Abstract
Background & Aims
The incidence and prevalence of inflammatory bowel diseases (IBD) continue to increase worldwide. We sought to update incidence rates of Crohn's disease (CD) and ulcerative colitis (UC) in a well-defined United States (US) population, calculating values for Olmsted County, Minnesota through 2010. We also calculated prevalence values.
Methods
The resources of the Rochester Epidemiology Project were used to identify county residents who were diagnosed with IBD (CD or UC), based on previously set criteria. Those with new diagnoses of CD or UC between 1970 and 2010 were identified as incidence cases, and those meeting diagnostic criteria on January 1, 2011 were identified as prevalence cases. Incidence rates were estimated (adjusted for age and sex to the US white population in 2010). Trends in incidence based on age at diagnosis, sex, and year of diagnosis were evaluated by Poisson regression.
Results
The incidence cohort included 410 CD patients (51% female) and 483 individuals with UC (56% male). Median age of diagnosis was 29.5 years for persons with CD (range, 4–93 years) and 34.9 years for UC (range, 1–91 years). From 2000 through 2010, the adjusted annual incidence rate for CD was 10.7 cases per 100,000 person-years (95% CI, 9.1–12.3 person-years) and for UC was 12.2 per 100,000 (95% CI, 10.5–14.0 person-years). On January 1, 2011, there were 380 residents with CD, with an adjusted prevalence of 246.7 cases per 100,000 persons (95% CI, 221.7–271.8 cases per 100,000 persons), and 435 residents with UC, with an adjusted prevalence of 286.3 (95% CI, 259.1–313.5 cases per 100,000 persons). Male sex was significantly associated with a higher incidence rate of UC, and younger age was significantly associated with a higher incidence rate of CD.
Conclusion
Estimated incidence rates for UC and CD in Olmsted County are among the highest in the US. Extrapolating the adjusted prevalence to the most recent US Census, there could be approximately 1.6 million persons in the US with IBD.
Keywords: Crohn's disease, ulcerative colitis, epidemiology, incidence, prevalence
INTRODUCTION
The incidence and prevalence of inflammatory bowel disease (IBD) continues to change world-wide, and rates of IBD have increased with time(1). While the highest reported rates are in North America, the United Kingdom, Northern Europe, and Australia, higher incidence rates are being reported in developing countries as these regions become more industrialized(1). The cause for this trend in unknown; however, environmental factors such as sanitation, diet, or microbial exposure have been hypothesized to be involved(1-3).
Population-based studies, which allow for complete case ascertainment and follow-up data, are important in studying these trends. A population-based cohort of Olmsted County, Minnesota (MN) residents with CD and UC has been studied since 1935(4-10). Between 1935 and 1975, there was a significant increase in UC incidence(4), and rates stabilized thereafter through 2000(8, 9). Higher UC incidence rates have been significantly associated with male gender and younger age group(9). Similarly, age- and sex-adjusted incidence rates of CD increased after 1940 and peaked in the 1964-73 time period(7). These rates continued to increase through 2000(9).
The descriptive epidemiology of the Olmsted County population-based cohort of IBD patients was last updated through 2000(9). Between 1940 and 2000, the age- and sex-adjusted annual incidence rates for CD and UC were reported at 8.8 cases per 100,000 person-years and 7.9 cases per 100,000, respectively(9). The prevalence of UC was noted to have decreased by 7% and the prevalence of CD increased by 31% between 1991 and 2000(9). This study aims to update the incidence and prevalence of CD and UC through 2011 in this population-based cohort of IBD patients. Further study of this cohort of patients may help elucidate the cause for changing epidemiologic trends given the distinct patient population that can easily be studied.
METHODS
Rochester Epidemiology Project
The Rochester Epidemiology Project (REP) is a unique medical records linkage system developed in the 1950s and supported by the National Institutes of Health. It exploits the fact that virtually all of the health care for the residents of Olmsted County is provided by two organizations: Mayo Medical Center, consisting of Mayo Clinic and its two affiliated hospitals (Rochester Methodist and Saint Marys), and Olmsted Medical Center, consisting of a smaller multispecialty clinic and its affiliated hospital (Olmsted Community Hospital). In any four-year period, over 95% of county residents are examined at either one of the two health care systems(11-13). Diagnoses generated from all outpatients visits, emergency room visits, hospitalizations, nursing home visits, surgical procedures, autopsy examinations, and death certificates are recorded in a central diagnostic index. Thus, it is possible to identify virtually all diagnosed cases of a given disease for which patients sought medical attention.
