Abstract
The modified Rodnan skin score (mRSS) is a measure of skin thickness and is used as a primary or secondary outcome measure in clinical trials of systemic sclerosis (scleroderma). This state-of-art review provides a historical perspective of the development of the mRSS, summarizes the performance of mRSS as an outcome measure, provides guidance on assessing mRSS, and makes recommendations for incorporation of the mRSS into clinical trials.
Introduction
The modified Rodnan skin score (mRSS) is a measure of skin thickness and is used as a primary or secondary outcome measure in clinical trials of systemic sclerosis (SSc, scleroderma). This article gives a brief history of the development of the mRSS, outlines practical aspects of assessing mRSS in clinical trials, and provides recommendations for the use of the mRSS in Phase 2 and 3 clinical trials where change in skin thickness is the primary or secondary outcome measure. This document highlights the views of scleroderma experts and is not meant to be used as a regulatory document.
Natural history of skin involvement in SSc
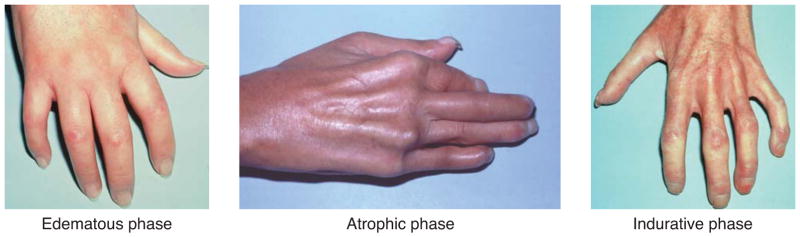
SSc is subclassified into diffuse cutaneous SSc (dcSSc) or limited cutaneous SSc (lcSSc) based on the extent of skin involvement. lcSSc is defined as skin thickening distal to the elbows and knees, with or without involvement of the face. dcSSc is characterized by the presence of skin thickening, proximal as well as distal, to the elbows and knees with or without involvement of the face(7). It is generally accepted that skin thickness tends to increase in early dcSSc and decrease in late dcSSc, although the time of peak involvement is typically 12–18 months after the onset of skin thickening. “Early” dcSSc is often defined as the period of rapidly increasing induration (“thickening”) of the skin. Although there is substantial individual heterogeneity, skin involvement in dcSSc may go through 3 phases: (i) an edematous phase that usually lasts 6–12 months; (ii) a fibrotic or indurative phase that lasts from 1–4 years or longer; and (iii) an atrophic phase that lasts for rest of the patient’s life, although rarely patients have a recurrence of progressive skin involvement in later disease (Figure 1). The duration of each phase may differ in each individual patient and the phases often overlap each other. The course of skin thickness also differs by serum autoantibodies—patients with anti-RNA polymerase-III tend to have more rapid progression than do those with anti-Scl-70 (topoisomerase I) antibody. In lcSSc, there is little change in skin thickness over time except in the subset who are anti-Scl-70 positive and progress to dcSSc over time(8).
Figure 1.
Three phases of skin involvement in diffuse cutaneous systemic sclerosis.
Skin thickness as surrogate of disease severity and mortality
Measurement of skin thickness is used as a surrogate for disease activity, severity and mortality in patients with dcSSc. In early dcSSc, an increase in skin thickening is generally associated with new or worsening internal organ involvement and increased mortality (7, 3). Worsening mRSS is associated with higher mortality, and both negative renal and cardiac outcomes (11). Internal organ involvement or worsening are particularly associated with the prior trajectory of skin thickening(7), and higher skin thickness progression rates are predictive of internal organ involvement and mortality(8, 1). In addition, patients who never achieved a high skin score have a lower frequency of major organ-based complications, and those with high skin scores that failed to improve by 3 years of disease have significantly higher mortality. Conversely, attenuation of peak skin score or improvement is associated with favorable outcomes, including better survival(11, 12). These points emphasize the potential benefit of including milder or early cases of SSc in clinical trials, such as designing studies to evaluate either a preventative (less worsening/less peak of mRSS) and/or improvement strategy(10, 6)
Historical perspective
Dr. Gerald Rodnan at the University of Pittsburgh theorized about, and then studied, the trajectory of skin thickening in the course of SSc. He noted that the skin, particularly the dermis, thickened initially and after some years usually thinned. He became convinced that an observer could, with practice, accurately estimate how thick skin is by palpating it. To substantiate his point, he developed a method for estimating thickness by clinical palpation using a 0–4 scale. He performed an experiment in which he estimated skin thickness of the distal forearm by skin palpation in patients with SSc and then performed a skin punch biopsy in that same location. He then weighed the plug of skin from the biopsy. The correlation between his clinical estimate of thickness and the weight of a 7-mm punch biopsy plug was 0.81(2). He further explored clinical palpation for estimating skin thickness in 26 cutaneous sites. The first full description of his methodology was published in 1982 in the context of a controlled study of D-penicillamine in SSc(5).
