Abstract
Obesity is the largest driver of chronic preventable diseases, accounting for an estimated $147 billion or 10 percent of total US healthcare costs in 2008. It has been forecasted that 42 percent of Americans will be obese by 2030. Mobile health (mHealth) technologies target and may modify the behavioral factors that lead to obesity to promote a healthy lifestyle. These technologies could potentially reduce the cost and the morbidity and mortality burden of obesity because of their inexpensive and portable nature. This study aimed to analyze the efficacy and cost-effectiveness of mHealth interventions for adult obesity in the United States. The methodology used in this study was a literature review of 54 articles. Weight, body mass index (BMI), waist circumference reductions, and favorable lifestyle behavior changes were noted across most studies. Existing data and research on efficacy and linked costs indicated that mHealth technologies were more effective than other methods and could be inexpensively delivered remotely to manage adult obesity, offering significant benefits over conventional care. Further studies on the costs and benefits of adapting such mHealth interventions in clinical settings are needed.
Keywords: adult, obesity, mHealth interventions, cost, efficacy
Introduction
Obesity—declared an epidemic in 1999—is the single greatest public health threat in the United States.1 In 2015, adult obesity rates exceeded 35 percent four states—Alabama, Louisiana, Mississippi, and West Virginia. Moreover, the rates were above 20 percent in other states, including: Georgia, Kentucky, Illinois, Oregon, Pennsylvania, and Texas.2 If current trends continue, the national obesity rate has been projected to climb from 35.7 percent in 2012 to 42 percent by 2030.3
Obesity increases the risk of serious comorbidities such as diabetes mellitus, cardiovascular diseases, and endometrial cancer, thereby resulting in high morbidity, mortality, and healthcare costs.4, 5, 6 In 2008, these obesity-linked healthcare costs were an estimated $147 billion, constituting 10 percent of the national medical budget.7 In 2011, a study using a simulation model predicted that healthcare expenses due to obesity-related preventable diseases in the United States will rise by $48–66 billion per year by 2030.8
Lifestyle modifications consisting of behavioral interventions such as diet monitoring, exercise program, and counseling have resulted in clinically significant weight loss in obese people.9 However, long-term adherence to these modifications has often been quite expensive, time consuming, and challenging.10
Mobile health (mHealth) has been defined by the World Health Organization as medical and public health practice supported by mobile devices, such as mobile phones, patient monitoring devices, personal digital assistants, and other wireless devices.11 It can be categorized into six categories: education, clinical decision support, remote data collection and analysis, health promotion and awareness, remote monitoring, and integrated care and diagnostic support.12
Utilization of mHealth has surged because of its portable, accessible, and cost-effective nature.13, 14, 15 For instance, short message services (SMS) is a popular, low-cost, and simple way to deliver health information.16 Likewise, smartphones have gained popularity and are being adopted for the prevention and control of obesity because they offer multiple functionalities.17 Different types of mobile applications have already been developed for general use in obesity management, utilizing features such as movement sensors, microphones and cameras.18, 19 For example, smartphone software could utilize motion sensors and GPS to create maps of exercise routes and provide users with real-time feedback regarding movement speed, step counts, energy expenditure, and the completion of exercise goals. In addition, diet cameras could recognize foods and calculate the calorie content of a meal automatically from images or videos, requiring limited human input.20, 21
Thus, mobile technology has proffered an exciting opportunity to remotely deliver obesity interventions.22 This opportunity raises the question as to whether such interventions are truly better—more effective and cheaper—compared with conventional practices, making it crucial to assess their effectiveness and costs. Therefore, the purpose of this study was to identify mobile interventions currently directed toward adult obesity in the United States and to evaluate their efficacy and related costs.
Methodology
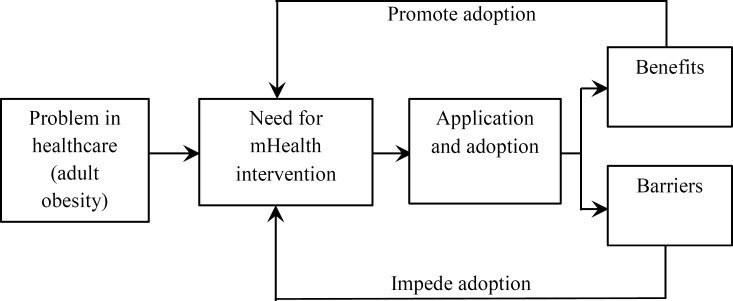
The conceptual framework for this research conformed to the steps and research framework used by Yao, Chu, and Li (2010).23 The framework elucidates the course of mHealth adoption for management of the adult obesity epidemic. If the process of mHealth programs’ leading to improved care access for obese adults while diminishing parallel healthcare expenses is to be investigated, their effectiveness and corresponding costs must first be pinpointed. Akin to the cyclic progression of any project, the process of technology adoption begins when problems in the existing system necessitate assessment of needs, which subsequently results in the creation and institution of a solution. The solution here is the application of mHealth interventions. The process involves an evaluation of the benefits of and barriers to mHealth utilization after it is adopted, and the evaluation is repeated to assess the benefits and barriers related to the technology (see Figure 1). This conceptual framework is suitable for the present study because it centers on means of application of new technology in healthcare settings. Moreover, the internal validity of this approach is supported by its successful replication in past studies.24, 25, 26
Figure 1.
Research Framework
Source: Adapted from Yao, W., C. H. Chu, and Z. Li. “The Use of RFID in Healthcare: Benefits and Barriers.” Proceedings of the 2010 IEEE International Conference on RFID Technology and Applications (RFID-TA) (2010): 128–34.
The hypothesis of this study was that mHealth interventions would demonstrate greater efficacy with minimal expense in preventing and controlling obesity when compared with standard care.
A systematic search methodology was used in this literature review. For the intent of this research question, a comprehensive and exhaustive systematic review or meta-analysis was not feasible because of the abundance of studies of heterogeneous quality. The literature review was conducted in three distinct stages:
determining the search strategy, and identifying and collecting literature;
establishing inclusion criteria, scrutinizing text for relevancy, and analyzing the literature data; and
identifying appropriate categories.
Step 1: Literature Identification and Collection
The electronic databases PubMed, EBSCOhost, ProQuest, Academic Search Premier, and Google Scholar were searched for the following terms: “mobile health interventions” or “mobile health apps” or “smart phone apps” and “obesity” and “Adults and “weight loss” or “physical activity” or “exercise” or “sedentary behavior” and “efficacy” or “cost-effectiveness” or “economic evaluation.” The International Journal of Medical Informatics, International Journal of Obesity, International Journal of Research in Medical Sciences, and other reliable healthcare websites, including those of the National Institutes of Health and the World Health Organization, were also used. Citations and abstracts identified in the search were also assessed to identify relevant articles.
Step 2: Establishment of Inclusion Criteria and Literature Analysis
As the utilization of mobile technology within healthcare increases, it is important to assess the effectiveness and value for the cost of the various mobile devices. Consequently, the literature was selected to include the efficacy and cost-effectiveness of the mobile health interventions for obesity. In an attempt to stay current in the research study, the search was limited to sources published since 2006. The search was also limited to sources attainable as full texts and to studies written in the English language and conducted in the United States.
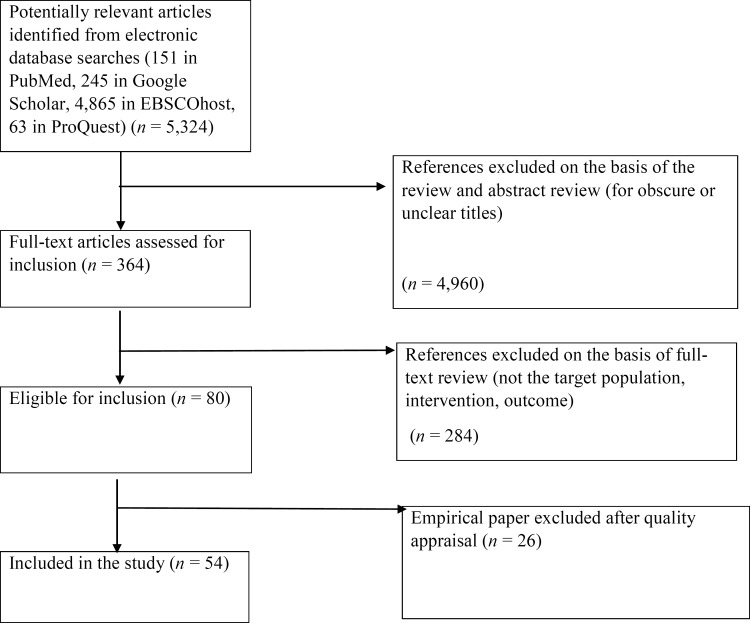
The methodology and results of the identified texts were analyzed, and key papers were identified and included within the research query. References were reviewed and determined to have satisfied the inclusion criteria if the material provided accurate information about physical activity, BMI, waist circumference, lifestyle behavior, and cost-effectiveness. From a total of 80 references found, 54 references were selected for this research study. A summary of the selection criteria and process is displayed in Figure 2. The literature search was conducted by B.W., K.G., and N.B. and was validated by A.C., who acted as a second reader and also double-checked that the references met the research study's inclusion criteria. D.P. reviewed the manuscript and revised it for clarity and consistency.
Figure 2.
Flow Diagram for Selection of Studies on mHealth Interventions for Adult Obesity in the United States, 2006–2016
Step 3: Literature Categorization
The results were sorted into the following categories: study characteristics, effect on body weight, effect on waist circumference and BMI, effect on lifestyle behavior (change in dietary intake and change in physical activity), effect on adherence and satisfaction, and cost efficacy.
Results
A summary of studies that examined the effects of mobile apps on various aspects of obesity appears below. Table 1 describes characteristics of the studies that were examined, Table 2 lists the distribution of participants by gender and race for included studies, and Table 3 summarizes the effects of each study on the output parameters of the studies. The mHealth interventions included in the studies broadly utilized the following avenues to deliver the intervention: health information delivery, such as education or motivation (n = 17); reminders (n = 6); communication platform for patients to communicate with healthcare providers (n = 3); self-monitoring, such as patients’ recording of their diet or exercise trends (n = 12); peer or group support (n = 7); and remote monitoring, in which patient data are collected through remote peripheral monitoring devices (n = 10). Some studies were multifaceted and involved more than one of these types of intervention.
Table 1.