Case Ascertainment
The resources of the REP were used to identify all residents of Olmsted County who were diagnosed with either CD or UC from 1970 through 2010. Previously used definitions for CD and UC diagnoses were employed in this study(7-9). Cases of UC were diagnosed based on finding the following criteria on two occasions separated by at least six months: 1) diffusely granular or friable colonic mucosa on endoscopy; and 2) continuous mucosal involvement based on endoscopy or barium studies(9). CD cases were identified based on at least two of the following criteria found on two occasions, separated by at least two months: 1) history of abdominal pain, diarrhea, weight loss, malaise, and/or rectal bleeding; 2) endoscopic findings of linear ulceration, mucosal cobblestoning, skip areas, or perianal disease; 3) radiologic findings of fistula, stricture, mucosal cobblestoning, or ulceration; 4) laparotomy appearance of “creeping fat,” bowel wall induration, and mesenteric lymphadenopathy; or 5) histologic findings of transmural inflammation and/or epithelioid granulomas(9).
Medical records of previously identified cases of CD and UC (1970-2000) were reviewed to ensure that diagnoses were accurate. The following data were recorded: baseline demographic data including date of birth and sex, date of CD or UC diagnosis, and county residence status at: date of diagnosis; January 1, 2011; and date of last follow-up.
Statistical Analysis
Incidence rates for CD and UC were obtained by dividing the number of people diagnosed with CD or UC by the total population at risk. Rates were age- and sex- adjusted to the 2010 United States census for Caucasians(14). County residents who met diagnostic criteria on the preset date of January 1, 2011 were identified as prevalence cases, and this was estimated similarly to the incidence rates. Poisson regression analysis was used to determine if incidence rates were significantly associated with age, sex, or year of diagnosis. The adjusted prevalence of CD and UC in Olmsted County were used to extrapolate the number of US residents with CD and UC using the 2010 United States census.
RESULTS
A total of 893 patients with IBD were identified during the 1970-2010 period; there were 410 patients with CD and 483 patients with UC (Table 1). The median age at diagnosis of CD was 29.5 years (range, 3.8-93.1 years) and that of UC was 34.9 (1.2-94.1). Two hundred nine CD patients were female (51%), whereas 272 UC patients were male (56%). The diagnosis of CD and UC was most common in the 20 to 29 year-old age group.
Table 1.
Baseline characteristics of 893 residents of Olmsted County, Minnesota diagnosed with Crohn's disease (CD) and ulcerative colitis (UC) between 1970 and 2010.
| Characteristic | CD, N | UC, N | Total, N |
|---|---|---|---|
| Total | 410 | 483 | 893 |
| Sex | |||
| Male | 201 | 272 | 473 |
| Female | 209 | 211 | 420 |
| Age at Diagnosis (Median) | 29.5 | 34.9 | 32.7 |
Incidence
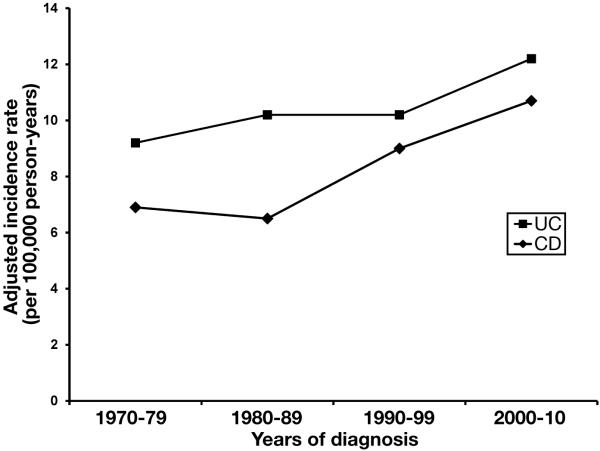
The overall age- and sex-adjusted incidence rates for CD and UC were 8.7 and 10.7 per 100,000 person-years, respectively, for the entire 1970-2010 period. The adjusted incidence rates for CD and UC in 2000-10 were 10.7 and 12.2 per 100,000 person-years, respectively (Figure 1). Age-specific rates for both CD and UC were estimated (Table 2). Adjusted rates by decade were estimated for CD and UC (Table 3).