Some years later, Dr. Rodnan’s colleagues modified his method by estimating skin thickness using a 0–3 scale in 17 body areas. Nine of the original areas (neck [1], shoulders [2], breasts [2], upper back [1], lower back [1], toes [2]) were dropped because clinical investigators found it too difficult to come to consensus due to high inter-observer variation. One of the first applications of this mRSS(11) was in a randomized clinical trial (RCT) of high-dose versus low-dose D-penicillamine in early dcSSc(11, 6).
During the same period when the mRSS was developed, several groups were exploring different ways of assessing global skin involvement in patients with SSc. For example, Kahaleh et. al. proposed a modification of the Rodnan technique for measuring skin thickness (scores ranged from 0–66)(4). Investigators at UCLA developed a skin scoring technique which involved assessment of skin tethering or hidebinding in 10 body areas (scores ranged from 0–30)(8). Another method assessed the percentage of total body surface area affected by scleroderma(6). However, consensus was eventually reached where the mRSS became the gold standard for measuring skin thickness in SSc(6).
The modified Rodnan Skin Score (mRSS) as an outcome measure
The mRSS meets the OMERACT filters of truth, discrimination, and feasibility (Figure 2), as detailed in Merkel et al(7). Briefly, mRSS has the following characteristics:
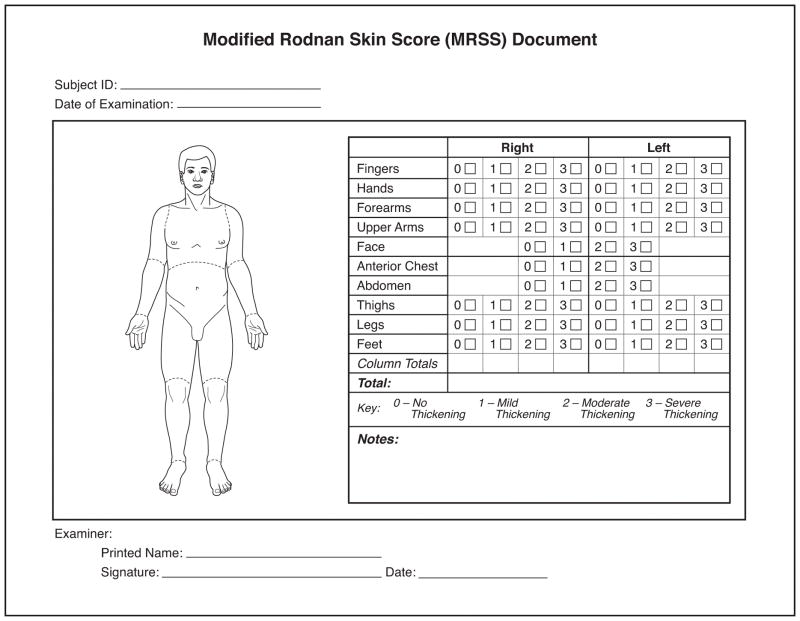
Figure 2.
Modified Rodnan skin score (mRSS) is assessed in 17 different areas. Case report form to capture mRSS.
Feasible: Easy to perform with no equipment and requires little time
Face Validity: Captures and measures skin thickness
Content Validity: Covers the affected body areas in SSc
Construct validity: Correlates with other measures of SSc such as durometer and ultrasound(5, 11)
Criterion Validity: Reflects the gold standard of skin biopsy(1). The correlation between clinical estimate of thickness by Dr. Rodnan and the weight of a 7-mm punch biopsy plug was 0.81(2). In addition, myofibroblast and hyalinized collagen scores on the skin biopsy correlated with the forearm mRSS score in a single center study(correlation coefficients of 0.83 and 0.78(11), respectively)
Sensitivity to change: Analysis of multicenter clinical trials show change over time. For example, the mRSS was able to differentiate between treatment with methotrexate and placebo in early dcSSc and between cyclophosphamide and placebo in the dcSSc subset in the Scleroderma Lung Study-I(25). The mRSS also improved in the Autologous Stem Cell Transplant Study(24) and showed a trend towards improvement with treatment with tociluzimab(10038). In addition, the minimal clinically important difference of the mRSS has been established in dcSSc and ranges between 3.5 to 5.3 units in the D-Penicillamine study (the mean baseline mRSS was 21 units(10)). The minimal clinically important difference estimates differ by the baseline mRSS and may be lower for recent trials that are recruiting milder skin thickening in dcSSc(10).
Utilizing the mRSS in clinical trials and routine care of systemic sclerosis
A. Practical aspects
-
1
Positioning of the patient: This is an important part of assessing mRSS. Each area examined should be in the relaxed position so the underlying muscles are relaxed to avoid falsely overestimating the area skin scores. Proper scoring cannot be done with patients in regular clothes. An examination gown or loose clothing is needed with appropriate use of sheet/drape. When evaluating the upper extremities, face, and anterior chest, we recommend the patient be seated in a relaxed position with arms by the side of the body. When evaluating the abdomen and lower extremities, we recommend the patient lie supine on an examination table or bed with the hips at 45 degrees’ flexion and feet are dorsiflexed.
