% for all variables; (for mother’s education 7.4% of respondents replied ‘Don’t Know’ and are excluded from the analyses). All research on human subjects was approved by the institution’s IRB.
Race/ethnicity and maternal education (hypothesized effect modifiers)
At baseline, respondents classified themselves by ethnicity (Hispanic or not Hispanic) and were then asked about their race (National Institutes of Health (NIH), 2001). These responses were categorized as non-Hispanic white (20.2%), Hispanic (46.0%), Asian (20.5%), and “Multiracial/Other” (13.3%; which included African American 2.3%, American Indian 0.6%, Native Hawaiian 0.7%, Multiracial 9.8%). In addition to examining racial/ethnic differences in observed associations, we also included a measure of educational attainment of the participant’s mother (less than high school diploma/GED, high school diploma, or greater than high school education) as an indicator of family-SES.
Covariates
We adjusted for covariates known to be associated with sleep such as age, gender, and family structure (i.e., two-parent household versus single-parent household). We also adjusted for mental health using the Mental Health Inventory (MHI-5) (Berwick et al., 1991) which comprises five items focused on past month anxiety and depression symptoms. Scores on the MHI-5 were scaled such that they ranged from 0 to 100, with higher scores indicating better mental health (α=0.78). Finally, we included an indicator for whether the student had attended one of the original intervention schools.
Sleep measures
Participants were asked when they “usually go to bed” and “wake up” separately for weekdays and weekend days. Similar measures have been used in several prior studies with adolescents (Larson et al., 2015; Pasch et al., 2010), and have been shown to significantly correlate with diary and actigraphy assessments (Wolfson et al., 2003). Specific sleep outcomes were chosen that have previously been linked with diverse indicators of adolescent behavioral and physical health (National Sleep Foundation, 2000) and included: self-reported bedtimes (weekdays and weekends), total sleep time (TST; derived from reported bedtimes and wake times (weekdays and weekends)), the difference between weekend and weekday sleep (i.e., weekend TST-weekday TST), and trouble sleeping assessed by a single item from the Patient Health Questionnaire (PHQ) Somatic Symptom Severity Scale which asked: “During the past 4 weeks, how much have you been bothered by any of the following problems?”, with response options including: not bothered, bothered a little, bothered a lot (Kroenke et al., 2002). Given the considerable variability in adolescent sleep patterns during the school week and on the weekends, we analyzed weekday and weekend bedtimes and TST separately.
Neighborhood measures
We utilized three subjective measures and one objective measure of neighborhood disadvantage as predictors of our sleep outcomes. Neighborhood cohesion, monitoring, and safety were our three subjective neighborhood measures. Neighborhood cohesion was comprised of two positive (e.g. “people in my neighborhood are willing to help their neighbor”) and two negative (e.g. “People in my neighborhood generally don’t get along with each other”) items which were rated on a 5-point scale (1=Strongly agree, 5=Strongly disagree), drawn from the Sampson Social Cohesion scale (Sampson et al., 1997). Positive items were reverse coded and averaged for a neighborhood cohesion score where a higher value indicates more cohesion (α=0.67). Three items from Sampson’s social control scale (cite) assessed Neighborhood Monitoring (Sampson et al., 1997) (e.g. “If a group of neighborhood children were skipping school and hanging out on a street corner, how likely is it that your neighbors would do something about it?”). These items were rated on a 5-point scale (1=very unlikely, 5=very likely) and averaged such that a higher score indicates more monitoring (α=0.67). Six items assessed Neighborhood Safety (Winstanley et al., 2008) (e.g., “There is a lot of crime in my neighborhood”) and were rated on a 5-point scale (1=Strongly agree, 5=Strongly disagree). The six items were averaged such that a higher score indicates more neighborhood safety (α=0.92). Our objective measure of Neighborhood-Level Poverty was defined as the percent of the population below the federal poverty level in each census tract which we obtained from the American Community Survey five-year average for 2009–2013. This variable was linked to respondent’s census tracts which were geocoded using 2010-based Census geography definitions.
Analytic Strategy
Descriptive statistics (mean/SD or percentage) are presented for sociodemographic characteristics, and sleep outcomes. Additionally, we describe differences in subjective and objective neighborhood measures separately by race/ethnicity and mother’s education. For these comparisons we utilized analysis of variance (ANOVA) and post-hoc tests to examine pairwise comparisons among the four racial/ethnic groups and the three mother’s education categories. Due to the large number of post-hoc tests, we used the Benjamini and Hochberg method to adjust p-values (Benjamini and Hochberg, 1995).