Figure 1.
Age- and sex-adjusted incidence rate of Crohn's disease (CD) and ulcerative colitis (UC) in a population-based cohort of Olmsted County patients between 1970 and 2010.
Table 2.
Age-specific incidence rate (cases per 100,000 person-years) of Crohn's disease and ulcerative colitis by gender in Olmsted County, Minnesota (1970-2010).
| Crohn's disease | ||||||
|---|---|---|---|---|---|---|
| Age | Female (N) | Female (Incidence) | Male (N) | Male (Incidence) | Total (N) | Total (Incidence) |
| 1-19 | 38 | 5.6 | 51 | 7.3 | 89 | 6.5 |
| 20-29 | 68 | 17.7 | 52 | 15.3 | 120 | 16.6 |
| 30-39 | 28 | 7.7 | 37 | 10.2 | 65 | 8.9 |
| 40-49 | 29 | 9.4 | 20 | 6.6 | 49 | 8.0 |
| 50-59 | 22 | 9.2 | 22 | 9.6 | 44 | 9.4 |
| 60-69 | 6 | 3.6 | 12 | 8.2 | 18 | 5.8 |
| 70-93 | 18 | 8.7 | 7 | 5.5 | 25 | 7.5 |
| Total | 209 | 8.9 | 201 | 9.1 | 410 | 9.0 |
| Ulcerative colitis | ||||||
|---|---|---|---|---|---|---|
| Age | Female (N) | Female (Incidence) | Male (N) | Male (Incidence) | Total (N) | Total (Incidence) |
| 1-19 | 25 | 3.7 | 30 | 4.3 | 55 | 4.0 |
| 20-29 | 63 | 16.4 | 72 | 21.3 | 135 | 18.7 |
| 30-39 | 43 | 11.8 | 56 | 15.4 | 99 | 13.6 |
| 40-49 | 38 | 12.3 | 49 | 16.2 | 87 | 14.2 |
| 50-59 | 15 | 6.3 | 27 | 11.8 | 42 | 8.9 |
| 60-69 | 13 | 7.8 | 18 | 12.4 | 31 | 9.9 |
| 70-93 | 14 | 6.8 | 20 | 15.7 | 34 | 10.2 |
| Total | 211 | 8.9 | 272 | 12.3 | 483 | 10.6 |
Table 3.
Age- and sex-adjusted incidence rate (cases per 100,000 person-years) for Crohn's disease and ulcerative colitis by decade in Olmsted County, Minnesota between 1970 and 2010.
