Abstract
In 2010, the American Heart Association introduced a new conceptual framework to encourage a focus on primary prevention and provided a definition for “ideal cardiovascular health”. In this study we examined the relationship between positive childhood experience and ideal cardiovascular health in mid-life, and the extent to which education, depression, and social support mediate this association. Data are from participants in the Midlife and Aging in the United States study who completed a clinic-based assessment of health (N = 1255, aged 34–84 years, 2004–2005). We created a positive childhood experiences index based on retrospective report of eight childhood experiences, and calculated a continuous ideal cardiovascular health score for each participant following the American Heart Association’s definition of ideal, intermediate and poor cardiovascular health across seven health metrics (analyses conducted in 2015–2016). Positive childhood experiences were associated with ideal cardiovascular health: compared to individuals in the lowest quartile, respondents in the second, third, and fourth quartile of positive childhood experiences scored 0.42 (standard error (SE) = 0.18), 0.92 (SE = 0.18) and 1.04 (SE = 0.18) units higher on ideal cardiovascular health, adjusting for age, sex, and race. Respondent’s education, depression status, and social support fully mediated the direct effect of positive childhood experiences on ideal cardiovascular health, with the largest indirect effect for education. These results suggest that positive childhood experiences are associated with ideal cardiovascular health in midlife. Strategies to promote cardiovascular wellbeing may benefit from a focus on social interventions early in life; educational attainment, major depression, and social support may represent key points of intervention.
Keywords: Ideal cardiovascular health, Aging, Epidemiology, Life course, Childhood factors
Cardiovascular diseases (CVD) are the leading cause of death for men and women in the United States and accounted for >801,000 deaths in 2013 (Mozaffarian et al., 2016). CVD processes begin in early life (Berenson et al., 1998; Berenson and Srnivasan, 2005; Lloyd-Jones et al., 2009; Mahoney et al., 1991), and social factors during childhood shape CVD risk across the life course (Gundersen et al., 2011; Pollitt et al., 2005; Slopen et al., 2013; Slopen et al., 2011). National policy statements from both the American Heart Association (AHA) (Lloyd-Jones et al., 2010) and the American Academy of Pediatrics (Garner et al., 2012) highlight childhood as a critical time point for the prevention of CVD. Traditionally, research on the influence of childhood experiences on chronic disease risk has focused on how disadvantage during childhood (Doom et al., 2016; Lehman et al., 2005; Pollitt et al., 2007, 2008; Pollitt et al., 2005) confers elevated risk for poor outcomes, including cardiovascular diseases (Galobardes et al., 2006; Johnson et al., 2013; Loucks et al., 2011; Miller et al., 2011; Shonkoff et al., 2009). To date, limited research has considered the influences of positive experiences during childhood for cardiovascular wellbeing in later life (Appleton et al., 2013; Laitinen et al., 2013; Pulkki-Råback et al., 2015; Sood and Gidding, 2016; Lehman et al., 2005; Russek and Schwartz, 1997; Slopen et al., 2016; Sood and Gidding, 2016; Westerlund et al., 2013), in contrast to disease as the outcome (Lehman et al., 2005; Russek and Schwartz, 1997; Slopen et al., 2016; Westerlund et al., 2013).In this study, we examined the relationship between positive childhood experience and an ideal cardiovascular health in a large sample of adults in mid-life, and evaluated the extent to which education, depression, and social support in midlife mediate this association.
In 2010, the AHA set a goal to improve the cardiovascular health of the population by introducing a new conceptual framework to encourage a focus on primary prevention (Lloyd-Jones et al., 2010). The AHA’s approach—consistent with the World Health Organization’s definition of health as “a state of complete physical, mental, and social wellbeing and not merely the absence of disease or infirmity”—defines “ideal,” “intermediate, and “poor cardiovascular health for seven metrics that can be monitored over time (Lloyd-Jones et al., 2010). The definition includes four health behaviors (i.e., smoking, weight, physical activity, and diet) and three health factors (i.e., blood pressure, total cholesterol, and glycemia) (Lloyd-Jones et al., 2010). Individuals who achieve a greater number of ideal metrics have lower risk of incident myocardial infarction and stroke (Dong et al., 2012), cancer (Rasmussen-Torvik et al., 2013), and mortality (Dong et al., 2012; Yang et al., 2012). The prevalence of ideal cardiovascular health in the US (defined as “ideal across all metrics) is very low (Bambs et al., 2011; Folsom et al., 2011; Ford et al., 2012; Shay et al., 2012; Yang et al., 2012). For example, in a population-based study of 12,744 participants ages 45–64 years, 0.1% met ideal levels across all seven indicators (Folsom et al., 2011). Although the concept encourages consideration of health-promoting factors (Ford, 2012), limited research has examined the social factors in childhood (Appleton et al., 2013; Pulkki-Råback et al., 2015) or adulthood (Caleyachetty et al., 2015; Unger et al., 2014) associated with ideal cardiovascular health in mid-life.
We are aware of three prior studies that examined childhood characteristics in relation to ideal cardiovascular health. Using prospective data from the New England Family Study (n = 415) (Appleton et al., 2013), Appleton and colleagues documented a positive association between attention regulation, cognitive ability, and positive home environment at 7 years and favorable cardiovascular health in adulthood (mean age = 42.2 years). Drawing on data from 477 men and 612 women in the Cardiovascular Risk in Young Finns Study, Pulkki-Raback and colleagues found that psychosocial factors between the ages of 3 and 18 years were associated with ideal cardiovascular health in adulthood (mean age = 37.2 years) (Pulkki-Råback et al., 2015). Similarly, a cross-national comparison study using population-based cohorts from Finland (n = 1883), Australia (n = 1803), and the United States (n = 723) (Laitinen et al., 2013) found that childhood socioeconomic position and parental smoking were inversely associated with ideal cardiovascular health 19–31 years later (30–48 years at follow-up).
The current study builds on prior research to examine positive childhood experiences and ideal cardiovascular health, and potential underlying pathways, using a large national sample of US adults in midlife. Informed by life course theory (Ben-Shlomo and Kuh, 2002; Ben-Shlomo et al., 2014), we hypothesized that positive childhood experiences would show a dose-response association with ideal cardiovascular health, and that education, major depression, and social support would mediate this association.