For our primary analyses, we conducted a series of models that regressed each individual sleep outcome on each of the neighborhood measures in separate models, controlling for sociodemographics, the intervention school indicator (0/1), and mental health symptoms. Continuous sleep outcomes (bedtimes, TST, and weekend-weekday TST difference) were modeled with general linear models. Multinomial logistic regression was employed for our three-level categorical trouble sleeping outcome with “not at all bothered” by trouble sleeping serving as the reference category. We expanded on this basic model by running two additional sets of models, one set included the interaction of race/ethnicity with the neighborhood predictors and the other set included the interaction of mother’s education with the neighborhood predictors. This allowed us to test whether the association of the neighborhood measures with the sleep outcomes differed by race/ethnicity and mother’s education. All models were clustered by census tract to account for similarities among youth in the same neighborhoods (i.e., tracts).
Results
Our sample was 54.19% female, mostly Hispanic (45.97%; Asian=20.54%, non-Hispanic White=20.14%, Multi-racial/other=13.36%), and approximately 17.31 (SD=0.67) years old (Table 1). The majority of respondents had a mother with greater than a high school degree/GED (67.78 %) and lived in a two parent household (65.06%). On average respondents reported going to bed at 11:22pm during the week and TST during the week was approximately 7.40 hours (SD=1.41). Average bedtime was later during the weekend (12:34am) and TST was longer (9.09 hours, SD=1.63) than on weekdays. Slightly over half (53%) of the respondents reported not being bothered by trouble sleeping, 31% said they were bothered a little and 16% were bothered a lot.
Table 1.
Sample Descriptives
| Overall | ||
|---|---|---|
|
| ||
| n=2493 | ||
|
| ||
| Mean/ % | SD | |
| Demographics | ||
| Age | 17.31 | 0.67 |
| Female (%) | 54.19 | |
| Race/Ethnicity () | ||
| Asian | 20.54 | |
| Hispanic | 45.97 | |
| Multi-Racial/Other | 13.36 | |
| White | 20.14 | |
| Mother’s Education (%) | ||
| <High School/GED | 14.60 | |
| High School Diploma | 17.63 | |
| >High School/GED | 67.78 | |
| Two Parent Household (%) | 65.06 | |
| MHI-5 | 65.66 | 20.56 |
| Sleep Outcomes | ||
| Weekday Bedtimea | 11:22 | |
| Weekend Bedtimea | 12:34 | |
| Weekday Total Sleep Time, Hours | 7.40 | 1.41 |
| Weekend Total Sleep Time, Hours | 9.09 | 1.63 |
| Difference in Total Sleep Time | 1.69 | 1.92 |
| Bothered By Trouble Sleeping (%) | ||
| A Little | 31.00 | |
| A Lot | 15.86 | |
| Not Bothered | 53.14 | |
Note.
Estimated average bedtimes are reported. Analyses conducted with the bedtime variables use minutes from midnight, scaled to every 10 minutes.
Calculated as weekend − weekday Bedtime
Table 2 presents descriptive information for the subjective and objective neighborhood measures overall and both by race/ethnicity and mother’s education. For race/ethnicity, white respondents reported the most neighborhood cohesion, the most monitoring, the greatest neighborhood safety and the lowest percentage below the federal poverty line. Hispanic respondents had the lowest averages on neighborhood subjective measures and a greater percentage fell below the federal poverty line. Those with a mother that had greater than a high school education had the highest neighborhood cohesion, monitoring and safety scores, and the lowest percentage below the federal poverty line on average. All omnibus tests for significance were significant at p<.0001.
Table 2.