| Crohn's disease | ||||||
|---|---|---|---|---|---|---|
| Decade | Female (N) | Female (Incidence) | Male (N) | Male (Incidence) | Total (N) | Total (95% Confidence Interval) |
| 1970-1979 | 41 | 8.2 | 26 | 5.7 | 67 | 6.9 (5.1-8.8) |
| 1980-1989 | 35 | 5.8 | 37 | 7.3 | 72 | 6.5 (4.9-8.1) |
| 1990-1999 | 46 | 8.2 | 50 | 9.9 | 96 | 9.0 (7.1-10.9) |
| 2000-2010 | 87 | 10.6 | 88 | 10.8 | 175 | 10.7 (9.1-12.3) |
| 1970-2010 | 209 | 8.6 | 201 | 8.9 | 410 | 8.8 (7.9-9.7) |
| Ulcerative colitis | ||||||
|---|---|---|---|---|---|---|
| Decade | Female (N) | Female (Incidence) | Male (N) | Male (Incidence) | Total (N) | Total (95% Confidence Interval) |
| 1970-1979 | 39 | 8.1 | 40 | 10.3 | 79 | 9.2 (7.0-11.4) |
| 1980-1989 | 32 | 6.0 | 63 | 14.6 | 95 | 10.2 (8.0-12.5) |
| 1990-1999 | 52 | 8.7 | 62 | 11.8 | 114 | 10.2 (8.2-12.2) |
| 2000-2010 | 88 | 10.7 | 107 | 14.0 | 195 | 12.2 (10.5-13.9) |
| 1970-2010 | 211 | 8.8 | 272 | 12.8 | 483 | 10.7 (9.7-11.7) |
Crohn's Disease
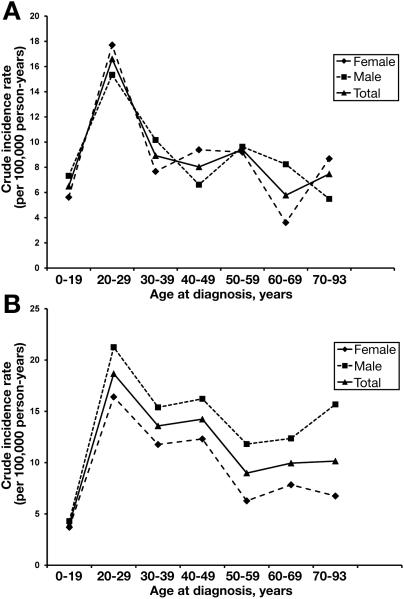
The age- and sex-adjusted incidence rates for CD increased during the study period of 1970 through 2010. Younger age (p<0.001) and a later calendar year of diagnosis (p=0.003) were significantly associated with a higher incidence of CD in Poisson regression analysis. The 20 to 29 year-old age group had the highest crude incidence rate of CD (16.6 cases per 100,000 person-years), while the 1-19 year-old age group had the lowest (6.5 per 100,000) (Table 2). Overall incidence rates for CD were similar in men and women, and incidence rates for both groups sharply decreased after the age of 29 years (Figure 2A). About two-thirds of cases of CD were diagnosed under the age of 40 years. In the Poisson regression, sex was not significantly associated with higher incidence rates of CD (p=0.93). The age-adjusted incidence rate for females was 8.6 per 100,000 person-years and that of males was 8.9 per 100,000 person-years.
Figure 2.
A) Incidence of Crohn's disease (CD) by age group in Olmsted County, MN among 410 CD patients between 1970 and 2010. B) Incidence of ulcerative colitis (UC) by age group in Olmsted County, MN among 483 UC patients between 1970 and 2010.
Ulcerative Colitis
The age- and sex-adjusted incidence rates for UC tended to increase during the 1970-2010 study period. In the Poisson regression analysis, sex was associated with higher incidence rates of UC (p<0.001), with men having consistently higher incidence rates than women across all age groups (Figure 2B). The age-adjusted UC incidence rate for males was 12.8 cases per 100,000 person-years and that for women was 8.8 per 100,000. Neither age (p=0.35) nor calendar year of diagnosis (0=0.06) were associated with a higher incidence of UC in the Poisson analysis. The highest crude incidence rate of UC was observed in the 20 to 29 year-old age group (18.7 cases per 100,000 person-years) while the lowest rate was seen in the 1-19 age group (4.0 per 100,000) (Table 2).
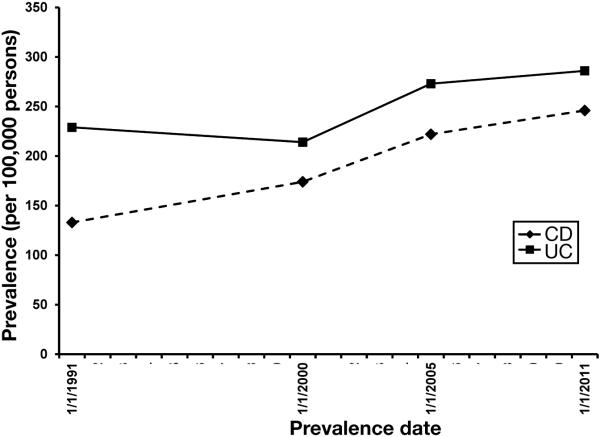
Prevalence
There were a total of 380 county residents with CD and 435 with UC on January 1, 2011. Therefore, the age- and sex-adjusted prevalence for CD and UC were 246.7 cases per 100,000 persons and 286.3 per 100,000 persons, respectively. The prevalence for CD and UC in 2001 had been 174 and 214 cases per 100,000 persons, respectively(9). Thus, the prevalence of CD has increased by 41% and that of UC by 33% during the intervening ten years (Figure 3).
