Abstract
Purpose:
Emergency hip surgery generally has worse outcomes than elective hip surgery, even when adjusted for patient and surgical factors. Do-not-resuscitate (DNR) status patients are typically at higher perioperative risk and undergo a narrow range of surgical procedures. We aimed to compare the outcomes after hip surgery of differing degrees of urgency in this cohort.
Materials and Methods:
Using National Surgical Quality Improvement Program (NSQIP) data, we conducted univariate and multivariate analyses comparing outcomes of DNR status patients after emergency and nonemergency hip surgery (2007-2013). We conducted a subanalysis of mortality in elective versus nonelective cases (elective variable introduced from 2011).
Results:
Of 668 hip surgery cases in DNR status patients, 210 (31.4%) were emergency and 458 (68.8%) were nonemergency. There were no significant associations between emergency and nonemergency surgery regarding patient demographics, comorbidities, functional capacity, anesthesia type, or operative duration. There was no significant difference in the 30-day postoperative mortality between emergency (21.4%) and nonemergency (16.4%) or between elective (19.6%) and nonelective (18.3%) hip fracture surgeries performed in patients with preexisting DNR status. Morbidity patterns in emergency vs nonemergency cases demonstrated no significant differences, with the commonest 3 complications being transfusion (21.0% and 21.4%, respectively), urinary tract infection (9.5% and 7.9%, respectively), and pneumonia (both at 5.2%). The 30-day home discharge rates were low at 4.7% and 5.6%, respectively. Multivariate analysis demonstrated no significant associations between emergency and nonemergency surgery for mortality, discharge destination, length of stay or complications, except perioperative myocardial infarction (3.7% vs 1.3%, P < .04).
Conclusion:
For patients with DNR status, both emergent and non-emergent hip surgery carries high mortality, greatly exceeding rates predicted for that patient by American College of Surgeons NSQIP risk calculators. Morbidity rates and patterns for patients with DNR status are also similar in emergency and nonemergency groups. These data may be useful in discussing risk and obtaining adequately informed consent in DNR patients undergoing hip surgery.
Keywords: hip surgery, hip fracture, do not resuscitate, informed consent, emergency, elective, DNR
Introduction
Urgent and elective hip surgeries are common procedures in the elderly individuals. However, in general, outcomes are worse for emergency or urgent hip surgery than for elective hip surgery.1,2 Multiple factors contribute, including differences in the baseline patient demographic, comorbidities, and the types of surgery required.3,4 The elderly population is growing, while the incidence of surgery in the elderly individuals is increasing. Additionally, the spread of surgical procedures narrows with increasing age. The most common surgical procedures in the elderly individuals are orthopedic, namely, elective knee arthroplasty in 65- to 84-year-olds and urgent treatment of hip fracture or dislocation in those older than 85 years.5,6 The ratio of emergency to elective procedures performed also increases with increasing age.7
Do-not-resuscitate (DNR) status is implemented either on patient preference or when the responsible physician expects cardiopulmonary resuscitation to be medically futile due to multiple comorbidities or end-stage disease. The DNR status has therefore been considered a potential surrogate marker for short life expectancy and is associated with poor surgical outcomes. However, up to 15% of patients who have DNR status do undergo surgical procedures each year.8 It is unknown exactly which surgeries are most commonly performed in patients with DNR status; however, hip surgery may be expected to form a substantial group. Outcomes in this specific DNR group are currently unknown.
Patients with DNR orders undergoing emergency or nonelective hip surgery are likely to score highly for predicted postoperative mortality and morbidity, although no models exist that take DNR status into account. Because nonsurgical management carries ongoing, overwhelming risk of mortality and morbidity, hip fracture is rarely managed conservatively.9 High degrees of risk may therefore be reasonably tolerated. However, to obtain an adequate informed consent, likely risk must still be evaluated, disclosed to the patient or family, and managed expectantly by the hospital team. In contrast to nonelective hip surgery, elective hip surgeries aim to improve the quality of life by relieving symptoms, although a nonsurgical management may be a reasonable alternative in high-risk patients.10 In patients with DNR orders undergoing elective procedures, relevant cohort-specific, patient-centered outcome data are needed to consider risk versus benefit prior to surgery.
The outcomes for patients with DNR orders undergoing hip surgery have not been studied previously. We hypothesized that patients with DNR status undergoing emergency or nonelective hip surgery have worse outcomes than those undergoing nonemergency or elective hip surgery. Here, we report outcomes of patients with DNR status undergoing emergency and nonemergency hip surgery including a subset analysis comparing elective with nonelective surgery.
Methods
Data Source
The American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) is a data registry consisting of cases reported from approximately 400 participating sites. The ACS-NSQIP has been well validated with data entry overseen by a designated surgical clinical reviewer at each site.11 Full details regarding variables and their definitions are provided by NSQIP.12 Institutional review board (Brigham and Women’s Hospital, Boston, Massachusetts) approval was obtained for analysis of the data and was exempted from the consent requirement due to the deidentified nature of the data.
Outcomes
Patients were included in the study if a DNR order was present, per the wording provided in the NSQIP Participant Use Data File:
If the patient has had a Do-Not-Resuscitate (DNR) order written in the physician’s order sheet of the patient’s chart and it has been signed or co-signed by an attending physician, enter “YES.” There must be active DNR order at the time the patient is going to the OR. However, if the DNR order, as defined above, was rescinded immediately prior to surgery, in order to operate on the patient, enter “YES.”
Patient’s data were excluded if Current Procedural Terminology (CPT) or DNR status was not reported.
