Abstract
Objectives
To study the patterns of weight change after spinal cord injury (SCI) and identify associated risk factors.
Study design
Cohort study.
Setting
Sixteen Spinal Cord Injury Model Systems (SCIMS), USA.
Participants
One thousand and ninety-four individuals with an SCI who were entered into the SCIMS and had a 1-year follow-up between October 2006 and November 2012.
Intervention
Not applicable.
Outcome measure
Change in body mass index (BMI) during the first year of injury. Height and weight were assessed during inpatient rehabilitation and 1 year after injury.
Results
Mean BMI decreased from 26.3 to 25.8 kg/m² during the first year after SCI (mean change: −0.5 kg/m² (standard deviation: 3.58)). Weight loss was mainly observed among individuals classified as overweight or obese during rehabilitation (n = 576) with a BMI decrease of 1.4 kg/m², which varied significantly by sex, education, neurological level, and the presence of vertebral injury. Weight gain was noted among individuals classified as underweight or normal weight during rehabilitation (n = 518) with a BMI increase of 0.5 kg/m², with the greatest increase among individuals of Hispanic origin (1.2 kg/m²), other marital status (1.2 kg/m²), age group 31–45 years (1.1 kg/m²), with less than high school education (1.1 kg/m²), without spinal surgery (0.9 kg/m²), and with motor functionally incomplete injury (0.8 kg/m²).
Conclusion
Our findings suggest that strategies for weight management should be addressed after a SCI to ameliorate the potential for unhealthful weight change, particularly among at-risk groups.
Keywords: Spinal cord injury, Body mass index, Obesity, Rehabilitation
Introduction
Individuals with disabilities have a higher prevalence of obesity than the general population.1 The prevalence of overweight and obesity in individuals with spinal cord injury (SCI) varies between 40 and 66% defined by body mass index (BMI).2 When compared to able-bodied persons, persons with SCI carry ∼13% more fat for any given BMI.3 Obesity has been linked to an increased risk of cardiovascular and metabolic disease, which may be higher and occur at a younger age in individuals with SCI.4,5 The cardiovascular mortality rate for individuals with SCI is also estimated to be higher than able-bodied individuals.6
Immediately following a SCI, individuals experience weight loss due to increased metabolic demand related to severe trauma.7 Infection, decreased caloric intake, and psychological factors, such as adjustment disorder and depression, are factors that may also contribute to weight loss after SCI. In clinical practice, patients are often encouraged to increase their caloric intake to offset the injury–stress response, but may not be adequately counseled on appropriate nutrition and weight control after stabilization of their injury. However, within the first year of SCI, there is a decrease in the caloric needs of individuals with SCI secondary to a lowering of the basal metabolic rate, which increases their risk for obesity.8 A 2% imbalance between intake and energy expenditure may result in a weight increase of 20–30 kg over a decade, which has been associated with an increase in chronic disease.9
Obesity may introduce additional barriers such as increased lack of mobility, decreased independence, and a lack of community integration, which may all lead to a decreased quality of life. Obesity has also been linked as a risk factor for pressure ulcers, urinary tract infections, pain, and spasticity, which are all common medical complications following a SCI.10 Obesity also impedes the caregiver's ability to assist with activities of daily living such as toileting, bathing, dressing, and transfers, thus impacting overall quality of care.11
There is a limited literature on weight change after SCI, and more specifically, factors associated with patterns of weight gain or loss after SCI. Two studies have examined the prospective trend of BMI during the first 5 years after injury.12,13 Crane et al. observed a mean increase in BMI of 2.3 kg/m2 by 5 years post-injury among 85 men and 1 female with SCI. For participants who had a mean increase in BMI >2.0 kg/m2 at 5 years post-injury, the mean change in BMI during the first year was 1.1 kg/m2. In a study by de Groot et al.,13 a mean increase in BMI of 0.96 kg/m2 was observed from discharge from rehabilitation to 1 year after discharge among 144 individuals with SCI. Our objective was to study the patterns of weight change 1-year post-SCI and to identify any factors associated with weight change, using data from the largest National Spinal Cord Injury Database.
Methods
Data were retrieved from 16 Spinal Cord Injury Model Systems (SCIMS) within the National Spinal Cord Injury Database. Variables include demographics, injury and medical characteristics, psychosocial wellbeing, and functional independence measures obtained during the initial hospitalization and at years 1, 5, and every 5 years post-injury. This database is believed to capture data from ∼13% of new SCI cases each year. Details about this database have been described elsewhere.14 The Institutional Review Board at each Model System site approved the research study.
This study was limited to participants with a traumatic SCI who were older than 17 years and discharged between October 2006 and November 2012 (n = 3961), when height and weight were collected. Participants were excluded if there was no documentation of weight and height during rehabilitation (n = 11) as well as at 1-year follow-up for various reasons including: no 1-year follow-up (n = 513); deceased before follow-up (n = 122), neurological recovery within first year (n = 18); had not attended follow-up visit to date (n = 741); and/or weight not obtained at follow-up contact (n = 1462). Our final analytical sample was 1094.