Figure 3.
Age- and sex-adjusted prevalence of Crohn's disease (CD) and ulcerative colitis (UC) in Olmsted County between 1970-2011.
DISCUSSION
This study of the descriptive epidemiology of CD and UC in a population-based cohort of Olmsted County, MN patients between 1970 and 2010 showed an increase in CD and UC incidence and prevalence. Whereas the incidence of CD was 8.8 cases per 100,000 person-years and that of UC was 7.9 per 100,000 in 1990-2000, the rates increased to 10.7 per 100,000 and 12.2 per 100,000 for CD and UC, respectively, in the 2000-10 study period (Figure 1). We found that younger age and later calendar years of diagnosis were significantly associated with CD incidence; however, only male gender was associated with a higher incidence rate of UC. The age- and sex-adjusted prevalence of CD was 246.7 cases per 100,000 persons and that of UC was 286.2 per 100,000 on January 1, 2011.
When compared to January 1, 2000 (214 cases per 100,000 persons)(9), the prevalence was 34% higher for UC in 2011 (Figure 2). In comparison, there was a 41% increase in CD prevalence between 2001 (174 cases per 100,000) and 2011(9). When we had previously compared the prevalence of UC and CD between 1991 and 2001, there had been a 31% increase in CD prevalence and minimal change in UC prevalence(9). The increasing prevalence of CD and UC may well be due in part to patients living longer with the disease, as they usually are diagnosed at a younger age, and have a normal or near-normal life expectancy on average. This concept of “compounding prevalence” has been previously noted (15).
Multiple studies have assessed the epidemiological trends of CD and UC in various countries (16-21). Canadian population-based studies have reported some of the highest rates of IBD world-wide (18, 22, 23). In Ontario, Benchimol et al found an increase in the incidence and prevalence of CD and UC between 1998 and 2008, with a particularly significant increase in the pediatric population (i.e., age <18 years) (22). During this time period, the incidence rate of CD increased from 9.6 to 12.1 cases per 100,000 person-years, and that of UC increased from 10.7 to 12.1 per 100,000 (22). The most recent incidence rate for UC in Olmsted County during 2000-2010 was comparable to that of Ontario, whereas the CD incidence rate in Olmsted County was slightly lower.
There were a few differences between the study by Benchimol and colleagues and ours. Benchimol and coworkers had a larger sample size, and they used administrative data such as ICD-9 codes, billing claims, and medication prescription data (22). Their means of identifying IBD patients by these methods were validated. The validation algorithm for children with IBD had a sensitivity of 89.6%-91.1% and a specificity of 99.5-99.9%, and the algorithm for adults with IBD had lower sensitivity (76.8% to 92.3%) and specificity (96.2%-99.1%) (22). On the other hand, our study was a population-based cohort in which the medical records of each potential IBD case was manually reviewed for predetermined diagnostic criteria, rather than relying on administrative data.
A pediatric population-based study from Iceland examined the incidence of CD and UC in children younger than 16 years(16). Between 1951 and 2000, the incidence rate of CD increased from 0.2 cases per 100,000 person-years to 2.3 per 100,000, and the rate of UC increased from 1.1 per 100,000 to 2.4 per 100,000(16). In the 2001-10 study period, the incidence rates declined slightly to 2.3 cases per 100,000 person-years for CD and 2.4 per 100,000 for UC(16). In comparison, among those younger than 19 years of age in Olmsted County, the overall 1970-2010 incidence of CD was 6.4 cases per 100,000 person-years and that of UC was 4.0 per 100,000. The cause for the higher incidences of CD and UC at younger ages in Olmsted County is unclear; one might speculate that environmental factors may play a role, but these apparent differences may also be due to different age cutoffs.