Study Sample
The 2007 to 2013 NSQIP data were compiled into a single file containing 306 variables across 2.8 million surgical cases. All cases of patients under age 18 at the time of operation, trauma, and transplant surgeries and all cases where the patient is listed with an American Society of Anesthesiologists physical status (ASA PS) class 6, representing a brain-dead organ donor, were excluded from the NSQIP. All cases failing to report the do-not-resuscitate variable were excluded from the analysis. Given these criteria, a total of 1 585 453 cases were included in our analysis.
We isolated all admissions for hip surgery using CPT codes: 27125 (Hemiarthroplasty, hip, partial [eg, femoral stem prosthesis, bipolar arthroplasty]), 27130 (Arthroplasty, acetabular and proximal femoral prosthetic replacement [total hip arthroplasty], with or without autograft or allograft), 27132 (Conversion of previous hip surgery to total hip arthroplasty, with or without autograft or allograft), 27134 (Revision of total hip arthroplasty; both components, with or without autograft or allograft), 27136 (Open treatment of femoral fracture, proximal end, neck, internal fixation, or prosthetic replacement), 27137 (Revision of total hip arthroplasty; acetabular component only, with or without autograft or allograft), and 27138 (Revision of total hip arthroplasty; femoral component only, with or without allograft). This yielded a total of 668 hip surgeries performed in patients with a DNR order.
Emergency surgery is defined by ACS-NSQIP as “YES” if the surgeon and anesthesiologist report the case as emergent. ACS-NSQIP defines an “emergency case” as a case “usually performed within a short interval of time between patient diagnosis or the onset of related preoperative symptomatology. It is implied that the patient’s well-being and outcome is potentially threatened” by any unnecessary delay. The NSQIP undergoes dynamic review and development, and in 2011, an additional data point regarding scheduling (“Elective?”: Yes/No) was added to NSQIP’s Participant Use Files. Consequently, we compared emergency and nonemergency cases between 2007 and 2013 and additionally compared elective and nonelective cases between 2011 and 2013, inclusive.
Patient demographic data were collected for age, ASA PS classification, sex, race, Hispanic ethnicity, height, weight, body mass index (BMI), and surgical relative value units and surgical service. Preoperative comorbidity data were collected for functional status prior to surgery (activities of daily living [ADLs]), baseline dyspnea, diabetes mellitus (insulin and noninsulin dependent); smoking status; and presence of chronic obstructive pulmonary disease, congestive heart failure, coronary artery disease (a composite of a history of angina, myocardial infarction [MI], percutaneous coronary interventions, or cardiac surgery), hypertension, chronic kidney disease, cerebrovascular accidents, preoperative weight loss of greater than 10% in the previous 6 months, sepsis physiology, and previous operation within the past 30 days.
Data regarding the surgical procedure were collected for the primary surgical procedure CPT code, surgical resident postgraduate year, surgical wound classification, total anesthesia, and surgical control time and anesthesia type.
To identify whether various preoperative demographic and comorbidity variables or surgical factors were independent risk factors associated with emergency surgery, a univariate logistic regression model was fitted for all preoperative variables. Risk factors were defined as statistically significant with odds ratios (ORs) not including 1.00 in their 95% confidence interval (CI), representing an α of <.05.
We collected the following outcomes, with 30-day follow-up: death, return to the operating room (within 30 days for any reason), and, in a binary format, the following complications: superficial and deep space surgical site infections, postoperative pneumonia, unplanned intubation, failure to wean from the ventilator, progressive renal insufficiency and acute renal failure requiring dialysis, urinary tract infections, cerebrovascular accidents, MI, postoperative bleeding requiring transfusion of packed red blood cells, deep venous thrombosis requiring therapy, pulmonary embolism, and postoperative sepsis. Discharge destination (home, skilled care, or rehabilitation facility) and total length of stay were also collected. All outcomes were reported as percentages, with the numerator defined as the absolute count reporting a given outcome and the denominator defined as the total number of cases reporting any outcome for that variable. To assess for the association between surgery schedule and adverse outcomes, both univariate regression and multivariate regression were performed. For the logistic regression, ORs were reported with their associated 95% CIs. The ORs not including 1.00 in their 95% CIs were considered statistically significant.
Statistical Analysis
R Project for Statistical Computing (R version 3.2.3) was used to perform all statistical analysis. Differences between cohorts were assessed using the Pearson χ2 test for categorical variables and using the Student’s t test for continuous variables.