Dependent variable
The primary outcome measure was BMI change (relative weight change) during the first year after SCI. Weight was assessed on a wheelchair-accessible scale with study participants wearing light clothing at admission to rehabilitation and during the year 1 follow-up visit. Height was measured in a supine position with legs outstretched and feet in dorsiflexion or by participant self-report during rehabilitation. BMI (kg/m2) was used to determine weight status according to the National Heart, Lung, and Blood Institute (NHLBI)15 guidelines: underweight (<18.5), normal (18.5–24.9), overweight (25.0–29.9), and obese (≥30.0).
Independent variables
Trained personnel obtained demographic and medical information during the initial hospitalization. Level and completeness of injury were assessed at discharge from the initial hospitalization with the International Standards for Neurological Classification of Spinal Cord Injury.16 For this analysis, participants were grouped into one of the three categories according to AIS level: tetraplegia with AIS A, B, or C (Tetra ABC); paraplegia with AIS A, B, or C (Para ABC); and AIS D and E (AIS DE). Based on the International SCI Data Standards,17 vertebral injury was defined as any break, rupture, or crack in any bone that is a part of the vertebral column from the occiput to the coccyx. Spinal surgery referred to laminectomy, spinal decompression, spinal fusion, or internal fixation of the spine. Associated injury referred to the presence of any of the following injuries occurring at the time of SCI: traumatic brain injury (Glasgow Coma Scale ≤12), non-vertebral fractures, severe facial injuries affecting sense organs, traumatic amputations of an arm or leg, severe hemorrhaging, or damage to any internal organ requiring surgery. The occurrence of any unplanned hospitalization after discharge from initial hospital care was documented at year 1 follow-up.
Statistical analysis
Mean and standard deviation (SD) was used to summarize the BMI values at admission to rehabilitation, BMI values at year 1, and BMI changes between rehabilitation and year 1 across demographic and clinical characteristics. Comparisons of BMI values and changes across participant characteristics were examined by the analysis of variance. BMI change between the initial and year 1 assessment within each group was determined by a paired t-test. Multiple regression analysis was used to identify factors that independently contributed to weight change. To examine the influence of baseline weight status on the change in BMI during the first year after injury, the above analyses were further stratified by the baseline BMI (<25 and ≥25 kg/m2). Statistical significance was set at P < 0.05.
Selection bias
To assess potential selection bias, we examined differences between included and excluded participants. There were no statistically significant differences between the excluded (n = 2867) and included participants (n = 1094) in terms of sex, race/ethnicity, marital status, education, and baseline BMI (Table 1). However, study participants were younger (40.9 vs. 43.6), had a higher employment rate (61.9 vs. 57.9%), and had more severe injuries (American Spinal Injury Association Impairment Scale (AIS) D and E: 33.7 vs. 37.1%), as well as were more likely to be students or trainees (9.4 vs. 7.2%), compared to excluded participants.
Table 1.
Comparison of demographic characteristics between study participants and non-participants
| Characteristics | Participants (N = 1094) | Non-participants (N = 2867) | P value | |
|---|---|---|---|---|
| Age at injury (years), mean (SD) | 40.9 (16.9) | 43.6 (18.3) | <0.01 | |
| Baseline BMI (kg/m2), mean (SD) | 26.3 (6.0) | 26.6 (6.4) | 0.11 | |
| Sex, n (%) | ||||
| Female | 212 (19.4) | 620 (21.8) | 0.10 | |
| Male | 881 (80.6) | 2229 (78.2) | ||
| Race/ethnicity, n (%) | ||||
| White | 693 (63.6) | 1693 (61.2) | 0.05 | |
| Black | 287 (26.3) | 711 (25.7) | ||
| Hispanic | 81 (7.4) | 248 (8.9) | ||
| Other | 29 (2.7) | 116 (4.2) | ||
| Marital status, n (%) | ||||
| Single | 484 (44.3) | 1248 (44.1) | 0.54 | |
| Married | 441 (40.3) | 1106 (39.1) | ||
| Other | 168 (15.4) | 474 (16.8) | ||
| Education, n (%) | ||||
| Less than high school | 175 (16.5) | 462 (18.2) | 0.18 | |
| High school | 621 (58.6) | 1407 (55.3) | ||
| College or higher | 263 (24.8) | 675 (26.5) | ||
| Occupation, n (%) | ||||
| Employed | 675 (61.9) | 1641 (57.9) | <0.01 | |
| Student or trainee | 102 (9.4) | 204 (7.2) | ||
| Other | 314 (28.8) | 987 (34.9) | ||
| Neurological impairment, n (%) | ||||
| AIS DE | 365 (33.7) | 970 (37.1) | 0.03 | |
| Para ABC | 387 (35.7) | 818 (31.3) | ||
| Tetra ABC | 332 (30.6) | 829 (31.7) | ||
Results
Sample characteristics
Baseline BMI of the 1094 participants averaged 26.3 kg/m2 (SD: 5.98), (weight: 81.6 kg (SD: 19.47)), which varied significantly by age, sex, marital status, education, occupation, neurological impairment, as well as by the presence of vertebral injury and associated injury (P < 0.05, Table 2). The average BMI measured at 1-year post-injury was 25.8 kg/m2 (SD: 5.79), (weight 80.1 kg (SD: 19.14)), which also differed significantly by age, marital status, occupation, neurological impairment, and the presence of vertebral injury (P < 0.05).