In contrast to other studies that have shown increasing incidence rates for CD and UC, a population-based study from the Canadian maritime province of Nova Scotia showed a decrease in CD and UC incidence between 1996 and 2009 (23). Age-adjusted incidence rates for CD and UC decreased from 27.4 cases per 100,000 person-years to 17.7 per 100,000, and from 21 per 100,000 to 16.7 per 100,000, respectively, during the study period (23). Similar to the study by Benchimol and coworkers, diagnoses of IBD were made based on a validated database scoring system—administrate data such as ICD-9 codes taken together with physician billing claims and, if hospitalized, discharge diagnoses (23,24). The reason for the declining incidence in Nova Scotia is unclear. However, the number of diagnoses may have been underestimated if patients were not hospitalized or seeking healthcare, such as in the case of mild disease as noted by the authors.
Globally, however, 75% of CD studies and 60% of UC studies have shown a statistically significant increase in incidence (1). Our study is in keeping with this global trend(1). Although western nations have the highest incidence of CD and UC, previously low incidence regions such as Asia have recently had increasing rates of CD and UC (19, 25,26).
The reasons for increasing incidence of CD and UC are relatively unknown. It has been noted that those who emigrate from a low prevalence area to a higher prevalence region are at increased risk of developing IBD, thereby suggesting an environmental etiology (1). IBD is more prevalent in urban regions compared to rural areas, and in industrial nations compared to developing regions (1). These data suggest that changes in diet, lifestyle, and sanitation, among others, may be the particular environmental causes (3,27). However, further investigation must be undertaken to fully elucidate this.
The increased incidence of CD and UC leads to an increased economic burden with higher healthcare utilization. Since many patients are diagnosed with IBD at a young age, this leads to lifelong medical treatment and loss of productivity at work. It is estimated that days of work lost and disability amounts to about 50% of the cost (28). Not only is the higher healthcare burden caused by medications, procedures, and hospitalizations, but this may also be due to an aging population of IBD patients who are living longer with the disease as evidenced by the “compounding prevalence” of the disease (15).
The strength of this study is that all case ascertainment was based on clinical diagnoses and medical record review rather than on administrative data. All available patient data were reviewed due to the linked diagnostic index. Since greater than 95% of Olmsted County residents receive their health care at either Mayo Medical Center or Olmsted Medical Center, we were able to capture essentially all patients with a diagnosis of either CD and UC (29).
Conversely, there are a few limitations of this study, similar to those that have been discussed in previous studies of this cohort (9). There may be limited follow-up in some cases, especially in those instances when patients moved out of the county. The population of Olmsted County is relatively small (21, 22). Finally, the population of Olmsted County is not as diverse racially and ethnically as much of the U.S.; for example, as of the 2010 U.S. census, about 83.4% of Olmsted County residents were non-Hispanic Caucasian. Given the fairly homogenous population, generalizability of these data may not be possible in populations with disparate racial makeup.
In summary, the incidence rates of CD and UC in Olmsted County, MN continued to rise over the past decade. The combined prevalence of CD and UC in Olmsted County in 2011 was over 530 cases per 100,000. Stated another way, about 1 in 200 Olmsted County residents in 2011 had IBD. Finally, extrapolating the adjusted prevalence to the current US census, there are approximately 785,000 U.S. residents with CD and 910,000 with UC, for a total of about 1.6 million U.S. residents with IBD. However, these figures should be considered a rough approximation of the true number of CD and UC cases in the US, as our adjusted prevalence was based on the 2010 US Caucasian population. Future aims include using this updated cohort as a basis for studying the etiology of these trends.
Acknowledgement
The authors are grateful to Lawrence Timmons and Debra Jewell for data abstraction. Supported in part by the Mayo Foundation for Medical Education & Research, and made possible by: 1) CTSA grant number UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health; and 2) the Rochester Epidemiology Project (Grant number R01 AG034676 from the National Institute on Aging). The contents of the publication are solely the responsibility of the authors and do not necessarily represent the official view of the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: Doctors Shivashankar and Tremaine and Mr. Harmsen have no conflicts of interest to disclose. Doctor Loftus has consulted for UCB Pharma, Takeda, Janssen, AbbVie, Amgen, Seres Therapeutics, Sun Pharma, Eli Lilly, Mesoblast, and Bristol-Myers Squibb, and has received research support from UCB Pharma, Takeda, Janssen, AbbVie, Amgen, Pfizer, Robarts Clinical Trials, Celgene, Receptos, Gilead, and Seres Therapeutics.