-
2
Assessing skin thickness:
-
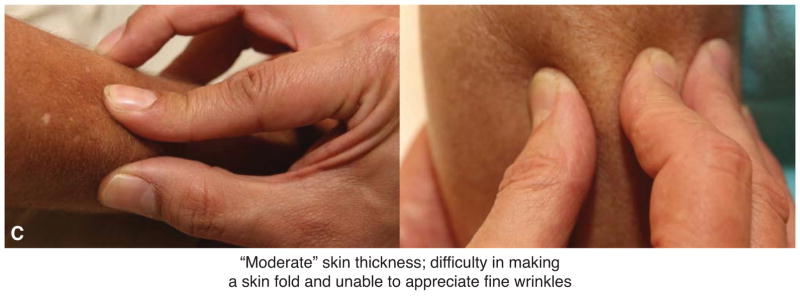
There are 2 techniques to accomplish this by palpation of the skin (Figure 3a).
Use an index finger and thumb where the skin is rolled or pinched gently to gauge thickness.
Use two thumbs to form a fold of skin between advancing lateral thumb borders. This method may be easier when skin overlies bone such as in the fingers and on the dorsum of the hands.
It is important to understand the relative distribution of subcutaneous fat and underlying musculoskeletal structures in different anatomical areas as they may alter the examiner’s appreciation of skin thickness.
Skin should be scored based on how it feels and not how it looks. For example, shiny skin or abnormally pigmented skin does not imply increased thickness.
-
Figure 3.
Figure 3a: Assessment of mRSS using index finger and thumb or two thumbs to measure thickness. mRSS =0 where there is no appreciable skin thickness.
Figure 3b: mRSS =1 where there is mild skin thickness.
Figure 3c: mRSS =2 where there is moderate skin thickness.
Figure 3d: mRSS =1 where there is severe skin thickness.
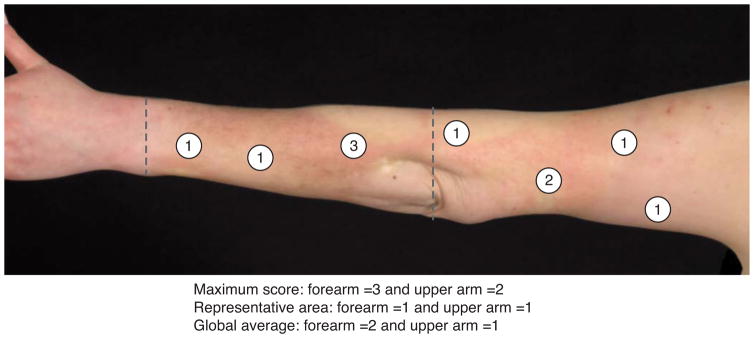
B. Global average vs. maximum score vs. most representative area of an anatomic area
There are differences in scoring mRSS in clinical practice but we recommend standardizing mRSS measurement in clinical trials. The 3 commonly used techniques include:
Maximum score: The examiner assigns a score to individual anatomic areas according to the most severe local involvement. For example, if the distal forearm has a patch considered 2 whereas the remainder of the forearm is 1, then would be given a score of 2 is recorded.
Representative area: The examiner scores individual areas with a score that is most representative of the area. In the example above, 1 would be the most representative score.
Global average: The examiner scores individual areas and takes average of the area. In the example above, 1 would be the most representative score. However, if the distal forearm had areas scored 2 and 3 whereas the majority of the forearm is 1, the average would be 2 (differs from representative area where the score would be 1). Some investigators prefer not to divide the scored region formally into subareas but prefer to provide an average score that reflects overall skin thickness and accounts for the observed variation in a more flexible fashion. Both methods are sound and acceptable.
We propose using either the “representative area” or “global average” method (Figure 4). In addition, there is a theoretical disadvantage of using “maximum score” as it may limit sensitivity to change. Consider an area over the forearm [as an example] that remains a 3 but the other forearm areas improve. Using maximum score, the forearm will continue to be scored as 3 despite definite improvement. One point of clarification is that if an area of skin has 1 but no more severe thickening, then the score of 1 is given; i.e. for global average, maximizing applies in this situation.
Figure 4.
Various techniques to assess mRSS of anatomic areas as shown over the forearm and upper arm.
-
3
Scoring of each individual cutaneous area (Figure 3a–3d):
mRSS =0 is “normal skin” where the examiner appreciates fine wrinkles but no skin thickness is present.
mRSS =1 is defined as definite but “mild” skin thickness where the examiner can easily make skin folds between 2 fingers; fine wrinkles are acceptable.
mRSS =2 is defined as “moderate” skin thickness with difficulty in making skin folds and no wrinkles.
mRSS =3 is defined as “severe” skin thickness with inability to make skin folds between 2 examining fingers.