Table 2.
Change in BMI during the first year of injury
| Participants (N) | BMI during rehabilitation (kg/m2) | BMI at year 1 (kg/m2) | BMI change (kg/m2) | P value for BMI change | P value* | Adjusted P value** | |
|---|---|---|---|---|---|---|---|
| Overall | 1094 | 26.3 (5.98) | 25.8 (5.79) | −0.48 | <0.01 | – | – |
| Age | |||||||
| 18–30 | 403 | 24.2 (5.52)a | 23.8 (5.36)b | −0.41 | 0.02 | 0.12 | 0.08 |
| 31–45 | 234 | 27.1 (5.87) | 26.8 (5.58) | −0.24 | 0.35 | ||
| 46–60 | 301 | 27.9 (6.27) | 27.5 (6.05) | −0.44 | 0.04 | ||
| 61–88 | 156 | 27.5 (5.18) | 26.4 (5.14) | −1.10 | <0.01 | ||
| Sex | |||||||
| Male | 881 | 26.1 (5.68)a | 25.7 (5.65) | −0.44 | <0.01 | 0.38 | <0.01 |
| Female | 212 | 27.1 (7.07) | 26.5 (6.32) | −0.68 | 0.01 | ||
| Race/ethnicity | |||||||
| White | 693 | 26.5 (5.81) | 25.9 (5.72) | −0.61 | <0.01 | 0.33 | 0.70 |
| Black | 287 | 25.9 (6.14) | 25.6 (5.77) | −0.25 | 0.32 | ||
| Hispanic | 81 | 26.3 (6.51) | 26.3 (6.10) | −0.03 | 0.78 | ||
| Other | 29 | 25.2 (7.02) | 24.5 (6.46) | −0.68 | 0.22 | ||
| Marital status | |||||||
| Single | 484 | 24.8 (5.40)a | 24.4 (5.34)b | −0.40 | 0.01 | 0.02 | 0.04 |
| Married | 441 | 27.7 (6.30) | 26.9 (5.89) | −0.78 | <0.01 | ||
| Other | 168 | 27.0 (5.70) | 27.1 (5.85) | 0.09 | 0.69 | ||
| Education | |||||||
| Less than high school | 175 | 25.3 (6.39)a | 27.2 (5.58) | −0.16 | 0.51 | <0.01 | 0.06 |
| High school | 621 | 26.1 (5.98) | 25.8 (5.85) | −0.29 | 0.06 | ||
| College or higher | 263 | 27.1 (5.42) | 26.1 (5.57) | −1.03 | <0.01 | ||
| Occupation | |||||||
| Employed | 675 | 26.7 (6.09)a | 26.3 (5.87)b | −0.42 | <0.01 | 0.65 | 0.58 |
| Student or trainee | 102 | 23.6 (4.97) | 23.2 (4.98) | −0.41 | 0.17 | ||
| Other | 314 | 26.4 (5.85) | 25.8 (5.63) | −0.64 | <0.01 | ||
| Neurological level | 0.11 | 0.03 | |||||
| AIS DE | 365 | 27.1 (5.77)a | 26.9 (5.59)b | −0.26 | 0.09 | ||
| Para ABC | 387 | 25.9 (5.79) | 25.5 (5.97 | −0.42 | 0.02 | ||
| Tetra ABC | 332 | 25.9 (6.40) | 25.0 (5.68) | −0.82 | <0.01 | ||
| Vertebral injury | |||||||
| Yes | 865 | 26.0 (5.80)a | 25.4 (5.62)b | −0.53 | <0.01 | 0.39 | 0.15 |
| No | 226 | 27.7 (6.50) | 27.3 (6.21) | −0.30 | 0.20 | ||
| Associated injury | |||||||
| Yes | 476 | 25.9 (6.01)a | 25.5 (5.84) | −0.43 | 0.02 | 0.65 | 0.58 |
| No | 615 | 26.6 (5.96) | 26.1 (5.75) | −0.53 | <0.01 | ||
| Spinal surgery | |||||||
| Yes | 842 | 26.4 (6.01) | 26.0 (5.82) | −0.6 | <0.01 | 0.20 | 0.91 |
| No | 248 | 25.8 (5.91) | 25.6 (5.72) | −0.2 | 0.30 | ||
| Rehospitalization | |||||||
| Yes | 687 | 26.6 (5.96) | 25.9 (5.87) | −0.7 | <0.01 | 0.14 | 0.57 |
| No | 383 | 26.2 (6.05) | 25.8 (5.79) | −0.4 | <0.01 | ||
aP < 0.05, comparison of baseline BMI across groups.
bP < 0.05, comparison of BMI at year 1 across groups.
*Comparison of BMI changes across groups.
