Abstract
[Purpose] This study report a case of a patient with hemiparetic stroke who showed significantly reduced foot pain when ankle spasticity was reduced using nerve and motor point blocks with 20% ethyl alcohol. [Subject and Methods] A 58-year-old woman with left hemiparesis following intracranial hemorrhage five years previously presented with pain in the left fifth metatarsal head for two years (numeric rating scale[NRS]: 8). Erythema and edema were observed on the lateral aspect of the head of the fifth metatarsal bone. She was diagnosed with a Tailor’s bunion. Spasticity was observed in the left ankle plantar flexor and ankle supinator (Modified Ashworth Scale: 1+). Using 20% ethyl alcohol, a block in the medial and lateral motor branches to the gastrocnemius muscle of the left tibial nerve and the motor point of the left posterior tibialis muscle was performed. [Results] After the alcohol block, spasticity had almost disappeared and foot pain was significantly reduced (NRS: 1). Results from the foot pressure measurement system test showed foot contact pressure was highly distributed to the lateral forefoot pre-block. After the block, the distribution of foot contract pressure was similar to normal distribution. [Conclusion] Clinicians should consider the possibility that spasticity can contribute to foot pain.
Keywords: Tailor’s bunion, Spasticity, Alcohol block
INTRODUCTION
Spasticity is a frequent consequence of stroke1, 2). In the lower leg, spasticity usually occurs in ankle plantar flexor and supinator muscles3). This condition alters musculoskeletal position or alignment during walking4). This malposition or malalignment causes mechanical stress to foot joints in the lateral forefoot area, and joints under this stress are likely to be inflamed and painful4). Foot pain causes difficulty in standing and walking, and thus limits daily living activities. Accordingly, management of foot pain is necessary in patients with stroke. The malposition or malalignment of the foot can be managed by the control of spasticity. It was proposed that correcting the malposition or malalignment can reduce abnormal mechanical pressure in specific areas of the foot, which leads to a reduction in foot pain. Of the several options available for the management of spasticity, the clinical usefulness of nerve and motor point blocks with alcohol has been well demonstrated5,6,7).
In the current study, whether a reduction of ankle spasticity using nerve and motor point blocks with 20% ethyl alcohol can manage foot pain was examined.
SUBJECT AND METHODS
A 58-year-old woman visited the rehabilitation department of a university hospital due to piercing pain (numeric rating scale [NRS]: 8) in the left fifth metatarsal head for two years. Erythema and edema were present on the lateral aspect of the head of the fifth metatarsal bone (Fig. 1A). The patient provided informed signed consent for participation in the study. The study was approved by the research ethics committee of Yeungnam University Hospital (YUH-16-0425-D7). On the foot X-ray, the fourth and fifth intermetatarsal angle of the left foot was 7.7° (Fig. 1B). She was diagnosed with a Tailor’s bunion. She had a history of intracerebral hemorrhage on the right basal ganglia about five years previously. She had spasticity in the left ankle plantar flexor and ankle supinator. The degree of her spasticity was a Modified Ashworth Scale (MAS)8) of 1+. The ankle clonus was checked and found to be 2–3 beats. Additionally, slight motor weakness (Medical Research Council9): 4+) in the left upper and lower extremities was shown. Other neurological symptoms, including sensory and cognitive deficits, were not present. At first, 0.5 ml of 2% lidocaine with 10 mg triamcinolone acetonide was injected into the tender point of the left fifth metatarsal head area. Two weeks after this injection the NRS score was unchanged.
Fig. 1.