Subjective and Objective Neighborhood Measures by Race/Ethnicity and Mother’s Highest Education†
| Overall | Asian | Hispanic | Multiracial/Other | White | < HS | HS | >HS | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| n=2493 | n=512 | n=1146 | n=333 | n=502 | N=337 | N=407 | N=1565 | |
|
| ||||||||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |
| Neighborhood Cohesion | 3.48 (0.77) | 3.59h,w (0.70) | 3.31a,m,w (0.76) | 3.55h,w (0.75) | 3.74a,h,m (0.77) | 3.16h,g (0.74) | 3.36l,g (0.8 0) | 3.60l,h (0.75) |
| Neighborhood Monitoring | 3.50 (0.92) | 3.55h,w (0.83) | 3.39a,w (0.93) | 3.51w (1.00) | 3.72a,h,m (0.88) | 3.32g (0.95) | 3.30g (0.9 5) | 3.60l,h (0.89) |
| Neighborhood Safety | 4.14 (0.95) | 4.27h (0.87) | 3.96a,m,w (1.00) | 4.27h (0.93) | 4.36h (0.84) | 3.74h,g (0.99) | 3.97l,g (1.0 0) | 4.28l,h (0.89) |
| Neighborhood Poverty¥ | 12.99 (8.64) | 9.37h,m (6.23) | 16.47a,m,w (9.43) | 11.40a,h,w (7.95) | 9.21h,m (5.04) | 19.8 9h,g (9.36) | 14.1 7l,g (8.7 1) | 10.74 l,h (7.37) |
Note.
All P-values from ANOVA tests are statistically significant at p<.0001.
N’s for mother’s education categories do not sum to 2493 due to item missingness. Post-hoc tests were conducted to test for differences between the racial/ethnic categories and mother’s education categories. The Benjamini and Hochberg false discovery rate (FDR) correction was used to adjust p-values given the multiple testing. Superscripts race/ethnicity indicate significance at p<.05: “a” significantly different than Asian, “h” significantly different than Hispanic, “m” significantly different than multiracial /other, “w” significantly different than white. Superscripts for mother’s education indicate significance at p<.01: “l” less than high school, “h” high school, “g” greater than high school.
Percent below Federal poverty level.
Main effects
Results of multivariable main effects models showed that as neighborhood cohesion increased, the odds of being bothered a little or bothered a lot by trouble sleeping decreased (Table 3). Additionally, teens from neighborhoods with a greater percentage below the federal poverty line reported earlier weekday and weekend bedtimes. There were no significant main effects of neighborhood safety or monitoring on adolescent sleep outcomes.
Table 3.
Models Predicting Sleep-Related Outcomes using Subjective and Objective Neighborhood Characteristicsa
| Weekday Bed Time (10 mins) | Weekend Bed Time (10 mins) | TST Weekday (Hour) | TST Weekend (Hour) | TST Difference (Weekend−Weekday) | Bothered A Lot |
Bothered A Little |
|
|---|---|---|---|---|---|---|---|
| Est (95% CI) | Est (95% CI) | Est (95% CI) | Est (95% CI) | Est (95% CI) | OR (95% CI) | OR (95% CI) | |
| Subjective Neighborhood Characteristics | |||||||
| Neighborhood Cohesion | 0.00 (−0.41, 0.41) | −0.41 (−0.99, 0.17) | −0.01 (−0.10, 0.07) | 0.02 (−0.08, 0.12) | 0.04 (−0.08, 0.16) | 0.74 (0.63, 0.86)*** | 0.80 (0.70, 0.90)*** |
| Neighborhood Monitoring | −0.22 (−0.62, 0.17) | 0.20 (−0.26, 0.66) | 0.03 (−0.04, 0.10) | −0.03 (−0.11, 0.05) | −0.06 (−0.15, 0.04) | 0.98 (0.84, 1.14) | 1.04 (0.92, 1.16) |
| Neighborhood Safety | 0.06 (−0.34, 0.46) | −0.11 (−0.64, 0.41) | 0.02 (−0.05, 0.09) | 0.01 (−0.09, 0.10) | −0.01 (−0.13, 0.10) | 0.92 (0.80, 1.05) | 0.97 (0.86, 1.10) |
| Objective Neighborhood Characteristic | |||||||
| Neighborhood Poverty | −0.09 (−0.14, −0.05)*** | −0.06 (−0.11, −0.01)* | 0.00 (−0.01, 0.01) | 0.00 (−0.01, 0.01) | 0.00 (−0.01, 0.01) | 1.00 (0.99, 1.02) | 1.01 (0.99, 1.02) |
All neighborhood predictors entered individually in a model to predict each sleep outcome, with covariate adjustment.