**Comparison of BMI changes across groups, after adjusting for baseline weight and listed variables.
During the first year after injury, 209 (19.1%) participants maintained their weight (loss or gain of <2 kg), 365 (33.4%) participants gained >2 kg, while 47.5% of the participants (n = 530) lost >2 kg (Fig. 1). At baseline, 4.1, 31.2, and 21.5% of study participants were classified as underweight, overweight, and obese, respectively. These measurements changed to 6.7% underweight, 30.5% overweight, and 20.0% obese at year 1. The majority of study participants (61.5%) fell into the same BMI categories between rehabilitation and year 1 follow-up (Table 3). However, of the 473 normal-weight participants at rehabilitation, 90 (19.0%) became overweight, 11 (2.3%) became obese, and 44 (9.3%) became underweight at 1-year follow-up.
Figure 1.
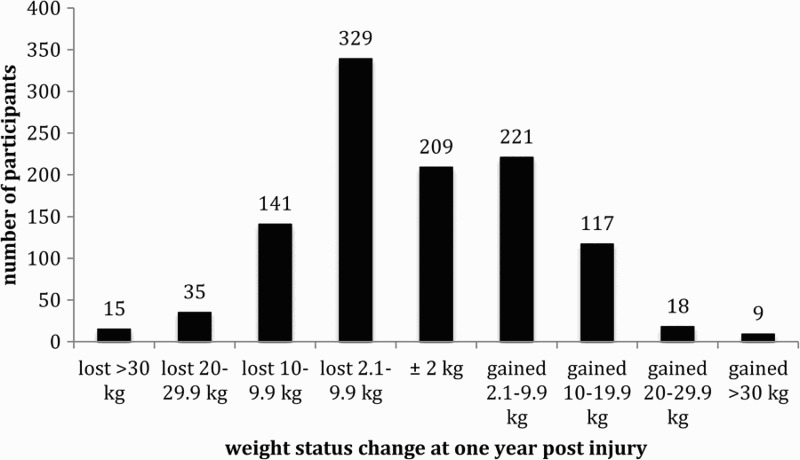
Participant weight loss and gain at 1-year follow-up.
Table 3.
Comparison of weight status at baseline and 1-year follow-up
| 1-year post-injury weight status |
|||||
|---|---|---|---|---|---|
| Baseline weight status | Underweight | Normal | Overweight | Obese | Total |
| Underweight | 22 | 22 | 1 | 0 | 45 |
| Normal | 44 | 328 | 90 | 11 | 473 |
| Overweight | 6 | 108 | 171 | 56 | 341 |
| Obese | 1 | 10 | 72 | 152 | 235 |
| Total | 73 | 468 | 334 | 219 | 1094 |
Overweight and obese at baseline
As shown in Table 2, the average change in BMI during the first year after injury was −0.5 kg/m2 (SD: 3.58); (weight: −1.5 kg (range −50 to 64.6)). The weight loss, however, was mainly observed among individuals classified as overweight and obese (BMI ≥ 25 kg/m2) during rehabilitation (Table 4), with BMI decrease by 1.4 kg/m2, from 30.5 kg/m2 during rehabilitation to 29.1 kg/m2 at 1-year post-injury (P < 0.0001). The decrease in BMI among overweight and obese participants was noted regardless of age, race/ethnicity, sex, education, occupation, neurological level, and the presence of vertebral injury, associated injury, spinal surgery, and rehospitalization, but not other marital status (divorced, widowed, etc.; −0.66 kg/m2, P = 0.12). The non-significant BMI change for the other race/ethnic groups (Native Americans, Asian, etc.; −1.34 kg/m2, P = 0.14) was likely due to a small sample size (n = 12).
Table 4.