Based on sensitivity analysis, and using an α of .05, 2 tail function, and our total sample size of 666, we have 90% power to detect an effect size of 0.016 (1.6%). Calculations were performed using G*Power.13
Results
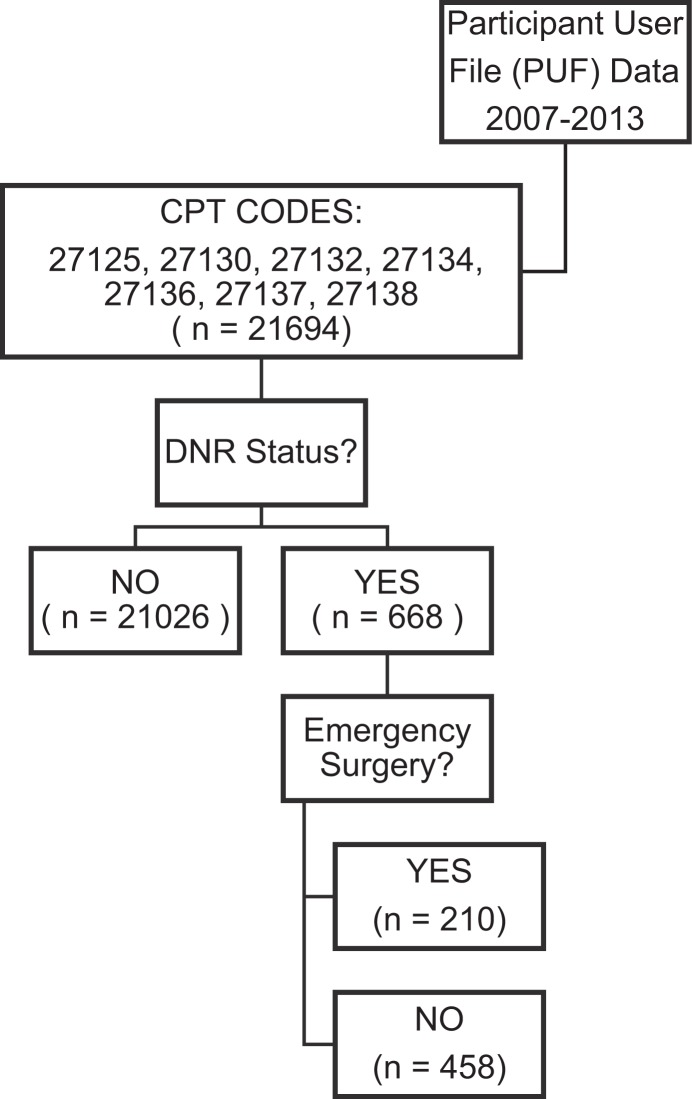
The ACS-NSQIP 2007 to 2013 Participant User Files (PUFs) yielded 668 patients with DNR status undergoing hip surgery (Figure 1). Of these, 210 (31.4%) cases were emergency and 458 (68.8%) were nonemergency.
Figure 1.
Flow diagram of the inclusion criteria yielding study population: do-not-resuscitate (DNR) status patients undergoing emergency and nonemergency hip surgery.
Hip surgery was more common in females than males, both for emergency (71.9% vs 28%) and nonemergency surgery (73.2% vs 26.8%), as shown in Table 1. However, there was no significant association between gender and undergoing emergency versus nonemergency surgery. Patients listing ethnicity as “other” were significantly more likely to undergo emergency surgery than patients listing ethnicity as “white” (OR: 2.84 [95% CI: 2.01-4.01]). Mean age was slightly higher for emergency patients, at 85.8 (standard deviation [SD] 5.6) versus 84.7 (SD 6.9), P = .03. The >80 age-groups comprised 89% of those undergoing emergency surgery and 82.8% of those undergoing nonemergency surgery. Compared to those younger than 65 years, increasing age was not significantly associated with increased likelihood of surgery being emergency versus nonemergency: for 65 to 80 years, OR 1.52 (0.31-7.5) and for >80 years, OR 2.47 (0.54-11.37).
Table 1.
Patients With DNR Status Undergoing Emergency and Nonemergency Hip Surgery: Demographics and Comorbidities.
| Demographics | Emergency | Nonemergency | Univariate Regression | ||
|---|---|---|---|---|---|
| n | % | n | % | OR (95% CI) | |
| Male | 59 | 28.10 | 122 | 26.75 | 1.07 (0.74-1.54) |
| Female | 151 | 71.91 | 334 | 73.25 | Reference |
| White | 95 | 45.24 | 321 | 70.09 | Reference |
| Black | 1 | 0.48 | 4 | 0.87 | 0.84 (0.09-7.65) |
| Asian | 1 | 0.48 | 1 | 0.22 | 3.38 (0.21-54.54) |
| Other | 106 | 50.48 | 126 | 27.51 | 2.84 (2.01-4.01) |
| Hispanic ethnicity | 2 | 0.95 | 2 | 0.44 | 3.2 (0.45-23.03) |
| Age | |||||
| Mean (SD) | 85.8 (5.6) | 84.7 (6.9) | P = .0265 | ||
| <65 | 2 | 0.95 | 10 | 0.02 | Reference |
| 65-80 | 21 | 10.00 | 69 | 0.15 | 1.52 (0.31-7.5) |
| >80 | 187 | 89.05 | 379 | 0.83 | 2.47 (0.54-11.37) |
| BMI | |||||
| Mean (SD) | 23.84 (5.3) | 24.21 (5.6) | P = .4894 | ||
| <18.5 | 17 | 8.10 | 39 | 0.09 | 1.11 (0.59-2.08) |
| 18.5-25 | 74 | 35.24 | 188 | 0.41 | Reference |
| 25-30 | 32 | 15.24 | 90 | 0.20 | 0.9 (0.56-1.47) |
| >30 | 16 | 0.08 | 42 | 0.09 | 0.97 (0.51-1.83) |
| Functional capacity | |||||
| No dyspnea | 178 | 84.76 | 395 | 86.25 | Reference |
| Dyspnea moderate exertion | 23 | 10.95 | 47 | 10.26 | 1.09 (0.64-1.84) |
| Dyspnea at rest | 9 | 4.29 | 16 | 3.49 | 1.25 (0.54-2.88) |
| ADLs—Independent | 71 | 33.81 | 189 | 41.27 | Reference |
| ADLs—Part independent | 102 | 48.57 | 206 | 44.98 | 1.32 (0.92-1.89) |
| ADLs—Total dependent | 35 | 16.67 | 61 | 13.32 | 1.53 (0.93-2.51) |
| Comorbidities | |||||
| Diabetes | 25 | 11.91 | 74 | 16.16 | 0.7 (0.43-1.14) |
| Smoker | 10 | 4.76 | 27 | 5.90 | 0.8 (0.38-1.68) |
| COPD | 22 | 10.48 | 69 | 15.07 | 0.66 (0.4-1.1) |
| CHF | 10 | 4.76 | 16 | 3.49 | 1.38 (0.62-3.1) |
| CAD | 44 | 20.95 | 76 | 16.59 | 1.33 (0.88-2.01) |
| HTN | 151 | 71.91 | 338 | 73.80 | 0.91 (0.63-1.31) |
| CKD | 5 | 2.38 | 14 | 3.06 | 0.77 (0.27-2.18) |
| CVA | 41 | 19.52 | 86 | 18.78 | 1.05 (0.69-1.59) |
| Weight loss | 9 | 4.29 | 9 | 1.97 | 2.23 (0.87-5.71) |
| Sepsis | 25 | 0.12 | 71 | 0.16 | 0.73 (0.45-1.19) |
| Prior operation last 30 days | 4 | 1.91 | 9 | 1.97 | 0.97 (0.29-3.18) |
| ASA class | |||||
| 1-2 | 12 | 5.7 | 43 | 9.39 | Reference |
