Abstract
Purpose
Maxillomandibular fixation (MMF) can be performed using various techniques. Two common approaches utilized are arch bars and bone screws. Arch bars are the gold standard and inexpensive, but often require increased procedure time. Bone screws with wire fixation is a popular alternative, but more expensive than arch bars. The differences in costs of care, complications, and operative times between these two techniques are analyzed.
Methods
A chart review was conducted on patients treated over the last twelve years at our institution. 44 patients with CPT code 21453 (closed reduction of mandible fracture with interdental fixation) with an isolated mandible fracture were used in our data collection. The operating room (OR) costs, procedure duration, and complications for these patients were analyzed.
Results
Operative times were significantly shorter for patients treated with bone screws (p<0.002). The costs for one trip to the OR for either method of fixation did not show any significant differences (p<0.840). More patients with arch bar fixation (62%) required a second trip to the OR for removal in comparison to those with screw fixation (31%)(p<0.068). This additional trip to the OR added significant cost. There were no differences in patient complications between these two fixation techniques.
Conclusions
MMF with bone screws represents an attractive alternative to fixation with arch bars in appropriate scenarios. Screw fixation offers reduced costs, fewer trips to the OR, and decreased operative duration without a difference in complications. Cost savings were noted most significantly in a decreased need for secondary procedures in patients who were treated with MMF screws. Screw fixation offers potential for reducing the costs of care in treating patients with minimally displaced or favorable mandible fractures.
Introduction
Treatment of facial fractures costs the US healthcare system upwards of $1 billion yearly(1). In a study of 21,244 hospital admissions of patients who underwent treatment of a facial fracture in 2008, open reduction and internal fixation of mandible fractures represented 52.2% of these admissions at a mean hospital cost of about $50,000 per patient. Closed reduction of mandible fractures comprised 12.1% of the above hospital admissions and cost about $26,000 per patient(1). Care for patients with mandibular injury is provided by multiple specialties, including Plastic Surgery (PRS), Oral and Maxillofacial Surgery (OMFS), and Otolaryngology (ENT). This variation may lead to differences in treatment patterns reported in the literature. Variability in surgical treatment of mandible fractures, timing and rate of complications will significantly impact overall cost.
Maxillomandibular fixation (MMF) can be performed using numerous methods(2–4). Traditionally, MMF has been performed with Erich arch bars or interdental ligatures(5, 6). While arch bars themselves are inexpensive, they suffer from a number of potential disadvantages. These include time-consuming application, greater risk of sharp puncture injury to the operator, and the possibility for periodontal trauma(2, 7–9).
An alternative to the use of arch bars is the use of specially designed self-drilling, self-tapping bone screws placed into the maxilla and mandible with stainless steel wires typically spanning between these devices(3, 10–12). MMF screws have been shown to provide fixation equal to that of arch bars, although they have also been noted to be more expensive(8, 9, 13). These screws offer several advantages in comparison to arch bars, such as ease of application and removal, reduced operating room time, decreased risk of injury from sharp wires, and the ability to provide better oral hygiene when in place(9, 14). MMF screws are not free of complications, however, and injuries to tooth roots are a problem occasionally seen with placement. Loss of fixation after screw loosening can also be an issue. While each of these two methods has unique flaws, both have been shown to be effective in providing MMF(15, 16). Patients may benefit from the use of one of these methods over the other, depending on the clinical scenario and operator preference.
Given the extensive expenditures associated with treatment of mandible fractures, a cost analysis of different management techniques may improve efficiency of the healthcare system, while also potentially optimizing patient care. Considering that MMF is used in the majority of patients, we sought to investigate the differences in costs of care, complications, and operative times in patients treated with closed reduction of isolated mandibular fractures by plastic surgeons in the academic setting.
Methods
Study Design
Data were collected retrospectively after Institutional Review Board approval. An extensive chart review was conducted on patients treated by the Division of Plastic and Reconstructive Surgery in the last twelve years at our home institution (2001–2013). One hundred sixty-two patients with the isolated CPT code 21453 (closed reduction of mandible fracture with interdental fixation) were used in our data collection. Patients who underwent internal fixation and those who sustained simultaneous operative facial trauma to any area other than the mandible were excluded. Eliminating patients who were treated with open reduction allowed us to look precisely at the time of device application and fixation without other confounding factors that prolong the operative procedure. Only patients with permanent dentition were included in the study.