Change in BMI during the first year of injury among 576 individuals classified as overweight and obese during rehabilitation (BMI ≥ 25 kg/m2)
| N | BMI during rehabilitation (kg/m2) | BMI at year 1 (kg/m2) | BMI change (kg/m2) | P value for BMI change | P value* | Adjusted P value** | |
|---|---|---|---|---|---|---|---|
| Overall | 30.5 (5.17)a | 29.1 (5.44)b | −1.35 | <0.01 | – | – | |
| Age | |||||||
| 18–30 | 143 | 29.6 (5.66)a | 27.9 (5.73)b | −1.61 | <0.01 | 0.46 | 0.41 |
| 31–45 | 135 | 30.7 (5.03) | 29.5 (5.12) | −1.25 | <0.01 | ||
| 46–60 | 192 | 31.3 (5.33) | 30.2 (5.61) | −1.06 | <0.01 | ||
| 61–88 | 106 | 30.0 (4.06) | 28.3 (4.67) | −1.68 | <0.01 | ||
| Sex | |||||||
| Male | 108 | 30.0 (4.89)a | 28.8 (5.41)b | −1.25 | <0.01 | 0.13 | 0.0003 |
| Female | 467 | 32.5 (5.87) | 30.6 (5.33) | −1.86 | <0.01 | ||
| Race/ethnicity | |||||||
| White | 385 | 30.3 (5.00) | 28.9 (5.33) | −1.36 | <0.01 | 1.00 | 0.96 |
| Black | 136 | 30.8 (5.26) | 29.5 (5.28) | −1.30 | <0.01 | ||
| Hispanic | 39 | 31.3 (6.03) | 29.9 (6.12) | −1.32 | 0.06 | ||
| Other | 12 | 31.0 (7.29) | 29.7 (7.07) | −1.34 | 0.14 | ||
| Marital status | |||||||
| Single | 193 | 29.9 (4.50) | 28.6 (5.04) | −1.34 | <0.01 | 0.11 | 0.17 |
| Married | 283 | 30.9 (5.61) | 29.3 (5.62) | −1.61 | <0.01 | ||
| Other | 99 | 30.4 (5.02) | 29.8 (5.62) | −0.66 | 0.12 | ||
| Education | |||||||
| <High school | 71 | 30.6 (6.77) | 28.7 (5.92) | −1.97 | <0.01 | 0.11 | 0.02 |
| High school | 313 | 30.6 (5.06) | 29.5 (5.29) | −1.06 | <0.01 | ||
| ≥College | 165 | 30.1 (4.47) | 28.5 (5.30) | −1.61 | <0.01 | ||
| Occupation | |||||||
| Employed | 378 | 30.5 (5.33) | 29.4 (5.52) | −1.17 | <0.01 | 0.27 | 0.24 |
| Student/trainee | 29 | 29.4 (5.45) | 27.7 (5.66) | −1.62 | <0.01 | ||
| Other | 168 | 30.6 (4.74) | 28.9 (5.20) | −1.73 | <0.01 | ||
| Neurological level | |||||||
| AIS DE | 220 | 30.5 (4.76) | 29.6 (4.98) | −0.95 | <0.01 | <0.01 | <0.01 |
| Para ABC | 194 | 30.2 (4.93) | 29.2 (5.69) | −1.07 | <0.01 | ||
| Tetra ABC | 157 | 30.7 (6.01) | 28.4 (5.75) | −2.32 | <0.01 | ||
| Vertebral injury | |||||||
| Yes | 143 | 30.3 (5.07) | 28.8 (5.35)b | −1.50 | <0.01 | 0.11 | 0.02 |
| No | 431 | 31.1 (5.44) | 30.2 (5.59) | −0.91 | <0.01 | ||
| Associated injury | |||||||
| Yes | 228 | 30.7 (5.07) | 29.2 (5.41) | −1.49 | <0.01 | 0.49 | 0.66 |
| No | 346 | 30.4 (5.24) | 29.1 (5.47) | −1.26 | <0.01 | ||
| Spinal surgery | |||||||
| Yes | 448 | 30.6 (5.24) | 29.2 (5.40) | −1.36 | <0.01 | 0.91 | 0.29 |
| No | 125 | 30.2 (4.93) | 28.9 (5.58) | −1.32 | <0.01 | ||
| Rehospitalization | |||||||
| Yes | 206 | 30.8 (4.92) | 29.0 (5.44) | −1.76 | <0.01 | 0.07 | 0.39 |
| No | 357 | 30.4 (5.36) | 29.2 (5.48) | −1.16 | <0.01 | ||
aP < 0.05, comparison of BMI during rehabilitation across groups.
bP < 0.05, comparison of BMI at year 1 across groups.
*Comparison of BMI changes across groups.
**Comparison of BMI changes across groups, after adjusting for baseline weight and listed variables.
After accounting for baseline weight and participant characteristics, the degree of weight loss among overweight and obese participants differed significantly by sex, education, neurological level, and the presence of vertebral injury (Table 4). Weight loss was significantly greater for females than males (−1.86 vs. −1.25 kg/m2, P = 0.0003); for those having less than high school education or having a college or higher education vs. high school graduates (−1.97, −1.61, vs. −1.06 kg/m2, P = 0.02); and for those with vertebral injury vs. without vertebral injury (−1.50 vs. −0.91, P = 0.02). The Tetra ABC group had the largest BMI change (−2.32 kg/m2), followed by the Para ABC (−1.07 kg/m2) and AIS DE (−0.95 kg/m2) (P = 0.007).
Normal and underweight at baseline
Individuals with baseline BMI <25 kg/m2 gained weight during the first year after injury by 0.5 kg/m2, increasing from 21.7 kg/m2 during rehabilitation to 22.2 kg/m2 at 1-year post-injury (Table 5; P = 0.0002). The increase in BMI was noted across demographic and clinical characteristics, except for other race/ethnicity (−0.22 kg/m2, P = 0.70) and those with some college education (−0.06 kg/m2, P = 0.81). BMI change was not statistically significant for the 18–30 year or 61–88 year age groups, females, single marital status, students, or Para ABC injuries. The greatest increase in BMI was noted among individuals of Hispanic origin (1.16 kg/m2), of other marital status (1.15 kg/m2), in age group 31–45 years (1.14 kg/m2), with less than high school education (1.08 kg/m2), without spinal surgery (0.89 kg/m2), and with AIS DE injuries (0.79 kg/m2). The degree of weight gain varied significantly by age and marital status, after adjusting for baseline weight, demographics, and clinical characteristics.