| 3 | 126 | 60.00 | 291 | 63.54 | 1.55 (0.79-3.04) |
| 4 | 72 | 34.29 | 124 | 27.07 | 2.08 (1.03-4.2) |
| 5 | 0 | 0.00 | 0 | 0.00 | (0-∞) |
| Mean preoperative laboratory test results (SD) | |||||
| Creatinine | 1.04 (0.56) | 1.13 (0.83) | P = .152 | ||
| Albumin | 3.42 (0.55) | 3.41 (0.59) | P = .844 | ||
| Hematocrit | 35.93 (5.29) | 35.19 (5.11) | P = .095 | ||
| Platelets | 224.43 (87.5) | 218.2 (85.99) | P = .392 | ||
| INR | 1.15 (0.28) | 1.15 (0.29) | P = .771 | ||
| NSQIP risk calculators (SD) | |||||
| % Mortality probability | 0.12 (0.11) | 0.07 (0.08) | P < .001 | ||
| % Morbidity probability | 0.17 (0.07) | 0.13 (0.06) | P < .001 | ||
Abbreviations: ADL, activity of daily living; ASA, American Society of Anesthesiologists; CAD, coronary artery disease; CHF, congestive heart failure; CI, confidence interval; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; CVA, cerebrovascular accident; DNR, do not resuscitate; HTN, hypertension; OR, odds ratio; SD, standard deviation; NSQIP, National Surgical Quality Improvement Program; INR, interquartile range.
Emergency surgery patients had a slightly lower average BMI at 23.8 versus 24.2 kg/m2, but this was not significant (P = .49). There were no significant associations between emergency and nonemergency surgery for a range of patient factors including dyspnea on exertion or at rest, partial or full dependence for ADLs, or for the presence of comorbidities or preoperative laboratory values. Compared to ASA 1 to 2 patients, ASA 4 (2.08 [1.03-4.2]) were slightly more likely to undergo emergency than nonemergency surgery; however, this association was not present for ASA 3 patients.
The different case mixes of emergency and nonemergency surgery cases are demonstrated in Table 2. Emergency surgery cases were most likely to be either “Open treatment of femoral fracture, proximal end, neck, internal fixation, or prosthetic replacement” (OR: 3.74, CI: 1.62-8.62) or “Hemiarthroplasty, hip, partial” (eg, femoral stem prosthesis and bipolar arthroplasty; OR: 2.95, CI: 1.29-6.76). However, there was no association between emergency surgery and preoperative wound contamination (clean, contaminated, or dirty/infected) and type of anesthesia used (spinal vs general anesthesia) and no significant difference in time spent under anesthesia, operative time, or seniority of operating surgical resident.
Table 2.
Patients With DNR Status Undergoing Emergency and Nonemergency Hip Surgery: Operative and Anesthetic Factors.
| Emergency | Nonemergency | Univariate Regression | |||
|---|---|---|---|---|---|
| n | % | n | % | OR (95% CI) | |
| Surgical procedure: CPT | |||||
| 27125 | 93 | 44.29 | 160 | 34.93 | 3.74 (1.62-8.62) |
| 27130 | 7 | 3.33 | 45 | 9.83 | Reference |
| 27132 | 0 | 0.00 | 5 | 1.09 | 0 (0-∞) |
| 27134 | 1 | 0.48 | 9 | 1.97 | 0.71 (0.08-6.54) |
| 27136 | 107 | 50.95 | 233 | 50.87 | 2.95 (1.29-6.76) |
| 27137 | 0 | 0.00 | 3 | 0.66 | 0 (0-∞) |
| 27138 | 2 | 0.95 | 3 | 0.66 | 4.29 (0.6-30.38) |
| Wound class | |||||
| 1—Clean | 205 | 97.62 | 452 | 98.69 | Reference |
| 2—Clean/contaminated | 2 | 0.95 | 4 | 0.87 | 1.1 (0.2-6.07) |
| 3—Contaminated | 0 | 0.00 | 0 | 0.00 | (0-∞) |
| 4—Dirty/infected | 3 | 1.43 | 2 | 0.44 | 3.31 (0.55-19.94) |
| Anesthesia type | |||||
| General | 123 | 0.59 | 296 | 0.65 | Reference |
| Spinal | 83 | 0.40 | 156 | 0.34 | 1.6 (0.44-5.78) |
| Other | 4 | 0.02 | 6 | 0.01 | 1.28 (0.91-1.8) |
| Resident level | |||||
| Mean postgraduate year (SD) | 4.7 (1.9) | 4.29 (2.13) | P = .245 | ||
| Operating Room times | |||||
| Mean anesthesia time (SD) | 134.58 (83.66) | 131.94 (57.31) | P = .636 | ||
| Mean surgical time (SD) | 73.19 (39.71) | 76.32 (61.32) | P = .498 | ||
Abbreviations: CI, confidence interval; CPT, Current Procedural Terminology; DNR, do not resuscitate; OR, odds ratio; SD, standard deviation.