Author Roles:
Study concept and design: Shivashankar, Loftus
Acquisition of data: Shivashankar, Harmsen
Analysis and interpretation of data: Harmsen, Shivashankar, Loftus
Drafting of the manuscript: Shivashankar
Critical revision of the manuscript for important intellectual content: Loftus, Tremaine, Harmsen
Funding: Loftus
Study supervision: Loftus
REFERENCES
- 1.Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2011;142:46. doi: 10.1053/j.gastro.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 2.Loftus EV., Jr. Clinical epidemiology of inflammatory bowel disease: Incidence, prevalence, and environmental influences. Gastroenterology. 2004;126:1504–17. doi: 10.1053/j.gastro.2004.01.063. [DOI] [PubMed] [Google Scholar]
- 3.Bernstein CN. Assessing environmental risk factors affecting the inflammatory bowel diseases: a joint workshop of the Crohn's & Colitis Foundations of Canada and the USA. Inflammatory bowel diseases. 2008 doi: 10.1002/ibd.20494. [DOI] [PubMed] [Google Scholar]
- 4.Sedlack RE, Nobrega FT, Kurland LT, et al. Inflammatory colon disease in Rochester, Minnesota, 1935-1964. Gastroenterology. 1972;62:935–941. [PubMed] [Google Scholar]
- 5.Sedlack RE, Whisnant J, Elveback LR, et al. Incidence of Crohn's disease in Olmsted County, Minnesota, 1935-1975. American journal of epidemiology. 1980;112:759–763. doi: 10.1093/oxfordjournals.aje.a113048. [DOI] [PubMed] [Google Scholar]
- 6.Gollop JH, Phillips SF, Melton LJ, et al. Epidemiologic aspects of Crohn's disease: a population based study in Olmsted County, Minnesota, 1943-1982. Gut. 1987;29:49–56. doi: 10.1136/gut.29.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Loftus EV, Silverstein MD, Sandborn WJ, et al. Crohn's disease in Olmsted County, Minnesota, 1940-1993: incidence, prevalence, and survival. Gastroenterology. 1998;114:1161–1168. doi: 10.1016/s0016-5085(98)70421-4. [DOI] [PubMed] [Google Scholar]
- 8.Loftus EV, Silverstein MD, Sandborn WJ, et al. Ulcerative colitis in Olmsted County, Minnesota, 1940-1993: incidence, prevalence, and survival. Gut. 2000;46:336–343. doi: 10.1136/gut.46.3.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Loftus CG, Loftus EV, Jr., Harmsen WS, et al. Update on the incidence and prevalence of Crohn's disease and ulcerative colitis in Olmsted County, Minnesota, 1940-2000. Inflamm Bowel Dis. 2007;13:254–61. doi: 10.1002/ibd.20029. [DOI] [PubMed] [Google Scholar]
- 10.Stonnington CM, Phillips SF, Melton LJ, et al. Chronic ulcerative colitis: incidence and prevalence in a community. Gut. 1987;28:402–409. doi: 10.1136/gut.28.4.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.St Sauver JL, Grossardt BR, Leibson CL, et al. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87:151–60. doi: 10.1016/j.mayocp.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.St Sauver JL, Grossardt BR, Yawn BP, et al. Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol. 2012;41:1614–24. doi: 10.1093/ije/dys195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rocca WA, Yawn BP, St Sauver JL, et al. History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012;87:1202–13. doi: 10.1016/j.mayocp.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.US Census Bureau [March 15, 2016];Quick Facts. 2010 http://quickfacts.census.gov/qfd/states/27/27109.html.