Table 5.
Change in BMI during the first year of injury among 518 individuals classified as underweight and normal weight during rehabilitation (BMIE < 25 kg/m2)
| N | BMI during rehabilitation (kg/m2) | BMI at year 1 (kg/m2) | BMI change (kg/m2) | P value for BMI change | P value* | Adjusted P value** | |
|---|---|---|---|---|---|---|---|
| Overall | 21.7 (2.23) | 22.2 (3.52) | 0.49 | <0.01 | – | – | |
| Age | |||||||
| 18–30 | 260 | 21.3 (2.31)a | 21.5 (3.46)b | 0.24 | 0.17 | 0.06 | 0.05 |
| 31–45 | 99 | 22.1 (2.11) | 23.3 (3.96) | 1.14 | <0.01 | ||
| 46–60 | 109 | 22.0 (2.00) | 22.7 (3.06) | 0.66 | 0.01 | ||
| 61–88 | 50 | 22.0 (2.24) | 22.1 (3.16) | 0.13 | 0.78 | ||
| Sex | |||||||
| Male | 414 | 21.7 (2.22) | 22.2 (3.42) | 0.48 | <0.01 | 0.83 | 0.77 |
| Female | 104 | 21.6 (2.28) | 22.1 (3.89) | 0.55 | 0.13 | ||
| Race/ethnicity | |||||||
| White | 308 | 21.8 (2.22) | 22.1 (3.54) | 0.34 | 0.05 | 0.20 | 0.69 |
| Black | 151 | 21.4 (2.24) | 22.1 (3.53) | 0.71 | <0.01 | ||
| Hispanic | 42 | 21.7 (2.04) | 22.9 (3.66) | 1.16 | 0.02 | ||
| Other | 17 | 21.1 (2.56) | 20.9 (2.13) | −0.22 | 0.70 | ||
| Marital status | |||||||
| Single | 291 | 21.3 (2.34)a | 21.5 (3.28)b | 0.22 | 0.16 | 0.04 | 0.05 |
| Married | 158 | 22.1 (2.08) | 22.8 (3.62) | 0.70 | 0.01 | ||
| Other | 69 | 22.2 (1.76) | 23.4 (3.74) | 1.15 | <0.01 | ||
| Education | |||||||
| <High school | 104 | 21.7 (2.28) | 22.8 (3.82) | 1.08 | <0.01 | 0.03 | 0.08 |
| High school | 308 | 21.6 (2.25) | 22.1 (3.55) | 0.50 | <0.01 | ||
| ≥College | 98 | 22.0 (2.06) | 21.9 (3.06) | −0.06 | 0.81 | ||
| Occupation | |||||||
| Employed | 297 | 21.8 (2.29) | 22.3 (3.48) | 0.54 | <0.01 | 0.43 | 0.94 |
| Student/trainee | 73 | 21.3 (2.09) | 21.4 (3.27) | 0.08 | 0.83 | ||
| Other | 146 | 21.6 (2.15) | 22.2 (3.70) | 0.62 | 0.02 | ||
| Neurologic level | |||||||
| AIS DE | 145 | 21.9 (2.16) | 22.7 (3.56) | 0.79 | <0.01 | 0.24 | 0.10 |
| Para ABC | 193 | 21.6 (2.27) | 21.8 (3.45) | 0.23 | 0.27 | ||
| Tetra ABC | 175 | 21.5 (2.23) | 22.0 (3.51) | 0.52 | 0.03 | ||
| Vertebral injury | |||||||
| Yes | 434 | 21.7 (2.21) | 22.1 (3.54) | 0.44 | <0.01 | 0.37 | 0.77 |
| No | 83 | 21.5 (2.32) | 22.3 (3.40) | 0.77 | 0.02 | ||
| Associated injury | |||||||
| Yes | 248 | 21.5 (2.28) | 22.0 (3.76) | 0.55 | <0.01 | 0.62 | 0.79 |
| No | 269 | 21.8 (2.17) | 22.2 (3.26) | 0.42 | 0.01 | ||
| Spinal surgery | |||||||
| Yes | 394 | 21.8 (2.16) | 22.1 (3.54) | 0.36 | 0.02 | 0.09 | 0.12 |
| No | 123 | 21.3 (2.42) | 22.2 (3.43) | 0.89 | <0.01 | ||
| Rehospitalization | |||||||
| Yes | 144 | 21.7 (2.14) | 22.3 (3.93) | 0.52 | 0.04 | 0.89 | 0.96 |
| No | 330 | 21.6 (2.29) | 22.1 (3.31) | 0.49 | <0.01 | ||
aP < 0.05, comparison of BMI during rehabilitation across groups.
bP < 0.05, comparison of BMI at year 1 across groups.
*Comparison of BMI changes across groups.