The 30-day mortality was higher at 21.4% for emergency surgery compared to 16.4% for nonemergency surgery (Table 3). However, there was no significant association demonstrated between emergency or nonemergency surgery and mortality. Of emergency and nonemergency patients at 30-day follow-up, 4.8% and 5.8% had been discharged home, 21.4% and 19.0% to skilled care, and 7.8% and 11.0% to rehabilitation. Again, discharge destination was not associated with emergency rather than nonemergency surgery.
Table 3.
Patients With DNR Status Undergoing Emergency and Nonemergency Hip Surgery: Outcomes.
| Emergency | Nonemergency | Univariate Regression OR (95% CI) | Multivariate Regression OR (95% CI) | |||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Death | 45 | 21.43 | 75 | 16.38 | 1.39 (0.92-2.1) | 1.39 (0.9-2.15) |
| Discharge destination | ||||||
| Home | 10 | 4.76 | 26 | 5.68 | Reference | Reference |
| Skilled care | 45 | 21.43 | 87 | 19.00 | 1.34 (0.6-3.03) | 0.74 (0.3-1.85) |
| Rehab | 16 | 7.62 | 50 | 10.92 | 0.83 (0.33-2.09) | 0.48 (0.17-1.33) |
| Reoperations | ||||||
| Return to Operating Room | 5 | 2.38 | 18 | 3.93 | 0.6 (0.22-1.63) | 0.59 (0.21-1.64) |
| Complications | ||||||
| Superficial SSI | 1 | 0.48 | 7 | 1.53 | 0.31 (0.04-2.52) | 0.34 (0.04-2.83) |
| Organ/space SSI | 1 | 0.48 | 3 | 0.66 | 0.73 (0.08-7.02) | 1.02 (0.09-11.4) |
| Pneumonia | 11 | 5.24 | 24 | 5.24 | 1 (0.48-2.08) | 0.79 (0.37-1.7) |
| Unplanned intubation | 3 | 1.43 | 4 | 0.87 | 1.64 (0.36-7.42) | 1.72 (0.36-8.25) |
| Failure to wean | 2 | 0.95 | 2 | 0.44 | 2.19 (0.31-15.67) | 1.9 (0.26-14.05) |
| Acute kidney injury | 1 | 0.48 | 3 | 0.66 | 0.73 (0.08-7.02) | 0.68 (0.07-6.98) |
| Dialysis | 2 | 0.95 | 1 | 0.22 | 4.39 (0.4-48.73) | 3.16 (0.28-35.86) |
| Urinary tract infection | 20 | 9.52 | 36 | 7.86 | 1.23 (0.7-2.19) | 1.15 (0.64-2.08) |
| CVA | 1 | 0.48 | 3 | 0.66 | 0.73 (0.08-7.02) | 1.4 (0.11-17.91) |
| Myocardial infarction | 8 | 3.81 | 6 | 1.31 | 2.98 (1.02-8.71) | 2.61 (0.88-7.73) |
| Transfused (intra/post) | 44 | 20.95 | 98 | 21.40 | 0.97 (0.65-1.45) | 1.03 (0.68-1.56) |
| DVT | 3 | 1.43 | 5 | 1.09 | 1.31 (0.31-5.55) | 1.49 (0.34-6.48) |
| Pulmonary embolism | 1 | 0.48 | 5 | 1.09 | 0.43 (0.05-3.73) | 0.4 (0.05-3.5) |
| Composite sepsis | 5 | 2.38 | 8 | 1.75 | 1.37 (0.44-4.25) | 1.08 (0.34-3.39) |
| Admission, days | ||||||
| Mean Operation to discharge (SD) | 8.22 (9.66) | 6.92 (6.77) | P = .046 | |||
| Mean length of stay (SD) | 9.38 (9.81) | 8.98 (9.19) | P = .617 | |||
Abbreviations: CI, confidence interval; CVA, cerebrovascular accident; DNR, do-not-resuscitate; DVT, deep venous thrombosis; OR, odds ratio; SSI, surgical site infection.
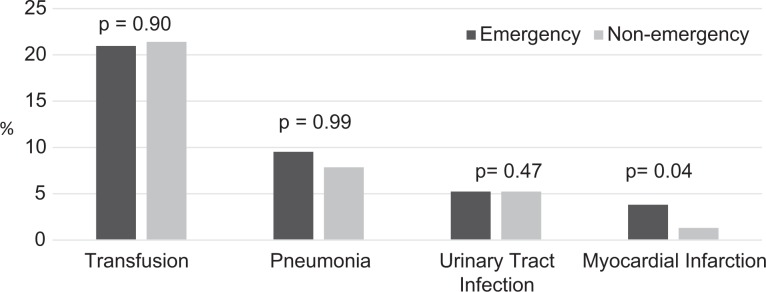
The most common complications after emergency and nonemergency patients were transfusion (21.0% and 21.4%, respectively, P = .90), urinary tract infection (9.5% and 7.9%, respectively, P = .99), and pneumonia (5.2% in both groups, P = 0.47) and MI (3.7% and 1.3%, P < .04). Therefore, only MI demonstrated significance when comparing rates in emergency and nonemergency patients (Figure 2). Despite having DNR status preoperatively, a total of 7 patients underwent unplanned intubation, 4 failed to wean from intubation, and 3 started dialysis. Mean time from surgery to discharge was significantly longer at 8.22 (SD 9.66) days for emergency surgery versus 6.92 (SD 6.77) days for nonemergency surgery, P < .05. However, total mean length of stay was not significantly longer at 9.38 (SD 9.81) days for emergency surgery versus 8.98 (SD 9.19) days for nonemergency surgery, P = .62.