1. Methods
1.1. Sample
The data are from the Midlife in the United States (MIDUS) study, an interdisciplinary effort to investigate the relationships between social, psychological, behavioral factors and health. The first wave of MIDUS (MIDUSI, 1994–1995) enrolled 7108 non-institutionalized individuals ages 25 to 74 years through random digit dialing from across the US, including siblings for some respondents and some pairs of twins (Brim et al., 2004). The second wave (MIDUSII, 2004–2005) followed up 4963 (70%) of the original participants, and newly recruited 592 African Americans from Milwaukee, WI (Radler and Ryff, 2010). Participants who completed the psychosocial survey at MIDUSII and were healthy enough to travel (N = 3191) were invited to participate in a biomarker substudy that required an overnight stay at one of three General Clinical Research Centers. A total of 1255 individuals completed comprehensive biological assessments. Participants enrolled in the biomarker project were similar to non-participants with regard to sex, age, race, marital status, income and chronic conditions, but were more highly educated (Dienberg Love et al., 2010).
We present complete case analysis for our main results (N = 1147). Participants in the complete case sample had higher ideal cardiovascular health scores and more positive childhood experiences, were more likely to be white and highly educated, and were less likely to be depressed, compared to the excluded individuals. Results from multiple imputed data sets in supplemental tables (N = 1255). Participants provided informed consent, and the study was approved by Institutional Review Boards at participating institutions. Analyses were conducted in 2015–2016.
1.2. Measures
1.2.1. Positive childhood experiences index
We created a positive childhood experiences index based on the presence or absence of eight components: high parental education, high perceived SES, two-parent family, residential stability, no smokers residing in home, high parental warmth, high emotional support and high instrumental support (range: 0 to 8; details below). Factor analysis confirmed the presence of a single factor for the index. Quartiles for the index were created such that the top quartile indicated the most positive experiences.
1.2.1.1. High parental education
Each participant reported his/her mother’s and father’s highest education levels. We created an indicator for high parental education (using the highest value for either mother or father), whereby 4-year college degrees or more were considered as high.
1.2.1.2. High perceived SES
Participants reported on their family financial status during childhood compared to the average family. Responses ranged from 1 (a lot better off) to 7 (a lot worse off). Participants who reported a lot better off or somewhat better off were categorized as “high perceived SES.”
1.2.1.3. Two-parent family
Family structure in early life was queried with a single yes/no question: “Did you live with both of your biological parents up until you were 16? Participants who responded affirmatively were categorized as growing up in two-parent family.
1.2.1.4. Residential stability
Residential mobility in childhood was assessed with a single question: “how many times during your childhood did you move to a totally new neighborhood or town? Following prior work (Bures, 2003), participants who reported <3 moves were categorized as stable.
1.2.1.5. No smokers residing in home
Respondents were asked: “During your first 16 years, did you live with anyone in your household who smoked cigarettes or other tobacco products? (response options: no one, father, mother, someone else). Respondents who reported “no one was considered as having no smokers in home.
1.2.1.6. High parental warmth
Parental warmth in early life was queried with a six-item Parental Support Scale (Rossi, 2001) (e.g., “how much did your mother/father understand your problems and worries?”), with responses ranging from 1 (a lot) to 4 (not at all). Responses were reverse-coded such that a higher score represents greater warmth, and averaged responses across all items (α = 0.91) (Rothrauff et al., 2009). We created quartiles of the score, and participants in the top quartile were categorized as having high parental warmth.
1.2.1.7. High emotional support
Emotional support in childhood was assessed with five items from the Emotional Neglect subscale of the Childhood Trauma Questionnaire (Bernstein and Fink, 1998; Bernstein et al., 1994) (e.g., “there was someone in my family who helped me feel that I was important or special”), with responses ranging from 1 (never true) to 5 (very often true). A score was constructed by averaging responses across all items (α = 0.85), and we created quartiles of the score. Participants in the top quartile were considered as having high emotional support.
1.2.1.8. High instrumental support
Instrumental support in early life was measured with two items from the physical neglect subscale of the Childhood Trauma Questionnaire (Bernstein and Fink, 1998; Bernstein et al., 1994) (e.g., “there was someone to take me to the doctor if I needed it”), with responses ranging from 1 (never true) to 5 (very often true). A score was constructed by averaging responses on the two items (α = 0.61), and was dichotomized as high instrumental support (=5) and low support (<5); this threshold was selected based on the distribution of the data, which did not allow for a top quartile.
1.2.2. Ideal cardiovascular health
Following AHA’s definition of ideal, intermediate and poor cardiovascular health for adults (Folsom et al., 2011; Lloyd-Jones et al., 2010), we created a score based on seven cardiovascular disease risk factors or health behaviors assessed at the biomarker project. Participants self-reported their smoking status, frequency of vigorous and moderate physical activity, and frequency of dietary intake including the intake of fruit and vegetables, fish, whole grain, fast food (as a proxy for sodium intake) and sugared beverages. Participants’ total cholesterol, blood pressure and Hemoglobin A1c (HbA1c, as a proxy for fasting plasma glucose) were measured by trained staff, and their medication used to control cholesterol, blood pressure and diabetic conditions was queried. See Table 2 for definitions of poor, intermediate, and ideal for each metric. Following prior research with middle-aged participants (Folsom et al., 2011), we categorized each health metric as poor (score = 1), intermediate (score = 2), and ideal (score = 3) and summed across the metrics (potential range: 7 to 21), with higher scores reflecting better health.
Table 2.