- 15.Kaplan GG. The global burden of IBD: from 2015 to 2025. Nature reviews Gastroenterology & Hepatology. 2015;12:720–727. doi: 10.1038/nrgastro.2015.150. [DOI] [PubMed] [Google Scholar]
- 16.Agnarsson U, Björnsson S, Jóhansson JH, et al. Inflammatory bowel disease in Icelandic children 1951-2010. Population-based study involving one nation over six decades. Scandinavian journal of gastroenterology. 2013;48:1399–1404. doi: 10.3109/00365521.2013.845799. [DOI] [PubMed] [Google Scholar]
- 17.Lucendo AJ, Hervías D, Roncero Ó , et al. Epidemiology and temporal trends (2000-2012) of inflammatory bowel disease in adult patients in a central region of Spain. European journal of gastroenterology & hepatology. 2014;26:1399–1407. doi: 10.1097/MEG.0000000000000226. [DOI] [PubMed] [Google Scholar]
- 18.Bitton A, Vutcovici M, Patenaude V, et al. Decline in IBD incidence in Québec: part of the changing epidemiologic pattern in North America. Inflammatory bowel diseases. 2014;20:1782–1783. doi: 10.1097/MIB.0000000000000167. [DOI] [PubMed] [Google Scholar]
- 19.Kim HJ, Hann HJ, Hong SN, et al. Incidence and Natural Course of Inflammatory Bowel Disease in Korea, 2006-2012: A Nationwide Population-based Study. Inflammatory bowel diseases. 2015;21:623–630. doi: 10.1097/MIB.0000000000000313. [DOI] [PubMed] [Google Scholar]
- 20.Adamiak T, Walkiewicz-Jedrzejczak D, Fish D, et al. Incidence, clinical characteristics, and natural history of pediatric IBD in Wisconsin: a population-based epidemiological study. Inflammatory bowel diseases. 2013;19:1218–1223. doi: 10.1097/MIB.0b013e318280b13e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wilson J, Hair C, Knight R, et al. High incidence of inflammatory bowel disease in Australia: A prospective population based Australian incidence study. Inflammatory bowel diseases. 2010;16:1550–1556. doi: 10.1002/ibd.21209. [DOI] [PubMed] [Google Scholar]
- 22.Benchimol EI, Manuel DG, Guttmann A, et al. Changing age demographics of inflammatory bowel disease in Ontario, Canada: a population-based cohort study of epidemiology trends. Inflammatory bowel diseases. 2014;20:1761–1769. doi: 10.1097/MIB.0000000000000103. [DOI] [PubMed] [Google Scholar]
- 23.Leddin D, Tamim H, Levy AR. Decreasing incidence of inflammatory bowel disease in Eastern Canada: a population database study. BMC gastroenterology. 2013;14:140. doi: 10.1186/1471-230X-14-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rezaie A, Quan H, Fedorak RN, et al. Development and validation of an administrative case definition for inflammatory bowel diseases. Canadian journal of gastroenterology = Journal canadien de gastroenterologie. 2012;26:711–717. doi: 10.1155/2012/278495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ng SC. Epidemiology of inflammatory bowel disease: focus on Asia. Best practice & research. Clinical gastroenterology. 2014;28:363–372. doi: 10.1016/j.bpg.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 26.Zheng J, Zhu X, Huangfu Z, et al. Crohn's disease in mainland China: a systematic analysis of 50 years of research. Chinese journal of digestive diseases. 2005;6:175–181. doi: 10.1111/j.1443-9573.2005.00227.x. [DOI] [PubMed] [Google Scholar]
- 27.Shanahan F, Bernstein CN. The evolving epidemiology of inflammatory bowel disease. Current opinion in gastroenterology. 2009;25:301–305. doi: 10.1097/MOG.0b013e32832b12ef. [DOI] [PubMed] [Google Scholar]
- 28.van der Valk ME, Mangen MJ, Leenders M, et al. Healthcare costs of inflammatory bowel disease have shifted from hospitalisation and surgery towards anti-TNFalpha therapy: results from the COIN study. Gut. 2014;63:72–79. doi: 10.1136/gutjnl-2012-303376. [DOI] [PubMed] [Google Scholar]
- 29.St Sauver JL, Grossardt BR, Yawn BP, et al. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester epidemiology project. American journal of epidemiology. 2011;173:1059–1068. doi: 10.1093/aje/kwq482. [DOI] [PMC free article] [PubMed] [Google Scholar]