p<0.5,
p<0.01,
p<0.001
Maternal education interactions
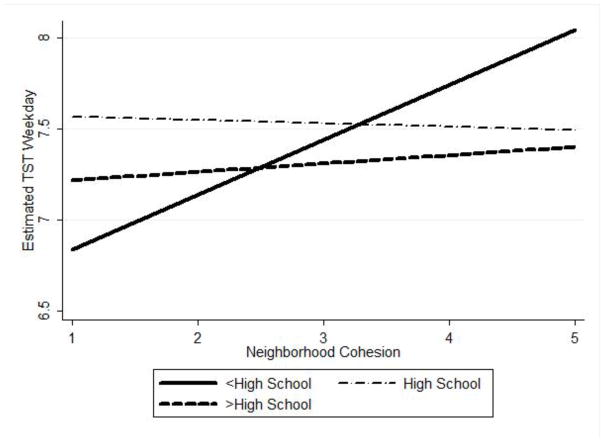
In multivariable models that included interaction terms between maternal education and neighborhood-level predictors, we found a significant interaction between neighborhood cohesion and maternal education on weekday TST (beta=0.28 (0.11), p=0.013).
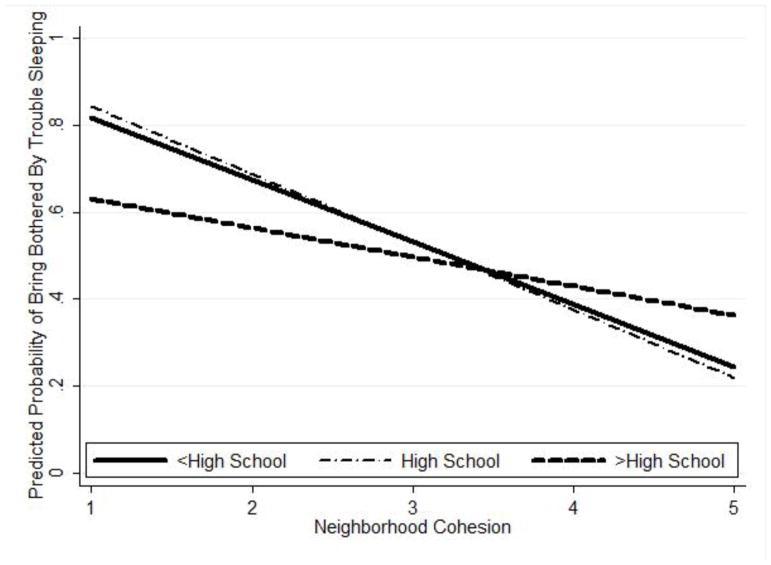
As shown in Figure 1, for adolescents with maternal education less than high school, as neighborhood cohesion increased, weekday TST time increased (after adjustment for covariates). However, for adolescents with maternal education of high school or greater, as neighborhood cohesion increased, the slope remained rather constant. Additionally, we found a significant interaction between maternal education and social cohesion on trouble sleeping such that for teens with mother’s with lower education there was a significant association between neighborhood cohesion and trouble sleeping (OR=0.65(1.19), p=0.012). To facilitate interpretation of this interaction effect, for graphical purposes only (Figure 2), we collapsed the categories of bothered a little and bothered a lot into bothered at all. The figure shows that there was a stronger, inverse association between neighborhood cohesion and odds of trouble sleeping among those with lower maternal education as compared to those with higher maternal education, after controlling for covariates.
Figure 1.
Interaction between maternal education and neighborhood cohesion on weekday total sleep time (TST).
Figure 2.
Interaction between maternal education and neighborhood cohesion on the predicted probability of having trouble sleeping.
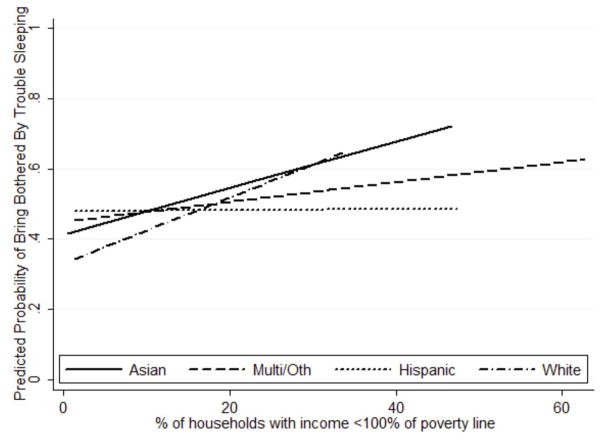
Race/ethnicity interactions
We found one significant interaction between race/ethnicity and neighborhood-level factors on sleep. Specifically, as shown in Figure 3, non-Hispanic white adolescents showed a stronger positive association between living in more impoverished neighborhoods (i.e., greater percentage of households living below the federal poverty) and risk of trouble sleeping compared to Hispanic and multi-racial/ other adolescents. However, it should be noted that there was a constriction of range in the neighborhood-level poverty variable, particularly for non-Hispanic whites where the average percent of households living below the poverty line was 9.22% (compared to 16.47% for Hispanics, 11.40% for multi-racial/other, and 9.37% for Asian youth).