Distribution of ideal cardiovascular health metrics, and prevalence by quartile of positive childhood experiences (N = 1147).
| Health metric | Definition | Total sample, mean (SD) or % | Positive childhood experiences quartile | P-value | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Q1 | Q2 | Q3 | Q4 | ||||
| Ideal Cardiovascular Health Score | Sum across the following seven metrics (ideal = 3, intermediate = 2, poor = 1), ranging from 8 to 21 | 14.72 (2.29) | 14.10(2.30) | 14.44(2.13) | 15.12(2.20) | 15.27(2.31) | <0.0001 |
| Smoking | <0.0001 | ||||||
| Ideal | Never or quit >12 months | 53.62 | 42.20 | 49.61 | 60.51 | 63.45 | |
| Intermediate | Former ≤ 12 months | 32.26 | 34.86 | 37.01 | 29.35 | 27.93 | |
| Poor | Current | 14.12 | 22.94 | 13.39 | 10.14 | 8.62 | |
| Body mass index | 0.07 | ||||||
| Ideal | <25 kg/m2 | 24.06 | 21.71 | 21.65 | 24.28 | 28.62 | |
| Intermediate | 25–29.99 kg/m2 | 35.40 | 33.33 | 34.65 | 35.14 | 38.62 | |
| Poor | ≥30 kg/m2 | 40.54 | 44.95 | 43.70 | 40.58 | 32.76 | |
| Physical activity | 0.0008 | ||||||
| Ideal | ≥150 min/wk moderate or ≥75 min/wk vigorous or ≥150 min/wk moderate + vigorous | 39.23 | 33.94 | 33.86 | 45.29 | 44.14 | |
| Intermediate | 1–149 min/wk moderate or 1–74 min/wk vigorous or 1– 149 min/wk moderate + vigorous | 19.35 | 17.43 | 18.50 | 20.29 | 21.38 | |
| Poor | None | 39.23 | 48.62 | 47.64 | 34.42 | 34.48 | |
| Health diet score | 0.14 | ||||||
| Ideal | 4–5 components | 21.97 | 16.82 | 22.44 | 24.28 | 25.17 | |
| Intermediate | 2–3 components | 56.93 | 58.41 | 58.66 | 55.07 | 55.52 | |
| Poor | 0–1 components | 21.10 | 24.77 | 18.90 | 20.65 | 19.31 | |
| Total cholesterol | 0.09 | ||||||
| Ideal | <200 mg/dL, without rx | 42.55 | 40.98 | 41.73 | 40.58 | 46.90 | |
| Intermediate | 200–239 mg/dL, or treated to <2(K) mg/dL | 48.04 | 46.18 | 48.03 | 52.54 | 45.86 | |
| Poor | ≥240 mg/dL | 9.42 | 12.84 | 10.24 | 6.88 | 7.24 | |
| Blood pressure | 0.07 | ||||||
| Ideal | <120/<8() mm Hg, without rx | 19.18 | 14.37 | 17.32 | 23.91 | 21.72 | |
| Intermediate | SBP 120–139 or DBP 80–89 mm Hg, or treated to <120/<80 mm Hg | 60.42 | 64.22 | 60.63 | 58.70 | 57.59 | |
| Poor | SBP ≥ l40or DBP ≥ 90 mm Hg | 20.40 | 21.41 | 22.05 | 17.39 | 20.69 | |
| HbA1c | 0.51 | ||||||
| Ideal | 0 < HbA1c < 5.7%, without rx | 32.26 | 29.97 | 29.92 | 34.78 | 34.48 | |
| Intermediate | 5.7% ≤ HbA1c < 6.5%, or treated to <5.7% | 53.62 | 55.66 | 53.54 | 53.99 | 51.03 | |
| Poor | ≥6.5% | 14.12 | 14.37 | 16.54 | 11.23 | 14.48 | |
Note: Percentages refer to the proportion of individuals within each category with that characteristic. P-value is derived from χ2 or analysis of variance tests.
1.2.3. Potential mediators
1.2.3.1. Education
Participants reported their highest grade of school or year of college completed. Responses were dichotomized as 4-year college or more and less than college degree.
1.2.3.2. Major depressive disorder
Depressive symptoms were assessed with the 20-item Center for Epidemiological Studies Depression (CES-D) scale (Radloff, 1977) administered at the time of biomarker collection (α = 0.90). Participants with scores ≤16 were considered as having major depression (Morozink et al., 2010; Radloff, 1977).
1.2.3.3. Social support
Emotional support from spouse or partner (if applicable; α = 0.90), other family members (α = 0.85), and friends (α = 0.89) was measured separately, each with a four-item scale (Schuster et al., 1990) (e.g., how much does your spouse or partner/friends/members of your family really care about you?). Two additional items were included in the spouse or partner scale (i.e., “how much does he or she appreciate you, “how much can you relax and be yourself around him or her”) (Schuster et al., 1990; Walen and Lachman, 2000). Responses ranged from 1 (a lot) to 4 (not at all) and were reverse coded with higher scores reflecting greater support. An overall score was calculated by averaging responses on support from the three sources (Brooks et al., 2014).
1.2.4. Covariates
Participants’ sex, race (white, black, others) and age at MIDUSII were included as covariates.
1.2.5. Statistical analyses
Statistical analyses were performed in SAS 9.3, Mplus 7th Edition, and SUDAAN 11.0.1. Chi-square and analysis of variance tests were used to examine the distribution of ideal cardiovascular health metrics in the total sample and across quartiles of the positive childhood experiences index. Generalized estimating equations (GEE) with an identity link and normal distribution were used to regress ideal cardiovascular health score on the quartiles of childhood positive experiences index, accounting for twin and sibling clusters, and adjusted for participants’ sex, race and age. We investigated mediators using two approaches. First, we conducted a series of GEE models with each potential mediator included individually, and then together. Second, we tested for mediation of the relationship between positive childhood experiences (as a continuous score) and ideal cardiovascular health using structural equation models, with mean and variance weighted least squares estimation to calculate the direct and indirect effects.
Finally, we conducted two sensitivity analyses. First, we regressed ideal cardiovascular health score on each individual component of the positive childhood experiences index separately, to evaluate if all components of the inventory were associated with our outcome in the expected direction. Second, we replicated our analyses using ten imputed data sets to evaluate if missing data influenced our results.