Mobile Interventions for Obesity: Study Characteristics
| Authors (Year) | Design | Theoretical Models | Sample Size | Participants | Trial length | Intervention/Control | Technological Components |
|---|---|---|---|---|---|---|---|
| Fukuoka et al. (2010) | SGPP | NM | 41 | Sedentary women, mean age 48.4 | 3 weeks | Mobile apps | SM, feedback, goal setting |
| Archer et al. (2012) | RCT | NM | 197 | GP, 18–65 years | 9 months | a. GWL b. GWL + SWA c. SWA d. Standard Care | SM |
| Rabin et al. (2011) | DD | NM | 15 | GP, mean age 38.9 years | 1 week/app | Mobile apps | NM |
| Turner et al. (2011) | RCT | SCT | 96 | GP, 18–60 years, BMI 25–45 | 6 months | a. Podcast b. Podcast + mobile | SM |
| Burke et al. (2012) | RCT | SCT | 210 | GP, ≤59 years, BMI 27–43 | 24 months | a. PDA + feedback b. PDA c. Paper diary | SM, CFC, SP |
| Allen et al. (2013) | RCT | SCT | 68 | GP, 21–65 years, BMI 28–42 | 6 months | a. Intensive counseling b. Intensive counseling + smartphone c. Less-intensive counseling + smartphone d. Smartphone | SM, CFC, SP |
| Kim et al. (2013) | RCT | NM | 45 | Older African American adults, mean age 69.3 | 6 weeks | a. SMS + pedometer + manual b. Pedometer + manual | SM |
| King et al. (2013) | RCT | SCT; Social influence theory; Operant conditioning principles | 68 | GP, mean age 59.1 | 7 weeks | a. App + feedback b. App + group communication c. App + positive reinforcement | SM, problem solving, goal setting |
| Napolita | RCT | SCT | 52 | Students, 18– | 8 weeks | a. Facebook + | SM, goal |
| no et al. (2013) | 29 years, BMI 25–50 | SMS + personalized feedback b. Facebook c. Wait-list control | setting, CFC, ITP | ||||
| Norman et al. (2013) | RCT | SCT, control theory, operant conditioning | 65 | GP, 25–55 years, BMI ≥25.0–39.9 | 4 months | a. SMS b. Usual care | SM |
| Shapiro et al. (2012) | RCT | SCT | 128 | GP, 21–65 years, BMI 25–39.9 | 12 months | a. SMS + MMS b. Monthly e-newsletters | SM, stimulus control tips, goal setting, problem solving |
| Spring et al. (2013) | RCT | NM | 69 | GP, mean age 57.7 | 6 months | a. Mobile b. Standard care | SM |
| Steinberg et al. (2013) | RCT | Self-regulation theory | 91 | GP, 18–60 years, BMI 25–40 | 6 months | a. SMS + usual care b. Usual care | SM, goal setting |
| Thomas et al. (2013) | Pilot study | Self-regulation theory | 20 | GP, 18–70 years, BMI 25–50 | 12–24 weeks | Mobile app | SM, feedback |
| Bond et al. (2014) | Experimental | NM | 30 | GP, 21–70 years, BMI ≥25 | 4 weeks | App-prompted physical activity breaks + feedback + SWA arm band | SM, goal setting, feedback |
| Laing et al. (2014) | RCT | NM | 212 | PCP | 6 months | a. Mobile app b. Usual care | SM, goal setting, feedback |
| Cowdery et al. (2015) | RCT | Self-determination theory | 40 | GP, 18–69 | 12 weeks | a. Mobile apps + PA tracker b. PA tracker | goal setting, monitoring |
| Gilliland et al. (2015) | Quasi-experimental | Behavioral economic theory | 208 | GP, 18% BMI >30 | 8–10 weeks | SMS + up-front surveys + phone interviews + follow-up surveys + Google analytics data | SM, ITP |
| Svetkey et al. (2015) | RCT | SCT and TTM | 365 | GP, 18–35 years, BMI ≥25 | 24 months | a. Interactive cell phone app b. Personal coaching + self-monitoring c. Control | SM, feedback |
| Sze et al. (2015) | Pilot study | TAM | 20 | Parents (90% female), age 44.1 (SD 7.8) years; BMI 34.2 (SD, 6.8) | 4 weeks | a. MAMRT + NI + EFT b. MAMRT + NI | SM, feedback, SP, ITP |
| Willey et al. (2016) | Quasi-experimental | NM | 10 | Females, 30–50 years, BMI 26.6–34 | 12 weeks | Mobile app | SM, feedback, SP, ITP |
Abbreviations: BMI, body mass index; CFC, counselor feedback and communication; DD, Descriptive Design; EFT, Episodic Future Thinking; GP, general population; GWL, group weight-loss education; ITP, individual tailored program; MAMRT, Mobile Audio Manager and Response Tracker;; MMS, Multimedia Messaging Service; NI, nutrition information; NM, not mentioned; PCP, primary care patient; RCT, randomized controlled trial; SCT, social cognitive theory; SGPP, single group pre- and post-intervention; SM, self-monitoring; SP, smartphone; SWA: Sense Wear Armband; TAM, technology acceptance model; TTM, transtheoretical model.
- Allen, Jerilyn K., Janna Stephens, Cheryl R. Dennison Himmelfarb, Kerry J. Stewart, and Sara Hauck. “Randomized Controlled Pilot Study Testing Use of Smartphone Technology for Obesity Treatment.” Journal of Obesity 2013 (2013): 151597.
- Archer, Edward, Erik J. Groessl, Xuemei Sui, Amanda C. McClain, Sara Wilcox, Gregory A. Hand, Rebecca A. Meriwether, and Steven N. Blair. “An Economic Analysis of Traditional and Technology-based Approaches to Weight Loss.” American Journal of Preventive Medicine 43, no. 2 (2012): 176–82.
- Bond, Dale S., J. Graham Thomas, Hollie A. Raynor, Jon Moon, Jared Sieling, Jennifer Trautvetter, Tiffany Leblond, and Rena R. Wing. “B-MOBILE: A Smartphone-based Intervention to Reduce Sedentary Time in Overweight/Obese Individuals: A Within-Subjects Experimental Trial.” PLoS One 9, no. 6 (2014): e100821.
- Burke, Lora E., Mindi A. Styn, Susan M. Sereika, Molly B. Conroy, Lei Ye, Karen Glanz, Mary Ann Sevick, and Linda J. Ewing. “Using mHealth Technology to Enhance Self-Monitoring for Weight Loss: A Randomized Trial.” American Journal of Preventive Medicine 43, no. 1 (2012): 20–26.
- Cowdery, Joan, Paul Majeske, Rebecca Frank, and Devin Brown. “Exergame Apps and Physical Activity: The Results of the ZOMBIE Trial.” American Journal of Health Education 46, no. 4 (2015): 216–22.
- Fukuoka, Yoshimi, Eric Vittinghoff, So Son Jong, and William Haskell. “Innovation to Motivation—Pilot Study of a Mobile Phone Intervention to Increase Physical Activity Among Sedentary Women.” Preventive Medicine 51, no. 3 (2010): 287–89.
- Gilliland, Jason, Richard Sadler, Andrew Clark, Colleen O'Connor, Malgorzata Milczarek, and Sean Doherty. “Using a Smartphone Application to Promote Healthy Dietary Behaviors and Local Food Consumption.” BioMed Research International 2015 (2015): 1–11.
- Kim, Bang Hyun, and Karen Glanz. “Text Messaging to Motivate Walking in Older African Americans: A Randomized Controlled Trial.” American Journal of Preventive Medicine 44, no. 1 (2013): 71–75.
- King, Abby C., Eric B. Hekler, Lauren A. Grieco, Sandra J. Winter, Jylana L. Sheats, Matthew P. Buman, Banny Banerjee, Thomas N. Robinson, and Jesse Cirimele. “Harnessing Different Motivational Frames Via Mobile Phones to Promote Daily Physical Activity and Reduce Sedentary Behavior in Aging Adults.” PloS One 8, no. 4 (2013): e62613.
- Laing, Brian Yoshio, Carol M. Mangione, Chi-Hong Tseng, Mei Leng, Ekaterina Vaisberg, Megha Mahida,
- Michelle Bholat, Eve Glazier, Donald E. Morisky, and Douglas S. Bell. “Effectiveness of a Smartphone Application for Weight Loss Compared with Usual Care in Overweight Primary Care Patients: A Randomized, Controlled Trial.” Annals of Internal Medicine 161, no. 10, suppl. (2014): S5–S12.
- Napolitano, Melissa A., Sharon Hayes, Gary G. Bennett, Allison K. Ives, and Gary D. Foster. “Using Facebook and Text Messaging to Deliver a Weight Loss Program to College Students.” Obesity 21, no. 1 (2013): 25–31.
- Norman, Gregory J., Julia K. Kolodziejczyk, Marc A. Adams, Kevin Patrick, and Simon J. Marshall. “Fruit and Vegetable Intake and Eating Behaviors Mediate the Effect of a Randomized Text-Message Based Weight Loss Program.” Preventive Medicine 56, no. 1 (2013): 3–7.
- Rabin, Carolyn, and Beth Bock. “Desired Features of Smartphone Applications Promoting Physical Activity.” Telemedicine and e-Health 17, no. 10 (2011): 801–3.
- Shapiro, Jennifer R., Tina Koro, Neal Doran, Sheri Thompson, James F. Sallis, Karen Calfas, and Kevin Patrick. “Text4Diet: A Randomized Controlled Study Using Text Messaging for Weight Loss Behaviors.” Preventive Medicine 55, no. 5 (2012): 412–17.
- Spring, Bonnie, Jennifer M. Duncan, E. Amy Janke, Andrea T. Kozak, H. Gene McFadden, Andrew DeMott, Alex Pictor, et al. “Integrating Technology into Standard Weight Loss Treatment: A Randomized Controlled Trial.” JAMA Internal Medicine 173, no. 2 (2013): 105–11.
- Steinberg, Dori M., Deborah F. Tate, Gary G. Bennett, Susan Ennett, Carmen Samuel Hodge, and Dianne S. Ward. “The Efficacy of a Daily Self-Weighing Weight Loss Intervention Using Smart Scales and E-mail.” Obesity 21, no. 9 (2013): 1789–97.
- Svetkey, Laura P., Bryan C. Batch, Pao-Hwa Lin, Stephen S. Intille, Leonor Corsino, Crystal C. Tyson, Hayden B. Bosworth, et al. “Cell Phone Intervention for You (CITY): A Randomized, Controlled Trial of Behavioral Weight Loss Intervention for Young Adults Using Mobile Technology.” Obesity 23, no. 11 (2015): 2133–41.
- Sze, Yan Yan, Tinuke Oluyomi Daniel, Colleen K. Kilanowski, R. Lorraine Collins, and Leonard H. Epstein. “Web-Based and Mobile Delivery of an Episodic Future Thinking Intervention for Overweight and Obese Families: A Feasibility Study.” JMIR mHealth and uHealth 3, no. 4 (2015): e97.
- Thomas, J. Graham, and Rena R. Wing. “Health-e-call, a Smartphone-assisted Behavioral Obesity Treatment: Pilot Study.” JMIR mHealth and uHealth 1, no. 1 (2013): e3.
- Turner-McGrievy, Gabrielle, and Deborah Tate. “Tweets, Apps, and Pods: Results of the 6-Month Mobile Pounds Off Digitally (Mobile POD) Randomized Weight-Loss Intervention among Adults.” Journal of Medical Internet Research 13, no. 4 (2011): e120.