Figure 3.
Interaction between race/ethnicity and neighborhood-level poverty on the predicted probability of having trouble sleeping.
Discussion
Consistent with objectives of Healthy People 2020 (2016), we examined the association between broader social and environmental determinants of adolescent sleep health disparities. Specifically, we assessed associations between subjective and objective indicators of neighborhood-level disadvantage and several key sleep outcomes in a racially/ ethnically diverse sample of older adolescents. Our work adds to the limited number of studies that have examined neighborhood-level influences on adolescent sleep in several ways. First, we include an older sample of adolescents, whereas much of the existing work has focused on children and/ or younger adolescents. Second, we include key sleep outcomes, including sleep timing, duration, variability, and quality, and we found different patterns of associations for neighborhood measures in relation to these specific sleep outcomes. Third, we examined both objective (via Census data) and subjective measures of neighborhood characteristics as separate correlates of health behaviors, which is critical given evidence of differential associations between objective and subjective neighborhood characteristics and health behaviors and outcomes (DeSantis et al., 2016; Schultz et al., 2013). Fourth, our inclusion of a large, racially/ ethnically and socioeconomically diverse sample of youth allowed us to examine the degree to which race/ ethnicity or maternal education moderated associations between neighborhood characteristics and sleep.
Consistent with our hypotheses, we found that lower neighborhood cohesion was associated with increased risk of trouble sleeping. Furthermore, the inverse association between neighborhood cohesion and trouble sleeping was stronger among adolescents who reported lower maternal education (as an indicator of family SES). Findings are consistent with the hypothesis that families with lower SES may have less organized houses, with more noise and less knowledge about sleep hygiene (Jarrin et al., 2014). This home environment, in conjunction with a less socially cohesive neighborhood, may potentiate the risk for poor sleep via increased exposure to stress, including neighborhood-level crime and disruption, lesser parental involvement around sleep-wake routines, lesser parental knowledge of healthy sleep hygiene practices (e.g., removal of technology at bedtime). These findings are consistent with a growing body of literature suggesting the importance of considering neighborhood-level factors in influencing individual’s health behaviors (DeSantis et al., 2016; Diez Roux and Mair, 2010). In contrast with prior work and our hypotheses, however, we did not find evidence of associations between perceived neighborhood safety and monitoring with adolescent sleep problems, duration, or timing. Perhaps the items we included to assess neighborhood-level safety and monitoring were too distal to influence sleep patterns, although they may be relevant for other adolescent risk behaviors, such as alcohol use.
Contrary to expectations, we found that greater objectively measured neighborhood poverty was associated with earlier rather than later bedtimes. Notably, however, there was no statistically significant difference in total sleep time based on neighborhood poverty, suggesting that adolescents from more impoverished neighborhoods were either waking up earlier or having more awakenings in the night, resulting in a net null effect on total sleep time, despite earlier bedtimes. These findings suggest the importance of considering other neighborhood and community influences on sleep, including school start times, and noise levels.
In addition, we found a significant interaction between neighborhood poverty and race/ethnicity on trouble sleeping, such that there was a stronger, positive association between living in more impoverished neighborhoods and risk of trouble sleeping for non-Hispanic Whites as compared to Hispanic or multi-racial/ other ethnic groups. This result should be interpreted with caution, however, given that Hispanic and multi-racial/”other” adolescents were significantly more likely to live in more impoverished neighborhoods than non-Hispanic Whites, and there were fewer non-Hispanic Whites who lived in the most impoverished neighborhoods. Nevertheless, findings are consistent with other work showing that there are stronger effects of neighborhood poverty on health risk behaviors, such as smoking in non-Hispanic white adolescents as compared to blacks (Nowlin and Colder, 2007), perhaps due to racial/ ethnic differences in susceptibility to both proximal (e.g., family) and distal (e.g, community) social influences on health behaviors. These findings emphasize how critical it is to consider both neighborhood and family-level risk factors for adolescent health behaviors.