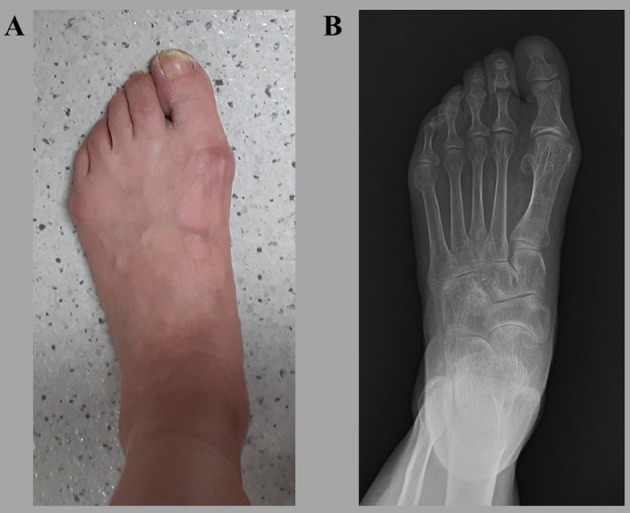
(A) An image of the patient’s left foot shows erythema and edema in the fifth metatarsal head area. (B) The left foot X-ray showed that the fourth and fifth intermetatarsal angle was 7.7°
It was proposed that the ankle spasticity in the patient caused repetitive pressure and shearing between the soft tissue and head of the fifth metatarsal bone. Thus, we considered the possibility that controlling spasticity might be helpful in the management of pain from the Tailor’s bunion, and decided to control spasticity in this patient using a nerve or motor point block with 20% ethyl alcohol. To reduce the spasticity of the left ankle plantar flexor, the medial and lateral motor branches to the gastrocnemius muscle of the left tibial nerve were completely blocked with 5 ml of 20% ethyl alcohol. The block of nerve branches was performed based on the method described by Jang et al5). To manage spasticity in the left ankle supinator a motor point block was performed in the left tibialis posterior muscle with 5 ml of 20% ethyl alcohol. For all procedures the patient lay in the prone position. Both nerve and motor points were located using the nerve stimulator at the popliteal area and at the mid-calf level, respectively. The cathode stimulating needle (Teflon-coated, 23-gauge needle) was slowly advanced in the direction of the nerve and posterior tibialis muscle. The needle hub was connected to injection tubing that bore the syringe containing the 20% ethyl alcohol. Contractions were seen and palpated as the tip came close to the nerve or motor point of the tibialis posterior. At this stage, the intensity of the current was between 3 mA and 5 mA. After the needle was placed close to the targeted nerve or motor point, the needle was rotated to reach the end-point. The tip is assumed to be in contact with the nerve or motor point when maximum contraction is obtained with minimum current. The needle was finally positioned at a current of 1 mA with nerve block and 3.5 mA with motor point block. Additionally, the patient underwent the stretching exercises for the left ankle plantar flexors and ankle supinators for 2 weeks after the alcohol block (Monday through Friday: 15 mins × 1 time/day).
To evaluate dynamic foot pressure, the foot pressure measurement system (FPMS) (TPScan; BioMechanics, Goyang, Korea) was used10). Dynamic foot contact pressure data during gait were recorded on the FPMS floor mat (40.5 × 40.5 cm2) at the middle of the gait test. The foot pressure was presented as a color: red is the highest pressure followed by orange, yellow, green, and blue. Foot contact pressure was evaluated twice before and one- month after the nerve and motor point block procedure. Before the procedure, contact pressure was highly distributed to the lateral forefoot, however, reduced distribution was observed in the medial forefoot and hindfoot (Fig. 2). After the procedure, the distribution of foot contract pressure was found to be similar to that of a normal control (56-year-old female individual).
Fig. 2.
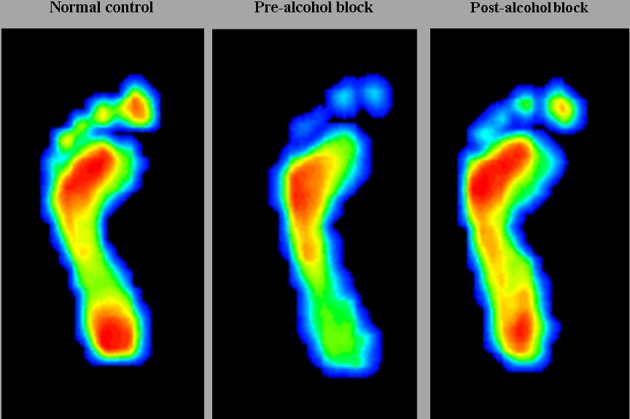
Foot pressure measurement image
The foot pressure image of a normal foot and the images of the patient’s foot pressure showing alterations pre-alcohol block and post-alcohol block.