2. Results
The mean age of the participants was 54.62 years (standard deviation (SD) = 11.73) (Table 1). There were more females than males (56.15%), and participants were predominantly white (81.52%). Over 40% of respondents had a 4-year college degree or higher, and 16% had current major depression. The average total positive childhood experiences index score was 3.46 (SD = 1.66; range: 0 to 8). The proportion of participants who endorsed the individual index components ranged from 17% (high perceived childhood SES) to 76% (two-parent family).
Table 1.
Descriptive characteristics of study participants (N = 1147).
| Mean (SD) or % | |
|---|---|
| Age, years (mean, SD) | 54.62 (11.73) |
| Race (%) | |
| Black | 15.43 |
| White | 81.52 |
| Other | 3.05 |
| Sex (%) | |
| Male | 43.85 |
| Female | 56.15 |
| Total, positive childhood experiences index (possible range: 0–8), mean (SD) | 3.46 (1.66) |
| Individual positive childhood experiences (%) | |
| Parental education college or higher | 41.85 |
| High perceived SES in childhood | 17.35 |
| Two parent family | 76.02 |
| Residential stability | 70.88 |
| No smokers residing in home | 28.77 |
| High parental warmth | 26.68 |
| High emotional support | 21.97 |
| High instrument support | 62.60 |
| Educational attainment (%) | |
| Less than college | 58.59 |
| College or more | 41.41 |
| Major Depression (%) | 15.61 |
| Social support score, mean (SD) | 3.44 (0.49) |
SD = standard deviation; SES = socioeconomic status.
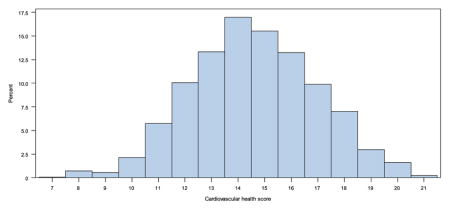
The ideal cardiovascular health score had an approximately normal distribution (Appendix 1), with a mean of 14.82 (SD = 2.29; range: 7 to 21). Across quartiles of positive childhood experiences, the ideal cardiovascular health score increased (p < 0.0001) (Table 2). The proportion of participants who met “ideal criteria for each of the 7 individual health metrics ranged from a high of 53.62% (smoking behavior) to a low of 19.18% (blood pressure). Bivariate analyses indicate that all indicators follow a pattern whereby ideal metric values are more common among respondents in the highest quartile of the positive childhood experiences inventory compared to those in the lowest quartile; however, overall group differences by quartile of positive childhood experiences were only significant (at p < 0.05) for smoking and physical activity.
Results from GEE models suggest that positive childhood experiences were associated with ideal cardiovascular health (Table 3): compared to individuals in the lowest quartile, respondents in the second, third, and fourth quartile of positive childhood experiences scored 0.42 (standard error (SE) = 0.18), 0.92 (SE = 0.18) and 1.04 (SE = 0.18) units higher on ideal cardiovascular health, adjusting for age, sex, and race. This pattern was slightly attenuated but maintained in models that additionally included respondent’s education, major depression, and social support (see Models 2–4). In a model that included all potential mediators simultaneously, respondents in the positive childhood experiences quartiles 3 and 4 continued to show greater ideal cardiovascular health scores compared to respondents in quartile 1 (p-values < 0.0001).
Table 3.
Beta coefficients and standard errors of linear regression models predicting the association between positive childhood experiences and ideal cardiovascular health score (n = 1147)a.
| Model 1 | Model 2 (model 1 + education) | Model 3 (model 1 + depression) | Model 4 (model 1 + social support) | Model 5: full model | |
|---|---|---|---|---|---|
| β (SE) | β (SE) | β (SE) | β (SE) | β (SE) | |
| Positive childhood experiences index | |||||
| Quartile 1 [ref.] | |||||
| Quartile 2 | 0.42 (0.18)* | 0.40 (0.17)* | 0.40 (0.18)* | 0.35 (0.18)* | 0.32 (0.17)~ |
| Quartile 3 | 0.92 (0.18)*** | 0.77 (0.17)*** | 0.86 (0.18)*** | 0.82 (0.18)*** | 0.64 (0.18)*** |
| Quartile 4 | 1.04 (0.18)*** | 0.78 (0.18)*** | 0.97 (0.18)*** | 0.89 (0.18)*** | 0.61 (0.18)*** |
| Educational attainment | |||||
| Less than college [ref.] | |||||
| College or more | 0.84 (0.14)*** | 0.82 (0.14)*** | |||
| Major depression | −0.51 (0.19)** | −0.35 (0.19)~ | |||
| Social support score | 0.43 (0.14)** | 0.34 (0.14)* |
Boldface indicates statistical significance (***p ≤ 0.001, **p ≤ 0.01, *p ≤ 0.05, ~p ≤ 0.10).
Note: Generalized estimating equations with identity link and normal distribution were used in all models to adjust for clustering by family and were calculated using SAS PROC GENMOD.
All models adjust for participant age, race, and sex.
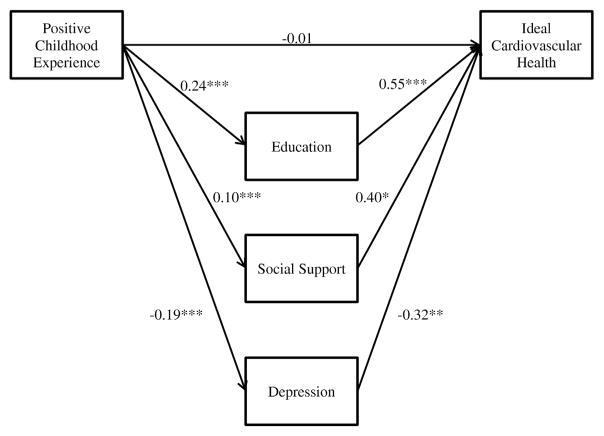
In structural equation models to examine potential mediators, positive childhood experience was positively associated with education (β = 0.24, p < 0.001) and social support (β = 0.10, p < 0.001), and negatively associated with depression (β = −0.19, p < 0.001) (Fig. 1 and Appendix 2). Education (β = 0.55, p < 0.001) and social support (β = 0.40, p < 0.01) were positively associated with ideal cardiovascular health, and depression was negatively associated with ideal cardiovascular health (β = −0.32, p < 0.01). Positive childhood experience was associated with ideal cardiovascular health indirectly through education (specific effect β = 0.13, p < 0.001), depression (specific effect β = 0.06, p < 0.05), and social support (specific effect β = 0.04, p < 0.05), and no direct effect was observed (β = −0.01, 95% CI = −0.12, 0.09; see Appendix 3 for model fit statistics).