- Willey, Steven, and James K. Walsh. “Outcomes of a Mobile Health Coaching Platform: 12-Week Results of a Single-Arm Longitudinal Study.” JMIR mHealth and uHealth 4, no. 1 (2016): e3.
Table 2.
Distribution of the Participants in the Included Studies by Gender and Race
| Authors (Year) | Participant Characteristics |
|||
|---|---|---|---|---|
| Gender | Percentage | Race/Ethnicity | Percentage | |
| Fukuoka et al. (2010) | F | 100% | Minority | 59% |
| Rabin et al. (2011) | GP | NR | ||
| Turner et al. (2011) | F | 48% | Non-Hispanic White | 75% |
| Non-Hispanic Black | 19% | |||
| Other | 6% | |||
| Archer et al. (2012) | F | 81.7% | NR | |
| Burke et al. (2012) | F | 84.8% | Non-Hispanic White | 78.1% |
| Allen et al. (2013) | F | 78% | Non-Hispanic Black | 49% |
| Kim et al. (2013) | F | 80.4% | Non-Hispanic Black | |
| King et al. (2013) | F | 73.5% | Non-Hispanic White, | 69% |
| Hispanic/Latino | 13% | |||
| Asian | 12% | |||
| Napolitano et al. (2013) | F | 86.5% | Non-Hispanic White | 57.7% |
| Non-Hispanic Black | 30.8% | |||
| Hispanic | 5.8% | |||
| Asian | 1.9% | |||
| Biracial/Multiracial | 1.9% | |||
| Other | 1.9% | |||
| Norman et al. (2013) | F | 80% | Non-Hispanic White | 75% |
| Shapiro et al. (2012) | F | 65% | Non-Hispanic White | 64% |
| Spring et al. (2013) | M | 85.5% | Non-Hispanic White | 75.4% |
| Non-Hispanic Black | 24.6% | |||
| Steinberg et al. (2013) | F | 75% | Non-Hispanic White | 74% |
| Thomas et al. (2013) | F | 95% | Non-Hispanic White | 85% |
| Non-Hispanic Black | 5% | |||
| American Indian | 5% | |||
| Bond et al. (2014) | F | 83.3% | Non-Hispanic White | 66.7% |
| Non-Hispanic Black, | 13.3% | |||
| American Indian, | 3.3% | |||
| Asian | 3.3% | |||
| Other | 13.3% | |||
| Laing et al. (2014) | F | 73% | Hispanic or Latino | 33% |
| Non-Hispanic White | 48% | |||
| Non-Hispanic Black | 19% | |||
| Asian | 8% | |||
| Native American/Pacific Islander | 2% | |||
| Cowdery et al. (2015) | F | 85% | Non-Hispanic White | 85% |
| Gilliland et al. (2015) | F | 66% | NR | |
| Svetkey et al. (2015) | F | 69.6% | Non-Hispanic White | 56.2% |
| Non-Hispanic Black | 36.2% | |||
| Other | 7.7% | |||
| Sze et al. (2015) | F | 90% | Non-Hispanic White | 90% |
| Other | 10% | |||
| Willey et al. (2016) | F | 100% | Non-Hispanic White | |
Abbreviations: F, female; M, male; GP, general population; NR, not reported.
- Allen, Jerilyn K., Janna Stephens, Cheryl R. Dennison Himmelfarb, Kerry J. Stewart, and Sara Hauck. “Randomized Controlled Pilot Study Testing Use of Smartphone Technology for Obesity Treatment.” Journal of Obesity 2013 (2013): 151597.
- Archer, Edward, Erik J. Groessl, Xuemei Sui, Amanda C. McClain, Sara Wilcox, Gregory A. Hand, Rebecca A. Meriwether, and Steven N. Blair. “An Economic Analysis of Traditional and Technology-based Approaches to Weight Loss.” American Journal of Preventive Medicine 43, no. 2 (2012): 176–82.
- Bond, Dale S., J. Graham Thomas, Hollie A. Raynor, Jon Moon, Jared Sieling, Jennifer Trautvetter, Tiffany Leblond, and Rena R. Wing. “B-MOBILE: A Smartphone-based Intervention to Reduce Sedentary Time in Overweight/Obese Individuals: A Within-Subjects Experimental Trial.” PLoS One 9, no. 6 (2014): e100821.
- Burke, Lora E., Mindi A. Styn, Susan M. Sereika, Molly B. Conroy, Lei Ye, Karen Glanz, Mary Ann Sevick, and Linda J. Ewing. “Using mHealth Technology to Enhance Self-Monitoring for Weight Loss: A Randomized Trial.” American Journal of Preventive Medicine 43, no. 1 (2012): 20–26.
- Cowdery, Joan, Paul Majeske, Rebecca Frank, and Devin Brown. “Exergame Apps and Physical Activity: The Results of the ZOMBIE Trial.” American Journal of Health Education 46, no. 4 (2015): 216–22.
- Fukuoka, Yoshimi, Eric Vittinghoff, So Son Jong, and William Haskell. “Innovation to Motivation—Pilot Study of a Mobile Phone Intervention to Increase Physical Activity Among Sedentary Women.” Preventive Medicine 51, no. 3 (2010): 287–89.
- Gilliland, Jason, Richard Sadler, Andrew Clark, Colleen O'Connor, Malgorzata Milczarek, and Sean Doherty. “Using a Smartphone Application to Promote Healthy Dietary Behaviors and Local Food Consumption.” BioMed Research International 2015 (2015): 1–11.
- Kim, Bang Hyun, and Karen Glanz. “Text Messaging to Motivate Walking in Older African Americans: A Randomized Controlled Trial.” American Journal of Preventive Medicine 44, no. 1 (2013): 71–75.
- King, Abby C., Eric B. Hekler, Lauren A. Grieco, Sandra J. Winter, Jylana L. Sheats, Matthew P. Buman, Banny Banerjee, Thomas N. Robinson, and Jesse Cirimele. “Harnessing Different Motivational Frames Via Mobile Phones to Promote Daily Physical Activity and Reduce Sedentary Behavior in Aging Adults.” PloS One 8, no. 4 (2013): e62613.
- Laing, Brian Yoshio, Carol M. Mangione, Chi-Hong Tseng, Mei Leng, Ekaterina Vaisberg, Megha Mahida, Michelle Bholat, Eve Glazier, Donald E. Morisky, and Douglas S. Bell. “Effectiveness of a Smartphone Application for Weight Loss Compared with Usual Care in Overweight Primary Care Patients: A Randomized, Controlled Trial.” Annals of Internal Medicine 161, no. 10, suppl. (2014): S5–S12.
- Napolitano, Melissa A., Sharon Hayes, Gary G. Bennett, Allison K. Ives, and Gary D. Foster. “Using Facebook and Text Messaging to Deliver a Weight Loss Program to College Students.” Obesity 21, no. 1 (2013): 25–31.
- Norman, Gregory J., Julia K. Kolodziejczyk, Marc A. Adams, Kevin Patrick, and Simon J. Marshall. “Fruit and Vegetable Intake and Eating Behaviors Mediate the Effect of a Randomized Text-Message Based Weight Loss Program.” Preventive Medicine 56, no. 1 (2013): 3–7.
- Rabin, Carolyn, and Beth Bock. “Desired Features of Smartphone Applications Promoting Physical Activity.” Telemedicine and e-Health 17, no. 10 (2011): 801–3.
- Shapiro, Jennifer R., Tina Koro, Neal Doran, Sheri Thompson, James F. Sallis, Karen Calfas, and Kevin Patrick. “Text4Diet: A Randomized Controlled Study Using Text Messaging for Weight Loss Behaviors.” Preventive Medicine 55, no. 5 (2012): 412–17.
- Spring, Bonnie, Jennifer M. Duncan, E. Amy Janke, Andrea T. Kozak, H. Gene McFadden, Andrew DeMott, Alex Pictor, et al. “Integrating Technology into Standard Weight Loss Treatment: A Randomized Controlled Trial.” JAMA Internal Medicine 173, no. 2 (2013): 105–11.
- Steinberg, Dori M., Deborah F. Tate, Gary G. Bennett, Susan Ennett, Carmen Samuel Hodge, and Dianne S. Ward. “The Efficacy of a Daily Self-Weighing Weight Loss Intervention Using Smart Scales and E-mail.” Obesity 21, no. 9 (2013): 1789–97.
- Svetkey, Laura P., Bryan C. Batch, Pao-Hwa Lin, Stephen S. Intille, Leonor Corsino, Crystal C. Tyson, Hayden B. Bosworth, et al. “Cell Phone Intervention for You (CITY): A Randomized, Controlled Trial of Behavioral Weight Loss Intervention for Young Adults Using Mobile Technology.” Obesity 23, no. 11 (2015): 2133–41.
- Sze, Yan Yan, Tinuke Oluyomi Daniel, Colleen K. Kilanowski, R. Lorraine Collins, and Leonard H. Epstein. “Web-Based and Mobile Delivery of an Episodic Future Thinking Intervention for Overweight and Obese Families: A Feasibility Study.” JMIR mHealth and uHealth 3, no. 4 (2015): e97.
- Thomas, J. Graham, and Rena R. Wing. “Health-e-call, a Smartphone-assisted Behavioral Obesity Treatment: Pilot Study.” JMIR mHealth and uHealth 1, no. 1 (2013): e3.
- Turner-McGrievy, Gabrielle, and Deborah Tate. “Tweets, Apps, and Pods: Results of the 6-Month Mobile Pounds Off Digitally (Mobile POD) Randomized Weight-Loss Intervention among Adults.” Journal of Medical Internet Research 13, no. 4 (2011): e120.
- Willey, Steven, and James K. Walsh. “Outcomes of a Mobile Health Coaching Platform: 12-Week Results of a Single-Arm Longitudinal Study.” JMIR mHealth and uHealth 4, no. 1 (2016): e3.
Table 3.