-
4
The same examiner should evaluate the skin thickness throughout the trial: Each outcome measure inherently has measurement variability. It is recommended that the same assessor examine the patient for the duration of the trial. The inter-observer variability of the mRSS is 4.6 units (coefficient of variation=25%) and the intra-observer variability is 2.5 units (coefficient of variation= 12%)(11), with these variabilities better than that of measuring swollen and tender joint counts in rheumatoid arthritis, both part of the standard assessment in that disease(6, 7). Others have found similar results for the variability of the mRSS.
-
5
Teaching reduces variability of mRSS: The mRSS is a validated outcome in dcSSc but, as in rheumatoid arthritis, training assessors reduces variability. In a 12 investigator SSc teaching course, the ICC was 0.639, an acceptable reliability. On repeat training 7 months later, the ICC was 0.684, essentially the same. These data indicate that repeated retraining over time is not necessary (at least over 7 months). However, inter-investigator variability was high at both training sessions (standard deviation: 3.5–5.3) emphasizing that the intra-person reproducibility of the mRSS is much higher than between examiners; highlighting the need to have the same investigator consistently measuring the same patient(7).
Additional unpublished data comes from an investigator meeting where training was conducted as part of a phase II clinical trial in dcSSc. Fourteen investigators were asked to perform mRSS on 2 subjects with dcSSc. Immediately after the completion of mRSS, each investigator viewed a video demonstration by an expert examining a subject exhibiting different aspects of skin scoring, followed by a live demonstration by an expert on 1 subject with SSc on standardization of mRSS in clinical trials. Then, the investigators examined the same 2 subjects again and recorded their mRSS. Using a linear mixed model with random effects for both subjects and physicians, the results indicated that the video demonstration led to a decrease in the investigator variability (standard deviation decreased from 3.7 units before training to 1.6 units after training, a decrease of 56%), while the variability in mRSS attributable to variability among patients decreased less noticeably after training (2.5 units to 2.0 units after training). The latter is expected as the variability in mRSS captures the inherent heterogeneity in mRSS that exist across subjects.
-
6
Caveats in mRSS measurement
The edematous phase of dcSSc is usually associated with non-pitting edema of the skin. The mRSS may be difficult to assess during the edematous phase of SSc and mRSS has been shown to be inaccurate in this setting, with a correlation between an edema score on physical examination and edema on biopsy of 0.069–0.169(1). There is no agreement upon the approach for determining thickness when skin has edema. ‘Puffiness’ of the skin, generally fingers, is scored as 0.
Tethering or hidebinding is defined as strong attachment of the lower dermis to the underlying subcutaneous tissues, making skin movement difficult even in the absence of skin thickening. Although tethering can occur in the fibrotic phase of the disease, it is also associated with atrophic or “thin” skin. The mRSS does not score tethering.
Atrophic skin should be given a mRSS of 0, although this is erroneously scored as 3 due to underlying tethering.
-
7
Other aspects
Assessment in pediatric population: In healthy children, the texture of the skin shows age-appropriate skin thickness due to increased subcutaneous fat tissue compared to adults and correlates with the body mass index and the Tanner stage(1). In healthy children, skin is often appreciated as thicker due to increased subcutaneous fat. The latter is correlated with body mass index (BMI) and Tanner stage and decreases with age and sexual maturation. mRSS is not yet validated in juvenile SSc but there are ongoing international efforts to accomplish this. Therefore, the mRSS assessment should be performed in specialized pediatric scleroderma centers and should be corrected for BMI and Tanner stages.
Ethnicity differences: There are significant differences in mRSS in different ethnic groups in dcSSc patients. Japanese patients have lower mRSS in U.S. and British cohorts, although there is no study comparing mRSS by the same examiners in different populations. These differences could be explained, in part, by different distribution of SSc-related serum autoantibodies among ethnic groups; i.e., a higher proportion of anti-RNA polymerase III antibody in U.S. and British populations, compared with Japanese patients(2).
Measurement in limited cutaneous SSc: The mRSS can be assessed in lcSSc but in this population it is not a surrogate of disease severity or mortality and is generally not sensitive to change (likely due to a ceiling effect).
Recommendations for assessing mRSS in clinical trials
A. Phase 3 trial focused on mRSS as the primary outcome measure or a key secondary outcome measure
Training is strongly encouraged for standardization of mRSS in any clinical trial of SSc. Each assessor who will be performing mRSS in the trial should undergo training. It should be highlighted that the same assessor should perform mRSS during the course of the trial. We recommend 2 phases for training and this is based on successful training conducted during the phase II trial (discussed above in the section ‘Teaching reduces variability of mRSS’) and in an ongoing phase III trial.
Teaching phase: This should be accomplished by a video demonstration (by an expert examining a patient with SSc demonstrating different aspects of skin scoring) followed by a live demonstration by an expert on one or more patients with SSc.
-
Evaluation Phase: Each trainee examines at least 3 patients with SSc. These patients should be different than the training patients, and should preferably reflect the inclusion criteria for the proposed trial.
The expert should first examine each patient and record his/her mRSS.
Trainees should be given the mRSS sheet (Figure 2) and asked to examine each patient.
-
Due to the measurement variability in mRSS, we recommend the following criteria for certification for the clinical trial.