Findings must be interpreted within the context of study limitations. In particular, given the cross-sectional analysis, causal relationships cannot be inferred. An additional limitation is the reliance on self-reported sleep, which may have introduced bias or common method variance with the self-reported assessments of neighborhood characteristics. Although we used multiple sleep measures, inclusion of both subjective and objective measures of sleep, as well as other important indicators of sleep disturbance (e.g., social jetlag) may provide a more comprehensive understanding of the links between neighborhoods and sleep in adolescence. Our findings are strengthened by inclusion of objectively measured neighborhood poverty via census tract data; however, examination of other objective characteristics of the neighborhood, including crime data, or observations of neighborhood disorder, such as graffiti, vacant lots, or broken windows is needed. Although this study was unique in evaluating neighborhood disadvantage and sleep associations in four distinct racial/ethnic groups, based on the distribution in the sample, the “Other” racial/ethnic group was a heterogeneous group consisting of African Americans, American Indians, Native Hawaiians, and Multi-ethnic respondents.
In summary, understanding both individual/ family-level and neighborhood level risk factors that contribute to adolescent sleep problems is critical to inform novel prevention and intervention efforts that consider the broader socio-environmental impacts on key health behaviors, such as sleep. Future research is needed to extend these findings to consider how sleep disturbances may mediate the effects of neighborhood disadvantage on downstream health consequences. The current study provides an important contribution to the scant literature in this area. Findings also have implications for policies that target both built and social environmental characteristics of neighborhoods as a means to improve population health and reduce pervasive health disparities, including disparities in sleep health.
Implications and Contributions Statement.
Our study is the first to examine both objectively and subjectively measured neighborhood factors in relation to sleep in older adolescents. Findings highlight the importance of considering how neighborhood environments influence sleep health, particularly during critical developmental periods, such as adolescence.
Highlights.
Examines objective and subjective neighborhood factors and sleep in adolescents.
Adolescence is a key period for studying socio-environmental influences on sleep.
Maternal education and race/ethnicity are important moderators.
Acknowledgments
Funding Source:
Work on this article was supported by a grant from the National Institute of Alcohol Abuse and Alcoholism ( R01AA020883) to Elizabeth D’Amico. The authors wish to thank Kirsten Becker and Megan Zander-Cotugno for overseeing the web based surveys.
Abbreviations
- MHI-5
Mental Health Inventory
- NSCH
National Survey of Children’s Health
- PHQ
Patient Health Questionnaire
- SES
socioeconomic status
- TST
total sleep time
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest:
All authors have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bagley EJ, Tu KM, Buckhalt JA, El-Sheikh M. Community violence concerns and adolescent sleep. Sleep Health. 2016;2:57–62. doi: 10.1016/j.sleh.2015.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamini Y, Hochberg Y. Controlling the false discovery rate - a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society Series B-Methodological. 1995;57:289–300. [Google Scholar]
- Berwick DM, Murphy JM, Goldman PA, Ware JE, Jr, Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Medical Care. 1991;29:169–176. doi: 10.1097/00005650-199102000-00008. [DOI] [PubMed] [Google Scholar]
- Brouillette RT, Horwood L, Constantin E, Brown K, Ross NA. Childhood sleep apnea and neighborhood disadvantage. The Journal of Pediatrics. 2011;158:789–795. e781. doi: 10.1016/j.jpeds.2010.10.036. [DOI] [PubMed] [Google Scholar]
- Carskadon MA, Acebo C, Jenni OG. Regulation of adolescent sleep: Implications for behavior. Annals of the New York Academy of Sciences. 2004;1021:276–291. doi: 10.1196/annals.1308.032. [DOI] [PubMed] [Google Scholar]
- Curcio G, Ferrara M, De Gennaro L. Sleep loss, learning capacity and academic performance. Sleep Medicine Reviews. 2006;10:323–337. doi: 10.1016/j.smrv.2005.11.001. [DOI] [PubMed] [Google Scholar]