Effect of Mobile Health Interventions on Different Study Parameters
| Authors (Year) | Study Parameters | |||||
|---|---|---|---|---|---|---|
| Body Weight (kg) | BMI (kg/m2) | Waist Circumference (cm) | Physical Activity Behavior | Dietary Behavior | Effects on Adherence/Satisfaction | |
| Fukuoka et al. (2010) | NE | NE | NE | Daily total steps increased by 800 or 15% over three weeks, SS | NE | Self-reported willpower improvements associated with step count increases |
| Archer et al. (2012) | NE | NE | NE | NE | NE | Participants found all three apps easy to use, somewhat helpful with an above average level of satisfaction |
| Rabin et al. (2011) | IG: 2.7%, CG: 2.7%, NS | IG: 0.91, CG: 0.26, SS | NE | Exercise self-monitoring rates (days/week), SS: IG: 2.6, CG: 1.2) Intentional physical activity (kcal/day), SS: IG: 196.4, CG: 100.9 | Decrease in daily calorie intake (kcal/day), NS: IG: 288.8, CG: 242.5 Self-reported diet (days/week): No differences | IG: App use to monitor diet 3.5 times more likely, more downloads per episode. CG: Majority used the website or paper. |
| Turner et al. (2011) | GWL and SWA: 6.59, SWA: 3.55, GWL: 1.86, CG: none; SS | NE | NE | NE | NE | NE |
| Burke et al. (2012) | PDA feedback: 2.32%, SS; PDA: 1.38%; CG: | NE | PDA feedback: 6.4%, PDA: 5%, CG: 4%, SS | NE | NE | IG: Greater weight loss in participants who were adherent >60% of the time |
| 1.94%; group differences NS | ||||||
| Allen et al. (2013) | IG: 2.3, CG: 0.63, NS | NE | NE | NE | IG: Positive effects on fruit and vegetable intake and eating behavior inventory scores | Response to messages: All (first week), two of three texts (by week 16) |
| Kim et al. (2013) | IG: 1.65 (1.8%), CG: 1.03 (0.8%), NS | NE | NE | IG: Steps increased to 3,000 steps/day, SS | NE | Text-messaging adherence moderately strong (60%–69%). Greater weight loss in adherent participants. |
| King et al. (2013) | IC + SP: 5.4, LIC + SP: 3.3, SS | IC: 0.8, IC + SP: 1.8, LIC + SP: 1.1, SP: 0.7, SS | IC: 3.0 (M), 3.19 (F); IC + SP: 7.01 (M), 5.68 (F); LIC + SP: 6.5 (M), 3.64 (F); SP: 3.38 (M), 0.88 (F), SS | Self-reported physical activity of moderate or greater intensity (hours/week) decreased in all groups (IC: −1.4, IC + SP: −2.0, LIC + SP: −3.6) except for slight increase in SP group (0.19) | Decrease in daily calorie intake (kcal/day), SS: IC: 415.6, IC +SP : 468.2, LIC + SP: 218.5, SP: 249.2 Increase in fruit and vegetable servings/day, NS: IC: 0.81, IC + SP: 0.51, LIC + SP: 2.1, SP: −0.05 | Adherence highest in IC + SP group: Counseling attendance: 72% App diet logging: 53% App physical activity logging: 32% Similar percentages for LIC + SP group |
| Napolitano et al. (2013) | NE | NE | NE | Increase in daily steps: IG: 679; CG: 398 Changes in MET: IG: 11.96; CG: 4.55 | NE | NE |
| Norman et al. (2013) | NE | NE | NE | Increases in brisk walking for all groups (IG 1: 71.1, IG 2: 122.9, | NE | Participants continued to use the applications for 211.0 days (IG 1), 199.3 days (IG 2), and 162.0 days (IG 3) after the study period |
| IG 3: 105.7) and MVPA for all groups (IG 1: 179.2, IG 2: 257.1, IG 3: 134.3), SS | ||||||
| Shapiro et al. (2012) | Facebook Plus: 2.4, Facebook: 0.63 CG: 0.24, SS | NE | NE | Differences within or among the groups: NS | Differences within or among the groups: NS | 97% found the program helpful and 100% would recommend the program |
| Spring et al. (2013) | IG: 2.9, CG: 0.02 (gain), SS | NE | NE | NE | NE | Adherent participants in the IG lost more weight than adherent or nonadherent participants in the control group |
| Steinberg et al. (2013) | IG: 7.7 (6.55%), CG: 1.5 (0.35%), SS | IG: 0.47, CG: 0.42, NS | NE | NE | IG participants self-weighed more days/week and consumed fewer calories/day than CG participants Daily caloric intake (kcal/day), SS: IG:1,509, CG:1,856 | IG: daily self-weighing was perceived positively |
| Thomas et al. (2013) | IG: 10.9 kg, no CG, SS | NE | NE | NE | NE | Adherence to self-monitoring: 85% All extended program participants gave the maximum rating for satisfaction and would recommend the program |
| Bond et al. (2014) | NE | NE | NE | SED decrease, SS, 3-min: 5.9%, 6-min: 5.6%, 12-min: 3.3% LPA increase, | NE | App use increased motivation to take PA breaks and reduced SED |
| SS, 3-min: 3.9%, 6-min: 3.9%, 12-min: 1.9% MVPA increase, SS, 3-min: 2.0%, 6-min: 1.7%, 12-min:1.3% | ||||||
| Laing et al. (2014) | IG: 0.30, CG: 0.27, NS | NE | NE | Self-reported exercise behaviors: difference NS | IG used “personal calorie goal” more often than CG did (group difference: 2.0 days/week) | Frequency of logins (mean total logins: 61) decreased rapidly after enrolment. No association between baseline characteristics and extent of app use or weight change. |
| Cowdery et al. (2015) | NE | IG:0.09 21, CG: 0.1879 (gain), NS | NE | Decrease in total MET (min/wk), NS: IG: 356.8 CG: 722 | NE | NE |
| Gilliland et al. (2015) | NE | NE | NE | NE | 80% benefited Greater participation associated with increased healthy eating. No influence on consumption behavior. | NE |
| Svetkey et al. (2015) | CP: 0.99, PC: 2.45, CG:1.44, NS | NE | NE | NE | NE | Self-weighing frequency(times/wk): CP: 4.0 (0–6 months), 2.1 (13–24 months) PC: 2.2 (0–6 months), 1.0 (13–24 months) All monthly calls completed: >90% (0–6 months), >87% (13–24 months) |
| Sze et al. (2015) | % overweigh | IG: 1.0, CG: | NE | NE | Decrease in calorie intake | IG: 87%, CG: 92.9% |
| t: IG: 4.6, CG: 1.1, SS | 0.2, SS | (kcal/day), SS: IG: 791.2, CG: 482.4 | ||||
| Willey et al. (2016) | IG: 6.13 (7.3%), no CG, SS | NE | IG: 7.2 (6.6%), no CG, SS | NE | NE | More app use associated with greater improvement in each health outcome but results were NS |
Abbreviations: BW, body weight; BMI, body mass index; CG, control group; CP, cell phone; F, female; GWL, group weight-loss education group; IC, intensive counseling; IG, intervention group; LIC, less-intense counseling; LPA, low-intensity physical activity; M, male; MVPA: moderate to vigorous intensity physical activity; NE: not evaluated; NS, nonsignificant; PA, physical activity; PC, personal coaching; SED: excessive sedentary time; SP, smartphone; SS, statistically significant; SWA: Sense Wear Armband.
- Allen, Jerilyn K., Janna Stephens, Cheryl R. Dennison Himmelfarb, Kerry J. Stewart, and Sara Hauck. “Randomized Controlled Pilot Study Testing Use of Smartphone Technology for Obesity Treatment.” Journal of Obesity 2013 (2013): 151597.
- Archer, Edward, Erik J. Groessl, Xuemei Sui, Amanda C. McClain, Sara Wilcox, Gregory A. Hand, Rebecca A. Meriwether, and Steven N. Blair. “An Economic Analysis of Traditional and Technology-based Approaches to Weight Loss.” American Journal of Preventive Medicine 43, no. 2 (2012): 176–82.
- Bond, Dale S., J. Graham Thomas, Hollie A. Raynor, Jon Moon, Jared Sieling, Jennifer Trautvetter, Tiffany Leblond, and Rena R. Wing. “B-MOBILE: A Smartphone-based Intervention to Reduce Sedentary Time in Overweight/Obese Individuals: A Within-Subjects Experimental Trial.” PLoS One 9, no. 6 (2014): e100821.
- Burke, Lora E., Mindi A. Styn, Susan M. Sereika, Molly B. Conroy, Lei Ye, Karen Glanz, Mary Ann Sevick, and Linda J. Ewing. “Using mHealth Technology to Enhance Self-Monitoring for Weight Loss: A Randomized Trial.” American Journal of Preventive Medicine 43, no. 1 (2012): 20–26.
- Cowdery, Joan, Paul Majeske, Rebecca Frank, and Devin Brown. “Exergame Apps and Physical Activity: The Results of the ZOMBIE Trial.” American Journal of Health Education 46, no. 4 (2015): 216–22.
- Fukuoka, Yoshimi, Eric Vittinghoff, So Son Jong, and William Haskell. “Innovation to Motivation—Pilot Study of a Mobile Phone Intervention to Increase Physical Activity Among Sedentary Women.” Preventive Medicine 51, no. 3 (2010): 287–89.
- Gilliland, Jason, Richard Sadler, Andrew Clark, Colleen O'Connor, Malgorzata Milczarek, and Sean Doherty. “Using a Smartphone Application to Promote Healthy Dietary Behaviors and Local Food Consumption.” BioMed Research International 2015 (2015): 1–11.
- Kim, Bang Hyun, and Karen Glanz. “Text Messaging to Motivate Walking in Older African Americans: A Randomized Controlled Trial.” American Journal of Preventive Medicine 44, no. 1 (2013): 71–75.
- King, Abby C., Eric B. Hekler, Lauren A. Grieco, Sandra J. Winter, Jylana L. Sheats, Matthew P. Buman, Banny Banerjee, Thomas N. Robinson, and Jesse Cirimele. “Harnessing Different Motivational Frames Via Mobile Phones to Promote Daily Physical Activity and Reduce Sedentary Behavior in Aging Adults.” PloS One 8, no. 4 (2013): e62613.
- Laing, Brian Yoshio, Carol M. Mangione, Chi-Hong Tseng, Mei Leng, Ekaterina Vaisberg, Megha Mahida, Michelle Bholat, Eve Glazier, Donald E. Morisky, and Douglas S. Bell. “Effectiveness of a Smartphone Application for Weight Loss Compared with Usual Care in Overweight Primary Care Patients: A Randomized, Controlled Trial.” Annals of Internal Medicine 161, no. 10, suppl. (2014): S5–S12.
- Napolitano, Melissa A., Sharon Hayes, Gary G. Bennett, Allison K. Ives, and Gary D. Foster. “Using Facebook and Text Messaging to Deliver a Weight Loss Program to College Students.” Obesity 21, no. 1 (2013): 25–31.
- Norman, Gregory J., Julia K. Kolodziejczyk, Marc A. Adams, Kevin Patrick, and Simon J. Marshall. “Fruit and Vegetable Intake and Eating Behaviors Mediate the Effect of a Randomized Text-Message Based Weight Loss Program.” Preventive Medicine 56, no. 1 (2013): 3–7.
- Rabin, Carolyn, and Beth Bock. “Desired Features of Smartphone Applications Promoting Physical Activity.” Telemedicine and e-Health 17, no. 10 (2011): 801–3.
- Shapiro, Jennifer R., Tina Koro, Neal Doran, Sheri Thompson, James F. Sallis, Karen Calfas, and Kevin Patrick. “Text4Diet: A Randomized Controlled Study Using Text Messaging for Weight Loss Behaviors.” Preventive Medicine 55, no. 5 (2012): 412–17.
- Spring, Bonnie, Jennifer M. Duncan, E. Amy Janke, Andrea T. Kozak, H. Gene McFadden, Andrew DeMott, Alex Pictor, et al. “Integrating Technology into Standard Weight Loss Treatment: A Randomized Controlled Trial.” JAMA Internal Medicine 173, no. 2 (2013): 105–11.