RESULTS
At the follow-up evaluation, two weeks after the alcohol block, the spasticity in the left ankle plantar flexor and supinator had disappeared (MAS: 0). In addition, ankle clonus was not present. Moreover, the pain in the left fifth metatarsal head was significantly reduced from NRS 8 to NRS 1. At one, two, and three months after the alcohol block the effects on ankle spasticity and foot pain were sustained.
DISCUSSION
In the present study, foot pain related to Tailor’s bunion was reduced after spasticity treatment using nerve and motor point block with 20% ethyl alcohol.
Approximately 65% of all patients with stroke experience spasticity1). In the lower leg, spasticity occurs most frequently in the ankle plantar flexor and supinator3). Although the incidence of foot pain in patients with stroke has not been investigated, patients with stroke are prone to have foot pain due to deteriorated musculoskeletal position or alignment induced by spasticity or motor weakness. The Tailor’s bunion or bunionette, which was first described by Davies in 194911), is a painful bony prominence on the lateral, dorsolateral, or plantar aspect of the head of the fifth metatarsal bone12). The conflict between the fifth metatarsal head and footwear has been reported to be the cause of Tailor’s bunions12). In the patient, the spasticity in the ankle plantar flexor and supinator appeared to cause repeated mechanical stress and chronic irritation in the fifth metatarsal head area, which is thought to induce a Tailor’s bunion.
For the management of foot pain due to Tailor’s bunion, corticosteroids were injected into the tender point of the fifth metatarsal head area; however, the patient’s pain was unresponsive to this injection. It was considered that non-controlled spasticity can lead to continuous mechanical stress or irritation and repeated occurrence of inflammation in the fifth metatarsal head area. Therefore, the spasticity was controlled using a block with 20% ethyl alcohol on the motor branches to the gastrocnemius muscle of the tibial nerve and the motor points of the posterior tibialis muscle. Several previous studies have shown the effectiveness and safety of these procedures. Alcohol acts by denaturing proteins, resulting in the splitting of myelin sheathes. After the block with ethyl alcohol, spasticity in this patient had almost disappeared (from MAS 1+ to MAS 0). Also, the patient received the stretching exercises for the ankle plantar flexors and the ankle supinators. The stretching exercise is known to effectively reduce spasticity13, 14) by increasing tissue extensibility15). It was thought that the reduced spasticity in the patient was attributed, at least in part, to the stretching exercises. It is thought that the mechanical stress and irritation in the fifth metatarsal head area during walking were significantly reduced with the disappearance of spasticity in this patient. When the stress and irritation were reduced after the management of spasticity, the pain due to Tailor’s bunion appeared to be significantly reduced.
In addition, the FPMS was used for detailed evaluation of the effect of the 20% ethyl alcohol block. Before the alcohol block, foot pressure during walking was highly concentrated in the lateral forefoot. After the control of spasticity with the alcohol block, increased contract foot pressure in the hindfoot and medial forefoot were observed. This change in pressure distribution is concurrent with the results of several previous studies10, 16, 17). Using FPMS, it was confirmed that mechanical stress abnormally concentrated on the fifth metatarsal head area was corrected to near normal following the alcohol blocks on the tibial nerve branches and the motor point of the tibialis posterior muscle. The correction of foot contact pressure distribution appears to have contributed to the pain reduction in the fifth metatarsal head area.
In conclusion, the case of a patient with chronic hemiparetic stroke whose pain due to Tailor’s bunion showed relief following the control of spasticity using nerve and motor point blocks with 20% ethyl alcohol was reported. This study showed that deteriorated foot position or alignment induced by spasticity and malposition/malalignment-related foot pain can be successfully managed by nerve and motor point blocks with 20% ethyl alcohol. On the basis of the clinical experience in this study, when clinicians treat foot pain in patients with stroke, they should consider the possibility that spasticity can contribute to the development of foot pain. This is first study to show that management of spasticity can reduce foot pain in a patient with hemiparetic stroke. However, since this study reports a single case, further studies involving a larger number of patients are necessary.