Figure 2.
Most common complications (%) in patients with do-not-resuscitate (DNR) status undergoing emergency and nonemergency hip surgery.
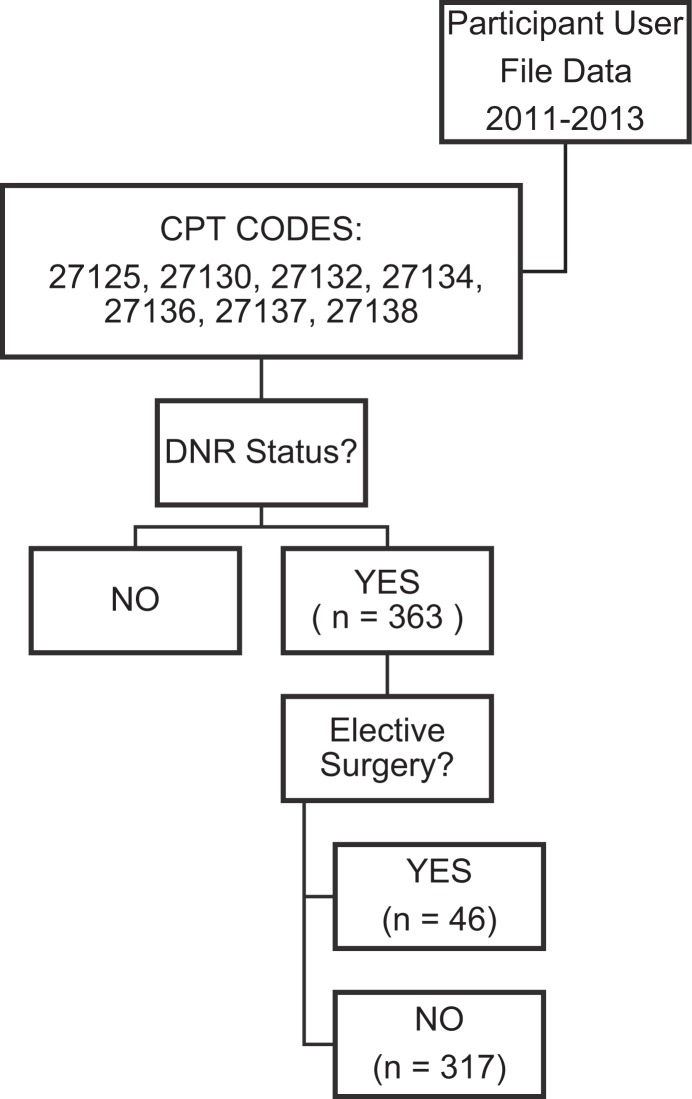
We also analyzed a subgroup for whom data on “elective” versus “nonelective” were also collected (Figure 3). From 2011 to 2013, 363 patients with DNR status underwent hip surgery, of which 46 were coded as elective and 317 were coded as nonelective. Multivariate regression analysis demonstrated no significant associations with mortality or discharge destination for nonelective versus elective hip surgery patients with DNR status (Table 4). The 30-day mortality was 19.6% and 18.3% for elective and nonelective cases, respectively. Discharge home within 30 days occurred in 19.6% and 8.5% of elective and nonelective cases, respectively. Discharge to rehab within 30 days occurred in 17.4% and 18.3% of elective and nonelective cases, respectively. Discharge to skilled care homes within 30 days occurred in 39.1% and 36.0% of elective and nonelective cases, respectively. However, average surgery to discharge time was shorter for elective 6.04 days (SD 3.89) versus nonelective surgery 9.19 days (SD 9.06) in DNR patients (P = .02). Average total length of stay was also shorter after elective surgery, at 7.0 days (SD 4.01) versus 11.3 days (SD 11.28), P = .01.
Figure 3.
Flow diagram of the inclusion criteria yielding study population: patients with do-not-resuscitate (DNR) status undergoing elective and nonelective hip surgery
Table 4.
Patients With DNR Status Undergoing Elective and Nonelective Hip Surgery: Outcomes.
| Elective | Nonelective | Univariate Regression | Multivariate Regression | |||
|---|---|---|---|---|---|---|
| n | % | n | % | OR (95% CI) | OR (95% CI) | |
| Outcomes | ||||||
| Death | 9 | 19.6 | 58 | 18.3 | 1.06 (0.48-2.31) | 1.2 (0.53-2.71) |
| Home | 9 | 19.6 | 27 | 8.5 | Reference | Reference |
| Skilled care, not home | 18 | 39.1 | 114 | 36.0 | 0.47 (0.19-1.17) | 0.63 (0.22-1.79) |
| Rehab | 8 | 17.4 | 58 | 18.3 | 0.41 (0.14-1.19) | 0.52 (0.16-1.69) |
| Mean duration, days | ||||||
| Surgery to discharge (SD) | 6.04 (3.89) | 9.19 (9.06) | P = .021 | |||
| Total length of stay (SD) | 7.0 (4.01) | 11.3 (11.28) | P = .011 | |||
Abbreviations: CI, confidence interval; DNR, do not resuscitate; OR, odds ratio; SD, standard deviation.