Patient age, sex, and fracture pattern were recorded. The operating room costs and operative duration for each case were analyzed. Any secondary trips to the operating room for device removal were also recorded. Complications such as infection, injury to tooth roots, and post-operative malocclusion were documented. Orthopantograms were evaluated for screw placement. Postoperative clinic notes were analyzed for evidence of infection or malocclusion.
A cost comparison was conducted between arch bars and screws to determine if the differences in surgical time or number of trips to the operating room would offset the increased cost of screws.
Statistical Analysis
Groups were compared using independent Student’s t-test for continuous variables. Fisher’s exact test was employed to compare the proportions of patients requiring re-operation between the two groups. The mid-p correction values reported were obtained using a programming code (Cardillo G. 2010. MyFisher: the definitive function for the Fisher’s exact and conditional test for any RxC matrix) run in MatLab R2011b (The MathWorks, Inc. Natick, Massachusetts). All other statistical analyses were performed using IBM SPSS Version 20 (Armonk, NY). For all comparisons, a p-value of less than .05 was considered statistically significant. Results are displayed as mean ± SD.
Results
A total of forty-four subjects met the study conditions. The majority of patients were male (72% male and 28% female). Age ranged from 14 to 70 years old with a mean of 27.5 years. Fracture types included isolated angle, condyle, and body as well as multiple fractures involving the condyle/angle and parasymphyseal regions (Table 1).
Table 1. Fracture Type.
Number of patients per group.
| Number of Patients (n) | ||
|---|---|---|
| Screws | Arch Bars | |
| Condyle | 4 (27%) | 13 (45%) |
| Angle | 5 (33%) | 1 (3%) |
| Body | 2 (13%) | 6 (21%) |
| Parasymphyseal/Condyle or Angle | 4 (27%) | 9 (31%) |
| Total | 15 | 29 |
In comparison to arch bars, the use of screws significantly reduced operative time by an average of 59 minutes (86 ± 37 minutes versus 27 ± 14 minutes, p<0.002) (Fig 1). Regardless, the cost of care for one trip to the operating room for either method of fixation ($3550 ± 1042 USD for arch bars and $3862 ± 1018 for screws) did not significantly differ (p<0.840) (Fig 2). However, more patients with arch bar fixation (62%) required a second trip to the operating room for arch bar removal in comparison to those with screw fixation (31%, p<0.069) (Fig 3). The incidences of malocclusion and infection in this cohort were 0%. Two patients in the screw fixation group experienced screw loosening prematurely (13.3%), while no patients experienced hardware failure in the arch bar group. There was evidence of tooth root injury on panoramic radiograph in one of the 15 patients (6.7%) treated with maxillomandibular fixation screws.
Figure 1.
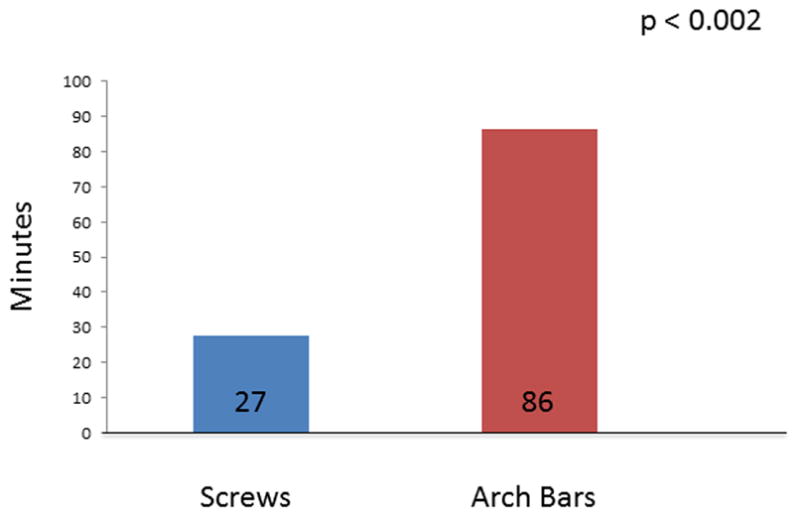
Comparison of operative time between fixation with screws versus arch bars.
Figure 2.

Comparison of cost (of one operation) between fixation with screws versus arch bars.
Figure 3.

Percentage of patients requiring second trip to the operating room for device removal.