If the trainee is within +/−5 units of the expert’s total score (5 units is beyond the measurement variability of mRSS(11)) for each of the patients, then the trainee has passed the Evaluation phase.
If the trainee is within +/−5 units of the experts’ score for 2 of 3 patients, then the expert should review the discrepancies with the trainee and clarify concerns. The trainee should be asked to review the mRSS training video and then considered to have passed the Evaluation phase.
If the trainee is within +/−5 units of the experts’ score for 0 or 1 of 3 patients, then the trainee should repeat the training, either on the same day or at another time.
Certification (Figure 5): Due to logistical issues (requirements of patients and costs associated with live training), it may be appropriate to accept the certification for other trials if the assessor has undergone live training, passed the evaluation phase, and has performed the mRSS in an ongoing or recent trial within the last two years. This assumes that the assessor is currently performing mRSS in an ongoing trial or has done so in the recent past. In addition, regular evaluation should be conducted during the course of a trial to assess intra-rater reliability. Otherwise, they are encouraged to undergo recertification.
Figure 5.
An example of certification to be provided to trainees.
B. Phase 3 trial where mRSS is a secondary outcome measure or a Phase 2 trial focused on mRSS as the primary outcome measure or key secondary outcome measure
We encourage use the aforementioned plan for standardization of the mRSS, but we acknowledge the costs associated with training each assessor. In lieu of a formal training session, training at an investigator meeting could include a mRSS training video and live demonstration on a minimum of 1 SSc patient. Trainees should be provided enough time for clarifications. Each trainee should receive a certificate at the end of investigator meeting which should be part of the regulatory binder for the trial.
Finally, we recommend discussing the above-outlined guidance with the regulatory agencies associated with a specific research trial or drug development program.
C. Other practical aspects in a clinical trial
How often to conduct the mRSS: Based on change in mRSS in the published clinical trials and extensive experience of the authors in clinical practice, mRSS usually does not have clinically meaningful changes (≧4 points) in less than 3 months. However, there may be pharmacological targets where an earlier effect may be seen on mRSS. Therefore, it is reasonable to assess mRSS at least every 3 months in a clinical situation.
Avoid looking at prior mRSS scores and asking patients to judge change in skin score since the previous visit to reduce bias.
Ask patients to avoid application of moisturizers or cosmetics on day of skin scoring.
In conclusion, we have provided recommendations for performance of mRSS and have highlighted some areas of uncertainty that can form the agenda for future research.
Footnotes
CONFLICTS
Dr. Khanna has consultancy relationships with Actelion, Bayer, Bristol-Myers Squibb, ChemomAb, Corbus, Cytori, Eicos, EMD Serono, Genentech/Roche, Gilead, Glaxo SmithKline, MedImmune, Medac, and Sanofi-Aventis/Genzyme. He has received research funding from Astra-Zeneca, Bayer, Bristol-Myers Squibb, and Pfizer. This work was funded in part by the NIH/NIAMS K24 AR06312 grant.
Dr. Furst has consultancy relationships and/or has received research funding in relationship grant/research from Amgen, BMS, NIH, Novartis, Pfizer, Roche/Genentech, AbbVie, Amgen, BMS, Cytori, Janssen, NIH, Novartis, Pfizer, Roche/Genentech, and UCB.
Dr. Clements has no relevant conflicts.
Dr. Allanore has consultancy relationships and/or has received research funding in relationship with the treatment of systemic sclerosis from Actelion, Bayer, Biogen Idec, Bristol-Myers Squibb, Genentech/Roche, Inventiva, Medac, Pfizer, Sanofi/Genzyme, Servier and UCB.
Dr. Baron has no relevant conflicts.
Dr. Czirjak has consultancy relationships with the treatment of systemic sclerosis from Actelion, Bayer, Genentech/Roche, Inventiva, Medac, and Pfizer.
Dr. Distler has/had consulting relationships from 4 D Science, Actelion, Active Biotec, Chemom AG, Bayer, BiogenIdec, BMS, Boehringer Ingelheim, ChemomAb, EpiPharm, espeRare foundation, Genentech/Roche, GSK, Inventiva, Lilly, medac, Mepha, MedImmune, Pharmacyclics, Pfizer, Sanofi, Serodapharm, and Sinoxa; and grants from Actelion, Bayer, Boehringer Ingelheim, Pfizer, and Sanofi. Patent licensed: mir-29 for the treatment of systemic sclerosis. Speaker fees from AbbVie, iQone Healthcare, Mepha
Dr. Foeldvari has consultancy relationships with Bayer, Roche-Genentech, Novartis, Abbive, Chugai. Speakers fee: Pfizer, Abbvie, and Medac
Dr. Kuwana has consultancy or speaker fees from Bayer, Boehringer Ingelheim, Chugai, Actelion, and Glaxo SmithKline, and/or has received research funding from Chugai, Actelion, and Bayer.