Discussion
In this study we describe, for the first time, the specific outcomes experienced by patients with DNR status undergoing emergency and nonemergency hip surgeries. The 30-day mortality was high in both groups at 21.4% and 16.4%, respectively, and the most common complications after both emergency and nonemergency surgeries were transfusion requirement, urinary tract infection, pneumonia, and MI. However, none of our outcomes, including 30-day mortality, length of stay, or any the complications except perioperative MI, were significantly higher or more likely in emergency than nonemergency patients. This suggests risk in emergency and nonemergency surgery may be more similar than expected for patients with DNR status than in the wider demographic. Our unexpected findings are in contrast to several studies demonstrating higher risk in emergency versus nonemergency surgeries across a range of surgical specialties, including orthopedic surgery and specifically hip surgery.2,14,15
The emergency and nonemergency groups were broadly comparable in terms of demographic and patient factors, with two exceptions. We were unable to account for the patterns of ethnicity in patients undergoing emergency versus nonemergency care, specifically for patients categorized as “white” versus “other.” It could relate to more general socioeconomic and ethnic variation in access to scheduled and unscheduled health care. However, as the ethnic categorization of “other” may comprise small numbers of a highly diverse patient group, it would be difficult to draw comparisons against it. This, along with increased likelihood of being ASA PS grade 4, was one of the few demographic differences demonstrated between the patient groups undergoing emergency and nonemergency care.
A major limitation of our data set was the change in coding practice to introduce an “elective surgery?” variable in 2011, in addition to the “emergency surgery?” variable. Prior to 2011, only data regarding emergency or nonemergency surgery were available. Cases are coded in NSQIP as “emergency” if a surgeon or anesthesiologist schedules the case as such, though the intention is that this category denotes cases occurring within a short period of time. The most common surgery performed for both emergency and nonemergency cases was “hip replacement for fracture,” at approximately 50% each. This provides evidence of variation as to whether hip fracture surgery was documented as emergency or urgent, and urgent surgery is not currently an NSQIP-coded variable. It is not possible to determine whether classification as “emergency” was on clinical grounds, for example, neurovascular compromise, or for scheduling purposes, in an attempt to meet institutional or national guideline-based admission to surgery time targets. This may lead to crossover between the two groups studied and could be a confounding factor. It is possible that there is a degree of subjectivity or local practice in labeling “emergent” versus “nonemergent.” Therefore, “elective” versus “nonelective,” which has now been adopted, may be more suitable coding.
To attempt to address this potential confounding factor, we performed a second analysis of 363 patients from 2011 to 2013, for whom elective or nonelective status could be determined. While this provided a smaller group of patients to study, the findings were consistent with the comparison of emergency and nonemergency surgery patients. Mortality approached 20% in both elective and nonelective groups, rates of discharge home or to normal place of care were low, and transfer to skilled care was high. However, we failed to demonstrate significant differences between elective and nonelective DNR patients undergoing hip surgery, neither in terms of mortality nor discharge home versus care facilities. There was a nonsignificant finding that length of stay of elective patients was between half and a third that of nonelective surgery patients. Due to smaller patient numbers, we were unable to perform detailed comparisons of individual demographics or specific complications. This study would be more powerful when repeated with a larger data set and could therefore be worth revisiting.
The 30-day mortality rates we report for nonemergency and elective hip surgery in patients with DNR status are higher than those reported in the literature and also higher than age and comorbidity-matched patients using the NSQIP risk calculator.16,17 We found that in our cohort, the NSQIP-ACS risk calculator18 had underestimated mortality considerably for patients with the demographics and comorbidities found in our sample. The calculator predicted average mortality of 12% for emergency and 7% for nonemergency hip fracture surgery. In contrast, we found average mortality of 21.4% for emergent and 16.4% for nonemergent hip surgery in our DNR status patients. Informed consent and shared decision-making requires disclosure of outcomes specific to the patient and the procedure. The onus is on the physician to provide accurate risk assessment; however, there are pitfalls if models are based on samples that do not represent the patient in question well, thus over- or underestimating risk.19,20 This study provides outcomes that may be more relevant specifically to patients with DNR status undergoing a range of hip surgeries, whether elective, emergency, or otherwise.
Our finding reaffirms that patients with DNR status are a cohort in whom hip surgery is inherently high risk, apparently regardless of the urgency of surgery. Although there are myriad different ethical or social reasons influencing assignment of DNR status, healthcare providers associate DNR status with minimal physiological reserve, especially in the surgical patient. While DNR is not a variable that is currently included in any surgical risk stratification system, it may be useful to consider our findings when assessing risk–benefit of elective and nonelective surgeries in these patients. High mortality in itself is not a barrier to surgery in the elderly individuals, as surgery can relieve pain and improve morbidity, which are important targets, while keeping with a patient’s goals of care, even if survival and discharge do not subsequently occur.
In a review of Medicare data, Kwok et al determined that of those patients aged 65 and older who died in 2008, 31.9% underwent a surgical procedure in the year before death, 18.3% underwent a procedure in the last months of life, and 8.0% underwent a procedure in the last week of life.21 This analysis highlights the fact that surgical care of the elderly individual is frequently conducted near the end of their life. Hip surgery consists of a spectrum of emergency through to elective indications, presenting a target for harm avoidance or reduction in those nearing the end of life. For some patients, elective procedures might be avoided after careful risk–benefit analysis; however, other patients with an existing DNR status may require unavoidable emergency hip surgery, and high-risk surgery may be appropriate with either curative or predominantly palliative intent. All these patients require informed consent, so understanding patterns of adverse events is important.