Discussion
For surgeons with less experience treating mandible fractures, application of arch bars can be challenging and time consuming. Placement of MMF with screws can provide a simpler and faster method of fixation. We found a significant reduction in operative time with the use of screws for MMF versus arch bars when performed by plastic surgeons at our institution (p<0.002). Even with this difference, the overall costs per procedure did not significantly differ at our institution (p<0.841) in part due to the increased cost of screws in comparison to that of arch bars. West and colleagues(14) did identify a cost difference between these techniques. In their study, maxillomandibular fixation with screws saved $661 per patient. This was due to reduced operating room time required to place screws (4 minutes) based on estimation that arch bars would on average take one hour to place and remove.
Our average of 86 minutes for arch bar placement is similar to that in the Oral Maxillofacial Surgery literature (8, 9). However, these values can vary widely, with some reports of significantly shorter times for application(2). This demonstrates the significant variability in application times for arch bars, even within each specialty and likely reflects differences in experience within the specialties.
In our cohort, more patients with arch bar fixation (62%) required a second trip to the operating room for arch bar removal in comparison to those with screw fixation (31%). While we realize that arch bars and screws can be removed in the clinic setting, the results are a reflection of the experience at our institution(14). Possible explanations for removal in the OR are patient comfort, increased time efficiency, and fewer risks to the operator. This additional trip contributed to a cost of approximately $1200, making treatment with arch bars more expensive when considering the costs of application and removal in the operating room.
With an average cost of $26,000 USD per patient, emphasis on reducing costs to both the patient and the provider is of great interest for treatment of mandible fractures(1). Generally, opening an operating room for a case incurs a fee in addition to the requisite personnel, anesthesia, and supply fees. Furthermore, reserving an operating room for removal of arch bars places this room (which can potentially be used for other cases) out of commission. Even though arch bar removal may only require 15 minutes, turnaround time increases this total to well over an hour. The allocation of operating room personnel and other resources for this secondary removal procedure is not cost-effective.
The use of Erich arch bars and MMF screws each present advantages and disadvantages, yet both have been reported to be equally effective for closed treatment of minimally displaced and favorable mandible fractures (15, 16). Fixation screws cannot provide stability to an alveolar ridge fracture or affected dentition as an arch bar. Although we are only referring to closed treatment of mandible fractures in this study, arch bars can be used as a tension band when internal fixation is required; MMF screws cannot be used in this fashion(17). For unfavorable or grossly displaced fractures, it may be prudent to use arch bars and ideally, internal fixation. Additionally, in cases where compromised occlusion is present, arch bars may provide better fixation. Screws allow for better dental hygiene while MMF is in place, as well as reduction in the incidence of periodontal damage that can be seen with arch bar use (2, 14). Still, tooth root injury is reported to occur with an incidence of about 4–6.5% in patients that undergo placement of MMF screws (10, 16). By using direct visualization in line with the long axis of the screw, more accurate placement between tooth roots can be achieved. If the operator’s visual line is at a different angle than the long axis, improper placement may occur. On evaluation of postoperative orthopantograms, tooth root injury occurred in 1 of 15 patients in our population.
Fixation with MMF screws is not without its own complications. With chronic, repeated stress, MMF screws can lose their purchase in bone and adequate immobilization may be lost. One study advises caution, as long term fixation (greater than 5 weeks) with screws may not be as efficacious as that with arch bars due to screw loosening(9). Repeated stress can also loosen wire fixation of arch bars. Meticulous attention to application of MMF fixation screws can ensure reduction in the incidence of screw loosening and subsequent loss of fixation. Placement perpendicular to bone with a conscious effort to minimize yaw will ensure that the hole created with the self-drilling screws will have optimal purchase and minimal potential for screw movement. Correct placement of screws is critical to maintaining appropriate occlusion with pre-stretched wires through the immobility period. Fractures that result in a posterior open bite may benefit from more distal placement of MMF screws (between second premolar and molar). Mesial placement of MMF screws may provide better fixation for fractures that result in an anterior open bite.
Limitations of our study include the variability of surgeons performing these procedures. As mentioned previously, all of the surgeons were plastic surgery trained. Twenty-one different attending surgeons and numerous residents performed these fixations over the past twelve years. Discrepancies in technique could not be controlled for in this study, leading to wide variability in the timing of MMF application. Additionally, in comparison to other studies, the average length of arch bar application was higher, likely due to trainee involvement in the procedures. Limitations also include the inability to robustly analyze any complications, as there was no standardized protocol for postoperative care or imaging. This study, therefore, is limited in scope to focus on costs and operative time, and cannot strongly discuss complications or outcomes on these patients. These factors have previously been evaluated in the literature (9, 13–16).