Dr. Matucci-Cerinic has active consultancies or has received grant support from Amgen, BMS, Pfizer, Bruno farma, and Actelion. Consultant: BMS, Actelion, Pfizer, Inventiva, Chemomab
Dr. Mayes has consultancy relationship with and/or has received research funding from Bayer, Boehringer-Ingelheim, Corbus, Cytori, Genentech/Roche.
Dr. Medsger has consultancy relationship with iBio.
Dr. Merkel has consultancy relationship with and/or has received research funding from Actelion, Bristol-Myers Squibb, ChemoCentryx, Genentech/Roche, Glaxo SmithKline, Kypha, MedImmune/AztraZeneca, PrincipoBio, Sanofi-Aventis/Genzyme.
Dr. Pope has consultancy relationship with AbbVie, Actelion, Amgen, Bayer, BMS, Hospira, Janssen, Lilly, Merck, Novartis, Pfizer, Roche, Sanofi, UCB.
Dr. Seibold has consultancy relationship with Anthera, Bayer, BioGen IDEC, Blade Therapeutics, Boehringer Ingelheim, Covis Pharma, Cytori, Eiger, EMD Serono, Milestone, Mitsubishi, Sanofi-Aventis, Teva and Xenikos. There are no speaker’s bureaus or stock holdings.
Dr. Steen has consultancy fees from Bristol Myers Squibb, Cytori, Bayer, Gilead, and research grant funding from CSL Behring, United Therapeutics and Gilead, and Clinical Trial research funding from Cytori, Roche, Boehringer Ingelheim, EMD Serono, Covis, and Reata
Dr. Stevens has consultancy relationship or received research funding form Actelion, GSK, Bayer and Pfizer and has received speakers fees from Actelion and GSK
Dr. Denton has consultancy relationships with or speaker fees from Actelion, Bristol-Myers Squibb, GlaxoSmithKline, Bayer, Sanofi-Aventis, Boehringer Ingelheim, Genentech-Roche, and CSL Behring, and research grant funding from GlaxoSmithKline, Actelion, Novartis, CSL Behring.
References
- 1.LeRoy EC, Medsger TA., Jr Criteria for the classification of early systemic sclerosis. J Rheumatol. 2001;28(7):1573–6. Epub 2001/07/27. [PubMed] [Google Scholar]
- 2.Perera A, Fertig N, Lucas M, Rodriguez-Reyna TS, Hu P, Steen VD, Medsger TA., Jr Clinical subsets, skin thickness progression rate, and serum antibody levels in systemic sclerosis patients with anti-topoisomerase I antibody. Arthritis and rheumatism. 2007;56(8):2740–6. doi: 10.1002/art.22747. [DOI] [PubMed] [Google Scholar]
- 3.Shand L, Lunt M, Nihtyanova S, Hoseini M, Silman A, Black CM, Denton CP. Relationship between change in skin score and disease outcome in diffuse cutaneous systemic sclerosis: application of a latent linear trajectory model. Arthritis Rheum. 2007;56(7):2422–31. doi: 10.1002/art.22721. [DOI] [PubMed] [Google Scholar]
- 4.Clements PJ, Wong WK, Hurwitz EL, Furst DE, Mayes M, White B, Wigley F, Weisman M, Barr W, Moreland L, Medsger TA, Jr, Steen V, Martin RW, Collier D, Weinstein A, Lally E, Varga J, Weiner SR, Andrews B, Abeles M, Seibold JR. The Disability Index of the Health Assessment Questionnaire is a predictor and correlate of outcome in the high-dose versus low-dose penicillamine in systemic sclerosis trial. Arthritis Rheum. 2001;44(3):653–61. doi: 10.1002/1529-0131(200103)44:3<653::AID-ANR114>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 5.Clements PJ, Hurwitz EL, Wong WK, Seibold JR, Mayes M, White B, Wigley F, Weisman M, Barr W, Moreland L, Medsger TA, Jr, Steen VD, Martin RW, Collier D, Weinstein A, Lally E, Varga J, Weiner SR, Andrews B, Abeles M, Furst DE. Skin thickness score as a predictor and correlate of outcome in systemic sclerosis: high-dose versus low-dose penicillamine trial. Arthritis Rheum. 2000;43(11):2445–54. doi: 10.1002/1529-0131(200011)43:11<2445::AID-ANR11>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 6.Domsic RT, Rodriguez-Reyna T, Lucas M, Fertig N, Medsger TA., Jr Skin thickness progression rate: a predictor of mortality and early internal organ involvement in diffuse scleroderma. Ann Rheum Dis. 2011;70(1):104–9. doi: 10.1136/ard.2009.127621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Steen VD, Medsger TA., Jr Improvement in skin thickening in systemic sclerosis associated with improved survival. Arthritis and rheumatism. 