Fig. 1.
Mediation of positive childhood experiences and ideal cardiovascular health by education, social support and major depression.
We conducted two sensitivity analyses. First, in models that regressed the ideal cardiovascular health score on each individual component of the positive childhood experiences index separately (Appendix 4), all components of the inventory showed positive associations with ideal cardiovascular health, although the magnitude of the associations varied, and statistical significance at p < 0.05 was present only for five of the eight indicators. Second, replication of our analyses using 10 imputed data sets produced identical conclusions, although there were some modest changes to some coefficients(Appendices 4 and 5).
3. Discussion
In this study of 1147 adults in midlife, positive childhood experiences were associated with higher ideal cardiovascular health scores. We advance prior research by examining this association in an older national sample, and conducting mediation analyses using structural equation models to estimate direct and indirect effects. Respondent’s education, major depression status, and social support fully mediated the direct effect of positive childhood experiences on ideal cardiovascular health score, with the largest indirect effect for education. In sensitivity analyses that considered each component of the positive childhood experiences index separately, residential stability, high emotional support, high instrumental support, high parental education, and no smokers residing in home were each associated with higher ideal cardiovascular health score, with the largest associations for the latter two domains. This study adds to the existing literature suggesting that social environments are associated with ideal cardiovascular health in midlife (Caleyachetty et al., 2015; Unger et al., 2014) and that childhood environments (Appleton et al., 2013; Laitinen et al., 2013; Pulkki-Råback et al., 2015) set the stage for conditions in adulthood that drive this association.
Although findings from this study cannot address causality, our results are consistent with prior prospective research using other samples with conceptually similar childhood predictors (Appleton et al., 2013; Laitinen et al., 2013; Pulkki-Råback et al., 2015), and extends this work by documenting associations and pathways in an older and larger sample drawn from across the US, and using a rich multidimensional assessment of childhood experiences. Our findings are also consistent with evidence from several experimental studies which suggest that school-based (Campbell et al., 2014; Conti et al., 2015) and family-based (Miller et al., 2014) interventions can have benefits for cardiometabolic outcomes and behaviors years and even decades later. To best inform prevention strategies, detailed longitudinal studies with repeated measures of childhood social environment and cardiovascular health metrics are needed to identify sensitive periods for the effects of exposures, and to explore periods of vulnerability for each health metric. It may also be valuable for these future studies to use dynamic mediation models (Huang and Yuan, 2016) to examine the time-variant nature of potential psychological and behavioral mediators across the life course, and to consider environmental modifiers, such as school (Spriggs et al., 2009) or neighborhood context (Slopen et al., 2014).
3.1. Limitations
There are several notable limitations to consider. First, positive childhood experiences were assessed retrospectively; although the literature generally supports the use of retrospective reports about childhood (Brewin et al., 1993), it is possible that reports were influenced by current health or psychopathology (Hardt and Rutter, 2004). Second, to create a comprehensive measure of positive childhood experiences based on the information available in MIDUS, we constructed an inventory using dichotomized variables reflecting a variety of domains; this approach was necessary to combine multiple types of positive experiences, but limits information about strength, chronicity, and timing. Third, the item that inquired about family structure only assessed whether the participant resided with both biological parents; some respondents who did not endorse this item may have had two adults in their household, and this could have included adoptive or step-parents. Fourth, MIDUS was not designed to measure ideal cardiovascular health as defined by the AHA; therefore we did not have data on diet or physical activity that conformed to the traditional definitions. Finally, the generalizability of this study is limited, given that Whites and high SES individuals are over-represented in MIDUSII.
4. Conclusions
Our study finds that positive childhood experiences are associated with ideal cardiovascular health in midlife, and that this association is fully mediated by educational attainment, absence of major depression, and greater social support. Efforts to promote and address disparities in cardiovascular health may benefit from a focus on social factors during the childhood period, including the broad array of social policies that shape disparities in childhood experiences. Furthermore, mediators including educational attainment, major depression, and social support may represent key points of intervention to promote ideal cardiovascular health in the US population.
Acknowledgments
This research was supported by grant P3022586 from the W. K. Kellogg Foundation, and grant P01-AG020166 from the National Institute on Aging to conduct a longitudinal follow-up of the MIDUS (Midlife in the United States) investigation. The original MIDUS study was supported by the John D. and Catherine T. MacArthur Foundation Research Network on Successful Midlife Development. Support was also provided by grant 1UL1RR025011 (University of Wisconsin) from the Clinical and Translational Science Award program of the National Center for Research Resources, National Institutes of Health.
Appendix 1. Distribution of ideal cardiovascular health score, midlife in the United States biomarker study (N = 1147)
Appendix 2. Total, direct, and indirect effects of mediation analysis (N = 1147)
| Estimate | 95% CIa | |
|---|---|---|
| Total effect | 0.23*** | (0.14, 0.31) |
| Total indirect | 0.23*** | (0.17, 0.31) |
| Specific indirect effects | ||
| Via education | 0.13*** | (0.08, 0.19) |
| Via depression | 0.06* | (0.02, 0.12) |
| Via social support | 0.04* | (0.01, 0.08) |
| Direct effect | −0.01 | (−0.12, 0.09) |
Boldface indicates statistical significance (*p < 0.05, **p < 0.01, ***p < 0.001).
95% bootstrapped confidence interval.