Conclusion
Based on our study data, MMF screws were found to be more cost effective than arch bars. Cost savings were noted most significantly in a decreased need for secondary procedures in patients who were treated with MMF screws. Screw fixation offers potential for reducing the costs of care in treating patients with mandible fractures. MMF screws can potentially be placed in the ER or in clinic for patients with simple mandibular fractures, precluding fees associated with the operating room. Similar to correct placement of arch bars, MMF screw placement requires proper training and skill necessary for successful outcome and avoiding dental injury. Arch bars and MMF screws obtain good outcomes; however, the use of screws in minimally displaced or favorable fractures reduces OR time and the need for secondary procedures.
With increased focus on the economy of healthcare, MMF screws represent an attractive, cost-effective alternative to fixation with arch bars in patients with simple mandibular fractures.
Acknowledgments
Research reported in this publication was supported by the Washington University Institute of Clinical and Translational Sciences grant UL1 TR000448 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH) and the Children’s Discovery Institute. The content is solely the responsibility of the authors and does not necessarily represent the official view of the NIH.
Footnotes
Scott J Farber, MD, Title: Resident in Plastic and Reconstructive Surgery, Affiliation: Washington University in St. Louis Division of Plastic and Reconstructive Surgery, farbers@wudosis.wustl.edu, Role: This author helped design the study, conduct the study, analyze the data, and write the manuscript, Conflicts: Scott J Farber reported no conflicts of interest, Attestation: Scott J Farber has seen the original study data, reviewed the analysis of the data, approved the final manuscript, and is the first and corresponding author
Alison K Snyder-Warwick, MD, Title: Assistant Professor of Plastic and Reconstructive Surgery, Affiliation: Washington University in St. Louis Division of Plastic and Reconstructive Surgery, snyderak@wudosis.wustl.edu, Role: This author helped write the manuscript, Conflicts: Alison K Snyder-Warwick reported no conflicts of interest, Attestation: Alison K Snyder-Warwick has seen the original study data, reviewed the analysis of the data, approved the final manuscript
Gary B Skolnick, BS, Title: Senior Data Analyst, Affiliation: Washington University in St. Louis Division of Plastic and Reconstructive Surgery, skolnickg@wudosis.wustl.edu, Role: This author helped analyze the data and write the manuscript, Conflicts: Gary B Skolnick reported no conflicts of interest, Attestation: Gary B Skolnick has seen the original study data, reviewed the analysis of the data, approved the final manuscript
Albert S Woo, MD, Title: Assistant Professor of Plastic and Reconstructive Surgery, Affiliation: Washington University in St. Louis Division of Plastic and Reconstructive Surgery, wooa@wudosis.wustl.edu, Role: This author helped analyze the data and write the manuscript, Conflicts: Albert S Woo is a consultant for Osteomed, however does not receive royalties and reported no conflicts of interest, Attestation: Albert S Woo has seen the original study data, reviewed the analysis of the data, and approved the final manuscript
Kamlesh B Patel, MD, Title: Assistant Professor of Plastic and Reconstructive Surgery, Affiliation: Washington University in St. Louis Division of Plastic and Reconstructive Surgery, patelk@wudosis.wustl.edu, Role: This author helped design the study, conduct the study, analyze the data, and write the manuscript, Conflicts: Kamlesh B Patel reported no conflicts of interest, Attestation: Kamlesh B Patel has seen the original study data, reviewed the analysis of the data, approved the final manuscript, and is the senior author
Financial Disclosures: Dr. Patel is a consultant for Stryker CMF. Dr. Woo is a consultant for Osteomed. The other authors have no conflicts of interest to report.