2001;44(12):2828–35. doi: 10.1002/1529-0131(200112)44:12<2828::aid-art470>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 8.Dobrota R, Maurer B, Graf N, Jordan S, Mihai C, Kowal-Bielecka O, Allanore Y, Distler O, et al. Prediction of improvement in skin fibrosis in diffuse cutaneous systemic sclerosis: a EUSTAR analysis. Annals of the rheumatic diseases. 2016;75(10):1743–8. doi: 10.1136/annrheumdis-2015-208024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maurer B, Graf N, Michel BA, Muller-Ladner U, Czirjak L, Denton CP, Tyndall A, Metzig C, Lanius V, Khanna D, Distler O, et al. Prediction of worsening of skin fibrosis in patients with diffuse cutaneous systemic sclerosis using the EUSTAR database. Annals of the rheumatic diseases. 2015;74(6):1124–31. doi: 10.1136/annrheumdis-2014-205226. [DOI] [PubMed] [Google Scholar]
- 10.Rodnan GP, Lipinski E, Luksick J. Skin thickness and collagen content in progressive systemic sclerosis and localized scleroderma. Arthritis Rheum. 1979;22(2):130–40. doi: 10.1002/art.1780220205. [DOI] [PubMed] [Google Scholar]
- 11.Steen VD, Medsger TA, Jr, Rodnan GP. D-Penicillamine therapy in progressive systemic sclerosis (scleroderma): a retrospective analysis. Annals of internal medicine. 1982;97(5):652–9. doi: 10.7326/0003-4819-97-5-652. [DOI] [PubMed] [Google Scholar]
- 12.Clements PJ, Lachenbruch PA, Seibold JR, Zee B, Steen VD, Brennan P, Silman AJ, Allegar N, Varga J, Massa M, et al. Skin thickness score in systemic sclerosis: an assessment of interobserver variability in 3 independent studies. The Journal of rheumatology. 1993;20(11):1892–6. [PubMed] [Google Scholar]
- 13.Clements PJ, Furst DE, Wong WK, Mayes M, White B, Wigley F, Weisman MH, Barr W, Moreland LW, Medsger TA, Jr, Steen V, Martin RW, Collier D, Weinstein A, Lally E, Varga J, Weiner S, Andrews B, Abeles M, Seibold JR. High-dose versus low-dose D-penicillamine in early diffuse systemic sclerosis: analysis of a two-year, double-blind, randomized, controlled clinical trial. Arthritis and rheumatism. 1999;42(6):1194–203. doi: 10.1002/1529-0131(199906)42:6<1194::AID-ANR16>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 14.Kahaleh MB, Sultany GL, Smith EA, Huffstutter JE, Loadholt CB, LeRoy EC. A modified scleroderma skin scoring method. Clin Exp Rheumatol. 1986;4(4):367–9. [PubMed] [Google Scholar]
- 15.Clements PJ, Lachenbruch PA, Ng SC, Simmons M, Sterz M, Furst DE. Skin score. A semiquantitative measure of cutaneous involvement that improves prediction of prognosis in systemic sclerosis. Arthritis Rheum. 1990;33(8):1256–63. doi: 10.1002/art.1780330828. [DOI] [PubMed] [Google Scholar]
- 16.Mendoza FA, Nagle SJ, Lee JB, Jimenez SA. A prospective observational study of mycophenolate mofetil treatment in progressive diffuse cutaneous systemic sclerosis of recent onset. The Journal of rheumatology. 2012;39(6):1241–7. doi: 10.3899/jrheum.111229. [DOI] [PubMed] [Google Scholar]
- 17.Clements PJ. Measuring disease activity and severity in scleroderma. Current opinion in rheumatology. 1995;7(6):517–21. [PubMed] [Google Scholar]
- 18.Merkel PA, Aydin SZ, Boers M, Direskeneli H, Herlyn K, Seo P, Suppiah R, Tomasson G, Luqmani RA. The OMERACT core set of outcome measures for use in clinical trials of ANCA-associated vasculitis. J Rheumatol. 2011;38(7):1480–6. doi: 10.3899/jrheum.110276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Merkel PA, Silliman NP, Denton CP, Furst DE, Khanna D, Emery P, Hsu VM, Streisand JB, Polisson RP, Akesson A, Coppock J, van den Hoogen F, Herrick A, Mayes MD, Veale D, Seibold JR, Black CM, Korn JH Group CATR, Scleroderma Clinical Trials C. Validity, reliability, and feasibility of durometer measurements of scleroderma skin disease in a multicenter treatment trial. Arthritis and rheumatism. 2008;59(5):699–705. doi: 10.1002/art.23564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wiese AB, Berrocal VJ, Furst DE, Seibold JR, Merkel PA, Mayes MD, Khanna D. Correlates and responsiveness to change of measures of skin and musculoskeletal disease in early diffuse systemic sclerosis. Arthritis care & research. 2014;66(11):1731–9. doi: 10.1002/acr.22339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Furst DE, Clements PJ, Steen VD, Medsger TA, Jr, Masi AT, D’Angelo WA, Lachenbruch PA, Grau RG, Seibold JR. The modified Rodnan skin score is an accurate reflection of skin biopsy thickness in systemic sclerosis. J Rheumatol. 1998;25(1):84–8. [PubMed] [Google Scholar]