Acknowledgments
This work was supported by the 2016 Yeungnam University Research Grant.
REFERENCES
- 1.Gallichio JE: Pharmacologic management of spasticity following stroke. Phys Ther, 2004, 84: 973–981. [PubMed] [Google Scholar]
- 2.Karakoyun A, Boyraz İ, Gunduz R, et al. : Electrophysiological and clinical evaluation of the effects of transcutaneous electrical nerve stimulation on the spasticity in the hemiplegic stroke patients. J Phys Ther Sci, 2015, 27: 3407–3411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Keenan MA: The management of spastic equinovarus deformity following stroke and head injury. Foot Ankle Clin, 2011, 16: 499–514. [DOI] [PubMed] [Google Scholar]
- 4.Kaplan PE: Rehabilitation of stroke. Burlington: Butterworth-Heinemann, 2003, pp 158–159. [Google Scholar]
- 5.Jang SH, Ahn SH, Park SM, et al. : Alcohol neurolysis of tibial nerve motor branches to the gastrocnemius muscle to treat ankle spasticity in patients with hemiplegic stroke. Arch Phys Med Rehabil, 2004, 85: 506–508. [DOI] [PubMed] [Google Scholar]
- 6.Kong KH, Chua KS: Intramuscular neurolysis with alcohol to treat post-stroke finger flexor spasticity. Clin Rehabil, 2002, 16: 378–381. [DOI] [PubMed] [Google Scholar]
- 7.Lee DG, Jang SH: Ultrasound guided alcohol neurolysis of musculocutaneous nerve to relieve elbow spasticity in hemiparetic stroke patients. NeuroRehabilitation, 2012, 31: 373–377. [DOI] [PubMed] [Google Scholar]
- 8.Bohannon RW, Smith MB: Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther, 1987, 67: 206–207. [DOI] [PubMed] [Google Scholar]
- 9.Jang SH, Choi BY, Chang CH, et al. : Prediction of motor outcome based on diffusion tensor tractography findings in thalamic hemorrhage. Int J Neurosci, 2013, 123: 233–239. [DOI] [PubMed] [Google Scholar]
- 10.Son SM, Park IS, Yoo JS: Short-term effect of botulinum toxin a injection on spastic equinovarus foot in cerebral palsy patients: a study using the foot pressure measurement system. Ann Rehabil Med, 2015, 39: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davies H: Metatarsus quintus valgus. BMJ, 1949, 1: 664–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ajis A, Koti M, Maffulli N: Tailor’s bunion: a review. J Foot Ankle Surg, 2005, 44: 236–245. [DOI] [PubMed] [Google Scholar]
- 13.Tupimai T, Peungsuwan P, Prasertnoo J, et al. : Effect of combining passive muscle stretching and whole body vibration on spasticity and physical performance of children and adolescents with cerebral palsy. J Phys Ther Sci, 2016, 28: 7–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.You YY, Her JG, Woo JH, et al. : The effects of stretching and stabilization exercise on the improvement of spastic shoulder function in hemiplegic patients. J Phys Ther Sci, 2014, 26: 491–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Monaghan K, Horgan F, Blake C, et al. : Physical treatment interventions for managing spasticity after stroke. Cochrane Database Syst Rev, 2011, 7: 1–25. [Google Scholar]
- 16.Chang CH, Miller F, Schuyler J: Dynamic pedobarograph in evaluation of varus and valgus foot deformities. J Pediatr Orthop, 2002, 22: 813–818. [PubMed] [Google Scholar]
- 17.Park ES, Kim HW, Park CI, et al. : Dynamic foot pressure measurements for assessing foot deformity in persons with spastic cerebral palsy. Arch Phys Med Rehabil, 2006, 87: 703–709. [DOI] [PubMed] [Google Scholar]