**Comparison of BMI changes across groups, after adjusting for baseline weight and listed variables.
Discussion
The present study of 1094 participants with baseline BMI of 26.3 kg/m2 shows a decrease in BMI by 0.5 kg/m2 at 1 year after SCI, particularly among those classified as overweight and obese during rehabilitation (n = 576, baseline BMI = 30.5 kg/m2, BMI change = −1.4 kg/m2). In contrast, individuals with baseline BMI<25 kg/m2 (n = 518, baseline BMI = 22.2 kg/m2) gained weight during the first year after SCI by 0.5 kg/m2. Previous research conducted in the Netherlands13 with a smaller sample size (N = 144) and lower overall BMI (23.6 kg/m2) showed a BMI increase of 0.9 kg/m2 between discharge from rehabilitation (median days since injury = 266) and 1 year after discharge (median days since injury = 631), which is similar to our finding among participants with baseline BMI <25 kg/m2, although the follow-up period is not exactly comparable.
Similar to previous research showing a higher prevalence of overweight and obesity in older individuals with SCI,18 the Netherlands study reported age as the only factor related to absolute BMI, projecting a BMI increase by 1 kg/m2 for every 10-year increase in age between age 20 and 69 years, while the change in BMI over time was not different by age, sex, and neurological lesion. Our study shows age variation in absolute BMI at baseline as well as at 1-year follow-up, with the lowest BMI among the 18–30 year group and highest BMI among the 46–60 year group. Interestingly, we observed that individuals age 61 or older with a BMI <25 kg/m2 had the smallest weight gain compared to the other age groups (0.1 kg/m2) and those with a BMI ≥25 had the largest weight loss (1.68 kg/m2). This finding is likely explained by the fact that when older adults are subjected to acute inactivity, such as bed rest they tend to experience an accelerated loss of muscle mass at a higher rate than immobile younger individuals.19
Previous investigation of individuals with chronic SCI suggests that the prevalence of overweight and obesity is higher in people with paraplegia compared to those with tetraplegia.3,20 This may be due to the higher density of lean body tissue compared to fat tissue.3 Spungen et al. measured body composition using dual-energy X-ray absorptiometry and reported that paraplegics had a higher amount of lean tissue (45.9 kg ± 0.09) compared to tetraplegics (42.2 kg ± 1.00).3 Another explanation may be that paraplegics tend to have more independence with meal preparation and feeding than tetraplegics. We observed that individuals with an AIS DE had a higher absolute BMI during rehabilitation and at 1-year post-injury compared to the other neurological groups. These participants also lost the least weight among participants with a baseline BMI ≥25 kg/m2 and gained the most weight among those with a BMI <25 kg/m2, as compared with their neurological counterparts. Our findings suggest that as neurological impairment improves there is a higher propensity for weight gain. The factors mentioned above may explain the trend of increasing BMI with greater neurological function, which needs further confirmation by long-term follow-up.
Our results showed a wide range in weight change during the first year after SCI, from losing 50 kg to gaining 65 kg. However, only a small proportion of the variance in relative weight change can be explained by baseline weight, demographics, and clinical characteristics of study participants (R2 = 0.15). The observed differences in weight change based on baseline BMI category may be due to overweight and obese individuals having more reserves to lose, intentional weight loss, or both. In contrast, normal weight and underweight individuals may have received excessive supplemental nutrition post-injury. Further research is needed to identify risk factors that contribute to detrimental weight change within a year after SCI, including but not limited to nutrition, physical activity, adjustment disorder, depression, and family support. Our study findings may aid in the early identification of the at-risk groups for detrimental weight change, such as potential weight gain for AIS DE injuries as well as persons of age 31–45 years, Hispanic ethnicity, other marital status, and less than high school education.
A major limitation to our research study is the lack of body composition assessment. Unfortunately, the SCIMS does not collect information on body composition. This valuable information would have allowed us to evaluate the loss or gain of fat and fat-free mass during the first year after injury. Exclusion of 2867 individuals may have introduced selection bias into our study and therefore limit the generalizability of our study findings to the SCI population at large. The present study obtained baseline body weight during rehabilitation, but not at the time of injury, which limits our understanding of weight change after SCI. Also, the use of measured and self-reported height could lead to potential misclassification of weight status. Nonetheless, the large and diverse sample derived from the SCIMS standardized database is the strength of this study. To our knowledge, this study is the largest to date conducted to characterize weight change after SCI by demographic and clinical factors.
Conclusion
Our findings confirm that individuals with SCI will initially lose weight. However, some individuals may continue to lose weight and consequently become underweight, while others may gain extreme amounts of weight following rehabilitation. Therefore, healthcare professionals need to recognize that strategies for appropriate nutrition and physical activity need to be addressed during rehabilitation and subsequent outpatient clinic visits to alleviate the potential for detrimental weight change as early as during the first year after injury. Future research is needed to identify predictors of underweight and obesity development after SCI and to improve physician recognition of potentially harmful patterns of weight change.
Disclaimer statements
Contributors DP conceived and designed the study, interpreted data, wrote part of the article, and revised article; OA interpreted data, wrote part of the article, and revised article; and YC designed study, analyzed data, interpreted data, wrote part of the article, and revised article.
Funding This research was supported by the National Institute on Disability and Rehabilitation Research, Office of Special Education and Rehabilitation Services, United States Department of Education, Washington, DC (grant no. H133A110002).