- Steinberg, Dori M., Deborah F. Tate, Gary G. Bennett, Susan Ennett, Carmen Samuel Hodge, and Dianne S. Ward. “The Efficacy of a Daily Self-Weighing Weight Loss Intervention Using Smart Scales and E-mail.” Obesity 21, no. 9 (2013): 1789–97.
- Svetkey, Laura P., Bryan C. Batch, Pao-Hwa Lin, Stephen S. Intille, Leonor Corsino, Crystal C. Tyson, Hayden B. Bosworth, et al. “Cell Phone Intervention for You (CITY): A Randomized, Controlled Trial of Behavioral Weight Loss Intervention for Young Adults Using Mobile Technology.” Obesity 23, no. 11 (2015): 2133–41.
- Sze, Yan Yan, Tinuke Oluyomi Daniel, Colleen K. Kilanowski, R. Lorraine Collins, and Leonard H. Epstein. “Web-Based and Mobile Delivery of an Episodic Future Thinking Intervention for Overweight and Obese Families: A Feasibility Study.” JMIR mHealth and uHealth 3, no. 4 (2015): e97.
- Thomas, J. Graham, and Rena R. Wing. “Health-e-call, a Smartphone-assisted Behavioral Obesity Treatment: Pilot Study.” JMIR mHealth and uHealth 1, no. 1 (2013): e3.
- Turner-McGrievy, Gabrielle, and Deborah Tate. “Tweets, Apps, and Pods: Results of the 6-Month Mobile Pounds Off Digitally (Mobile POD) Randomized Weight-Loss Intervention among Adults.” Journal of Medical Internet Research 13, no. 4 (2011): e120.
- Willey, Steven, and James K. Walsh. “Outcomes of a Mobile Health Coaching Platform: 12-Week Results of a Single-Arm Longitudinal Study.” JMIR mHealth and uHealth 4, no. 1 (2016): e3.
Effect on Body Weight
Because body weight is the most important parameter associated with obesity, it is reasonable that a majority of the studies examined this parameter directly. A total of 9 of the 14 mobile intervention studies that reported body weight changes found that the intervention group lost more weight than the control group. In these studies, the range of weight loss in the intervention group was 1.27 kg to 10.9 kg, compared with −1.14 kg to 2.45 kg for the control group. The Weighing Everyday to Improve and Gain Health plan, for example, used a smartphone-enabled scale for daily weighing, with a web-based weight loss graph and weekly e-mails with tailored feedback and lessons, and a study of the plan found that the intervention group lost more weight compared with the control group at 6 months (6.55 percent [7.7 kg] vs. 0.35 percent [1.5 kg]) and that a greater percentage achieved 5 percent weight loss (42.6 percent of the intervention group vs. 6.8 percent of the control group) and 10 percent weight loss (27.7 percent of the intervention group vs. 0 percent of the control group).27 The Health-E-Call treatment, which included a smartphone-based component (Health-E-Call app) and a minimal in-person component, resulted in an average weight loss of 10.9 kg, with 90 percent and 70 percent of participants reaching the 5 percent and 10 percent weight-loss milestones at 24 weeks, respectively.28 In another study, college students in a group that received Facebook plus text messaging and personalized feedback lost 2.4 kg compared with 0.63-kg loss in the Facebook-only group and 0.24-kg loss in the waiting-list groups at eight weeks.29 In contrast, the Mobile Pounds Off Digitally study—which required the one group to use a diet and physical activity monitoring app on their mobile device and to interact with study counselors and other participants on Twitter in addition to using to the podcasts that the podcast-only group used—demonstrated an equal degree of weight loss (2.7 percent each) in the two groups.30 (See Table 1.)
Out of the four interventions employing other mHealth devices, two had significant findings favoring the intervention. During a study that tested whether the outcome of physician-directed weight-loss treatment could be improved by adding mobile technology, the mobile technology group lost a mean of 3.9 kg more than the group that received the standard treatment.31 The Self-Monitoring and Recording using Technology trial found mean weight loss of 2.32 percent with use of personal digital assistants (PDAs) with feedback for weight self-monitoring, while the control group lost 1.94 percent.32 Another study demonstrated weight loss of 1.86 kg in the group weight-loss education group, 3.55 kg in a group that used armbands, and 6.59 kg in the group that used both of these approaches.33 (See Table 3.)
Evidence found during a systematic review that investigated the benefits of self-regulatory smartphone apps for weight loss in obese adults was suggestive of the usefulness of these apps for diet self-regulation for weight loss because participants in the smartphone application group in all studies lost at least some body weight. However, no significant difference in the weight loss was found in comparison with other self-monitoring methods.34
The authors of a study of innovative interventions to foster behavioral change in overweight and obese individuals noted three systematic reviews of the use of mHealth to address obesity. Two of these reviews concluded that mHealth was associated with moderate weight loss and positive behavioral changes, while one review showed that the use of SMS data offers numerous methodological benefits over conventional behavioral therapy despite being in its early stages.35
Effects on Waist Circumference and BMI
Three studies that tracked waist circumference reported reduction in waist circumference, while three of five trials measuring BMI documented a decrease in BMI. The Smart Coach for Lifestyle Management trial noted that waist circumference reductions in the intensive counseling/smartphone group were 7.01 cm in males and 5.68 cm in females, compared with 3.00 cm in males and 3.19 cm in females in the control group. Reductions in BMI of 1.3 kg/m2 in the intensive counseling/smartphone group and 1.4 kg/m2 in the control groups were seen.36 In the Self-Monitoring and Recording using Technology trial, the highest percentage reduction of waist circumference—6.4 percent—occurred in that group that used PDAs with feedback, whereas in the PDA-only and control groups the reductions in waist circumference were 5.0 percent and 4.0 percent, respectively.37 In another study, the intervention group using a mobile app called YouPlus reduced their mean waist circumference by 7.2 cm, or 6.6 percent.38 (See Table 3.)
In a post hoc analysis of the effects of an app called Mobile Pounds Off Digitally, app users reported significantly lower BMI at 6 months (31.5 kg/m2) than nonusers (32.5 kg/m2).39 Examination of the effect of the Mobile Audio Manager and Response Tracker system app, which utilized Episodic Future Thinking (EFT) as the behavior-modifying technique to induce weight loss in a pilot study, demonstrated a higher decline in BMI (1.0 vs. 0.2 kg/m2) in the EFT group versus controls. App users also stated that the system was useful, helpful, and easy to use.40 (See Table 3.)
Effects on Lifestyle Behavior: Change in Dietary Behavior
Changes in eating behavior with or without changes in fruit and vegetable intake were examined in six studies.41, 42, 43, 44, 45, 46 In a study of a four-month mDiet intervention wherein the experimental group received two to five weight-management text messages per day and a comparison group received the usual care, with the use of three 24-hour recalls to assess fruit/vegetable intake change and the use of eating behavior inventory (EBI) scores to measure the change in eating behaviors, the authors concluded that moderate short-term weight loss (2.3 kg vs. 0.63 kg) was achieved by sending text messages that promoted healthy eating strategies.47 In the Mobile Pounds Off Digitally study, users of the app and podcasts had a nonsignificantly higher EBI score of 12.4 points with lower fruit intake of 1.4 cups per day and vegetable intake of 2.2 cups per day, compared with podcast-only users’ 9.8 points, 1.6 cups of fruit per day, and 2.6 cups of vegetables per day.48 In the Smart Coach for Lifestyle Management study, it was found that the number of fruit and vegetable servings per day increased in all groups (0.81 for intensive counseling, 0.51 for intensive counseling/smartphone, and 2.1 for less-intensive counseling/smartphone) except for the smartphone-only group, which had a slight decrease (0.05).49
An investigation of the ability of the MyFitnessPal app to influence dietary behavior in primary care patients found that the intervention group receiving app download assistance and 6 months of usual care used a “personal calorie goal” for an extra two days per week compared with the control participants receiving no such assistance.50 In a study in which a smartphone app intervention tool (SMARTAPPetite) targeted change in eating behavior as a primary outcome, a strong association between program participation and improvement in healthy eating was seen, including a direct effect on the consumption of healthy foods.51 In another study, the Episodic Future Thinking group found the Mobile Audio Manager and Response Tracker system more helpful that other methods in affecting eating behavior, with Likert scale ratings of 4.3 in that group versus 3.9 in the control group.52 (See Table 3.)
Daily caloric intake changes were measured in several studies, but none of the results were statistically significant. Decreases in caloric intake of 415.6, 468.2, 218.5, and 249.2 kcal/day in the intensive counseling, intensive counseling/smartphone, less-intensive counseling/smartphone, and smartphone-only groups, respectively, were demonstrated in the Smart Coach for Lifestyle Management trial.53 Although none of their outcome measures were significantly different among any of the interventions studied, the researchers concluded that the results of their pilot trial of a weight-loss intervention using smartphone technology provided preliminary support for use of a smartphone app for self-monitoring as an adjunct to behavioral counseling.54 The Mobile Audio Manager and Response Tracker system trial found larger reductions in energy intake of 791.2 kcal/day in the Episodic Future Thinking group versus 482.4 kcal/day in the control group.55 In the Weighing Every Day to Improve and Gain Health plan, the treatment group consumed fewer calories (1,509 kcal/day) compared with control participants (1,856 kcal/day).56 In the Mobile Pounds Off Digitally study, the group using podcasts and the app minimized their energy intake by 288.8 kcal/day, with controls demonstrating a decrease of 242.5 kcal/day.57 (See Table 3.)
Effects on Lifestyle Behavior: Change in Physical Activity
In five out of nine studies, physical activity levels increased in the mobile device intervention groups relative to the controls. Assessment of physical activity by recording the step counts was done during the Text4Diet trial. Compared to the controls (which received only monthly newsletters), the experimental group receiving daily interactive SMS and MMS increased their step count to 3000 steps per day from their baseline levels, and these higher step counts were associated with greater weight loss. There was a lack of group weight loss differences over 12 months (2.27 lb vs 3.64 lb; control vs intervention) but an improvement in weight-related behaviors and weight outcomes was noted.58 In a study over a much shorter time period (6 weeks) that evaluated effects of thrice weekly text messaging on older non-Hispanic blacks adults, small improvements of 679 and 398 in daily steps and of 11.96 and 4.55 points in perceived activity levels (leisure time exercise questionnaire scores) were seen in the experimental and control group, respectively.59
One study developed and tested three types (social, analytic and affective) of mobile apps in a randomized clinical trial. Participants across all three apps reported significant mean increases of 100.8 minutes/week in brisk walking and of 188.6 minutes/week in MVPA across the eight-week intervention period and significant decreases in the daily amount of discretionary time spent viewing television. All three apps were found to be generally easy to use and acceptable by the participants, who had no prior experience with smartphones.60 Another study reported an average increase of 100.8 mins/week in brisk walking and 188.6 mins/week in MVPA for its three intervention groups.61 While daily total step increased by approximately 800 or 15 percent over three weeks in the study whose participants that were encouraged daily via the mobile phone prompts to increase steps by 20 percent from the previous week.62 Post-hoc analysis in the Mobile Pounds Off Digitally study revealed app users had higher exercise self-monitoring rates (2.6 vs 1.2 days/week) and intentional physical activity (196.4 vs 100.9 kcal/day) than non-app users.63
The ability of B-Mobile app, that prompts users to take physical activity, breaks and delivers feedback on Excessive Sedentary Time (SED) which is a surrogate measure for obesity, to decrease SED and increase Low Intensity Physical Activity (LPA) and Moderate to Vigorous Intensity Physical Activity (MVPA) was evaluated in a study. A decrease in the average percentage SED by 5.9 percent, 5.6 percent and 3.3 percent was noted in three-minute, six-minute and 12-minute activity breaks, respectively. Also, an increase in percentage LPA by 3.9 percent, 3.9 percent, 1.9 percent, and percent MVPA by 2 percent, 1.7 percent and 1.3 percent, respectively, was seen in these three groups.64 A combination of Exergame smartphone apps and motivational texts was evaluated for 12 weeks with results that found the intervention group's activity levels dropped lesser than controls (−356.8 vs −722 min/week MET).65 (See Table 3.)