- D’Amico EJ, Tucker JS, Miles JNV, Zhou AJ, Shih RA, Green HD., Jr Preventing alcohol use with a voluntary after-school program for middle school students: Results from a cluster randomized controlled trial of choice. Prevention Science. 2012;13:415–425. doi: 10.1007/s11121-011-0269-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeSantis A, Troxel WM, Beckman R, Ghosh-Dastidar B, Hunter GP, Hale L, Buysse DJ, Dubowitz T. Is the association between neighborhood characteristics and sleep quality mediated by psychological distress? An analysis of perceived and objective measures of 2 Pittsburgh neighborhoods. Sleep Health. 2016;2:277–282. doi: 10.1016/j.sleh.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux AV, Mair C. Neighborhoods and health. Annals of the New York Academy of Sciences. 2010;1186:125–145. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- Felden ÉPG, Leite CR, Rebelatto CF, Andrade RD, Beltrame TS. Sleep in adolescents of different socioeconomic status: A systematic review. Revista Paulista de Pediatria (English Edition) 2015;33:467–473. doi: 10.1016/j.rpped.2015.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale L, Hill TD, Burdette AM. Does sleep quality mediate the association between neighborhood disorder and self-rated physical health? Preventive Medicine. 2010;51:275–278. doi: 10.1016/j.ypmed.2010.06.017. [DOI] [PubMed] [Google Scholar]
- Hale L, Hill TD, Friedman E, Javier Nieto F, Galvao LW, Engelman CD, Malecki KMC, Peppard PE. Perceived neighborhood quality, sleep quality, and health status: Evidence from the survey of the health of Wisconsin. Social Science & Medicine. 2013;79:16–22. doi: 10.1016/j.socscimed.2012.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasler BP, Clark DB. Circadian misalignment, reward-related brain function, and adolescent alcohol involvement. Alcoholism: Clinical and Experimental Research. 2013;37:558–565. doi: 10.1111/acer.12003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill TD, Burdette AM, Hale L. Neighborhood disorder, sleep quality, and psychological distress: Testing a model of structural amplification. Health & Place. 2009;15:1006–1013. doi: 10.1016/j.healthplace.2009.04.001. [DOI] [PubMed] [Google Scholar]
- Ivanenko A, Crabtree VM, Gozal D. Sleep and depression in children and adolescents. Sleep Medicine Reviews. 2005;9:115–129. doi: 10.1016/j.smrv.2004.09.006. [DOI] [PubMed] [Google Scholar]
- Jarrin DC, McGrath JJ, Quon EC. Objective and subjective socioeconomic gradients exist for sleep in children and adolescents. Health Psychology. 2014;33:301–305. doi: 10.1037/a0032924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Javaheri S, Storfer-Isser A, Rosen CL, Redline S. Association of short and long sleep durations with insulin sensitivity in adolescents. Journal of Pediatrics. 2011;158:617–623. doi: 10.1016/j.jpeds.2010.09.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandel DB, Kiros GE, Schaffran C, Hu MC. Racial/ethnic differences in cigarette smoking initiation and progression to daily smoking: A multilevel analysis. American Journal of Public Health. 2004;94:128–135. doi: 10.2105/ajph.94.1.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Maslowsky J, Hamilton A, Schulenberg J. The great sleep recession: Changes in sleep duration among US adolescents, 1991 2012. Pediatrics. 2015 doi: 10.1542/peds.2014-2707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korupp SE, Ganzeboom HBG, Van der Lippe TV. Do mothers matter? A comparison of models of the influence of mothers’ and fathers’ educational and occupational status on children’s educational attainment. Quality and Quantity. 2002;36:17–42. [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-15: Validity of a new measure for evaluating the severity of somatic symptoms. Psychosomatic Medicine. 2002;64:258–266. doi: 10.1097/00006842-200203000-00008. [DOI] [PubMed] [Google Scholar]
- Larson N, Laska MN, Story M, Neumark-Sztainer D. Sports and energy drink consumption are linked to health-risk behaviours among young adults. Public Health Nutrition. 2015;18:2794–2803. doi: 10.1017/S1368980015000191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews KA, Hall M, Dahl RE. Sleep in healthy black and white adolescents. Pediatrics. 2014;133:E1189–E1196. doi: 10.1542/peds.2013-2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore M, Kirchner HL, Drotar D, Johnson N, Rosen C, Redline S. Correlates of adolescent sleep time and variability in sleep time: The role of individual and health related characteristics. Sleep Medicine. 2011;12:239–245. doi: 10.1016/j.sleep.2010.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health (NIH) NIH policy and guidelines on the inclusion of women and minorities as subjects in clinical research. 2001 http://grants.nih.gov/grants/funding/women_min/guidelines_amended_10_2001.htm.