References
- 1.Nalliah RP, Allareddy V, Kim MK, et al. Economics of facial fracture reductions in the United States over 12 months. Dental traumatology: official publication of International Association for Dental Traumatology. 2013;29:115–120. doi: 10.1111/j.1600-9657.2012.01137.x. [DOI] [PubMed] [Google Scholar]
- 2.Ayoub AF, Rowson J. Comparative assessment of two methods used for interdental immobilization. Journal of cranio-maxillo-facial surgery: official publication of the European Association for Cranio-Maxillo-Facial Surgery. 2003;31:159–161. doi: 10.1016/s1010-5182(03)00022-2. [DOI] [PubMed] [Google Scholar]
- 3.Schneider AM, David LR, DeFranzo AJ, et al. Use of specialized bone screws for intermaxillary fixation. Ann Plast Surg. 2000;44:154–157. doi: 10.1097/00000637-200044020-00005. [DOI] [PubMed] [Google Scholar]
- 4.Park KN, Oh SM, Lee CY, et al. Design and application of hybrid maxillomandibular fixation for facial bone fractures. J Craniofac Surg. 2013;24:1801–1805. doi: 10.1097/SCS.0b013e3182a21163. [DOI] [PubMed] [Google Scholar]
- 5.Rowe NL. The history of the treatment of maxillo-facial trauma. Annals of the Royal College of Surgeons of England. 1971;49:329–349. [PMC free article] [PubMed] [Google Scholar]
- 6.Rowe NLKHC. Fractures of the facial skeleton. Baltimore: Williams and Wilkins; 1955. [Google Scholar]
- 7.Avery CM, Johnson PA. Surgical glove perforation and maxillofacial trauma: to plate or wire? The British journal of oral & maxillofacial surgery. 1992;30:31–35. doi: 10.1016/0266-4356(92)90133-4. [DOI] [PubMed] [Google Scholar]
- 8.Nandini GD, Balakrishna R, Rao J. Self Tapping Screws v/s Erich Arch Bar for Inter Maxillary Fixation: A Comparative Clinical Study in the Treatment of Mandibular Fractures. J Maxillofac Oral Surg. 2011;10:127–131. doi: 10.1007/s12663-011-0191-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rai A, Datarkar A, Borle RM. Are maxillomandibular fixation screws a better option than Erich arch bars in achieving maxillomandibular fixation? A randomized clinical study. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 2011;69:3015–3018. doi: 10.1016/j.joms.2010.12.015. [DOI] [PubMed] [Google Scholar]
- 10.Coletti DP, Salama A, Caccamese JF., Jr Application of intermaxillary fixation screws in maxillofacial trauma. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 2007;65:1746–1750. doi: 10.1016/j.joms.2007.04.022. [DOI] [PubMed] [Google Scholar]
- 11.Roccia F, Rossi P, Gallesio C, et al. Self-tapping and self-drilling screws for intermaxillary fixation in management of mandibular fractures. J Craniofac Surg. 2009;20:68–70. doi: 10.1097/SCS.0b013e318190df2f. [DOI] [PubMed] [Google Scholar]
- 12.Bissada E, Abou-Chacra Z, Ahmarani C, et al. Intermaxillary screw fixation in mandibular fracture repair. Journal of otolaryngology - head & neck surgery = Le Journal d'oto-rhino-laryngologie et de chirurgie cervico-faciale. 2011;40:211–215. [PubMed] [Google Scholar]
- 13.Ingole PD, Garg A, Shenoi SR, et al. Comparison of intermaxillary fixation screw versus eyelet interdental wiring for intermaxillary fixation in minimally displaced mandibular fracture: a randomized clinical study. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 2014;72:958.e951–957. doi: 10.1016/j.joms.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 14.West GH, Alan Griggs J, Chandran R, et al. Treatment Outcomes With the Use of Maxillomandibular Fixation Screws in the Management of Mandible Fractures. Journal of Oral and Maxillofacial Surgery. 2014;72:112–120. doi: 10.1016/j.joms.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 15.Coburn DG, Kennedy DW, Hodder SC. Complications with intermaxillary fixation screws in the management of fractured mandibles. The British journal of oral & maxillofacial surgery. 2002;40:241–243. doi: 10.1054/bjom.2001.0771. [DOI] [PubMed] [Google Scholar]
- 16.Hashemi HM, Parhiz A. Complications Using Intermaxillary Fixation Screws. Journal of Oral and Maxillofacial Surgery. 2011;69:1411–1414. doi: 10.1016/j.joms.2010.05.070. [DOI] [PubMed] [Google Scholar]
- 17.Ellis E, 3rd, Miles BA. Fractures of the mandible: a technical perspective. Plast Reconstr Surg. 2007;120:76S–89S. doi: 10.1097/01.prs.0000260721.74357.e7. [DOI] [PubMed] [Google Scholar]