Effect on Adherence and Satisfaction
All ten studies measuring program adherence recorded greater levels in the intervention group compared to the control, with four noting association of greater adherence with greater weight loss. Adherence in the intervention groups ranged from 60 percent-85 percent. On specific examination of impact of three mobile apps on adherence and satisfaction, all participants found each of the apps easy to use and somewhat helpful with an above average level of satisfaction (Likert scale score: Exercise Tracker-3.00, iFitnessHero-3.73, iTreadmill-4.29).66 Additionally, one study reported increased self-weighing frequencies for the patients (2.1 vs. 1 times/week) when compared to controls.67 (See Table 3.)
Cost Efficacy
Only one study evaluated cost-effectiveness of Sense Wear Armband, a mobile armband device that can be used to provide weight loss intervention, concluding that the technology-based approaches were more cost effective and efficacious than traditional approaches in promoting weight loss via lifestyle changes in sedentary, overweight, and obese adults. The estimated costs per participant per kg lost for each group was $129.15 for Group Weight-Loss education group, $51.43 for Sense Wear Armband, and $55.42 for group using both. This cost for Group Weight-Loss education group was approximately $60 more than for the Sense Wear Armband alone.68
In a systematic review of technological components of weight management programs such as SMS, websites, and smartphone apps, efficacy data for only four apps (FitBit, iStepLog, My Meal Mate and Weight Watchers Mobile) out of the 22 analyzed were available and of these, FitBit One counted steps reliably, iStepLog increased likelihood to log steps, users were more adherent to My Meal Mate app than website or paper methods with overall weight loss of 4.6 kg over six months and Weight Watchers Mobile app + comprehensive program users were eight times more likely to reach their goal of 5-10 percent weight loss than those in the self-help group. All these apps were free to download.69
Another study reported extremely affordable SMS costs of average 10¢ per message sent and received.70 In the course of the Text4Diet trial, participants were reimbursed for SMS costs of $10/month. The trial also explored willingness of the participants to pay for the intervention and found that 89 percent were willing to pay $4.99 for the intervention.71
Behavioral Weight Loss treatment (BWL) has traditionally involved long individual or group treatment sessions needing considerable time and resource investment from the patients resulting in restricted access outside research settings. The costs to implement behavioral weight-loss and lifestyle-change program for individuals with serious mental illnesses in community settings for a 12-month (30-session) intervention were reported to be $16,427 or $1095 per participant.72 In a pilot study, Health-E-Call treatment was proposed as an alternative to the expensive BWL in an attempt to diminish costs and barriers to it.73 Mobile Pounds Off Digitally (another BWL alternative) was reported as a remotely deliverable, low-cost (free to download podcast and apps) intervention with minimal participant contact requirement.74
Relatively low execution costs were reported for the Mobile Audio Manager and Response Tracker system because additional user creation and the supporting software were free, and the system could be used on any device.75 In the Smart Coach for Lifestyle Management trial, the authors reasoned that face-to-face counseling supplemented with mobile technology was cost-effective because they noted weight loss levels comparable to that of the intensive counseling/smartphone group in the less-intensive counseling/smartphone group.76
Discussion
Although a clear majority of the studies examining effects of obesity-related mobile apps on body weight found that the intervention group lost more weight than the control group did, this finding was not universal. Smartphone-enabled mobile apps appeared to be more effective than PDA-enabled or armband apps, although only a single study evaluated the effectiveness of each of the latter two types of apps. Considering the now nearly ubiquitous nature of smartphones in the United States (there are an estimated 222.9 smartphone users in the United States in 2016, a figure that is projected to rise to 264.3 million by 202177), these positive findings regarding smartphone-enabled apps for obesity management are viewed as a positive sign for the future.
Effects of obesity-related apps on lifestyle behaviors were mixed, and the fact that such behaviors are surrogate measures of effectiveness must be kept in mind. The effects of mHealth apps on waste circumference and BMI were generally positive, as were the results measuring changes in dietary behavior as an output measure, but the variety of actual metrics used to measure changes in dietary behavior (e.g., consumption of consumption of fruits and vegetables, achievement of personal calorie goals, changes in daily caloric intake) make comparisons of the different studies problematic at best. Similar concerns existed with studies in which the outcome variable was changes in physical activity, especially because of the fact that increased physical activity, such as in the form of increased step count, was not necessarily associated with weight loss. This finding may be due to the general unreliability of most of these apps to count steps accurately.
Overall, the effects of obesity-related apps on patient satisfaction and adherence were positive and cost effective, and costs associated with the purchase and use of obesity-related apps were generally, but not always, relatively low, especially when compared with the costs associated with conventional behavioral weight loss therapy.
This literature review aimed to analyze results of all trials utilizing mobile technology directed at overweight and/or obese populations concerning their effectiveness and cost in comparison to conventional care. Consistent evidence suggested that mobile-based technological interventions have been efficacious in leading to changes in weight, BMI, waist circumference, and lifestyle behavior.
Lifestyle behaviors related to diet, physical activity, and sedentary behavior were mainly targeted. The interventions measuring changes in dietary intake and dietary behavior revealed an increase in fruit and vegetable intake and positive changes in eating behavior in all participants using the interventions under study. Overall, 80 percent of the studies that investigated caloric intake demonstrated a decrease in daily caloric intake. Furthermore, with these interventions, an increase in physical activity in the form of daily steps and exercise ranging from low to vigorous in intensity was observed in more than half of the studies.
Among the studies reviewed, we found minimal discussion or evaluation of the costs relative to the benefits of mHealth obesity interventions, with the exception of one study that found the estimated cost per participant per kilogram lost via technology-based approaches to be lower than the cost of traditional approaches. Few studies of the efficacy of mHealth interventions mentioned associated costs or made inferences regarding the inexpensiveness of their interventions without citing the actual cost or running a cost-effectiveness analysis. Many of the apps included in these studies were offered for free, while some had minimal costs associated with the SMS component of the intervention. A large portion of the mobile apps analyzed were free or inexpensive, permitting easy access to the general population.
This literature review was limited by the design and quality of included studies, the number of databases accessed, and the search strategy utilized. It was difficult to identify the potential impact of mHealth on obesity-related measures because of the wide variation in study design. Also, with respect to quality, several studies were performed on small sample sizes and were of short duration, so inferences should be drawn with caution. Although some studies did not find clinically significant results during their short trial duration, the possibility of a longer-duration intervention producing possible significant results cannot be ruled out. Another main concern was that the publications on the cost-effectiveness of mHealth interventions for adult obesity were sparse, which restricts the generalizability of the findings. Furthermore, mobile device use necessitates that the study population possess a certain education level and socioeconomic status. Additionally, as the studies were evaluated to establish relevancy, publication and research bias cannot be ruled out.
In general, few studies addressed the cost-effectiveness of mHealth technologies. Most studies conducted so far have focused on assessing the quality of the outcomes, and these studies should continue, especially considering the quickly evolving nature of market offerings. However, in order to assess their usability and value for the money, further studies analyzing the cost-effectiveness of mobile health interventions are warranted. Additionally, whether a combination of conventional and mobile interventions for obesity would offer greater benefit for the cost, compared with a mobile-only approach, needs to be further studied.
A 2016 presentation at the European Obesity Summit indicated that nearly 29,000 weight management apps were currently available online from five mobile app stores (the Apple store, the Google store, the Amazon store, the Blackberry store, and the Windows store), but only 17 of them (less than 0.5 percent) had been developed using any kind of verifiable professional expertise.78 Not only are better designed obesity-related apps needed, but many more well-designed studies are necessary to evaluate the market offerings in this fast-changing field.
Conclusion
In this study, mHealth interventions were found to be more effective than conventional approaches in facilitating behavior modifications to promote weight loss and lifestyle changes to prevent and control adult obesity. Available data on concomitant expenses seem to indicate that these interventions can potentially be remotely delivered relatively inexpensively, improving access, promoting healthcare efficiency, and reducing the healthcare cost burden.
Contributor Information
Niharika N. Bhardwaj, Marshall University in Huntington, WV.
Bezawit Wodajo, Marshall University in Huntington, WV.
Keerthi Gochipathala, Marshall University in Huntington, WV.
David P. Paul, III, Monmouth University in West Long Branch, NJ.
Alberto Coustasse, Marshall University in South Charleston, WV.
Notes
- 1.Ogden Cynthia L., Carroll Margaret D., Kit Brian K., Flegal Katherine M. “Prevalence of Childhood and Adult Obesity in the United States, 2011–2012.”. JAMA. 2014;311(8):806–84. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Trust for America's Health and Robert Wood Johnson Foundation. “Adult Obesity in the United States 2015.” Available at http://stateofobesity.org/adult-obesity/ (accessed February 24, 2017).