- 22.Kissin EY, Merkel PA, Lafyatis R. Myofibroblasts and hyalinized collagen as markers of skin disease in systemic sclerosis. Arthritis Rheum. 2006;54(11):3655–60. doi: 10.1002/art.22186. [DOI] [PubMed] [Google Scholar]
- 23.Tashkin DP, Elashoff R, Clements PJ, Goldin J, Roth MD, Furst DE, Arriola E, Silver R, Strange C, Bolster M, Seibold JR, Riley DJ, Hsu VM, Varga J, Schraufnagel DE, Theodore A, Simms R, Wise R, Wigley F, White B, Steen V, Read C, Mayes M, Parsley E, Mubarak K, Connolly MK, Golden J, Olman M, Fessler B, Rothfield N, Metersky M Scleroderma Lung Study Research G. Cyclophosphamide versus placebo in scleroderma lung disease. N Engl J Med. 2006;354(25):2655–66. doi: 10.1056/NEJMoa055120. [DOI] [PubMed] [Google Scholar]
- 24.van Laar JM, Farge D, Sont JK, Naraghi K, Marjanovic Z, Larghero J, Schuerwegh AJ, Marijt EW, Vonk MC, Schattenberg AV, Matucci-Cerinic M, Voskuyl AE, van de Loosdrecht AA, Daikeler T, Kotter I, Schmalzing M, Martin T, Lioure B, Weiner SM, Kreuter A, Deligny C, Durand JM, Emery P, Machold KP, Sarrot-Reynauld F, Warnatz K, Adoue DF, Constans J, Tony HP, Del Papa N, Fassas A, Himsel A, Launay D, Lo Monaco A, Philippe P, Quere I, Rich E, Westhovens R, Griffiths B, Saccardi R, van den Hoogen FH, Fibbe WE, Socie G, Gratwohl A, Tyndall A, Group EESS. Autologous hematopoietic stem cell transplantation vs intravenous pulse cyclophosphamide in diffuse cutaneous systemic sclerosis: a randomized clinical trial. Jama. 2014;311(24):2490–8. doi: 10.1001/jama.2014.6368. [DOI] [PubMed] [Google Scholar]
- 25.Khanna D, Denton CP, Jahreis A, van Laar JM, Frech TM, Anderson ME, Baron M, Chung L, Fierlbeck G, Lakshminarayanan S, Allanore Y, Pope JE, Riemekasten G, Steen V, Muller-Ladner U, Lafyatis R, Stifano G, Spotswood H, Chen-Harris H, Dziadek S, Morimoto A, Sornasse T, Siegel J, Furst DE. Safety and efficacy of subcutaneous tocilizumab in adults with systemic sclerosis (faSScinate): a phase 2, randomised, controlled trial. Lancet. 2016;387(10038):2630–40. doi: 10.1016/S0140-6736(16)00232-4. [DOI] [PubMed] [Google Scholar]
- 26.Khanna D, Furst DE, Hays RD, Park GS, Wong WK, Seibold JR, Mayes MD, White B, Wigley FF, Weisman M, Barr W, Moreland L, Medsger TA, Jr, Steen VD, Martin RW, Collier D, Weinstein A, Lally EV, Varga J, Weiner SR, Andrews B, Abeles M, Clements PJ. Minimally important difference in diffuse systemic sclerosis: results from the D-penicillamine study. Annals of the rheumatic diseases. 2006;65(10):1325–9. doi: 10.1136/ard.2005.050187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Scott DL, Choy EH, Greeves A, Isenberg D, Kassinor D, Rankin E, Smith EC. Standardising joint assessment in rheumatoid arthritis. Clinical rheumatology. 1996;15(6):579–82. doi: 10.1007/BF02238547. [DOI] [PubMed] [Google Scholar]
- 28.Pope JE, Baron M, Bellamy N, Campbell J, Carette S, Chalmers I, Dales P, Hanly J, Kaminska EA, Lee P, et al. Variability of skin scores and clinical measurements in scleroderma. The Journal of rheumatology. 1995;22(7):1271–6. [PubMed] [Google Scholar]
- 29.Czirjak L, Nagy Z, Aringer M, Riemekasten G, Matucci-Cerinic M, Furst DE, Eustar The EUSTAR model for teaching and implementing the modified Rodnan skin score in systemic sclerosis. Ann Rheum Dis. 2007;66(7):966–9. doi: 10.1136/ard.2006.066530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Foeldvari I, Wierk A. Healthy children have a significantly increased skin score assessed with the modified Rodnan skin score. Rheumatology. 2006;45(1):76–8. doi: 10.1093/rheumatology/kei106. [DOI] [PubMed] [Google Scholar]
- 31.Sobanski V, Dauchet L, Lefevre G, Lambert M, Morell-Dubois S, Sy T, Hachulla E, Hatron PY, Launay D, Dubucquoi S. Prevalence of anti-RNA polymerase III antibodies in systemic sclerosis: New data from a French cohort and a systematic review and meta-analysis. Arthritis & rheumatology. 2014;66(2):407–17. doi: 10.1002/art.38219. [DOI] [PubMed] [Google Scholar]