Case law has changed in recent years, and the standard of practice is to disclose all risks that a “prudent patient” would want to know, rather than those that a “reasonable physician” would explain.22 With increasing availability of risk calculators to bring representative statistics to the patient, increasingly surgeons, anesthesiologist, and other healthcare providers have the option to discuss risk quantitatively rather than qualitatively.23 Assessing the reproducibility or accuracy of these risk calculators in specific patient subgroup is an important process. While the cohort of orthopedic patients with DNR status is relatively small, it is not insignificant and it is growing, particularly for trauma. We hope that our outcome data, which are specific to this group, can be used to communicate risk more accurately.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Kazaure H, Roman S, Sosa JA. High mortality in surgical patients with do-not-resuscitate orders: analysis of 8256 patients. Arch Surg. 2011;146(8):922–928. [DOI] [PubMed] [Google Scholar]
- 2. Le Manach Y, Collins G, Bhandari M, et al. Outcomes after hip fracture surgery compared with elective total hip replacement. JAMA. 2015;314(11):1159–1166. [DOI] [PubMed] [Google Scholar]
- 3. Garg R, Bhalotra AR, Bhadoria P, Gupta N, Anand R. Reasons for cancellation of cases on the day of surgery—a prospective study. Indian J Anaesth. 2009;53(1):35–39. [PMC free article] [PubMed] [Google Scholar]
- 4. Mohanty S, Rosenthal RA, Russell MM, Neuman MD, Ko CY, Esnaola NF. Optimal perioperative management of the geriatric patient: best practices guideline from ACS NSQIP®/American Geriatrics Society. J Am Coll Surg. 2016;222(5):930–947. [DOI] [PubMed] [Google Scholar]
- 5. Dall TM, Gallo PD, Chakrabarti R, West T, Semilla AP, Storm MV. An aging population and growing disease burden will require a large and specialized health care workforce by 2025. Health Aff (Millwood). 2013;32(11):2013–2020. [DOI] [PubMed] [Google Scholar]
- 6. Deiner S, Westlake B, Dutton RP. Patterns of surgical care and complications in elderly adults. J Am Geriatr Soc. 2014;62(5):829–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Søreide K, Desserud KF. Emergency surgery in the elderly: the balance between function, frailty, fatality and futility. Scand J Trauma Resusc Emerg Med. 2015;23:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. La Puma J, Silverstein MD, Stocking CB, Roland D, Siegler M. Life-sustaining treatment: a prospective study of patients with DNR orders in a teaching hospital. Arch Intern Med. 1988;148(10):2193–2198. [DOI] [PubMed] [Google Scholar]
- 9. Ooi LH, Wong TH, Toh CL, Wong HP. Hip fractures in nonagenarians--a study on operative and non-operative management. Injury. 2005;36(1):142–147. [DOI] [PubMed] [Google Scholar]
- 10. Marks R. Non-operative management of hip osteoarthritis. Pain Stud Treat. 2015;3(2):7–22. [Google Scholar]
- 11. Shiloach M, Frencher SK, Jr, Steeger JE, et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2010;210(1):6–16. [DOI] [PubMed] [Google Scholar]
- 12. Ethical guidelines for the anesthesia care of patients with do-not-resuscitate orders or other directives that limit treatment. October 16, 2013. http://www.asahq.org/∼/media/Sites/ASAHQ/Files/Public/Resources/standards-guidelines/ethical-guidelines-for-the-anesthesia-care-of-patients.pdf. Accessed December 20, 2016.
- 13. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–191. [DOI] [PubMed] [Google Scholar]
- 14. Ingraham AM, Cohen ME, Raval MV, Ko CY, Nathens AB. Comparison of hospital performance in emergency versus elective general surgery operations at 198 hospitals. J Am Coll Surg. 2011;212(1):20–28.e21. [DOI] [PubMed] [Google Scholar]
- 15. Sathiyakumar V, Greenberg SE, Molina CS, Thakore RV, Obremskey WT, Sethi MK. Hip fractures are risky business: an analysis of the NSQIP data. Injury. 2015;46(4):703–708. [DOI] [PubMed] [Google Scholar]
- 16. Blom A, Pattison G, Whitehouse S, Taylor A, Bannister G. Early death following primary total hip arthroplasty: 1,727 procedures with mechanical thrombo-prophylaxis. Acta Orthopaedica. 2006;77(3):347–350. [DOI] [PubMed] [Google Scholar]
- 17. Berstock JR, Beswick AD, Lenguerrand E, Whitehouse MR, Blom AW. Mortality after total hip replacement surgery: a systematic review. Bone Joint Res. 2014;3(6):175–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Development and evaluation of the Universal ACS NSQIP surgical risk calculator: a decision aide and informed consent tool for patients and surgeons. J Am Coll Surg. 2013;217(5):833–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ramesh VJ, Rao GS, Guha A, Thennarasu K. Evaluation of POSSUM and P-POSSUM scoring systems for predicting the mortality in elective neurosurgical patients. Br J Neurosurg. 2008;22(2):275–278. [DOI] [PubMed] [Google Scholar]
- 20. Gomes A, Rocha R, Marinho R, et al. Colorectal surgical mortality and morbidity in elderly patients: comparison of POSSUM, P-POSSUM, CR-POSSUM, and CR-BHOM. Int J Colorectal Dis. 2015;30(2):173–179. [DOI] [PubMed] [Google Scholar]
- 21. Kwok AC, Semel ME, Lipsitz SR, et al. The intensity and variation of surgical care at the end of life: a retrospective cohort study. Lancet. 378(9800):1408–1413. [DOI] [PubMed] [Google Scholar]
- 22. Murray B. Informed consent: what must a physician disclose to a patient? Virtual Mentor. 2012;14(7):563–566. [DOI] [PubMed] [Google Scholar]
- 23. Dennehy L, White S. Consent, assent, and the importance of risk stratification. Br J Anaesth. 2012;109(1):40–46. [DOI] [PubMed] [Google Scholar]