Appendix 3. Model fit summary
| Model | χ2 | df | CFI (≥0.95)a | SRMR (≤0.08) | RMSEA (≤0.06) | χ2 Difference | df | p-Value |
|---|---|---|---|---|---|---|---|---|
| Initial model | 192.695 | 12 | 0.689 | 0.063 | 0.115 | 139.619 | 1 | p < 0.0001 |
| Final model | 53.076 | 11 | 0.928 | 0.035 | 0.058 |
Note: Several modifications were made to improve the fit of the model. Modifications that significantly improved the model fit and were theoretically plausible were included. Six total modifications were made to the model. Covariances were added for: 1) social support and depression; 2) education with depression; age with race; age with depression; age with social support; and positive childhood experiences with race.
Model fit criterion based on Hu and Bentler (1999).
Appendix 4. Beta coefficients and standard errors of linear regression models predicting the association between individual components of the positive childhood experiences index and ideal cardiovascular health score (complete case and multiple imputation data)
| Complete case analysis, n = 1147 β (SE) |
Multiple imputation analysis (n = 1255 β (SE) |
|
|---|---|---|
| Parental education college or higher | 0.61 (0.14)*** | 0.59 (0.14)*** |
| High perceived SES in childhood | 0.23 (0.18) | 0.15 (0.17) |
| Two parent family | 0.31 (0.17)~ | 0.31 (0.16)~ |
| Residential stability | 0.38 (0.14)** | 0.35 (0.14)* |
| No smokers residing in home | 0.66 (0.14)*** | 0.61 (0.14)*** |
| High parental warmth | 0.27 (0.14)~ | 0.26 (0.14)~ |
| High emotional support | 0.43 (0.15)** | 0.32 (0.15)* |
| High instrument support | 0.32 (0.13)* | 0.39 (0.13)** |
Note: Generalized estimating equations with identity link and normal distribution were used in all models to adjust for clustering by family and were calculated using SAS PROC GENMOD. Beta coefficients were estimated in 8 separate regression models (one for each predictor). All models adjust for participant age, race, and sex. Boldface indicates statistical significance (***p ≤ 0.001, **p ≤ 0.01, *p ≤ 0.05, ~p ≤ 0.10). Multiple imputation results are from 10 imputed data sets.
Appendix 5. Beta coefficients and standard errors of linear regression models predicting the association between positive childhood experiences and ideal cardiovascular health score (n = 1255)
| Model 1 β (SE) |
Model 2 (model 1 + education) β (SE) |
Model 3 (model 1 + depression) β (SE) |
Model 4 (model 1 + social support) β (SE) |
Model 5: full model β (SE) |
|
|---|---|---|---|---|---|
| Positive childhood experiences index | |||||
| Quartile 1 [ref.] | |||||
| Quartile 2 | 0.37 (0.17)* | 0.34 (0.17)* | 0.34 (0.17) | 0.30 (0.17)~ | 0.24 (0.17) |
| Quartile 3 | 0.86 (0.17)*** | 0.69 (0.16)*** | 0.79 (0.17)*** | 0.74 (0.17)*** | 0.55 (0.17)** |
| Quartile 4 | 0.92 (0.18)*** | 0.64 (0.18)** | 0.84 (0.17)*** | 0.75 (0.18)*** | 0.44 (0.18)* |
| Educational attainment | |||||
| Less than college [ref.] | |||||
| College or more | 0.91 (0.14)*** | 0.90 (0.14)*** | |||
| Major depression | −0.55 (0.18)** | −0.38 (0.18)* | |||
| Social support score | 0.50 (0.13)** | 0.42 (0.13)** |
Note: Results from 10 imputed data sets. Generalized estimating equations with identity link and normal distribution were used in all models to adjust for clustering by family and were calculated using SAS PROC GENMOD. All models adjust for participant age, race, and sex. Boldface indicates statistical significance (***p ≤ 0.001, **p ≤ 0.01, *p ≤ 0.05, ~p ≤ 0.10).
Footnotes
Disclosures
None.
References
- Appleton AA, Buka SL, Loucks EB, Rimm EB, Martin LT, Kubzansky LD. A prospective study of positive early-life psychosocial factors and favorable cardiovascular risk in adulthood. Circulation. 2013;127:905–912. doi: 10.1161/CIRCULATIONAHA.112.115782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bambs C, Kip KE, Dinga A, Mulukutla SR, Aiyer AN, Reis SE. Low prevalence of “ideal cardiovascular health in a community-based population: the heart strategies concentrating on risk evaluation (Heart SCORE) study. Circulation. 2011;123:850–857. doi: 10.1161/CIRCULATIONAHA.110.980151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol. 2002;31:285–293. [PubMed] [Google Scholar]
- Ben-Shlomo Y, Mishra G, Kuh D. Life Course Epidemiology. In: Ahrens W, Pigeot I, editors. Handbook of Epidemiology. Springer; New York: 2014. pp. 1521–1549. [Google Scholar]
- Berenson GS, Srnivasan SR. Cardiovascular risk factors in youth with implications for aging: the Bogalusa heart study. Neurobiol Aging. 2005;26:303–307. doi: 10.1016/j.neurobiolaging.2004.05.009. [DOI] [PubMed] [Google Scholar]
- Berenson GS, Srinivasan SR, Bao WH, Newman WP, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. N Engl J Med. 1998;338:1650–1656. doi: 10.1056/NEJM199806043382302. [DOI] [PubMed] [Google Scholar]
- Bernstein D, Fink L. Manual for the Childhood Trauma Questionnaire. The Psychological Corporation; New York: 1998. [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, Sapareto E, Ruggiero J. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry. 1994;151:1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Gotlib IH. Psychopathology and early experience: a reappraisal of retrospective reports. Psychol Bull. 1993;113:82–98. doi: 10.1037/0033-2909.113.1.82. [DOI] [PubMed] [Google Scholar]
- Brim OG, Ryff CD, Kessler RC. How Healthy Are We?: A National Study of Well-being at Midlife. University of Chicago Press; Chicago: 2004. [Google Scholar]
- Brooks KP, Gruenewald T, Karlamangla A, Hu P, Koretz B, Seeman TE. Social relationships and allostatic load in the MIDUS study. Health Psychol. 2014;33:1373–1381. doi: 10.1037/a0034528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bures RM. Childhood residential stability and health at midlife. Am J Public Health. 2003;93:1144–1148. doi: 10.2105/ajph.93.7.1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caleyachetty R, Echouffo-Tcheugui JB, Muennig P, Zhu W, Muntner P, Shimbo D. Association between cumulative social risk and ideal cardiovascular health in US adults: NHANES 1999–2006. Int J Cardiol. 2015;191:296–300. doi: 10.1016/j.ijcard.2015.05.007. [DOI] [PubMed] [Google Scholar]