- 3.Centers for Disease Control and Prevention (CDC). “Press Briefing Transcript: CDC Weight of the Nation Press Briefing..” May 7, 2012. Available at http://www.cdc.gov/media/releases/2012/t0507_weight_nation.html (accessed August 25, 2016)
- 4.Schmandt Rosemarie E., Iglesias David A., Na Co Ngai, Lu Karen H. “Understanding Obesity and Endometrial Cancer Risk: Opportunities for Prevention.”. American Journal of Obstetrics and Gynecology. 2011;205(6):518–25. doi: 10.1016/j.ajog.2011.05.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Apovian Caroline M., Gokce Noyan. “Obesity and Cardiovascular Disease.”. Circulation. 2012;125(9):1178–82. doi: 10.1161/CIRCULATIONAHA.111.022541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akholkar Pankaj J., Gandhi Amita A. “Prevalence of Obesity in Diabetic and Non-diabetic Population.”. International Journal of Research in Medical Sciences. 2015;3(8):2114–17. [Google Scholar]
- 7.CDC. “Adult Obesity Facts.” September 21, 2015. Available at https://www.cdc.gov/obesity/data/adult.html (accessed August 25, 2016)
- 8.Wang Y. Claire, McPherson Klim, Marsh Tim, Gortmaker Steven L., Brown Martin. “Health and Economic Burden of the Projected Obesity Trends in the USA and the UK.”. The Lancet. 2011;378(9793):815–25. doi: 10.1016/S0140-6736(11)60814-3. [DOI] [PubMed] [Google Scholar]
- 9.Unick Jessica L., Jakicic John M., Marcus Bess H. “Contribution of Behavior Intervention Components to 24-Month Weight Loss.”. Medicine and Science in Sports and Exercise. 2010;42(4):745. doi: 10.1249/MSS.0b013e3181bd1a57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Henry Robert R., Chilton Robert, Timothy Garvey W. “New Options for the Treatment of Obesity and Type 2 Diabetes Mellitus (Narrative Review).”. Journal of Diabetes and Its Complications. 2013;27(5):508–18. doi: 10.1016/j.jdiacomp.2013.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kay Misha, Santos Jonathan, Takane Marina. “mHealth: New Horizons for Health through Mobile Technologies.”. World Health Organization. 2011;64(7):66–71. [Google Scholar]
- 12.Howitt Peter, Darzi Ara, Yang Guang-Zhong, Ashrafian Hutan, Atun Rifat, Barlow James, Blakemore Alex, et al. “Technologies for Global Health.”. The Lancet. 2012;380(9840):507–35. doi: 10.1016/S0140-6736(12)61127-1. [DOI] [PubMed] [Google Scholar]
- 13.Coons Michael J., DeMott Andrew, Buscemi Joanna, Duncan Jennifer M., Pellegrini Christine A., Steglitz Jeremy, Pictor Alexander, Spring Bonnie. “Technology Interventions to Curb Obesity: A Systematic Review of the Current Literature.”. Current Cardiovascular Risk Reports. 2012;6(2):120–34. doi: 10.1007/s12170-012-0222-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bacigalupo R., Cudd P., Littlewood C., Bissell P., Hawley M.S., Buckley Woods H. “Interventions Employing Mobile Technology for Overweight and Obesity: An Early Systematic Review of Randomized Controlled Trials.”. Obesity Reviews. 2013;14(4):279–91. doi: 10.1111/obr.12006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Epstein Joel, Bequette Amanda W. “Smart Phone Applications in Clinical Practice.”. Journal of Mental Health Counseling. 2013;35(4):283. [Google Scholar]
- 16.Goggin Gerard. Cell Phone Culture: Mobile Technology in Everyday Life. New York: Routledge; 2006. [Google Scholar]
- 17.Wu Robert C., Morra Dante, Quan Sherman, Lai Sannie, Zanjani Samira, Abrams Howard, Rossos Peter G. “The Use of Smartphones for Clinical Communication on Internal Medicine Wards.”. Journal of Hospital Medicine. 2010;5(9):553–59. doi: 10.1002/jhm.775. [DOI] [PubMed] [Google Scholar]
- 18.Breton Emily R., Fuemmeler Bernard F., Abroms Lorien C. “Weight Loss—There Is an App for That! But Does It Adhere to Evidence-informed Practices?”. Translational Behavioral Medicine. 2011;1(4):523–29. doi: 10.1007/s13142-011-0076-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wolfenden Luke, Brennan Leah, Britton Ben I. “Intelligent Obesity Interventions Using Smartphones.”. Preventive Medicine. 2010;51(6):519–20. doi: 10.1016/j.ypmed.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 20.Ibid.
- 21.Kong Fanyu, Tan Jindong. “DietCam: Automatic Dietary Assessment with Mobile Camera Phones.”. Pervasive and Mobile Computing. 2012;8(1):147–63. [Google Scholar]
- 22.Klasnja Predrag, Pratt Wanda. “Healthcare in the Pocket: Mapping the Space of Mobile-Phone Health Interventions.”. Journal of Biomedical Informatics. 2012;45(1):184–98. doi: 10.1016/j.jbi.2011.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yao W., Chu C.H., Li Z. “The Use of RFID in Healthcare: Benefits and Barriers.”. Proceedings of the 2010 IEEE International Conference on RFID Technology and Applications (RFID-TA) 2010:128–34. [Google Scholar]
- 24.Coustasse A., Tomblin S., Slack C. “Impact of Radio-Frequency Identification (RFID) Technologies on the Hospital Supply Chain: A Literature Review.”. Perspectives in Health Information Management. Fall 2013 [PMC free article] [PubMed] [Google Scholar]
- 25.Deslich S., Coustasse A. “Expanding Technology in the ICU.”. Telemedicine and e-Health. 2014;20(5):485–92. doi: 10.1089/tmj.2013.0102. [DOI] [PubMed] [Google Scholar]
- 26.Porterfield A., Engelbert K., Coustasse A. “Electronic Prescribing: Improving the Efficiency and Accuracy of Prescribing in the Ambulatory Care Setting.”. Perspectives in Health Information Management. Spring 2014 [PMC free article] [PubMed] [Google Scholar]
- 27.Steinberg Dori M., Tate Deborah F., Bennett Gary G., Ennett Susan, Samuel Hodge Carmen, Ward Dianne S. “The Efficacy of a Daily Self-Weighing Weight Loss Intervention Using Smart Scales and E-mail.”. Obesity. 2013;21(9):1789–97. doi: 10.1002/oby.20396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thomas J. Graham, Wing Rena R. “Health-e-call, a Smartphone-assisted Behavioral Obesity Treatment: Pilot Study.”. JMIR mHealth and uHealth. 2013;1(1):e3. doi: 10.2196/mhealth.2164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Napolitano Melissa A., Hayes Sharon, Bennett Gary G., Ives Allison K., Foster Gary D. “Using Facebook and Text Messaging to Deliver a Weight Loss Program to College Students.”. Obesity. 2013;21(1):25–31. doi: 10.1002/oby.20232. [DOI] [PubMed] [Google Scholar]
- 30.Turner-McGrievy Gabrielle, Tate Deborah. “Tweets, Apps, and Pods: Results of the 6-Month Mobile Pounds Off Digitally (Mobile POD) Randomized Weight-Loss Intervention among Adults.”. Journal of Medical Internet Research. 2011;13(4):e120. doi: 10.2196/jmir.1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Spring Bonnie, Duncan Jennifer M., Amy Janke E., Kozak Andrea T., Gene McFadden H., DeMott Andrew, Pictor Alex, et al. “Integrating Technology into Standard Weight Loss Treatment: A Randomized Controlled Trial.”. JAMA Internal Medicine. 2013;173(2):105–11. doi: 10.1001/jamainternmed.2013.1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Burke Lora E., Styn Mindi A., Sereika Susan M., Conroy Molly B., Ye Lei, Glanz Karen, Ann Sevick Mary, Ewing Linda J. “Using mHealth Technology to Enhance Self-Monitoring for Weight Loss: A Randomized Trial.”. American Journal of Preventive Medicine. 2012;43(1):20–26. doi: 10.1016/j.amepre.2012.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Archer Edward, Groessl Erik J., Sui Xuemei, McClain Amanda C., Wilcox Sara, Hand Gregory A., Meriwether Rebecca A., Blair Steven N. “An Economic Analysis of Traditional and Technology-based Approaches to Weight Loss.”. American Journal of Preventive Medicine. 2012;43(2):176–82. doi: 10.1016/j.amepre.2012.04.018. [DOI] [PubMed] [Google Scholar]
- 34.Semper H. M., Povey R., Clark-Carter D. “A Systematic Review of the Effectiveness of Smartphone Applications That Encourage Dietary Self-Regulatory Strategies for Weight Loss in Overweight and Obese Adults.”. Obesity Reviews. 2016;17(9):895–906. doi: 10.1111/obr.12428. [DOI] [PubMed] [Google Scholar]
- 35.Okorodudu D. E., Bosworth H.B., Corsino L. “Innovative Interventions to Promote Behavioral Change in Overweight or Obese Individuals: A Review of the Literature.”. Annals of Medicine. 2015;47(3):179–85. doi: 10.3109/07853890.2014.931102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Willey Steven, Walsh James K. “Outcomes of a Mobile Health Coaching Platform: 12-Week Results of a Single-Arm Longitudinal Study.”. JMIR mHealth and uHealth. 2016;4(1):e3. doi: 10.2196/mhealth.4933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Burke Lora E., Styn Mindi A., Sereika Susan M., Conroy Molly B., Ye Lei, Glanz Karen, Ann Sevick Mary, Ewing Linda J. “Using mHealth Technology to Enhance Self-Monitoring for Weight Loss: A Randomized Trial”. [DOI] [PMC free article] [PubMed]
- 38.Willey Steven, Walsh James K. “Outcomes of a Mobile Health Coaching Platform: 12-Week Results of a Single-Arm Longitudinal Study”. [DOI] [PMC free article] [PubMed]
- 39.Turner-McGrievy Gabrielle M., Beets Michael W., Moore Justin B., Kaczynski Andrew T., Barr-Anderson Daheia J., Tate Deborah F. “Comparison of Traditional versus Mobile App Self-Monitoring of Physical Activity and Dietary Intake among Overweight Adults Participating in an mHealth Weight Loss Program.”. Journal of the American Medical Informatics Association. 2013;20(3):513–18. doi: 10.1136/amiajnl-2012-001510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sze Yan Yan, Oluyomi Daniel Tinuke, K. Kilanowski Colleen, Lorraine Collins R., Epstein Leonard H. “Web-Based and Mobile Delivery of an Episodic Future Thinking Intervention for Overweight and Obese Families: A Feasibility Study.”. JMIR mHealth and uHealth. 2015;3(4):e97. doi: 10.2196/mhealth.4603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Allen Jerilyn K., Stephens Janna, Dennison Himmelfarb Cheryl R., Stewart Kerry J., Hauck Sara. “Randomized Controlled Pilot Study Testing Use of Smartphone Technology for Obesity Treatment.”. Journal of Obesity. 2013;2013:151597. doi: 10.1155/2013/151597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Turner-McGrievy Gabrielle M., Beets Michael W., Moore Justin B., Kaczynski Andrew T., Barr-Anderson Daheia J., Tate Deborah F. “Comparison of Traditional versus Mobile App Self-Monitoring of Physical Activity and Dietary Intake among Overweight Adults Participating in an mHealth Weight Loss Program”. [DOI] [PMC free article] [PubMed]