- National Sleep Foundation. Adolescent sleep needs and patterns. 2000 http://sleepfoundation.org/sites/default/files/sleep_and_teens_report1.pdf.
- Nowlin PR, Colder CR. The role of ethnicity and neighborhood poverty on the relationship between parenting and adolescent cigarette use. Nicotine & Tobacco Research. 2007;9:545–556. doi: 10.1080/14622200701239613. [DOI] [PubMed] [Google Scholar]
- Office of Disease Prevention and Health Promotion (ODPHP) Adolescent health. 2016 https://www.healthypeople.gov/2020/topics-objectives/topic/Adolescent-Health.
- Panel on High-Risk Youth, Commission on Behavioral and Social Sciences and Education, National Research Council. Losing generations: Adolescents in high-risk settings. National Academy Press; Washington, DC: 1993. [Google Scholar]
- Pasch KE, Laska MN, Lytle LA, Moe SG. Adolescent sleep, risk behaviors, and depressive symptoms: Are they linked? American Journal of Health Behavior. 2010;34:237–248. doi: 10.5993/ajhb.34.2.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pattillo M. Black middle-class neighborhoods. Annual Review of Sociology. 2005;31:305–329. [Google Scholar]
- Powell NB, Schechtman KB, Riley RW, Li K, Troell R, Guilleminault C. The road to danger: The comparative risks of driving while sleepy. Laryngoscope. 2001;111:887–893. doi: 10.1097/00005537-200105000-00024. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Roberts CR, Chan W. Ethnic differences in symptoms of insomnia among adolescents. Sleep. 2006;29:359–365. doi: 10.1093/sleep/29.3.359. [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Schultz DJ, Reynolds KA, Sontag-Padilla LM, Lovejoy SL, Firth R, Pincus HA. Transforming systems for families at-risk for parental depression and early childhood developmental delays: Findings and lessons learned from the helping families raise healthy children initiative. RAND Corporation; Santa Monica, CA: 2013. p. RR122. http://www.rand.org/pubs/research_reports/RR122.html. [Google Scholar]
- Singh GK, Kenney MK. Rising prevalence and neighborhood, social, and behavioral determinants of sleep problems in US children and adolescents, 2003–2012. Sleep Disorders. 2013;2013:15. doi: 10.1155/2013/394320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smaldone A, Honig JC, Byrne MW. Sleepless in America: Inadequate sleep and relationships to health and well-being of our nation’s children. Pediatrics. 2007;119:S29–S37. doi: 10.1542/peds.2006-2089F. [DOI] [PubMed] [Google Scholar]
- Troxel WM, Lee L, Hall M, Matthews KA. Single-parent family structure and sleep problems in black and white adolescents. Sleep Medicine. 2014;15:255–261. doi: 10.1016/j.sleep.2013.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umlauf MG, Bolland AC, Bolland KA, Tomek S, Bolland JM. The effects of age, gender, hopelessness, and exposure to violence on sleep disorder symptoms and daytime sleepiness among adolescents in impoverished neighborhoods. Journal of Youth and Adolescence. 2014;44:518–542. doi: 10.1007/s10964-014-0160-5. [DOI] [PubMed] [Google Scholar]
- Winstanley EL, Steinwachs DM, Ensminger ME, Latkin CA, Stitzer ML, Olsen Y. The association of self-reported neighborhood disorganization and social capital with adolescent alcohol and drug use, dependence, and access to treatment. Drug and Alcohol Dependence. 2008;92:173–182. doi: 10.1016/j.drugalcdep.2007.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson AR, Carskadon MA, Acebo C, Seifer R, Fallone G, Labyak SE, Martin JL. Evidence for the validity of a sleep habits survey for adolescents. Sleep. 2003;26:213–216. doi: 10.1093/sleep/26.2.213. [DOI] [PubMed] [Google Scholar]
- Wong MM, Robertson GC, Dyson RB. Prospective relationship between poor sleep and substance-related problems in a national sample of adolescents. Alcoholism: Clinical and Experimental Research. 2015;39:355–362. doi: 10.1111/acer.12618. [DOI] [PMC free article] [PubMed] [Google Scholar]