- Campbell F, Conti G, Heckman JJ, Moon SH, Pinto R, Pungello E, Pan Y. Early childhood investments substantially boost adult health. Science. 2014;343:1478–1485. doi: 10.1126/science.1248429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conti G, Heckman JJ, Pinto R. The Effects of Two Influential Early Childhood Interventions on Health and Healthy Behaviors. National Bureau of Economic Research; 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dienberg Love G, Seeman TE, Weinstein M, Ryff CD. Bioindicators in the MIDUS national study: protocol, measures, sample, and comparative context. J Aging Health. 2010;22:1059–1080. doi: 10.1177/0898264310374355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong C, Rundek T, Wright CB, Anwar Z, Elkind MSV, Sacco RL. Ideal cardiovascular health predicts lower risks of myocardial infarction, stroke, and vascular death across whites, blacks, and Hispanics: the northern Manhattan study. Circulation. 2012;125:2975–2984. doi: 10.1161/CIRCULATIONAHA.111.081083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doom JR, Gunnar MR, Clark CJ. Maternal relationship during adolescence predicts cardiovascular disease risk in adulthood. Health Psychol. 2016;35:376–386. doi: 10.1037/hea0000285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57:1690–1696. doi: 10.1016/j.jacc.2010.11.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford ES. Ideal cardiovascular health: start young, finish strong. Circulation. 2012;135:1–10. doi: 10.1161/CIRCULATIONAHA.112.102327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford ES, Greenlund KJ, Hong Y. Ideal cardiovascular health and mortality from all causes and diseases of the circulatory system among adults in the United States. Circulation. 2012;125:987–995. doi: 10.1161/CIRCULATIONAHA.111.049122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galobardes B, Smith GD, Lynch JW. Systematic review of the influence of childhood socioeconomic circumstances on risk for cardiovascular disease in adulthood. Ann Epidemiol. 2006;16:91–104. doi: 10.1016/j.annepidem.2005.06.053. [DOI] [PubMed] [Google Scholar]
- Garner AS, Shonkoff JP, Siegel BS, Dobbins MI, Earls MF, McGuinn L, Pascoe J, Wood DL Comm Psychosocial Aspects Child F et al. Early childhood adversity, toxic stress, and the role of the pediatrician: translating developmental science into lifelong health. Pediatrics. 2012;129:E224–E231. doi: 10.1542/peds.2011-2662. [DOI] [PubMed] [Google Scholar]
- Gundersen C, Mahatmya D, Garasky S, Lohman B. Linking psychosocial stressors and childhood obesity. Obes Rev. 2011;12:e54–e63. doi: 10.1111/j.1467-789X.2010.00813.x. [DOI] [PubMed] [Google Scholar]
- Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J Child Psychol Psychiatry. 2004;45:260–273. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- Huang J, Yuan Y. Bayesian dynamic mediation analysis. Psychol Methods. 2016 doi: 10.1037/met0000073. (No Pagination Specified) https://www.ncbi.nlm.nih.gov/pubmed/27123750. [DOI] [PubMed]
- Hu LT, Bentler PM. Cut-off criteria for fit indexes in covariance structure analysis: conventional criteria vs. new alternatives. Struct Equ Model. 1999;6:1–55. [Google Scholar]
- Johnson SB, Riley AW, Granger DA, Riis J. The science of early life toxic stress for pediatric practice and advocacy. Pediatrics. 2013;131:319–327. doi: 10.1542/peds.2012-0469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laitinen TT, Pahkala K, Venn A, Woo JG, Oikonen M, Dwyer T, Mikkila V, Hutri-Kahonen N, Smith KJ, et al. Childhood lifestyle and clinical determinants of adult ideal cardiovascular health: the cardiovascular risk in young Finns study, the childhood determinants of adult health study, the Princeton follow-up study. Int J Cardiol. 2013;169:126–132. doi: 10.1016/j.ijcard.2013.08.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehman BJ, Taylor SE, Kiefe CI, Seeman TE. Relation of childhood socioeconomic status and family environment to adult metabolic functioning in the CARDIA study. Psychosom Med. 2005;67:846–854. doi: 10.1097/01.psy.0000188443.48405.eb. [DOI] [PubMed] [Google Scholar]
- Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, Ford E, Furie K, Go A, et al. Heart disease and stroke statistics - 2009 update a report from the American Heart Association statistics committee and stroke statistics subcommittee. Circulation. 2009;119:E21–E181. doi: 10.1161/CIRCULATIONAHA.108.191261. [DOI] [PubMed] [Google Scholar]
- Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic impact goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- Loucks EB, Almeida ND, Taylor SE, Matthews KA. Childhood family psychosocial environment and coronary heart disease risk. Psychosom Med. 2011;73:563–571. doi: 10.1097/PSY.0b013e318228c820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahoney LT, Lauer RM, Lee J, Clarke WR. Factors affecting tracking of coronary heart disease risk factors in children. The Muscatine study. Ann N Y Acad Sci. 1991;623:120–132. doi: 10.1111/j.1749-6632.1991.tb43723.x. [DOI] [PubMed] [Google Scholar]
- Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychol Bull. 2011;137:959–997. doi: 10.1037/a0024768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Brody GH, Yu T, Chen E. A family-oriented psychosocial intervention reduces inflammation in low-SES African American youth. Proc Natl Acad Sci. 2014;111:11287–11292. doi: 10.1073/pnas.1406578111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morozink JA, Friedman EM, Coe CL, Ryff CD. Socioeconomic and psychosocial predictors of interleukin-6 in the MIDUS national sample. Health Psychol. 2010;29:626–635. doi: 10.1037/a0021360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Després J-P, et al. Heart Disease and Stroke Statistics—2016 Update. A Report From the American Heart Association. 2016;133:e38–e360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- Pollitt RA, Rose KM, Kaufman JS. Evaluating the evidence for models of life course socioeconomic factors and cardiovascular outcomes: a systematic review. BMC Public Health. 2005;5:7. doi: 10.1186/1471-2458-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollitt RA, Kaufman JS, Rose KM, Diez-Roux AV, Zeng D, Heiss G. Early-life and adult socioeconomic status and inflammatory risk markers in adulthood. Eur J Epidemiol. 2007;22:55–66. doi: 10.1007/s10654-006-9082-1. [DOI] [PubMed] [Google Scholar]
- Pollitt RA, Kaufman JS, Rose KM, Diez-Roux AV, Zeng D, Heiss G. Cumulative life course and adult socioeconomic status and markers of inflammation in adulthood. J Epidemiol Community Health. 2008;62:484–491. doi: 10.1136/jech.2006.054106. [DOI] [PubMed] [Google Scholar]
- Pulkki-Råback L, Elovainio M, Hakulinen C, Lipsanen J, Hintsanen M, Jokela M, Kubzansky LD, Hintsa T, Serlachius A, et al. Cumulative effect of psychosocial factors in youth on ideal cardiovascular health in adulthood: the cardiovascular risk in young Finns study. Circulation. 2015;131:245–253. doi: 10.1161/CIRCULATIONAHA.113.007104. [DOI] [PubMed] [Google Scholar]
- Radler BT, Ryff CD. Who participates? Accounting for longitudinal retention in the MIDUS national study of health and well-being. J Aging Health. 2010;22:307–331. doi: 10.1177/0898264309358617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- Rasmussen-Torvik LJ, Shay CM, Abramson JG, Friedrich CA, Nettleton JA, Prizment AE, Folsom AR. Ideal cardiovascular health is inversely associated with incident cancer: the atherosclerosis risk in communities study. Circulation. 2013;127:1270–1275. doi: 10.1161/CIRCULATIONAHA.112.001183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi AS. Caring and Doing for Others: Social Responsibility in the Domains of Family, Work, and Community. University of Chicago Press; 2001. [Google Scholar]
- Rothrauff TC, Cooney TM, An JS. Remembered parenting styles and adjustment in middle and late adulthood. J Gerontol B Psychol Sci Soc Sci. 2009;64:137–146. doi: 10.1093/geronb/gbn008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russek L, Schwartz G. Feeling of parental caring predict health status in midlife: a 35-year follow-up of the Harvard mastery of stress study. J Behav Med. 1997;20:1–13. doi: 10.1023/a:1025525428213. [DOI] [PubMed] [Google Scholar]
- Schuster TL, Kessler RC, Aseltine RH., Jr Supportive interactions, negative interactions, and depressed mood. Am J Community Psychol. 1990;18:423–438. doi: 10.1007/BF00938116. [DOI] [PubMed] [Google Scholar]
- Shay CM, Ning H, Allen NB, Carnethon MR, Chiuve SE, Greenlund KJ, Daviglus ML, Lloyd-Jones DM. Status of cardiovascular health in US adults: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2003–2008. Circulation. 2012;125:45–56. doi: 10.1161/CIRCULATIONAHA.111.035733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. JAMA. 2009;301:2252–2259. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- Slopen N, Kubzansky LD, Koenen KC. Childhood adversity and inflammatory and immune biomarkers associated with cardiovascular risk in youth: a systematic review. Brain Behav Immun. 2011;26:239–250. doi: 10.1016/j.bbi.2011.11.003. [DOI] [PubMed] [Google Scholar]
- Slopen N, Goodman E, Koenen KC, Kubzansky LD. Socioeconomic and other social stressors and biomarkers of cardiometabolic risk in youth: a systematic review of less studied risk factors. PLoS One. 2013;8:e64418. doi: 10.1371/journal.pone.0064418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N, Non AL, Williams DR, Roberts AL, Albert MA. Childhood adversity, adult neighborhood context, and cumulative biological risk for chronic diseases in adulthood. Psychosom Med. 2014;76:481–489. doi: 10.1097/PSY.0000000000000081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N, Chen Y, Priest N, Albert MA, Williams DR. Emotional and instrumental support during childhood and biological dysregulation in midlife. Prev Med. 2016;84:90–96. doi: 10.1016/j.ypmed.2015.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sood E, Gidding SS. Childhood psychosocial determinants of cardiovascular health. Curr Cardiovasc Risk Rep. 2016;10:1–8. [Google Scholar]
- Spriggs AL, Halpern CT, Herring AH, Schoenbach VJ. Family and school socioeconomic disadvantage: interactive influences on adolescent dating violence victimization. Soc Sci Med. 2009;68:1956–1965. doi: 10.1016/j.socscimed.2009.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unger E, Diez-Roux AV, Lloyd-Jones DM, Mujahid MS, Nettleton JA, Bertoni A, Badon SE, Ning H, Allen NB. Association of neighborhood characteristics with cardiovascular health in the multi-ethnic study of atherosclerosis. Circ Cardiovasc Qual Outcomes. 2014;7:524–531. doi: 10.1161/CIRCOUTCOMES.113.000698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walen HR, Lachman ME. Social support and strain from partner, family, and friends: costs and benefits for men and women in adulthood. J Soc Pers Relat. 2000;17:5–30. [Google Scholar]
- Westerlund H, Gustafsson PE, Theorell T, Janlert U, Hammarström A. Parental academic involvement in adolescence, academic achievement over the life course and allostatic load in middle age: a prospective population-based cohort study. J Epidemiol Community Health. 2013;67:508–513. doi: 10.1136/jech-2012-202052. [DOI] [PubMed] [Google Scholar]
- Yang Q, Cogswell ME, Flanders W, et al. Trends in cardiovascular health metrics and associations with all-cause and cvd mortality among us adults. JAMA. 2012;307:1273–1283. doi: 10.1001/jama.2012.339. [DOI] [PMC free article] [PubMed] [Google Scholar]