- 43.Sze Yan Yan, Oluyomi Daniel Tinuke, Kilanowski Colleen K., Lorraine Collins R., Epstein Leonard H. “Web-Based and Mobile Delivery of an Episodic Future Thinking Intervention for Overweight and Obese Families: A Feasibility Study”. [DOI] [PMC free article] [PubMed]
- 44.Norman Gregory J., Kolodziejczyk Julia K., Adams Marc A., Patrick Kevin, Marshall Simon J. “Fruit and Vegetable Intake and Eating Behaviors Mediate the Effect of a Randomized Text-Message Based Weight Loss Program.”. Preventive Medicine. 2013;56(1):3–7. doi: 10.1016/j.ypmed.2012.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Laing Brian Yoshio, Mangione Carol M., Tseng Chi-Hong, Leng Mei, Vaisberg Ekaterina, Mahida Megha, Bholat Michelle, Glazier Eve, Morisky Donald E., Bell Douglas S. “Effectiveness of a Smartphone Application for Weight Loss Compared with Usual Care in Overweight Primary Care Patients: A Randomized, Controlled Trial.”. Annals of Internal Medicine. 2014;161(10, suppl.):S5–S12. doi: 10.7326/M13-3005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gilliland Jason, Sadler Richard, Clark Andrew, O'Connor Colleen, Milczarek Malgorzata, Doherty Sean. “Using a Smartphone Application to Promote Healthy Dietary Behaviors and Local Food Consumption.”. BioMed Research International. 2015;2015:1–11. doi: 10.1155/2015/841368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Norman Gregory J., Kolodziejczyk Julia K., Adams Marc A., Patrick Kevin, Marshall Simon J. “Fruit and Vegetable Intake and Eating Behaviors Mediate the Effect of a Randomized Text-Message Based Weight Loss Program”. [DOI] [PMC free article] [PubMed]
- 48.Turner-McGrievy Gabrielle M., Beets Michael W., Moore Justin B., Kaczynski Andrew T., Barr-Anderson Daheia J., Tate Deborah F. “Comparison of Traditional versus Mobile App Self-Monitoring of Physical Activity and Dietary Intake among Overweight Adults Participating in an mHealth Weight Loss Program”. [DOI] [PMC free article] [PubMed]
- 49.Allen Jerilyn K., Stephens Janna, Dennison Himmelfarb Cheryl R., Stewart Kerry J., Hauck Sara. “Randomized Controlled Pilot Study Testing Use of Smartphone Technology for Obesity Treatment”. [DOI] [PMC free article] [PubMed]
- 50.Laing Brian Yoshio, Mangione Carol M., Tseng Chi-Hong, Leng Mei, Vaisberg Ekaterina, Mahida Megha, Bholat Michelle, Glazier Eve, Morisky Donald E., Bell Douglas S. “Effectiveness of a Smartphone Application for Weight Loss Compared with Usual Care in Overweight Primary Care Patients: A Randomized, Controlled Trial”. [DOI] [PMC free article] [PubMed]
- 51.Gilliland Jason, Sadler Richard, Clark Andrew, O'Connor Colleen, Milczarek Malgorzata, Doherty Sean. “Using a Smartphone Application to Promote Healthy Dietary Behaviors and Local Food Consumption”. [DOI] [PMC free article] [PubMed]
- 52.Sze Yan Yan, Oluyomi Daniel Tinuke, K. Kilanowski Colleen, Lorraine Collins R., Epstein Leonard H. “Web-Based and Mobile Delivery of an Episodic Future Thinking Intervention for Overweight and Obese Families: A Feasibility Study”. [DOI] [PMC free article] [PubMed]
- 53.Allen Jerilyn K., Stephens Janna, Dennison Himmelfarb Cheryl R., Stewart Kerry J., Hauck Sara. “Randomized Controlled Pilot Study Testing Use of Smartphone Technology for Obesity Treatment”. [DOI] [PMC free article] [PubMed]
- 54.Ibid.
- 55.Willey Steven, Walsh James K. “Outcomes of a Mobile Health Coaching Platform: 12-Week Results of a Single-Arm Longitudinal Study”. [DOI] [PMC free article] [PubMed]
- 56.Steinberg Dori M., Tate Deborah F., Bennett Gary G., Ennett Susan, Samuel Hodge Carmen, Ward Dianne S. “The Efficacy of a Daily Self-Weighing Weight Loss Intervention Using Smart Scales and E-mail”. [DOI] [PMC free article] [PubMed]
- 57.Turner-McGrievy Gabrielle, Tate Deborah. “Tweets, Apps, and Pods: Results of the 6-Month Mobile Pounds Off Digitally (Mobile POD) Randomized Weight-Loss Intervention among Adults”. [DOI] [PMC free article] [PubMed]
- 58.King Abby C., Hekler Eric B., Grieco Lauren A., Winter Sandra J., Sheats Jylana L., Buman Matthew P., Banerjee Banny, Robinson Thomas N., Cirimele Jesse. “Harnessing Different Motivational Frames Via Mobile Phones to Promote Daily Physical Activity and Reduce Sedentary Behavior in Aging Adults.”. PloS One. 2013;8(4):e62613. doi: 10.1371/journal.pone.0062613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kim Bang Hyun, Glanz Karen. “Text Messaging to Motivate Walking in Older African Americans: A Randomized Controlled Trial.”. American Journal of Preventive Medicine. 2013;44(1):71–75. doi: 10.1016/j.amepre.2012.09.050. [DOI] [PubMed] [Google Scholar]
- 60.King Abby C., Hekler Eric B., Grieco Lauren A., Winter Sandra J., Sheats Jylana L., Buman Matthew P., Banerjee Banny, Robinson Thomas N., Cirimele Jesse. “Harnessing Different Motivational Frames Via Mobile Phones to Promote Daily Physical Activity and Reduce Sedentary Behavior in Aging Adults”. [DOI] [PMC free article] [PubMed]
- 61.Fukuoka Yoshimi, Vittinghoff Eric, Son Jong So, Haskell William. “Innovation to Motivation—Pilot Study of a Mobile Phone Intervention to Increase Physical Activity Among Sedentary Women.”. Preventive Medicine. 2010;51(3):287–89. doi: 10.1016/j.ypmed.2010.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bond Dale S., Graham Thomas J., Raynor Hollie A., Moon Jon, Sieling Jared, Trautvetter Jennifer, Leblond Tiffany, Wing Rena R. “B-MOBILE: A Smartphone-based Intervention to Reduce Sedentary Time in Overweight/Obese Individuals: A Within-Subjects Experimental Trial.”. PLoS One. 2014;9(6):e100821. doi: 10.1371/journal.pone.0100821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Turner-McGrievy Gabrielle M., Beets Michael W., Moore Justin B., Kaczynski Andrew T., Barr-Anderson Daheia J., Tate Deborah F. “Comparison of Traditional versus Mobile App Self-Monitoring of Physical Activity and Dietary Intake among Overweight Adults Participating in an mHealth Weight Loss Program”. [DOI] [PMC free article] [PubMed]
- 64.Cowdery Joan, Majeske Paul, Frank Rebecca, Brown Devin. “Exergame Apps and Physical Activity: The Results of the ZOMBIE Trial.”. American Journal of Health Education. 2015;46(4):216–22. [Google Scholar]
- 65.Rabin Carolyn, Bock Beth. “Desired Features of Smartphone Applications Promoting Physical Activity.”. Telemedicine and e-Health. 2011;17(10):801–3. doi: 10.1089/tmj.2011.0055. [DOI] [PubMed] [Google Scholar]
- 66.Bond Dale S., Graham Thomas J., Raynor Hollie A., Moon Jon, Sieling Jared, Trautvetter Jennifer, Leblond Tiffany, Wing Rena R. “B-MOBILE: A Smartphone-based Intervention to Reduce Sedentary Time in Overweight/Obese Individuals: A Within-Subjects Experimental Trial”. [DOI] [PMC free article] [PubMed]
- 67.Svetkey Laura P., Batch Bryan C., Lin Pao-Hwa, Intille Stephen S., Corsino Leonor, Tyson Crystal C., Bosworth Hayden B., et al. “Cell Phone Intervention for You (CITY): A Randomized, Controlled Trial of Behavioral Weight Loss Intervention for Young Adults Using Mobile Technology.”. Obesity. 2015;23(11):2133–41. doi: 10.1002/oby.21226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Archer Edward, Groessl Erik J., Sui Xuemei, McClain Amanda C., Wilcox Sara, Hand Gregory A., Meriwether Rebecca A., Blair Steven N. “An Economic Analysis of Traditional and Technology-based Approaches to Weight Loss”. [DOI] [PubMed]
- 69.Gilmore L. Anne, Duhé Abby F., Frost Elizabeth A., Redman Leanne M. “The Technology Boom a New Era in Obesity Management.”. Journal of Diabetes Science and Technology. 2014;8(3):596–608. doi: 10.1177/1932296814525189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shaw Ryan, Bosworth Hayden. “Short Message Service (SMS) Text Messaging as an Intervention Medium for Weight Loss: A Literature Review.”. Health Informatics Journal. 2012;18(4):235–50. doi: 10.1177/1460458212442422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shapiro Jennifer R., Koro Tina, Doran Neal, Thompson Sheri, Sallis James F., Calfas Karen, Patrick Kevin. “Text4Diet: A Randomized Controlled Study Using Text Messaging for Weight Loss Behaviors.”. Preventive Medicine. 2012;55(5):412–17. doi: 10.1016/j.ypmed.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 72.Stumbo Scott P., Yarborough Bobbi Jo H., Yarborough Micah T., Janoff Shannon L., Stevens Victor J., Lewinsohn Mark, Green Carla A. “Costs of Implementing a Behavioral Weight-Loss and Lifestyle-Change Program for Individuals with Serious Mental Illnesses in Community Settings.”. Translational Behavioral Medicine. 2015;5(3):269–76. doi: 10.1007/s13142-015-0322-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Thomas J. Graham, Wing Rena R. “Health-e-call, a Smartphone-assisted Behavioral Obesity Treatment: Pilot Study”. [DOI] [PMC free article] [PubMed]
- 74.Turner-McGrievy Gabrielle, Tate Deborah. “Tweets, Apps, and Pods: Results of the 6-Month Mobile Pounds Off Digitally (Mobile POD) Randomized Weight-Loss Intervention among Adults”. [DOI] [PMC free article] [PubMed]
- 75.Sze Yan Yan, Oluyomi Daniel Tinuke, Kilanowski Colleen K., Lorraine Collins R., Epstein Leonard H. “Web-Based and Mobile Delivery of an Episodic Future Thinking Intervention for Overweight and Obese Families: A Feasibility Study”. [DOI] [PMC free article] [PubMed]
- 76.Allen Jerilyn K., Stephens Janna, Dennison Himmelfarb Cheryl R., Stewart Kerry J., Hauck Sara. “Randomized Controlled Pilot Study Testing Use of Smartphone Technology for Obesity Treatment”. [DOI] [PMC free article] [PubMed]
- 77.Statista. “Number of Smartphone Users in the United States from 2010 to 2021 (in Millions).” Available at https://www.statista.com/statistics/201182/forecast-of-smartphone-users-in-the-us/ (accessed October 24, 2016)
- 78.Davenport Liam.“Very Few Mobile Weight-Loss Apps Have Professional Input.” Medscape, June 4, 2016. Available at http://www.medscape.com/viewarticle/864312?nlid=106108_2981&src=wnl_dne_160607_mscpedit&uac=210978HR&impID=1120160&faf=1 (accessed June 6, 2016)