Conflicts of interest None.
Ethics approval The paper received approved for the IRB at the University of Alabama at Birmingham.
References
- 1.Weil E, Wachterman M, McCarthy EP, Davis RB, O'Day B, Iezzoni LI, et al. . Obesity among adults with disabling conditions. JAMA 2002;288(10):1265–8. [DOI] [PubMed] [Google Scholar]
- 2.Chen Y, Cao Y, Allen V, Richards JS. Weight matters: physical and psychosocial well being of persons with spinal cord injury in relation to body mass index. Arch Phys Med Rehabil 2011;92(3):391–8. [DOI] [PubMed] [Google Scholar]
- 3.Spungen AM, Adkins RH, Stewart CA, Wang J, Pierson RN Jr, Waters RL, et al. . Factors influencing body composition in persons with spinal cord injury: a cross-sectional study. J Appl Physiol (1985) 2003;95(6):2398–407. [DOI] [PubMed] [Google Scholar]
- 4.Yekutiel M, Brooks ME, Ohry A, Yarom J, Carel R. The prevalence of hypertension, ischaemic heart disease and diabetes in traumatic spinal cord injured patients and amputees. Paraplegia 1989;27(1):58–62. [DOI] [PubMed] [Google Scholar]
- 5.Bauman WA, Spungen AM, Raza M, Rothstein J, Zhang RL, Zhong YG, et al. . Coronary artery disease: metabolic risk factors and latent disease in individuals with paraplegia. Mt Sinai J Med 1992;59(2):163–8. [PubMed] [Google Scholar]
- 6.Whiteneck GG, Charlifue SW, Frankel HL, Fraser MH, Gardner BP, Gerhart KA, et al. . Mortality, morbidity, and psychosocial outcomes of persons spinal cord injured more than 20 years ago. Paraplegia 1992;30(9):617–30. [DOI] [PubMed] [Google Scholar]
- 7.Thibault-Halman G, Casha S, Singer S, Christie S. Acute management of nutritional demands after spinal cord injury. J Neurotrauma 2009;28(8):1497–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cox SA, Weiss SM, Posuniak EA, Worthington P, Prioleau M, Heffley G. Energy expenditure after spinal cord injury: an evaluation of stable rehabilitating patients. J Trauma 1985;25(5):419–23. [PubMed] [Google Scholar]
- 9.Saltzmann E, Roberts SB. The role of energy expenditure in energy regulation: findings from a decade of research. Nutr Rev 1995;53(8):209–20. [DOI] [PubMed] [Google Scholar]
- 10.Anson CA, Shepherd C. Incidence of secondary complications in spinal cord injury. Int J Rehabil Res 1996;19(1):55–66. [DOI] [PubMed] [Google Scholar]
- 11.Blackmer J, Marshall S. Obesity and spinal cord injury: an observational study. Spinal Cord 1997;35(4):245–7. [DOI] [PubMed] [Google Scholar]
- 12.Crane DA, Little JW, Burns SP. Weight gain following spinal cord injury: a pilot study. J Spinal Cord Med 2011;34(2):227–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Groot S, Post MWM, Postma K, Sluis TA, Van der Woude LHV. Prospective analysis of body mass index during and up to 5 years after discharge from inpatient spinal cord injury rehabilitation. J Rehabil Med 2010;42(10):922–8. [DOI] [PubMed] [Google Scholar]
- 14.Stover SL, DeVivo MJ, Go BK. History, implementation, and current status of the National Spinal Cord Injury Database. Arch Phys Med Rehabil 1999;80(11):1365–71. [DOI] [PubMed] [Google Scholar]
- 15.U.S. Department of Health and Human Services, National Institutes of Health, National Heart, Lung and Blood Institute 1998 Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report (NIH Publication No. 98-4083) Retrieved from http://www.nhlbi.nih.gov/guidelines/obesity/ob_gdlns.pdf.
- 16.Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE, et al. . International standards for neurological classification of spinal cord injury. J Spinal Cord Med 2003;26(Suppl 1):S50–6. [DOI] [PubMed] [Google Scholar]
- 17.DeVivo MJ, Krause JS, Lammertse DP. Recent trends in mortality and causes of death among persons with spinal cord injury. Arch Phys Med Rehabil 1999;80(11):1411–9. [DOI] [PubMed] [Google Scholar]
- 18.Weaver FM, Collins EG, Kurichi J, Miskevics S, Smith B, Rajan S, et al. . Prevalence of obesity and high blood pressure in veterans with spinal cord injuries and disorders: a retrospective review. Am J Phys Med Rehabil 2007;86(1):22–9. [DOI] [PubMed] [Google Scholar]
- 19.Kortebein P, Ferrando A, Lombeida J, Wolfe E. Effect of 10 days of bed rest on skeletal muscle in healthy older adults. JAMA 2007;297(16):1772–4. [DOI] [PubMed] [Google Scholar]
- 20.Gupta N, White KT, Sandford PR. Body mass index in spinal cord injury—a retrospective study. Spinal Cord 2006;44(2):92–94. [DOI] [PubMed] [Google Scholar]


